Back to Journals » Clinical Ophthalmology » Volume 12
Visual outcomes, efficacy, and surgical complications associated with intracameral phenylephrine 1.0%/ketorolac 0.3% administered during cataract surgery
Authors Rosenberg ED, Nattis AS , Alevi D, Chu RL, Bacotti J , LoPinto RJ , D'Aversa G, Donnenfeld ED
Received 20 August 2017
Accepted for publication 22 November 2017
Published 21 December 2017 Volume 2018:12 Pages 21—28
DOI https://doi.org/10.2147/OPTH.S149581
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Eric D Rosenberg,1 Alanna S Nattis,2 David Alevi,3 Rachel L Chu,4 Joseph Bacotti,3 Ronald J LoPinto,3 Gerald D’Aversa,3 Eric D Donnenfeld5
1New York Medical College, Valhalla, NY, 2Lindenhurst Eye Physicians and Surgeons, Babylon, NY, 3Ophthalmic Consultants of Long Island, Rockville Centre, NY, 4Cornell University, Ithaca, NY, 5New York University Medical Center, New York, NY, USA
Aim: The purpose of this study was to compare visual outcomes, surgical time, and perioperative surgical complications after intracameral use of either phenylephrine/ketorolac (P/K) or epinephrine (Epi) during cataract surgery.
Methods: This was a single-center, retrospective case review of patients undergoing cataract surgery from August to November 2015. Of the 641 eyes of 389 patients who underwent cataract surgery, 260 eyes were administered phenylephrine 1.0%/ketorolac 0.3% and 381 eyes received Epi in the irrigation solution intraoperatively. All patients received a topical nonsteroidal anti-inflammatory drug regimen (bromfenac 0.07%, nepafenac 0.3%, or ketorolac 0.5%) for 3 days before surgery and topical tropicamide 1.0%, cyclopentolate 1.0%, and phenylephrine 2.5% on the day of surgery.
Results: Mean length of surgery (LOS) was 15.4±0.6 minutes. Although a positive correlation was noted between patient age and LOS (p<0.001), P/K was associated with a decrease in the LOS, when controlled for age quartiles. A statistically significant lower incidence of complications (1.1%) was observed with P/K use than Epi (4.5%; p=0.018). Among surgeons who used mydriatic-assist devices more frequently, P/K use was associated with a reduction in the use of these devices (p<0.001). When controlling for age quartile, patients of age groups 69–76 and 76–92 years who received P/K had significantly better uncorrected visual acuity at postoperative day 1 than those receiving Epi (p=0.003).
Conclusion: Intracameral use of phenylephrine 1.0%/ketorolac 0.3% during cataract surgery may be effective in maintaining mydriasis. It appears to be superior to intracameral Epi at reducing intraoperative and postoperative complications, need for pupillary dilating devices, and surgical time.
Keywords: cataract surgery, complications, pupillary miosis, phenylephrine, ketorolac
Introduction
Cataract surgery is one of the most frequently performed procedures worldwide. Age-related cataracts alone are expected to affect more than 30 million Americans by 2020.1,2 Advancements in cataract surgery techniques, technology, and pharmaceutical therapies have reduced the risks associated with the procedure and improved outcomes. In recent years, cataract surgery has evolved into an outpatient, relatively pain-free procedure with rapid recovery of vision. Perhaps as a result, patients now have very high expectations of cataract surgery, including a low tolerance for complications and pain.3,4
A small pupil (<6.0 mm) or intraoperative miosis is known to make cataract surgery more technically challenging and increase the risk of surgical complications such as capsular tears, lens decentration, retained lens fragments, postoperative inflammation, or vitreous loss.5–10 One group of researchers found a twofold increase in complications with each 1.0 mm reduction in pupil size.6
There are a variety of therapeutic treatments aimed at improving pupillary dilation and preventing intraoperative miosis, including several topical agents that have been approved by the US Food and Drug Administration (FDA) for ophthalmic use. Preoperative dilation with topical sympathomimetics, such as phenylephrine, and anticholinergics, such as cyclopentolate or tropicamide, have a long track record of efficacy. Topical nonsteroidal anti-inflammatory drugs (NSAIDs) can also reduce the severity and incidence of intraoperative miosis by preventing prostaglandin synthesis.11,12 Topical agents administered preoperatively can, however, be washed out of the intracameral space by the irrigation solution used during cataract surgery.13 Cardiac sympathomimetics such as epinephrine (Epi) or phenylephrine added to the irrigating solution are effective at preventing miosis but are not FDA approved for this use and may be subject to formulation errors and/or contamination.
Recently, an intracameral combination drug (phenylephrine 1.0%/ketorolac 0.3%, Omidria; Omeros, Seattle, WA, USA) intended to be added to the irrigating solution, was approved for cataract and intraocular lens replacement surgery. Containing both an α1-adrenergic receptor agonist and a nonselective cyclooxygenase 1 and 2 inhibitor, phenylephrine/ketorolac (P/K) combination has been shown to maintain pupillary mydriasis and reduce postoperative pain in a Phase III multicenter, randomized study.14
NSAIDs and adrenoceptor agonist agents have a long-standing history of use in the management of ocular pathology and topical ophthalmic preparations. Although intracameral ketorolac has not been previously studied during cataract surgery, intracameral administration would be expected to have some advantages. Since the intracameral combination drug is introduced into the operative irrigation solution prior to the case, it does not require any modification to current surgical techniques or procedures. Additionally, presenting the combination therapy intracamerally exposes the target tissues to a consistent concentration of drug, maintaining the pharmacological effects.14 Other recognized advantages of P/K over current techniques include prevention of intraoperative miosis, reduction of pain and discomfort, management of postoperative inflammation, reduction in the number of pre- and postoperative topical drops, and the availability of a bisulfite-free preparation.8,14,15
In the very limited peer-reviewed literature examining this combined agent thus far, the drug has not been evaluated in patients with risk factors for intraoperative miosis such as intraoperative floppy iris syndrome (IFIS) or pseudoexfoliation.8,14 Additionally, while all subjects in the FDA trial received standardized topical preoperative mydriatics (phenylephrine and tropicamide) and anesthetics (lidocaine or tetracaine), they did not receive intracameral Epi or a topical NSAID. The purpose of this study was to evaluate, in a real-world setting, the incidence of perioperative complications, length of surgery (LOS), and use of pupil dilation devices in a broad patient population, including those with comorbid conditions that would make surgery more difficult, such as IFIS, pseudoexfoliation, and otherwise poorly dilating pupils. To reflect common clinical practice, the P/K treatment group was compared to a control group receiving intracameral Epi, and all patients in the study received standard preoperative topical NSAIDs.
Methods
A single-center retrospective case review was performed for all cataract surgeries taking place at Island Eye Surgical Center, Carle Place, NY, over a 3-month period from August 2015 to November 2015, plus associated first-eye procedures as described below. Four surgeons (EDD, GD, JB, and RJL) were selected as having performed more than five cataract surgeries per week during the review period, including cases using intracameral P/K (Omidria) and cases using intracameral Epi without P/K. If the cataract surgery performed between the inclusion dates was a second-eye surgery, that subject’s first-eye surgery was included in the retrospective review as well, as long as the first eye underwent surgery after January 1, 2014. Exclusion criteria were age younger than 21 years, documented sensitivity to NSAIDs, and planned combined cataract and posterior segment surgeries. All other procedures performed by the selected surgeons during the review period were included. The study was conducted according to the tenets of the Declaration of Helsinki; additionally, this research was exempt from Institutional Review Board approval under the HHS policy: 45 CFR 46.101(b).
All patients received a topical NSAID regimen (bromfenac 0.07%, nepafanac 0.3%, or ketorolac 0.5%) for 3 days before surgery. On the day of surgery, all patients received topical tropicamide 1%, cyclopentolate 1%, and phenylephrine 2.5%. Depending upon the insurance coverage, either phenylephrine 1%/ketorolac 0.3% or Epi was used in the irrigation solution. P/K was stored between 20°C and 25°C and protected from ambient light at all times prior to use. Before each P/K case, one 4 mL single-patient-use vial of the combination drug was added to a 500 mL bottle of irrigation solution in the surgical suite. Once added to the irrigation solution, the drug was delivered intracamerally within the 4-hour recommended time frame. In the remaining patients, 1 cc of 1:1,000,000 concentration of bisulfite-free Epi was added to the irrigation solution.
Each chart was reviewed for surgeon name, date of surgery, age at time of surgery, sex, eye, use of the femtosecond laser, use of mydriatic-assist devices (Malyugin rings or iris hooks), use of P/K, history or current use of α1 antagonists, and perioperative complications. In addition, the charts of one surgeon (EDD, n=310 eyes) were reviewed for best-corrected visual acuity (BCVA) and uncorrected visual acuity (UCVA) preoperatively and at postoperative day 1 (POD 1) and month 1 (POM 1). All visual acuities were converted from Snellen to decimal format in order to facilitate calculation and statistical analysis.
Results were analyzed by age quartile. For statistical analyses, Student’s t-tests, correlation tests, z-score, analysis of variance (ANOVA), two-way ANOVA, and χ2 tests were utilized where appropriate. A p-value of <0.05 was considered significant. Regression models were fit to adjust for imbalance in group characteristics, and to assess the overall impact of independent variables on the outcomes of interest. Statistical analyses were performed using RStudio (https://www.r-project.org) and Excel (Microsoft Corporation, Redmond, WA, USA).
Results
Surgeons EDD, GD, JB, and RJL performed a total of 653 cataract surgery procedures during the review period. Twelve eyes were excluded based on previously indicated exclusion criteria. Of the 641 eyes of 389 patients analyzed, 413 were of female patients and 228 male; 323 were right eyes and 318 were left eyes. Fifty-three eyes had a positive history for α1 antagonist use. Two hundred seventy-eight eyes underwent pretreatment with the femtosecond laser. Of the 641 eyes, 260 were administered P/K intraoperatively, while the remaining 381 had Epi. The average age of a patient receiving phenylephrine/ketorolac was 75.4±0.9 years, while the average of a patient receiving Epi was 67.4±1.1 years (p<0.001). A mydriatic-assist device (Malyugin ring or iris hooks) was required to maintain mydriasis in 45 eyes.
Overall, the group receiving P/K were older than the group receiving Epi (Student’s t-test, p<0.0001), and more patients were female (Student’s t-test, p=0.0016) (Table 1). When comparing treatment groups across surgeons, the mean age of the groups receiving either P/K or Epi was significantly different (χ2, p=0.045 and p<0.0001, respectively), but the percent of female patients receiving P/K was similar for all surgeons (χ2, p=0.056). For both treatment groups, the percent of patients undergoing femtosecond laser was not significantly different overall (p=0.0980).
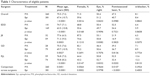  | Table 1 Characteristics of eligible patients |
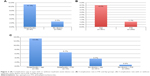
The average LOS was 15.4±0.6 minutes, ranging from 13.0±1.0 to 17.2±1.3 (Figure 1A and B). A positive correlation was noted between age and LOS (p<0.001) (Figure 1C). LOS was not exclusively dependent on sex (Student’s t-test, p=0.732) or eye (p=0.694), or use of P/K (p=0.676). However, when controlling for age quartile, the use of P/K was associated with a decrease in the LOS in most of the age quartiles compared to Epi (oldest quartile, age 78–92: 15.6±1.5 minutes vs 16.7±1.2 minutes; age 71–77: 16.0±1.8 vs 16.2±1.5; age 65–70: 13.7±1.7 vs 17.2±1.7; and youngest quartile, age 30–64: 10.2±3.7 vs 13.6±1.1; two-way ANOVA, p=0.049) (Figure 1D). In patients who received mydriatic-assist devices, or patients using α1 antagonists, the average LOS was longer (19.4±2.6 minutes vs 15.0±0.6 minutes, p<0.001, and 18.5±2.7 minutes vs 15.1±0.6 minutes, p<0.001, respectively). Interestingly, depending on the surgeon, utilizing the femtosecond laser either made surgeries quicker (EDD), slower (RJL), or did not affect the time (GD, JB) (Figure 1E).
Older age was associated with the use of mydriatic-assist devices (76.3±2.4 years vs 70.2±0.8 years, Student’s t-test, p<0.001) and α1 antagonist use (75.4±0.9 years vs 67.4±1.0 years, p<0.001). Patients electing to undergo pretreatment with the femtosecond laser were on average younger than those who preferred the traditional approach (69.4±1.2 years vs 71.6±1.1 years, Student’s t-test, p=0.005).
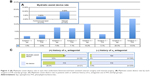
Complications noted during this study include dislocated lens with intraocular lens exchange or repositioning, retained lens fragments, lens fragments in the vitreous, wound leakage, capsular tear (with or without anterior vitrectomy), macular puckering following surgery, and retinal detachment following surgery. In total, 20 adverse events were recorded, for a complication rate of 3.1%. The incidence of complications was not associated with age (Student’s t-test, p=0.757). Complications were independent of surgeon (χ2 test, p=0.454), sex (p=0.371), eye (p=0.184), or history or current use of α1 antagonists (p=0.775). A higher incidence of complications was noted when mydriatic-assist devices were used (11.1% vs 2.5%, χ2 test, p=0.001), and a lower incidence of complications was appreciated when P/K was used (4.5% vs 1.1%, χ2 test, p=0.018) (Figure 2A and B). Complications occurred most frequently when mydriatic-assist devices were used in conjunction with intracameral Epi; conversely, complications occurred least frequently when P/K was administered without a mydriatic-assist device (χ2, p=0.001) (Figure 2C). There were no hemodynamically adverse events reported with P/K use intraoperatively.
Patients who had a history of, or were currently using, α1 antagonists were more likely to require mydriatic-assist devices (41.5% vs 3.9%, χ2, p<0.001). Patients who underwent pretreatment with the femtosecond laser were less likely to require mydriatic-assist devices (3.6% vs 9.6%, χ2, p=0.003) (Figure 3A). Mydriatic-assist devices were independent of P/K use (χ2, p=0.306). However, in surgeons who used mydriatic-assist devices more frequently, the use of P/K was associated with a reduction in the use of these devices (χ2, p<0.001) (Figure 3B). The use of P/K was also associated with a decreased need for mydriatic-assist devices in patients using α1 antagonists; however, this finding was not statistically significant due to the sample size (50% vs 28.6%, χ2, p=0.121, n=53) (Figure 3C).
The average preoperative BCVA was 0.50 (±0.03), while POD 1 and POM 1 UCVA were 0.40 (±0.03) and 0.78 (±0.03) respectively. There was no statistically significant difference in POD 1 UCVA or POM 1 BCVA between patients receiving P/K and those receiving Epi overall (Figure 4A). However, when controlling for age quartile, patients receiving P/K had significantly better POD 1 UCVA than those receiving Epi among the older two quartiles (age 69–76, 0.44±0.08 vs 0.38±0.10); age 76–92 (0.34±0.06 vs 0.23±0.08) (two-way ANOVA, p=0.003) (Figure 4B).
To assess the overall impact of independent variables on the outcomes of interest, logistic regression models were fit to adjust for the effect of surgeon, age quartile, sex, use of P/K, use of femtosecond laser, and α-antagonist use on the rate of complications and utilization of mydriatic-assist devices. In the overall sample, older age was associated with an increased rate of complications (p=0.01203), while use of P/K was associated with a significantly smaller rate of complications (p=0.0031) compared to Epi. Use of mydriatic-assist devices varied somewhat by surgeon, and was significantly lower in patients who underwent femtosecond-assisted laser procedures.
A linear regression model was fit to evaluate the effect of surgeon, age quartile, sex, use of femtosecond laser during surgery, and α-antagonist use on the length of surgical time. Overall, three surgeons (GD, JB, and RJL) all had significantly longer surgical times compared to EDD (p<0.05). Older age and use of α-antagonist medication were also associated with longer surgical times (p=0.0285 and p=0.0033, respectively).
Discussion
A previous study demonstrated the superiority of P/K vs placebo in maintaining mydriasis and reducing postoperative pain.14 This single-center, retrospective case study assessed the perioperative complications, surgical time, and visual outcomes of intracameral P/K vs Epi in a real-world setting. All patients received 3 days of preoperative topical NSAID, which was not given in the FDA trial. In addition, the control group in our study was administered intracameral Epi, which was not used in the FDA trial. Given the unique opportunity to study this drug in a typical practice setting, it was possible to analyze outcomes in a real-world treatment setting. Due to inclusion criteria in this study, patients receiving P/K were on average 8 years older than the control group receiving Epi-infused surgical irrigation fluid. Given the propensity for older individuals to have a positive history for α1-antagonist use, and the increased likelihood for mydriatric-assist device placement in older patients, it was surprising to find that perioperative complications remained fourfold less when the surgical protocol included P/K. Upon further investigation, there was a 17-fold increase in complications when mydriatic-assist devices were used in conjunction with intracameral Epi compared to cases with P/K and no mydriatic-assist devices; however, it should be noted that complications were halved when P/K was used in conjunction with a mydriatric-assist-device. It is conceivable that P/K increased overall visibility, thereby decreasing complication risk.7,16
One can assume that if a Malyugin ring or iris hooks were used intraoperatively, the surgeon judged the pupil to be miotic or considered there to be significant risk of miosis that warranted a pupillary expansion device.7 In the current study, we found a fourfold increase in complications associated with the use of mydriatic-assist devices. This increase in complications is thought secondary to the complexity of these types of cases, which are not uncommon in this referral group. Supporting this theory, we presented here that the use of P/K in α1-antagonist patients and the application of femtosecond laser in cataract surgery decreased the dependence on mydriatic-assist devices (-twofold and threefold, respectively). Additionally, in surgeons who used mydriatric-assist devices more frequently than 10% of the time, the application of P/K was found to decrease the need for mechanical dilatation.
Overall, there was no detectable difference in visual acuity between patients receiving P/K vs Epi-infused irrigation solution at POD 1 or POM 1. However, when controlling for age quartile, there was a significant improvement in POD 1 UCVA in the P/K eyes compared to the Epi eyes among the older age groups. The immediate improvement in POD 1 visual acuity may be attributed to the anti-inflammatory properties of ketorolac. Furthermore, the LOS was shorter in three of the four age quartiles when using P/K, independent of femtosecond laser application, which may have also contributed to the better postoperative results.
This study has several limitations worth noting. First, it was a single-center study with four surgeons, which may limit the generalizability of this study to other centers. With four surgeons, the total treatment effect may be confounded by differing technique or differing patient populations. We showed that the patient populations differed among surgeons by age, sex, and use of femtosecond laser. It is not clear whether these variables influenced the results in any tangible way. Additionally, it was a retrospective case review looking at a cohort of patients over a 4-month interval. While retrospective analyses lack the strength of a prospective, randomized trial, in this real-world setting a retrospective review may in fact decrease some elements of bias, particularly regarding surgeon performance. Therefore, the retrospective nature of this study best reflects the outcomes that occur in a natural practice setting. The window of analyzing complications ranged from 2 months to 1 year depending on the original date of surgery, which could lead to a lower number of complications detected among patients with the shortest follow-up. Patients were selected to receive P/K based on insurance status, which likely played a role in the older age in that group, but also may have introduced unintentional bias between treatment groups beyond the demographic information captured in Table 1. It is reasonable to suggest, however, that the older patients in the P/K group may have had a greater risk for complications, which would in fact attenuate the treatment effect. It should be noted that in this study the femtosecond laser was not utilized in patients with pupils <5 mm in size. Lastly, because complications were relatively infrequent, significant results were not always obtainable from the small sample sizes.
Conclusion
Cataract surgery is a well-established surgical procedure that provides expeditious functional visual improvement. Over time, innovation and improvement in existing procedural techniques along with pharmaceutical advancements have allowed cataract surgeons to reduce risk, enhance visual outcomes, and increase patient satisfaction. The addition of P/K to the surgeon’s regimen has been shown previously to maintain mydriasis and decrease postoperative pain.14 In this study, we also showed a decrease in intraoperative and postoperative complications, a reduction in the need for pupillary dilating devices, decreased age-adjusted surgical time, and an improvement in POD 1 UCVA in patients ≥69 years of age.
Acknowledgment
This study was supported by an unrestricted grant from Omeros Corporation (Seattle, WA, USA).
Disclosure
EDD is a consultant to Omeros. The authors report no other conflicts of interest in this work.
References
Gollogly HE, Hodge DO, St Sauver JL, Erie JC. Increasing incidence of cataract surgery: population-based study. J Cataract Refract Surg. 2013;39(9):1383–1389. | ||
Jay JL, Devlin ML. The increasing frequency of surgery for cataract. Eye. 1990;4(Pt 1):127–131. | ||
Fung D, Cohen MM, Stewart S, Davies A. What determines patient satisfaction with cataract care under topical local anesthesia and monitored sedation in a community hospital setting? Anesth Analg. 2005;100:1644–1650. | ||
Visser N, Nuijts RM, de Vries NE, Bauer NJ. Visual outcomes and patient satisfaction after cataract surgery with toric multifocal intraocular lens implantation. J Cataract Refract Surg. 2011;37(11):2034–2042. | ||
Ahmed A. Cataract surgery in small pupils: choosing the appropriate tool; 2013. Available from: http://crstodayeurope.com/articles/2013-sep/cataract-surgery-in-small-pupils-online-survey-choosing-the-appropriate-tool/. Accessed June 19, 2017. | ||
Guzek JP, Holm M, Cotter JB, et al. Risk factors for intraoperative complications in 1,000 extracapsular cataract cases. Ophthalmology. 1987;94(5):461–466. | ||
Hashemi H, Seyedian MA, Mohammadpour M. Small pupil and cataract surgery. Curr Opin Ophthalmol. 2015;26(1):3–9. | ||
Lawuyi LE, Gurbaxani A. The clinical utility of new combination phenylephrine/ketorolac injection in cataract surgery. Clin Ophthalmol. 2015;9:1249–1254. | ||
Mirza SA, Alexandridou A, Marshall T, Stavrou P. Surgically induced miosis during phacoemulsification in patients with diabetes mellitus. Eye. 2003;17(2):194–199. | ||
Narendran N, Jaycock P, Johnston RL, et al. The Cataract National Dataset electronic multicentre audit of 55,567 operations: risk stratification for posterior capsule rupture and vitreous loss. Eye. 2009;23(1):31–37. | ||
Donnenfeld ED. Current use of non-steroidal anti-inflammatory drugs in the treatment of ocular inflammation related to cataract surgery. Eur Ophthal Rev. 2012;6:172–177. | ||
Donnenfeld ED, Perry HD, Wittpenn JR, Solomon R, Nattis A, Chou T. Preoperative ketorolac tromethamine 0.4% in phacoemulsification outcomes: pharmacokinetic-response curve. J Cataract Refract Surg. 2006;32(9):1474–1482. | ||
Katsev DA, Katsev CC, Pinnow J, Lockhart CM. Intracameral ketorolac concentration at the beginning and end of cataract surgery following preoperative topical ketorolac administration. Clin Ophthalmol. 2017;11:1897–1901. | ||
Lindstrom RL, Loden JC, Walters TR, et al. Intracameral phenylephrine and ketorolac injection (OMS302) for maintenance of intraoperative pupil diameter and reduction of postoperative pain in intraocular lens replacement with phacoemulsification. Clin Ophthalmol. 2014;8:1735–1744. | ||
Colin J. The role of NSAIDs in the management of postoperative ophthalmic inflammation. Drugs. 2007;67(9):1291–1308. | ||
Malyugin B. Small pupil phaco surgery: a new technique. Ann Ophthalmol. 2007;39(3):185–193. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.