Back to Journals » Neuropsychiatric Disease and Treatment » Volume 11
Value of F-wave studies on the electrodiagnosis of carpal tunnel syndrome
Authors Alemdar
Received 17 March 2013
Accepted for publication 2 July 2015
Published 31 August 2015 Volume 2015:11 Pages 2279—2286
DOI https://doi.org/10.2147/NDT.S45331
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Murat Alemdar
Sakarya University Education and Research Hospital, Sakarya, Turkey
Background: F waves are late electrophysiological responses to antidromic activation of motor neurons and are used to evaluate the conduction along the whole length of peripheral nerves. We aimed to determine the diagnostic efficacies of minimum median nerve F-wave latency (FWL) and median-to-ulnar nerve F-wave latency difference (FWLD) on carpal tunnel syndrome (CTS).
Materials and methods: The electrophysiological studies consisted of sensory and motor nerve conduction and F-wave studies of the median and ulnar nerves. The best cut-off points of minimum median nerve FWL and FWLD for the diagnosis of CTS were detected for the whole study group and for different height subgroups (Group 1: 150–159 cm, Group 2: 160–169 cm, and Group 3: over 170 cm). The diagnostic efficacies of minimum median nerve FWL and FWLD were calculated for the whole CTS group and for the mild CTS group, separately.
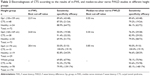
Results: The best cut-off point of minimum median nerve FWL on the diagnosis of CTS was determined as 24.60 ms for the whole group. It was 23.90 ms for Group 1, 24.80 ms for Group 2, and 28.40 ms for Group 3. The usage of these stratified cut-off points yielded a higher total diagnostic efficacy rate than single cut-off point usage (79.9% vs 69%, respectively; P=0.02). The best cut-off point of FWLD on the diagnosis of CTS was 0.80 ms for the whole group. It was 0.55 ms for Group 1, 0.30 ms for Group 2, and 0.85 ms for Group 3. Both the single cut-off point usage and the stratified chart usage for FWLD had equal diagnostic efficacy (85.1%). In the mild CTS group, diagnostic efficacy was 55.5% for minimum median nerve FWL and 78.8% for FWLD (P=0.0001).
Conclusion: Median-to-ulnar nerve FWLD yields a higher diagnostic efficacy than minimum median nerve FWL on the diagnosis of CTS. However, the sensitivities of both parameters are not satisfactory for the extremities with mild CTS, which compose the main group having diagnostic challenge.
Keywords: carpal tunnel syndrome, median nerve, F-wave
Introduction
Carpal tunnel syndrome (CTS) is the most common entrapment neuropathy caused by focal compression of the median nerve in the carpal tunnel. The prevalence of symptomatic and electrophysiologically confirmed CTS is approximately 3% among women and 2% among men.1 The diagnosis of CTS is mainly based on typical symptoms in disease history and signs in physical examination.2 However, electrodiagnostic studies are necessary to choice the treatment options and follow-up the disease progress.3–6 Electrodiagnosis is also helpful when the classic defining features of CTS are obscure.7 Transcarpal sensory or transcarpal sensory and motor conduction abnormalities of median nerve in the presence of normal ipsilateral ulnar nerve conduction are the main indicators of CTS on nerve conduction studies (NCSs).
In electrophysiologic practice, numerous conduction parameters are used during CTS search. The traditionally used ones deal with transcarpal sensory and motor conduction measures of median nerve. Elongation of median nerve wrist-to-abductor pollicis brevis (APB) muscle distal motor latency (DML) and decrease of compound muscle action potential amplitude over APB,8–10 elongation of wrist-to-digit or wrist-to-palm median nerve distal sensory latency,8–11 and slowing of sensory conduction velocity (SCV) of median nerve12,13 are helpful in the electrodiagnosis of CTS. However, the previous studies showed a wide range of sensitivity and specificity for them.8–15
The median-to-ulnar nerve comparative tests were also reported as useful tools for CTS diagnosis in previous electrophysiological researches. Median-to-ulnar nerve distal sensory latency difference (DSLD) from digit IV,15,16 DSLD between median nerve-to-digit II and ulnar nerve-to-digit V,16 SCV of the median nerve in comparison with the ulnar nerve over digit IV,17 and median-to-ulnar nerve DML difference16,18 are the main kinds of these comparative techniques. Italian CTS Study Group reported that the sensitivity of standard NCS tests (digit-to-wrist median nerve SCV and wrist-to-APB median nerve DML) was 83.5%, and addition of a comparative or segmental test enhanced the overall sensitivity of the NCSs up to 94.9%.12 In their extensive review, Jablecki et al8 reported pooled sensitivity of 65% and specificity of 98% for median nerve sensory conduction measures between wrist and digit, and sensitivity of 85% and specificity of 97% for comparison of median and ulnar nerve sensory conduction over wrist-to-digit IV segment. Schuhfried et al17 reported a high accuracy in the electrodiagnosis of CTS by determining the relative slowing of the antidromic median nerve SCV compared with ulnar nerve SCV over wrist-to-digit IV segment. They reported that the sensitivity was 83% and the specificity was 93% at a cut-off value of 10 m/s. After all, addition of a comparative or a segmental technique to the electrodiagnostic protocol could disclose median nerve conduction abnormalities in “standard negative” cases and enhance diagnostic efficiency of NCSs in CTS.
F waves are late electrophysiological responses to antidromic activation of motor neurons. Their classical application is related to the evaluation of conduction along the whole trunk of a peripheral nerve. Median nerve is an extension of the medial cord of the brachial plexus. The larger of the two terminal branches of medial cord of brachial plexus continue as ulnar nerve, while the smaller terminal branch forms the medial root of median nerve. Median nerve innervates APB muscle by its motor fibers originated from C8 and T1 roots. Ulnar nerve innervates abductor digiti minimi (ADM) muscle by its motor fibers, which again originated from same spinal roots. Therefore, generation of F waves of these two nerves over the mentioned muscles shares a common pathway at the level of brachial plexus and medulla spinalis. Any pathologic condition involving C8 and/or T1 roots or medial cord of brachial plexus is expected to prolong F-wave latencies (FWLs) of both nerves, whereas CTS is expected to prolong FWLs of median nerve, solely. Therefore, we decided to conduct a study searching the utility of comparing the minimum nerve minimum F-wave latency (m-FWL) recorded over APB with the ulnar nerve minimum F-wave latency (u-FWL) recorded over ADM for the electrodiagnosis of CTS. Herein, we present the results of our study searching the diagnostic efficacies of m-FWL and median-to-ulnar nerve FWL difference (FWLD) in CTS.
Methods
Population
The population of the study was composed of the patients who were referred to the Electroneuromyography (ENMG) Laboratory of Yenikent State Hospital (Sakarya, Turkey) for the NCS with suspicion of CTS within a year. This retrospective study was exempt from full review by the Yenikent State Hospital, Sakarya, Turkey, because it used only retrospective and de-identified patient data of the examiner. All subjects were examined by the author, and their data were also collected. The demographical data, symptoms, and signs of all the patients were recorded on the ENMG report. CTS was diagnosed clinically if at least three of the following six characteristic symptoms and signs were present: sensory abnormalities in the hand area of median nerve innervations, pain and/or parestesia exacerbating with recurrent flexion or extension, night pain, Tinel sign, Phalen sign, and abductor paresis in thumb. The exclusion criteria were (1) history of carpal tunnel release operation in studied extremity; (2) signs of plexopathy, cervical radiculopathy, or polyneuropathy; and (3) any abnormality in the ulnar NCS.
Electrophysiological studies
NCSs consisted of sensory nerve conduction, motor nerve conduction, and F-wave studies of the median and ulnar nerves. The nature of the procedure was explained to the subjects. They sat on a padded table with the upper limb supported. All the studies were performed in a warm room with the temperature maintained at 26°C–28°C. If necessary, the limb was warmed to maintain the temperature of 30°C with an infrared lamp.
Conduction studies were performed using standard techniques of supramaximal percutaneous stimulation with a constant current stimulator and surface electrode. The motor conduction of median nerve was examined by stimulating it on wrist and antecubital fossa. The nerve was stimulated with bipolar surface electrodes and the recording was carried out over the belly of APB muscle with surface electrodes. Median nerve sensory conduction studies were performed by stimulating on the wrist and recording the responses from digit II and digit IV, antidromically. Motor conduction studies of the ulnar nerve were performed by stimulating it on wrist and ulnar groove in elbow by bipolar surface electrodes. The motor responses were recorded over ADM muscle with surface electrodes. Ulnar nerve sensory conduction studies were performed by stimulating on the wrist and recording the responses from digit IV and digit V, antidromically. In order to study median and ulnar nerve F-wave responses, the nerves were stimulated on their stimulation points over the wrist with bipolar surface electrodes and the recordings were done over the belly of APB and ADM muscles with surface electrodes, respectively. The shortest FWL was measured after 16 repetitive stimulations and elicitation of at least six F-wave responses at least. In another term, the F-wave firing rate over 1/3 was warranted for the minimum FWL recording.
Motor latency was calculated from the start of the electrical artifact to the start of the first curve of the compound muscle action potential. Sensory onset latency was calculated from the start of the electrical artifact to the start of the sensory nerve action potential, and sensory peak latency was from the start of the electrical artifact to the peak of the sensory nerve action potential. The motor conduction velocity (MCV) was calculated dividing the distance by the difference of proximal and distal onset latencies. Normative values used for median and ulnar nerve traditional conduction parameters used in our laboratory were as follows: median nerve wrist-to-APB muscle motor latency <4.20 ms, ulnar nerve wrist-to-ADM muscle motor latency <3.30 ms, antidromic median nerve wrist-to-digit II (over 14 cm) sensory peak latency <3.50 ms, antidromic ulnar nerve wrist-to-digit V (over 12 cm) sensory peak latency <3.00 ms, antidromic median-to-ulnar nerve distal sensory peak latency difference from the digit IV <0.5 ms, median and ulnar nerve forearm MCV ≥50 m/s.
The electrophysiological severity was defined in the comment section of the ENMG report for the extremities with CTS. Mild CTS stage represents the cases with delayed median nerve sensory responses and normal motor responses. In moderate CTS, both median nerve sensory and motor responses are delayed. Severe CTS means delayed median nerve motor responses with unelicitable sensory responses. In extreme CTS, both median nerve sensory and median nerve motor responses are unelicitable.
Statistical analyses
All the data were analyzed using the SOFA (Statistics Open For All package) program (released with open source AGPL3 license © 2009-14; Paton-Simpson & Associates Ltd, Auckland, New Zealand). A P-value <0.05 was considered statistically significant. After tests for normality, statistical significance between the means was calculated using an independent-sample t-test for normally distributed data and the Mann–Whitney U-test for data not normally distributed.
The results of the conduction tests were documented using the 0.05-ms intervals for each variable. The point that indicates the least number of misdiagnosed cases (minimum value of sum of the false-negative and false-positive extremities) was determined as the best cut-off point. The sensitivity and specificity values in diagnosing CTS were calculated for these best cut-off points of m-FWL and median-to-ulnar nerve FWLD. The relationship between the height of the subjects and m-FWL, u-FWL, and median-to-ulnar nerve FWLD were analyzed with Pearson linear correlation test. Then, the study population was divided into three subgroups according to the heights of patients (Group 1: 150–159 cm, Group 2: 160–169 cm, and Group 3: over 170 cm). The best cut-off points were detected again in these defined subgroups. The sensitivity and specificity values were calculated for the detected best cut-off points in these height subgroups. Tukey multiple comparisons test was done for analyzing the data of different height subgroups, which were not normally distributed. The significance of the differences on diagnostic efficiency rates between the tested variables in CTS diagnosis was analyzed with the difference between two independent proportions test.
Results
Totally, 210 upper extremity recordings of 114 individuals were considered for inclusion. Twenty-five extremities of 24 patients with the ulnar nerve entrapment neuropathy at elbow (one with bilateral entrapment), four extremities of two patients with concomitant polyneuropathy, two extremities of two patients with Guyon canal entrapment neuropathy, one extremity of one patient with total ulnar nerve dissection, one extremity of one patient with unelicitable median nerve F-wave (extreme CTS), and three extremities of three patients with insufficient data were excluded. Therefore, 174 recordings belonging to 104 patients were included. There were 86 females and 18 males. The mean age was 44.8±11.8 years (range was 16–80 years, median age was 47 years). The difference between mean ages of the females and males was not statistically significant (44.2±11.5 years vs 47.7±13.4 years, respectively) (P=0.260). The majority of the study group is composed of housewives. Students, workers, and secretaries are the other common occupation groups.
CTS was clinically diagnosed in 96 (55.2%) extremities. There was no statistically significant difference in frequencies of CTS between females and males or between right extremities and left extremities (P>0.05 for both comparisons). The mean age of the extremities with CTS was older than the extremities without CTS (46.6±11.2 years vs 42.4±11.1 years, respectively) (P=0.015). Two extremities of a patient had typical signs and symptoms of CTS, although whole NCS parameters (including the ring finger comparison) were recorded within normal limits. Thirty-nine extremities had mild CTS, 48 extremities had moderate CTS, and seven extremities had severe CTS when American Association of Electrodiagnostic Medicine grading scheme for the severity of CTS was applied to the extremities with CTS that were diagnosed clinically and electrophysiologically.
The extremities with CTS had a greater mean m-FWL than healthy extremities (26.3±2.5 ms vs 24.2±1.7 ms, respectively) (P≤0.001). The mean u-FWL was slightly shorter on the extremities with CTS than healthy extremities (23.9±1.3 ms vs 24.6±2.1 ms, respectively) (P=0.006). The mean height of the individuals with healthy extremities was higher than one of the individuals with CTS in our study group (164.1±9.0 cm vs 160.0±6.6 cm, respectively) (P≤0.001). Therefore, the relative greatness of mean u-FWL value of healthy extremities in comparison with one of the extremities with CTS was most probably due to the high proportion of the healthy extremities on higher individuals.
The best cut-off point was determined as 24.60 ms for m-FWL in the diagnosis of CTS. If FWL values over 24.60 ms were accepted as prolonged, it would have the sensitivity of 72.9% (70/96) and the specificity of 64.1% (50/78) in CTS diagnosis. The diagnostic efficiency rate was 69.0% (120/174). The sensitivity of m-FWL was 39.0% (16/41) in mild CTS patients, and the diagnostic efficacy was 55.5% (66/119).
The means of median-to-ulnar nerve FWLD values were also significantly different between the extremities with CTS and ones without CTS. The mean median-to-ulnar nerve FWLD was 2.4±2.2 ms in the extremities with CTS and -0.37±0.92 ms in healthy extremities (P≤0.001). Best cut-off point for median-to-ulnar nerve FWLD was determined as 0.80 ms in the diagnosis of CTS for the whole study group. If FWLD values over 0.80 ms were accepted as prolonged and would have a sensitivity of 77.1% (74/96) and a specificity of 94.9% (74/78) in the diagnosis of CTS. The diagnostic efficiency rate was 85.1% (148/174). Therefore, the diagnostic efficacy of median-to-ulnar nerve FWLD was higher than that of m-FWL on CTS (z=3.567, P=0.0004). The sensitivity was 46.3% (19/41) in cases of mild CTS, and the diagnostic efficacy was 78.8% (93/119). Therefore, the diagnostic efficacy of median-to-ulnar nerve FWLD was also higher than m-FWL in mild CTS patients (z=-3.717, P=0.0001).
On healthy extremities, m-FWL and u-FWL were detected as having positive correlation with heights of the subjects, whereas median-to-ulnar nerve FWLD values had a negative correlation (P<0.001 for all variables; Pearson linear correlation test) (Figure 1). The negative correlation of median-to-ulnar nerve FWLD was due to more prominent elongation of u-FWL with increasing height than m-FWL. Then, we calculated the means of m-FWL, u-FWL, and median-to-ulnar nerve FWLD values of healthy extremities in height subgroups and saw a stratified distribution supporting these findings (Table 1). We determined the best cut-off points of m-FWL and median-to-ulnar nerve FWLD values for the electrodiagnosis of CTS in the different height subgroups (Table 2). When this stratified best cut-off point chart was used, the sensitivity and specificity of m-FWL in the diagnosis of CTS were detected as 69.8% (67/96) and 92.3% (72/78), respectively. The diagnostic efficiency rate of m-FWL was significantly improved from 69.0% to 79.9% compared with single cut-off point usage (z=-2.335, P=0.020). When the stratified chart was also applied for median-to-ulnar nerve FWLD, the sensitivity and specificity were 78.1% (75/96) and 93.6% (73/78) in the diagnosis of CTS, respectively. The diagnostic efficiency rate was 85.1% (148/174). Therefore, the diagnostic efficiency rates were the same for FWLD in the usage of single cut-off point and the usage of stratified cut-off point chart (85.1% vs 85.1%, respectively) (z=0.000, P=1.000).
Discussion
Transcarpal motor and sensory conduction studies of median nerve are used to establish the presence of distal focal compressive median neuropathy in patients with CTS. In electrophysiologic practice, the results of these conduction studies are compared with the commonly used limits determined from published charts or the limits of the laboratory itself. The severity of the CTS could also be staged electrophysiologically by the use of NCSs.3,14 Prolonged distal latencies of transcarpal sensory responses or sensory plus motor responses of median nerve are enough to diagnose the CTS in case of completely normal ipsilateral ulnar nerve conduction. The conduction techniques based on median-to-ulnar nerve sensory conduction comparison, in particular median-to-ulnar nerve DSLD over digit IV, were shown to be highly useful for the electrodiagnosis of CTS in early stages. Because of its high efficacy, median-to-ulnar nerve DSLD over digit IV is a routine procedure in our ENMG laboratory during the CTS search as in many centers. The possible usage of median-to-ulnar nerve motor conduction comparison techniques on the electrodiagnosis of CTS was also tested in some previous researches. Aygül et al16 reported that median nerve (APB)-to-ulnar (ADM) nerve DML difference over 1 ms had a sensitivity of 66% on electrodiagnosis of CTS. In another study, Chang et al18 reported that DML difference had a sensitivity of 70% in the diagnosis of CTS. However, its sensitivity on different grades of the CTS was not reported in both the papers.
Elongation of minimum FWL value is one of the best indicators of a conduction delay along a peripheral nerve and could be caused by any focal injury to the distal or proximal segment of the nerve trunk (eg, compressive neuropathies, traumatic nerve injuries, plexopathy) by any pathology affecting the whole length of the motor nerve fibers from the anterior horn of the spinal cord to the muscle (eg, polyneuropathy, toxic neuropathy) or by the disorders damaging the anterior horn (eg, motor neuron disease, radiculopathy). As the demyelinating injuries to the motor fibers of peripheral nerves could be well evaluated with minimum FWL measurement, it is becoming a nearly standard procedure of NCSs in many ENMG laboratories. However, there is little information about the usage of the F-wave studies in entrapment neuropathies.
In a previous study, we defined a high efficacy of comparing the FWLs of ipsilateral median and ulnar nerves on electrodiagnosis of ulnar neuropathy at elbow.19 We detected the diagnostic efficacy of 94.1% in this previous research including NCSs of 34 arms of 17 patients with unilateral left-sided ulnar neuropathy at elbow. In their study on 79 hands with CTS belonging to 50 patients, Sander et al20 described the usefulness of FWLDs in the diagnosis of CTS and reported that median-to-ulnar nerve FWLD had a diagnostic sensitivity of 78%. The authors suggested that this technique might be advantageous when a concomitant polyneuropathy is present, and they may also help avoid technical pitfalls and aid in identification of anatomic variants. Besides, Ozge et al21 revealed the value of F-wave parameters in increasing the diagnostic yield and differentiation of CTS subtypes (which were prominent demyelinating, prominent axonal, slight demyelinating types). In 2012, Cevik et al22 searched the diagnostic significance of the F-wave inversion (the term is used to define that the m-FWL exceeds a normal ipsilateral u-FWL by 1 ms) in 60 CTS patients who had a median nerve SCV over 50 m/s, and reported that it had the sensitivity of 53.3% and specificity of 93.3% on the diagnosis of early-stage CTS. In the study by Komurcu et al23 the value of F-wave inversion in diagnosing CTS was investigated. They reported the sensitivity of F-wave inversion as 56% and the specificity as 83.8% on the electrodiagnosis of CTS. In a recent study, Mondelli and Aretini24 reported that the overall sensitivity of F-wave inversion in the diagnosis of CTS was 50.8%, and it dropped to 8% in the early stages. As in our study, they also revealed that F-wave parameters did not add further useful information specifically related to electrodiagnosis of CTS.
In a retrospective study by Park et al25 which analyzed the relationship between clinical severity of CTS and various NCS parameters on 212 hands of 106 CTS patients, the cut-off value of FWLD was determined as 0.3 ms between asymptomatic and mild CTS groups, 2.3 ms between mild and moderate CTS groups, and 4.2 ms between the moderate and severe CTS groups. They concluded that electrophysiological parameters could be a good indicator to determine the clinical severity of CTS. As the elongation of F responses is related to the damage in motor fibers of peripheral nerves, the presence of abnormal m-FWL and median-to-ulnar nerve FWLD values in approximately half of the extremities with mild CTS in our study group raises the question whether the electrophysiologic grading system based on traditional NCS parameters (DML, MCV, and compound muscle action potential amplitude) is sensitive enough to detect the cases with motor fiber involvement? Further studies searching more reliable measures to detect the motor fiber involvement of median nerve in CTS patients with different clinical grades are needed to answer this question. Median-to-ulnar nerve FWLD values could also be further searched for usage in confirmation of motor fiber involvement and, therefore, in grading the CTS.
To the best of our knowledge, our study is the first one researching the value of m-FWL and median-to-ulnar nerve FWLD in different height subgroups for diagnosing the extremities with CTS. As it is not a time-consuming procedure, median-to-ulnar nerve FWLD could be easily evaluated during an NCS including F-wave recordings. The purpose of our study was to determine the efficacies of m-FWL and median-to-ulnar nerve FWLD in electrodiagnostic confirmation of CTS. We found that FWLD has a higher diagnostic efficacy than m-FWL on the electrodiagnosis of CTS. We also observed that, on healthy extremities, m-FWL and median-to-ulnar nerve FWLD values are affected from the height of the studied subjects. Therefore, we re-determined the best cut-off points of m-FWL and FWLD for the electrodiagnosis of CTS in different height intervals. m-FWL has a higher sensitivity and specificity in the diagnosis of CTS if the obtained result is compared with the cut-off point determined for the corresponding height interval of the subject. However, the usage of stratified cut-off point chart for median-to-ulnar nerve FWLD did not yield an extra improvement in the diagnostic efficiency rate in our study. Besides, we also analyzed the sensitivity and specificity of the researched tests for the extremities with mild CTS that compose the group having major diagnostic difficulties in electrophysiologic practice. Because the sensory fibers compose the outer layers of the median nerve in its topographical anatomy, the abnormalities in parameters testing median motor nerve fibers conduction are expected to occur in later stages of the nerve compression in carpal tunnel than the ones in sensory responses. In concordance with this assumption, we found that the sensitivities of m-FWL and median-to-ulnar nerve FWLD, which were also based on motor nerve fibers conduction, were not satisfactory in mild CTS cases.
A major limitation of our study was the lack of a third group, which represents one of the main pathology (polyneuropathy, radiculopathy, brachial plexopathy, thoracic outlet syndrome, etc) or group of symptomatic controls which should be considered in differential diagnosis of CTS. Besides, the number of individuals over 170 cm of height is not satisfactory to reach a more precise result.
m-FWL has a higher sensitivity and specificity when the obtained results were compared with the corresponding cut-off point value determined for the height interval of the studied subjects. However, it is difficult to comment on the elongation of m-FWLs in sole when trying to diagnose a distal focal compressive neuropathy like CTS. Practical use of F-wave studies in daily electrodiagnosis of CTS is very helpful to detect the pathological processes, which involve the peripheral nerves in their whole elongation. However, the localizing value of F-wave studies is limited on conduction delay through a focal segment like in CTS, which is an entrapment neuropathy at the wrist characterized by distal conduction delay of the median nerve. m-FWL calculates the overall motor conduction along the trunk of the nerve, the plexus, and the ventral roots, and any damage to these structures may be responsible for a delay of F-wave. Therefore, if we want to give importance to the elongated m-FWL on electrodiagnosis of CTS, we must also demonstrate that all the segments of median nerve proximal to the wrist are intact. In concordance, our study revealed that even if the stratified cut-off point chart was used, m-FWL had a lower diagnostic efficacy than many conduction parameters used on the electrodiagnosis of CTS, in particular for the extremities with mild CTS that compose the main group having diagnostic challenge during electrophysiological studies.
Median-to-ulnar nerve FWLD, another searched parameter in our study that is based on comparison of FWL of median nerve with ipsilateral ulnar nerve, yields a higher diagnostic efficacy than m-FWL. As an advantage, handling of a stratified best cut-off point chart is not necessary for using the FWLD as an electrodiagnostic parameter for CTS. However, its sensitivity was also low in mild CTS missing the diagnosis on more than half of the extremities with mild CTS.
In conclusion, although m-FWL and FWLD have an acceptable diagnostic efficacy values in general, we do not offer the usage of these parameters routinely for searching the CTS as their sensitivities are not satisfactory in the extremities with mild CTS. Rather, they could be useful in the electrodiagnosis of CTS when a concomitant polyneuropathy was present or if any technical pitfall occurred during sensory conduction recordings. However, future prospective studies are warranted to test this hypothesis.
Disclosure
The author reported no conflicts of interest or any financial support for this study.
References
Atroshi I, Gummesson C, Johnson R, Ornstein E, Ranstam J, Rosen I. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282:153–158. | ||
Graham B. The value added by electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2008;90(12):2587–2593. | ||
Aulisa L, Tamburrelli F, Padua R, Romanini E, Lo Monaco M, Padua L. Carpal tunnel syndrome: indication for surgical treatment based on electrophysiologic study. J Hand Surg [Am]. 1998;23:687–691. | ||
Aygül R, Ulvi H, Karatay S, Deniz O, Varoglu AO. Determination of sensitive electrophysiologic parameters at follow-up of different steroid treatments of carpal tunnel syndrome. J Clin Neurophysiol. 2005;22(3):222–230. | ||
Karsidag S, Sahin S, Hacikerim Karsidag S, Ayalp S. Long term and frequent electrophysiological observation in carpal tunnel syndrome. Eura Medicophys. 2007;43(3):327–332. | ||
Premoselli S, Sioli P, Grossi A, Cerri C. Neutral wrist splinting in carpal tunnel syndrome: a 3-and 6-months clinical and neurophysiologic follow-up evaluation of night-only splint therapy. Eura Medicophys. 2006;42(2):121–126. | ||
Wilder-Smith EP, Seet RC, Lim EC. Diagnosing carpal tunnel syndrome: clinical criteria and ancillary tests. Nat Clin Pract Neurol. 2006;2(7):366–374. | ||
Jablecki CK, Andary MT, Floeter MK, et al; American Association of Electrodiagnostic Medicine; American Academy of Neurology; American Academy of Physical Medicine and Rehabilitation. Practice parameter: electrodiagnostic studies in carpal tunnel syndrome. Neurology. 2002;58(11):1589–1592. | ||
Uzar E, Tamam Y, Acar A, et al. Sensitivity and specificity of terminal latency index and residual latency in the diagnosis of carpal tunnel syndrome. Eur Rev Med Pharmacol Sci. 2011;15(9):1078–1084. | ||
Chang MH, Liu LH, Lee YC, Wei SJ, Chiang HL, Hsieh PF. Comparison of sensitivity of transcarpal median motor conduction velocity and conventional conduction techniques in electrodiagnosis of carpal tunnel syndrome. Clin Neurophysiol. 2006;117(5):984–991. | ||
Atroshi I, Gummesson C, Johnsson R, Ornstein E. Diagnostic properties of nerve conduction tests in population-based carpal tunnel syndrome. BMC Musculoskelet Disord. 2003;4:9. | ||
Padua L, Giannini F, Girlanda P, et al. Usefulness of segmental and comparative tests in the electrodiagnosis of carpal tunnel syndrome: the Italian multicenter study. Italian CTS Study Group. Ital J Neurol Sci. 1999;20(5):315–320. | ||
Demirci S, Sonel B. Comparison of sensory conduction techniques in the diagnosis of mild idiopathic carpal tunnel syndrome: which finger, which test? Rheumatol Int. 2004;24(4):217–220. | ||
Stevens JC. AAEM minimonograph #26: the electrodiagnosis of carpal tunnel syndrome. Muscle Nerve. 1997;20(12):1477–1486. | ||
Seror P. Sensitivity of the various tests for the diagnosis of carpal tunnel syndrome. J Hand Surg Br. 1994;19(6):725–728. | ||
Aygül R, Ulvi H, Kotan D, Kuyucu M, Demir R. Sensitivities of conventional and new electrophysiological techniques in carpal tunnel syndrome and their relationship to body mass index. J Brachial Plex Peripher Nerve Inj. 2009;31:4–12. | ||
Schuhfried O, Vacariu G, Kopf A, Paternostro-Sluga T. Relative slowing of the median antidromic sensory nerve conduction velocity to the ring finger in screening for carpal tunnel syndrome. J Hand Surg. 2004;29(5):947–952. | ||
Chang MH, Wei SJ, Chiang HL, Wang HM, Hsieh PF, Huang SY. Comparison of motor conduction techniques in the diagnosis of carpal tunnel syndrome. Neurology. 2002;58(11):1603–1607. | ||
Alemdar M. Ulnar to median nerve minimum F-wave latency difference in confirmation of ulnar neuropathy at elbow. J Clin Neurophysiol. 2013;30(4):411–414. | ||
Sander HW, Quinto C, Saadeh PB, Chokroverty S. Sensitive median-ulnar motor comparative techniques in carpal tunnel syndrome. Muscle Nerve. 1999;22(1):88–98. | ||
Ozge A, Cömelekoglu U, Tataroglu C, Yalçinkaya DE, Akyatan MN. Subtypes of carpal tunnel syndrome: median nerve F wave parameters. Clin Neurol Neurosurg. 2002;104(4):322–327. | ||
Cevik MU, Altun Y, Uzar E, et al. Diagnostic value of F-wave inversion in patients with early carpal tunnel syndrome. Neurosci Lett. 2012;508(2):110–113. | ||
Komurcu HF, Kilic S, Anlar O. Value of F-wave inversion in diagnosis of carpal tunnel syndrome and it’s relation with anthropometric measurements. J Back Musculoskelet Rehabil. 2015;28(2):377–381. | ||
Mondelli M, Aretini A. Low sensitivity of F-wave in the electrodiagnosis of carpal tunnel syndrome. J Electromyogr Kinesiol. 2015;25(2):247–252. | ||
Park KM, Shin KJ, Park J, Ha SY, Kim SE. The usefulness of terminal latency index of median nerve and f-wave difference between median and ulnar nerves in assessing the severity of carpal tunnel syndrome. J Clin Neurophysiol. 2014;31(2):162–168. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.