Back to Journals » Infection and Drug Resistance » Volume 17
Vancomycin Resistant Enterococci Prevalence, Antibiotic Susceptibility Patterns and Colonization Risk Factors Among HIV-Positive Patients in Health-Care Facilities in Debre Berhan Town, Ethiopia
Authors Zike M, Ahmed AM, Hailu A , Hussien B
Received 11 October 2023
Accepted for publication 29 December 2023
Published 3 January 2024 Volume 2024:17 Pages 17—29
DOI https://doi.org/10.2147/IDR.S440479
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Mikiyas Zike,1 Abdurahaman Mohammed Ahmed,2 Awraris Hailu,2 Bedru Hussien3
1Debre Berhan Town Health Facilities, MoH, Debre Berhan, Amhara National Regional State, Ethiopia; 2Department of Epidemiology, Debre Berhan University, Debre Berhan, Amhara National Regional State, Ethiopia; 3Department of Public Health, Madda Walabu University, Goba, Oromia National Regional State, Ethiopia
Correspondence: Bedru Hussien, Department of Public Health, Madda Walabu University, P.O. Box 302, Goba, Oromia National Regional State, Ethiopia, Tel +251911997287, Email [email protected]
Background: The majority of multidrug-resistant organisms found in immunocompromised patients are enterococci. The rise of vancomycin-resistant enterococci (VRE) poses a significant threat to public health. There is a scarcity of information regarding the prevalence of VRE in Ethiopia.
Purpose: This study aims to determine the prevalence of VRE in fecal samples from Human Immunodeficiency Virus (HIV)-positive individuals, to identify associated factors, and to assess their susceptibility to selected commonly prescribed medications.
Patients and Methods: A cross-sectional study was conducted from April 1 to July 15, 2023, on 170 HIV-positive clients at Debre Berhan Town. A pre-tested structured questionnaire was used to collect socio-demographic and clinical data. Stool sample was collected by trained health workers, and processed by standard microbiological techniques. Kirby-Bauer disk diffusion method was used for antimicrobial susceptibility testing. Data entry and analysis was carried out by SPSS Version 25. Bivariate and multivariate logistic regressions were used to assess the associated factors. Variables with a p-value of < 0.05 were considered to be significantly associated with the outcome variables and the results were displayed with tables.
Results: From the total of 170 study participants, colonization of Enterococcus species was observed among 95 (55.9%). Vancomycin resistance was found in 13 (13.8%) of them with 95% confidence interval (CI) 7.4– 22.1. History of hospitalization Adjusted Odds Ratio (AOR): 11.9 (95% CI 1.11– 127.53); habit of eating uncooked food (AOR: 15.34 (95% CI 2.36– 99.63)) and invasive procedures (AOR: 23.07 (95% CI 3.54– 150)) were among the predictors of VRE. MDR (multidrug resistance) was observed in 83 (87.4%) of the isolates. The highest rate of resistance was observed for ampicillin with 72 (74.6%).
Conclusion: Vancomycin and multidrug resistance of enterococci among HIV patients are significant in ART clinics of Debre Berhan Town. These warrant applicable infection prevention guidelines in the health facilities and health education on food hygiene.
Keywords: Enterococci, vancomycin resistant, HIV patients, Ethiopia
Introduction
Enterococci are normally present as colonizers in the intestinal tract of humans and animals, and can be recovered from feces in large quantities.1 Enterococci are ubiquitous Gram-positive cocci, catalase-negative, non-spore-forming, facultative anaerobic organisms that belong to the Lancefield group D streptococci which were originally classified as enteric Gram-positive cocci and later included in the genus Streptococcus.2
Vancomycin-resistant enterococci (VRE) are a type of bacteria that are resistant to vancomycin.3 Out of more than 30 enterococci species recorded, only Enterococcus faecalis and Enterococcus faecium strains are responsible for the majority of human infections.4 Particularly, E. faecalis, which makes up about 80% of the strains in infection, was the main enterococci species recovered from a clinical material.4,5 It is known that enterococci may thrive in a variety of harsh conditions, including those that contain 6.5% NaCl, temperatures between 5 and 5°C, and pH ranges between 4.5 and 10. They can also hydrolyze esculin in the presence of 40% bile.4
VRE are of public health importance around the globe. For example, in Europe, proportions of vancomycin-resistant E. faecium (VREFm) was 19.0% (95% CI 16.8–21.5%) in 2018 with increasing trend from year to year across all European regions.2 In India, based on 19 selected studies, the pooled prevalence of VRE was estimated at 12.4% (95% CI 8.6–17.5).6 In Africa, an overall pooled prevalence of VRE was 26.8% (95% CI 10.7–43.0%) with a one-health perspective.7 In Ethiopia, different prevalence studies among different study populations and clinical specimens reported 6.7–22.7% VRE.8
VRE are usually spread by direct contact with hands, environmental surfaces or medical equipment that have been contaminated by the feces of an infected person. The most frequent nosocomial infections brought on by these organisms are urinary tract infections (linked to the use of instruments and the administration of antibiotics), then pelvic and intra-abdominal infections.9,10 Symptoms depend on the site of infection, but include fever and pain at the site. In the case of wounds, swelling, redness, and discharge (pus) may appear as signs of infection.11 They can be serious pathogens causing endocarditis, neonatal sepsis, and occasionally meningitis.10
VRE are particularly a threat to people with compromised immunity including human immunodeficiency virus (HIV) positive patients and also due to the fact that this segment of the population tends to have frequent visits/admission to health facilities which puts them at increased risk of infection with VRE.9,12–14 Given the prevalence of HIV infection in Sub-Saharan African countries in general (9.0%) and in Ethiopia (3% in urban setting) in particular, this is still of public health importance.15,16 It is imperative to have adequate information about the prevalence of VRE and susceptibility pattern of enterococci to commonly used antibiotics among HIV-positive patients in health facility settings to take suitable public health measures.
Colonization of VRE is associated with a number of known risk factors. These include: HIV patients’ immunosuppression, hospitalization history, neutropenia, renal insufficiency, bloodstream infection, admission to an intensive care unit, extended hospital stay, advanced age, invasive surgeries, multi-morbidity, and long-term antimicrobial medication.17–21
A significant issue with enterococci is their high level of antibiotic resistance, capacity to endure severe conditions in the community, and persistence in hospital settings.9,12,22
To the best of the researchers’ knowledge there is no adequate information with regard to VRE in the study population of the study area. Therefore, the objectives of this study were to determine the prevalence of VRE among HIV-positive patients and their antibiotics susceptibility pattern, and factors associated with VRE infections among HIV-positive patients in ART clinics of Debre Berhan Town, North Shewa, Amhara, Ethiopia, in 2023.
Materials and Methods
Study Design, Area, Setting, and Period
A health facility-based cross-sectional study was used to conduct the study. The study area is Debre Berhan town in North Shewa Zone, Amhara Regional State of Ethiopia. This town is located at the center of the country and 130 km away to the north of Addis Ababa, the capital. It is 695 km away from Bahir Dar, the main city of the region. Based on the 2007 national census conducted by the Central Statistical Agency of Ethiopia (CSA) the town has a total population of 65,631 of whom 31,668 are men by gender.17 According to the data obtained from the town health administration office, the total number of antiretroviral treatment (ART) patients is 3278. These patients are distributed among Debre Berhan Comprehensive Specialized Hospital, 2101; 04 Health Center, 918; Chacha Health Center, 175; and Ayer Tena Health Center, 84 (Gov. Report 2022). The study was conducted during the period between April 1 and July 15, 2023.
Study Population
Study population is all HIV-positive clients who were attending ART clinics in the health facilities of Debre Berhan town during the time of data collection.
Sample Size and Sampling Method
The sample size was determined by using a single population proportion formula, n = z2 p (1-p)/d2. Where “n” is the minimum sample size, “z” is 1.96 for 95% confidence interval, “p” is the probability, and “d” is the margin of error. A 5% margin of error (d=0.05), and p (11.4%) from the study conducted in Arba-Minch4 were used to calculate the sample size. Thus, n= (1.96)2 * 0.114(1–0.114)/(0.05)2 = 155. When a 10% nonresponse rate is added the sample size becomes 170. Participants were proportionally selected using a systematic sampling technique from the sampling frame of each health facility. There are four health facilities with ART clinics in the town. One hundred and nine, 46, 10, and 5 patients were selected in proportion of their total number in each HF during data collection. Lists of selected (systematic) patients from the registration books were prepared for each HF. Selected patients were ethically approached and those who fulfilled the eligibility criteria were enrolled addressing ethical issues. Substitution of the next individual (from the registration book) was employed when the criteria for enrolment was not fulfilled by a patient.
Inclusion Criteria
All adult (≥ 18 years old) HIV patients and < 18 years having surrogates who were attending ART clinics and who do not have a clear gastrointestinal infection and gastrointestinal bleeding at the time of data collection were eligible to be participants of the study.
Exclusion Criteria
HIV patients who were on antimicrobial treatment during the last 2 weeks prior to data collection, having obvious gastrointestinal infection and bleeding, and HIV patients < 18 years old who do not have surrogates were not eligible for the study.
Data Collection Instrument and Process
Development and Testing of the Data Collection Instrument
A structured questionnaire was first prepared in English and then translated to Amharic language (local language). The second version of the questionnaire was retranslated into the original one by language experts to evaluate its consistency. The questionnaire was then pre-tested.
Interview
The face-to-face interview technique was applied using trained data collectors to collect data related to socio-demographic, clinical, and treatment-related variables, as well as hygiene-related factors, from each study participant.
Sample Collection Storage and Transportation
Patients were provided with wide-mouthed, clean plastic containers and instructed to bring about 5–10 g stool specimens. Immediately after collection, approximately one gram of the fecal specimen was placed on a Bile Esculin Azide Agar (BEAA) medium and stored in a refrigerator within in a temperature range of 2–8°C until transported to the laboratory for processing. The collected stool specimens from each health facility were transported to Debre Birhan Comprehensive Specialized Hospital (DBCSH) using Carry Blair Transport Medium (Oxoid Ltd, UK).12,23
Bacterial Isolation and Identification
Using BEAA stool samples were streaked and then incubated for 24 hours at 37°C. Plates were checked for the presence of distinctive colonies with a dark halo in the center. The following phenotypic tests were used to identify characteristic colonies and presumptively identify them as enterococci:24 (a) Gram stains, only plates that yield Gram-positive cocci in pairs or short chains will be studied further. (b) Catalase testwas performed on suspected colonies according to standard microbiological procedure.12,25 (c) Growth in 6.5% NaCl where similar colonies from each plate were picked and inoculated into brain heart infusion (BHI) broth (Oxoid Ltd, UK) containing 6.5% NaCl and incubated at 37°C for 24–48 hours.5 Those isolates found to be Gram positive, catalase negative, and able to grow in BHI broth containing 6.5% NaCl were identified as enterococci.
Antimicrobial Susceptibility Testing
Each isolate’s antimicrobial susceptibility was tested using the Kirby-Bauer disk diffusion method on Muller-Hinton agar (Oxoid Ltd, UK). Well-isolated pure colonies of the same morphological type were selected from the Bile Azide Agar plate and preserved on Tryptone soya broth (Sisco Research Laboratories Pvt., India). Selected bacterial colonies were taken from pure cultures and put into a tube with sterile nutrient broth (Oxoid Ltd, UK). The tube was then incubated at 37°C until the suspension’s turbidity was adjusted to a McFarland standard (Hardy diagnostics, Canada) of 0.5. Then, the suspension was spread evenly on Muller–Hinton agar. The medium was incubated at 37°C for between 18 and 24 hours after being exposed to an antibiotic concentration gradient on discs. The following antibiotic discs were used to test the antimicrobial susceptibility of enterococci: vancomycin (30 µg), ampicillin (10 µg), penicillin (10 units), doxycycline (30 µg), chloramphenicol (30 µg), erythromycin (15 µg),12 erythromycin (5 µg), tetracycline (30 µg), ciprofloxacin (5 µg) and nitrofurantoin (300 μg).26 The status of resistance of the strain was determined by measuring the zone diameter (mm) and referring to CLSI standard for each drug of interest.27,28
Quality Control Measures
Training was given to data collectors about data collection procedures and interview techniques for one day. The questionnaire was pre-tested on 5% of the sample size in the nearby hospital (Hakim Gizaw Hospital) before the actual study was started and the necessary modification was made. In relation to laboratory quality control the sterility of newly prepared culture media was checked by incubating 5% of the batch at 35–37°C overnight before its use and evaluating it for possible growth or contamination. The performance testing was done at regular intervals and whenever a new batch of strain or reagent is prepared. The standard strain of S. aureus (ATCC 25923) was used as positive control and E. faecalis (ATCC 29212)20 were used as negative control. These strains are standard strains to be used as controls for this kind of procedure. The whole procedure and result interpretation was done strictly following the standard operating procedure (SOP).
Data Processing and Analysis
Initially, data were checked for completeness and coded. After coding, data were entered using EPI-data version 3.5.1. The data were exported to SPSS version 25 for further analysis. Frequency analysis was carried out to assess the prevalence of VRE. Logistic regression analyses were done to determine factors associated with vancomycin resistance of enterococci. Variables with p-value ≤ 0.2 in bivariate logistic regression were included in multi-variate analysis. Crude and adjusted odds ratios were calculated to quantify the strength of the association. The 95% confidence interval was determined and risk factors with p-value of less than 0.05 in multivariate analyses were considered as statistically significant.
Operational Definitions
Colonization of Enterococcus species within the context of this study is defined as the presence of enterococci with growth and multiplication in the GIT of a study participant that can be isolated on culture media and identified by colony characteristics, Gram staining, or biochemical tests.27
Antimicrobial resistance: the enterococci strains are considered to be resistant to a specific antibiotic if the diameter (to the nearest mm) of measured zone of inhibition, by the disc diffusion method, is smaller as compared with the CLSI standard.27,29
Vancomycin-resistant enterococci: strains of those enterococci labeled as resistant to vancomycin according to CLSI standard.27
Multi-drug resistance: resistance of enterococci strains against three or more antimicrobial classes according to CLSI standard.27,30
Results
Socio-Demographic and Clinical Characteristics of Study Participants
The research included 170 study participants with a response rate of 100%. The age range of the study participants was 19 to 72 with a mean age of almost 44 and a standard deviation of 12.36. About 62% (105/170) of them were female. The majority, more than 70% (123/170), of the participants were urban residents; and around 45% (77/170) were married. In terms of education, about a quarter (40/170) of them were illiterate while more than one third (63/170) had attained a college diploma. By occupation, about half (81/170) of them were on different types of occupations as government employees while a few (5/170) were daily laborers. The clinical characteristics considered important in this study were previous antibiotic treatment, invasive procedures performed, previous hospitalization, opportunistic infections, and habit of eating uncooked meat. The frequencies of these characteristics among the respondents are presented in Table 1.
 |
Table 1 Socio-Demographic and Clinical Characteristics of Study Participants (n = 170) Among HIV-Positive Clients in Debre Berhan, North Shewa, Ethiopia, 2023 |
Colonization of Enterococci Among HIV-Positive Individuals
From the total of 170 study participants, colonization of Enterococcus species was observed among 56% (95/170) of the participants. Nearly half (48/95) of the colonized patients were within the age range of 35 to 54. About two thirds (58/95) of the female clients were found to have been colonized. Of all the prevalence of enterococci colonization observed more than 70% (68/95) was contributed by participants from urban residence. Government employees accounted for a little less than half (45/95) while those with diploma or degree shared about one third (36/95) of the prevalence of enterococci colonization. More than half of the study participants with a history of previous antibiotic treatment and/or previous hospitalization were found to be colonized with enterococci (Table 2).
 |
Table 2 Prevalence of Enterococci and Their Resistance Against Vancomycin Among HIV-Positive Patients by Socio-Demographic and Clinical Characteristics in Debre Berhan, North Shewa, Ethiopia, 2023 |
Prevalence of VRE Among HIV-Positive Individuals
Vancomycin resistance was found among HIV-positive clients in 13.75% (13/95) with 95% CI 7.4–22.1. Among the Enterococci colonized participants about two thirds (8/13) who had VRE were within the age range of 25 to 44. Females were colonized by VRE species in almost half (7/13) of cases. Three quarters of the VRE (10/13) were among urban residents while farmers accounted for about half (6/13) of them. Only in one case (1/13) of participants with educational level of diploma or degree was VRE found. According to the clinical history almost all of the study participants who had history of previous hospitalization were colonized by VRE. The same is true for more than three quarters of those who had undergone invasive procedures (Table 2).
Associated Factors for Colonization of VRE Among the HIV-Positive Clients
In the bivariable logistic regressions model, factors that are associated with colonization of vancomycin resistant enterococci at p-value < 0.25 were invasive procedure performed, history of hospitalization, and habit of eating uncooked food. These were fit into a multivariable logistic regression model and revealed that invasive procedure performed (AOR = 23.07 (95% CI 3.54 −150)), history of hospitalization (AOR = 11.9 (95% CI 1.11–127.53)) and habit of eating uncooked food (AOR = 15.34 (95% CI 2.36–99.63)) were significantly associated with colonization of VRE (Table 3).
 |
Table 3 Multivariate Logistic Regression Analysis on Factors Associated with Vancomycin Resistance of Enterococci Among HIV-Positive Clients in Debre Berhan, North Shewa, Ethiopia, 2023 |
Antimicrobial-Resistance Pattern
In this study susceptibility tests for all the isolated enterococci were done against nine selected antibiotics. Among 95 enterococci isolates tested for commonly prescribed antimicrobial agents the highest rate of resistance was observed against ampicillin 72 (74.6%) followed by penicillin 56 (65.9%). Vancomycin was among the antibiotics tested to which the least proportion 13 (13.7%) of the isolates were resistant (Table 4). Sensitivity to all the drugs tested was observed with only about 3% of the isolates in this study. Resistance to three or more of the drugs including vancomycin (MDR) was observed with 83 (87.4%) of them. Fifty-nine (62.1%) were resistant to four to six antibiotics (Table 5).
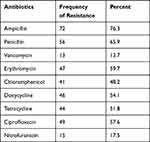 |
Table 4 Antimicrobial Resistance Pattern of Enterococci Among HIV-Positive Clients in Debre Berhan, North Shewa, Ethiopia, 2023 (n = 95) |
 |
Table 5 Multidrug Resistance Pattern of Enterococci Among HIV-Positive Clients at Debre Berhan, North Shewa, Ethiopia, 2023 |
Discussion
Enterococci have traditionally been regarded as low-grade pathogens, but have emerged as an increasingly important cause of nosocomial infections in the last decade. The prevalence of enterococci, rapid emergence of drug resistance and the increasing incidence of colonization with enterococci have become associated with major health threats globally.30 The epidemiology of enterococci is not fully understood since there are striking differences among different species of resistant isolates obtained from various geographic locations.2
The disk diffusion method used has its own advantages and disadvantages. The test simplicity, being the least costly of all susceptibility methods, the provision of categorical results easily interpreted by all clinicians, and flexibility in selection of disks for testing are among its advantages. Problem with accuracy of the test results and lack of mechanization or automation of the test are considered as constraints of the disc method. However, the disk test has been standardized for testing streptococci/enterococci and some other significant bacteria through use of specialized media, incubation conditions, and specific zone size interpretative criteria.31
The current study revealed the 55.9% rate of enterococci colonization in HIV-positive subjects which was greater than the finding from a cross-sectional study done at Hiwot Fana Specialized Hospital in Harar which was 26.2%.32 The increased colonization rate among HIV-positive clients may be attributed to the fact that HIV-positive clients are more likely to have a history of hospitalization in various health-care facilities33 which may help in colonization and drug resistance of these bacteria.
The prevalence of enterococci in the current study was lower than the report from different localities in Ethiopia such as Gondar, 88.9%;34 West Amhara area, 63.0%;12 and it was also lower than a study conducted in India, 80.6%.35 This discrepancy could be attributable to the fact that the previous study’s subjects were hospitalized adults and pediatric patients’ age.
The prevalence of VRE (13.8%) in the present study has proximity with studies done in a Malaysian tertiary hospital (10.7%).36 However, it was significantly higher than that of previous studies done in other parts of Ethiopia which reported 6.7%37,38 and was higher than that of a study conducted on ART patients in Ethiopia in different areas such as Dessie, 6.3%,39 West Amhara, 7.7%,5 and Gondar, 5.5%.40 The current finding is lower than that of studies done in different parts of the world including Nepal, 25.3%41, Brasilia, 17%,42 and Gondar, Ethiopia, 7%.40
Enterococci showed higher and variable resistance levels to different categories of tested antibiotics. The resistance against ampicillin (76.3%) was comparable with the finding from the study in Arba Minch, 79.9%;9 and Iran, 77.4%.42 But resistance to ampicillin in this study is higher than that reported from Dessie, 34.8%34 and Algeria, 30.4%.43 The resistance against chloramphenicol, 48.2% was in line with that of India, 42.3%.35 The resistance against erythromycin, 59.7%, was not far from 49.6% of ART clients in Arba Minch.9 This result of erythromycin is, however, much greater than that of Dessie, 2.4%, Ethiopia.39 On the other hand, it is lower than that of West Amhara, 94.0%12 and Gondar, 70.4%, Ethiopia.40 The ciprofloxacin resistance (57.6%) in the present study was in parallel with the results of studies in Addis Ababa, 53.3%, Ethiopia and Nepal, 61.5%.38,41 But it was higher than a report from Jimma, 36.4%37 Ethiopia and lower than that of Gondar, 70.8%, Ethiopia.40
These variations in AMR profile of Enterococci isolates to different antibiotics might indicate different enterococcal strain distribution in different geographic areas, variability in local antibiotic prescription policy and differences in antibiotic misuse practices.
Invasive procedures, history of hospitalization, and habit of eating uncooked food are found to be associated with colonization of VRE. History of hospitalization was also found to be a risk factor for VRE colonization according to studies from Arba Minch General Hospital,9 South India19 and a systematic review of several studies from different countries. This can be due to higher chance of getting infection from within the HF from already infected patients and higher probability of being exposed to antibiotics in these patients which can cause alteration of the competing microbial population and giving chance for VRE to prosper in the gastrointestinal tract and/or may induce the expression of resistant genes.44 Patients with invasive devices are also found to be at risk of being colonized by VRE.19
Limitations
The isolated enterococci were not identified to species level and no molecular characterization done due to limitation of resource. Confirmatory test method for vancomycin resistance was not done. Due to limited resources and a short study time, species identification was not investigated.
Conclusion
The prevalence of VRE among HIV patients visiting medical facilities in Debre Berhan Town was significant. Factors associated with VRE were related to health facility utilization (hospitalization and invasive procedures) and habits of consuming uncooked food that warrant applicable infection prevention guidelines in the health facilities and health education on food hygiene. The fact that a significant proportion of the isolates (87.4%) was MDR in this investigation indicates the seriousness of AMR in the studied population, demanding an appropriate response from concerned bodies. Further studies with increased sample size using genotypic methods are important.
Abbreviations
AOR, Adjusted Odd’s Ratio; AMR, Anti-microbial Resistance; AST, Antimicrobial Susceptibility Testing, CI, Confidence Interval; COR, Crude Odd’s Ratio; CLSI, Clinical Laboratory Standard Institute; HIV, Human Immunodeficiency Virus; MDR, Multidrug Resistance; VRE, Vancomycin Resistance Enterococci.
Data Sharing Statement
The corresponding author will provide the data gathered for this study upon reasonable request.
Ethics Approval and Consent to Participate
With the protocol number IRB 051/2022, Asrat Woldeyes Health Science Campus, Debre Berhan University, granted ethical clearance. A verbal informed consent form outlining the study’s goals and participants’ rights was verbally discussed with every study participant in accordance with the Declaration of Helsinki45 and this was acceptable as approved by the ethical committee of the institution. The questionnaires were securely handled after completion, and all access to the results was strictly controlled.
Acknowledgments
We acknowledge the contribution of the patients who were volunteers to become part of the study. We are also grateful to the data collectors, technical assistance of the laboratory technologists and the general support by Debre Berhan University.
Author Contributions
Mikiyas Zike is the principal investigator. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No specific grant was given to this research by any funding organization in the public, private, or non-profit sectors.
Disclosure
The authors declare no financial or other conflict of interest in this work.
References
1. Alemayehu T, Hailemariam M. Prevalence of vancomycin-resistant enterococcus in Africa in one health approach: a systematic review and meta-analysis. Sci Rep. 2020;10(1):1–10. doi:10.1038/s41598-020-77696-6
2. Ayobami O, Willrich N, Reuss A, Eckmanns T, Markwart R. The ongoing challenge of vancomycin-resistant Enterococcus faecium and Enterococcus faecalis in Europe: an epidemiological analysis of bloodstream infections. Emerging Microbes Infect. 2020;9(1):1180–1193. doi:10.1080/22221751.2020.1769500
3. Özsoy S, Ilki A. Detection of vancomycin-resistant enterococci (VRE) in stool specimens submitted for Clostridium difficile toxin testing. Braz J Microbiol. 2017;48(3):489–492. doi:10.1016/j.bjm.2016.12.012
4. Abera A, Tilahun M, Tekele SG, Belete MA, Abbassi MS. Prevalence, antimicrobial susceptibility patterns, and risk factors associated with enterococci among pediatric patients at Dessie Referral Hospital, Northeastern Ethiopia. Biomed Res Int. 2021;2021:1–9. doi:10.1155/2021/5549847
5. Weiner LM, Webb AK, Limbago B, et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2011–2014. Infect Control Hosp Epidemiol. 2016;37(11):1288–1301. doi:10.1017/ice.2016.174
6. Smout E, Palanisamy N, Valappil SP. Prevalence of vancomycin-resistant Enterococci in India between 2000 and 2022: a systematic review and meta-analysis. Antimicrob Resist Infect Control. 2023;12(1):79. doi:10.1186/s13756-023-01287-z
7. Alemayehu T, Hailemariam M. Prevalence of vancomycin-resistant enterococcus in Africa in one health approach: a systematic review and meta-analysis. Sci Rep. 2020;10(1):20542.
8. Ashagrie D, Genet C, Abera B. Vancomycin-resistant enterococci and coagulase-negative staphylococci prevalence among patients attending at Felege Hiwot Comprehensive Specialized Hospital, Bahir Dar, Ethiopia. PLoS One. 2021;16(4):e0249823. doi:10.1371/journal.pone.0249823
9. Regasa Dadi B, Solomon Z, Tesfaye M, Karunasagar I. Vancomycin resistant Enterococci and its associated factors among HIV infected patients on anti-retroviral therapy in Ethiopia. PLoS One. 2021;16(6):e0251727. doi:10.1371/journal.pone.0251727
10. Abamecha A, Wondafrash B, Abdissa A. Antimicrobial resistance profile of Enterococcus species isolated from intestinal tracts of hospitalized patients in Jimma, Ethiopia. BMC Res Notes. 2015;8(1):1–7. doi:10.1186/s13104-015-1200-2
11. Epidemiology Fact Sheets - Virginia Department of Health. Virginia Department of Health (.gov). Available from: https://www.vdh.virginia.gov›epidemiology-fact-sheets.
12. Agegne M, Abera B, Derbie A, Yismaw G, Shiferaw MB. Research Article Magnitude of Vancomycin-Resistant Enterococci (VRE) Colonization among HIV-Infected Patients Attending ART Clinic in West Amhara Government Hospitals. Int J Microbiol. 2018;2018. doi:10.1155/2018/7510157
13. Achenbach C, Flores E, Ferrell P, Pitrak D, Weber SG. Prevalence of and risk factors for colonization with vancomycin-resistant Enterococcus among human immunodeficiency virus–positive outpatients. Infect Control Hosp Epidemiol. 2006;27(1):102–104. doi:10.1086/499391
14. Vancomycin resistant Enterococci and its associated factors. National Institutes of Health (.gov). Availble from: https://pubmed.ncbi.nlm.nih.gov.
15. The Status of the HIV/AIDS Epidemic in Sub-Saharan Africa. Availble from: https://www.prb.org›resources›the-status-of-The-hiv-ai.
16. HIV/AIDS | Ethiopia | U.S. Agency for International Development. United States Agency for International Development (.gov). Availble from: https://www.usaid.gov›ethiopia›hivaids.
17. Zacharioudakis IM, Zervou FN, Ziakas PD, Rice LB, Mylonakis E. Vancomycin-resistant enterococci colonization among dialysis patients: a meta-analysis of prevalence, risk factors, and significance. Am J Kidney Dis. 2015;65(1):88–97. doi:10.1053/j.ajkd.2014.05.016
18. Zaas AK, Song X, Tucker P, Perl TM. Risk factors for development of vancomycin-resistant enterococcal bloodstream infection in patients with cancer who are colonized with vancomycin-resistant enterococci. Clinl Infect Dis. 2002;35(10):1139–1146. doi:10.1086/342904
19. Amberpet R, Sistla S, Parija SC, Thabah MM. Screening for intestinal colonization with vancomycin resistant enterococci and associated risk factors among patients admitted to an adult intensive care unit of a large teaching hospital. J clin diagn res. 2016;10(9):DC06. doi:10.7860/JCDR/2016/20562.8418
20. Yameen MA, Iram S, Mannan A, Khan SA, Akhtar N. Nasal and perirectal colonization of vancomycin sensitive and resistant enterococci in patients of paediatrics ICU (PICU) of tertiary health care facilities. BMC Infect Dis. 2013;13(1):1–10. doi:10.1186/1471-2334-13-156
21. Byun S-J, Kang J. Risk factors and clinical outcomes for vancomycin-resistant enterococcus colonization on intensive care unit admission. J Korean Acad Nurs. 2013;43(2):287–295. doi:10.4040/jkan.2013.43.2.287
22. Batistão D, Gontijo-Filho PP, Conceição N, Oliveira A, Ribas RM. Risk factors for vancomycin-resistant enterococci colonisation in critically ill patients. Memórias Inst Oswaldo Cruz. 2012;107(1):57–63. doi:10.1590/S0074-02762012000100008
23. Linfield RY, Campeau S, Injean P, et al. Practical methods for effective vancomycin-resistant enterococci (VRE) surveillance: experience in a liver transplant surgical intensive care unit. Infect Control Hosp Epidemiol. 2018;39(10):1178–1182. doi:10.1017/ice.2018.178
24. Raza T, Ullah SR, Mehmood K, Andleeb S. Vancomycin resistant Enterococci: a brief review. J Pak Med Assoc. 2018;68(5):768–772.
25. Cassone M, Zhu Z, Mantey J, et al. Interplay between patient colonization and environmental contamination with vancomycin-resistant Enterococci and their association with patient health outcomes in postacute care. In: Open Forum Infectious Diseases. Oxford University Press US; 2020.
26. Monica C. District Laboratory Practice in Tropical Countries. Cambridge University Press; 2006.
27. Wayne P. Clinical and Laboratory Standards Institute: Performance Standards for Antimicrobial Susceptibility Testing: Informational Supplement, M100. Clinical and Laboratory Standards Institute (CLSI); 2018.
28. Sahoo R, Jadhav S, Nema V. Journey of technological advancements in the detection of antimicrobial resistance. J Formos Med Assoc. 2023. doi:10.1016/j.jfma.2023.08.008
29. Punjabi K, Mehta S, Chavan R, Chitalia V, Deogharkar D, Deshpande S. Efficiency of biosynthesized silver and zinc nanoparticles against multi-drug resistant pathogens. Front Microbiol. 2018;9:2207. doi:10.3389/fmicb.2018.02207
30. Chiang H-Y, Perencevich EN, Nair R, et al. Incidence and outcomes associated with infections caused by vancomycin-resistant enterococci in the United States: systematic literature review and meta-analysis. Infect Control Hosp Epidemiol. 2017;38(2):203–215. doi:10.1017/ice.2016.254
31. Wayne PA Clinical and Laboratory Standards Institute Performance standards for antimicrobial disk susceptibility tests. Approved standard M2-A10; 2009.
32. Dawud A. Magnitude of Vancomycin Resistant Enterococci Colonization and Associated Factor Among HIV Infected Patients at Hiwot Fana Specialized University Hospital. Harar, eastern Ethiopia: Haramaya University; 2021.
33. Anderson AC, Jonas D, Huber I, et al. Enterococcus faecalis from food, clinical specimens, and oral sites: prevalence of virulence factors in association with biofilm formation. Front Microbiol. 2016;6:1534. doi:10.3389/fmicb.2015.01534
34. Abebe W, Endris M, Tiruneh M, Moges F. Prevalence of vancomycin resistant Enterococci and associated risk factors among clients with and without HIV in Northwest Ethiopia: a cross-sectional study. BMC Public Health. 2014;14(1):1–8. doi:10.1186/1471-2458-14-185
35. Deshpande VR, Karmarkar MG, Mehta PR. Prevalence of multidrug-resistant enterococci in a tertiary care hospital in Mumbai, India. J Infect Developing Countries. 2013;7(02):155–158. doi:10.3855/jidc.3018
36. Nor NSM, Abu NA, Rashid MA, Ismail M, Razak R. Bacterial pathogens and antibiotic resistance patterns in children with urinary tract infection in a Malaysian tertiary hospital. Med J Malays. 2015;70(3):153–157.
37. Toru M, Beyene G, Kassa T, Gizachew Z, Howe R, Yeshitila B. Prevalence and phenotypic characterization of Enterococcus species isolated from clinical samples of pediatric patients in Jimma University Specialized Hospital, south west Ethiopia. BMC Res Notes. 2018;11(1):1–6. doi:10.1186/s13104-018-3382-x
38. Ferede ZT, Tullu KD, Derese SG, Yeshanew AG. Prevalence and antimicrobial susceptibility pattern of Enterococcus species isolated from different clinical samples at Black Lion Specialized Teaching Hospital, Addis Ababa, Ethiopia. BMC Res Notes. 2018;11(1):1–6. doi:10.1186/s13104-018-3898-0
39. Ali S, Alemayehu M, Dagnew M, Gebrecherkos T. Research article vancomycin-resistant enterococci and its associated risk factors among HIV-positive and-negative clients attending Dessie Referral Hospital, Northeast Ethiopia. Int J Microbiol. 2018. doi:10.1155/2018/4753460
40. Yilema A, Moges F, Tadele S, et al. Isolation of enterococci, their antimicrobial susceptibility patterns and associated factors among patients attending at the University of Gondar Teaching Hospital. BMC Infect Dis. 2017;17(1):1–8. doi:10.1186/s12879-017-2363-3
41. Karna A, Baral R, Khanal B. Characterization of clinical isolates of Enterococci with special reference to glycopeptide susceptibility at a Tertiary Care Center of Eastern Nepal. Int J Microbiol. 2019;2019:1–8. doi:10.1155/2019/7936156
42. Shaghaghian S, Pourabbas B, Alborzi A, Askarian M, Mardaneh J. Vancomycin-Resistant Entrococci colonization in chronic hemodialysis patients and its risk factors in southern Iran (2005–2006). Iran Red Crescent Med J. 2012;14(10):686.
43. Djahmi N, Boutet-Dubois A, Nedjai S, Dekhil M, Sotto A, Lavigne J-P. Molecular epidemiology of Enterococcus sp. isolated in a university hospital in Algeria. Scand J Infect Dis. 2012;44(9):656–662. doi:10.3109/00365548.2012.673232
44. Papadimitriou-Olivgeris M, Drougka E, Fligou F, et al. Risk factors for enterococcal infection and colonization by vancomycin-resistant enterococci in critically ill patients. Infection. 2014;42(6):1013–1022. doi:10.1007/s15010-014-0678-1
45. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. PMID: 24141714. doi:10.1001/jama.2013.28105
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
