Back to Journals » Clinical Epidemiology » Volume 7
Validation of second trimester miscarriages and spontaneous deliveries
Authors Sneider K, Langhoff-Roos J , Sundtoft I , Christiansen OB
Received 20 March 2015
Accepted for publication 2 July 2015
Published 11 December 2015 Volume 2015:7 Pages 517—527
DOI https://doi.org/10.2147/CLEP.S85107
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Vera Ehrenstein
Kirstine Sneider,1 Jens Langhoff-Roos,2 Iben Blaabjerg Sundtoft,3 Ole Bjarne Christiansen4,5
1Department of Clinical Research, Vendsyssel Hospital, Hjørring, 2Department of Obstetrics, Rigshospitalet, University of Copenhagen, Copenhagen, 3Department of Obstetrics and Gynecology, Aarhus University Hospital, Aarhus, 4Department of Obstetrics and Gynecology, Aalborg University Hospital, Aalborg, 5The Fertility Clinic, University Hospital, Copenhagen, Denmark
Objective: To validate the diagnosis of second trimester miscarriages/deliveries (16+0 weeks to 27+6 weeks of gestation) recorded as miscarriages in the Danish National Patient Registry or spontaneous deliveries in the Danish Medical Birth Registry, and asses the validity of risk factors, pregnancy complications, and cerclage by review of medical records.
Materials and methods: In a cohort of 2,358 women with a second trimester miscarriage/delivery in first pregnancy and a subsequent delivery during 1997–2012, we reviewed a representative sample of 682 medical records. We searched for clinically important information and calculated positive predictive values of the registry diagnoses stratified by type of registry, as well as sensitivity, specificity, positive predictive value, and kappa coefficients of risk factors, pregnancy complications, and cerclage.
Results: Miscarriage/spontaneous delivery in the second trimester was confirmed in 621/682 patients (91.1%). Pregnancy complications in second trimester miscarriages were underreported, resulting in low sensitivities and poor to moderate agreements between records and registries. There was a good agreement (kappa >0.6) between medical records and the registries regarding risk factors and cerclage. The diagnosis of cervical insufficiency had “moderate” kappa values for both miscarriages and deliveries (0.55 and 0.57).
Conclusion: Spontaneous second trimester deliveries and miscarriages recorded in the registers were confirmed by medical records in 91%, but register-based information on pregnancy complications need to be improved. We recommend that all pregnancies ending spontaneously beyond the first trimester are included in the national birth registry and described by appropriate variables.
Keywords: second trimester, miscarriage, preterm birth, prematurity, registries, reproducibility of results, cerclage, cervical insufficiency
Corrigendum has been published
Introduction
Preterm delivery at or near the limit of viability is associated with a high neonatal mortality and morbidity.1 Survival rates increase progressively with each week gained between gestational week 23 and 28.2 It has been suggested that the risk factors and causes of miscarriage in 16–19 weeks are similar to those of spontaneous deliveries at 20–26 weeks.3,4 Therefore, we chose to define preterm delivery from 16 weeks, a cutoff previously used in a large-scale preterm birth classification study.5
Second trimester miscarriage/delivery is estimated to complicate approximately 0.5%–1% of all deliveries.6–9 Causes are numerous and complex, and require different preventive strategies.10–14 In cervical insufficiency, painless cervical dilation in the second trimester of pregnancy leads to expulsion of the fetus without uterine contractions.15–17 The lack of objective findings and diagnostic tests make the diagnosis of cervical insufficiency elusive. Identification of women with cervical insufficiency is important as recurrence risk is high and prophylactic treatments exist: progesterone and cerclage.18,19
Studies on large populations are required to explore uncommon phenotypes of spontaneous second trimester deliveries and subsequent pregnancy outcomes. Population-based studies rely on valid identification of diagnoses in the registries. Therefore, we present the results of a validation study of the diagnoses of spontaneous second trimester deliveries, risk factors, pregnancy complications, and procedures of cerclage in two national registries.
Materials and methods
The Danish National Patient Registry (DNPR) contains all hospital admissions in Denmark since 1977. The registry also contains 99.4% of all discharge records from Danish hospitals.20 All Danish citizens receive a ten-digit personal identification number, which is used as identification in the registries and medical records filed in the archives. Diagnoses are applied by physicians using the Danish version of the International Classification of Diseases 10th revision (ICD-10; 1994 onward). Outpatient contacts and visits to the emergency room have been recorded since 1995. All births and miscarriages are found in the DNPR, whereas only births are included in the Danish Medical Birth Registry (DMBR), which also includes variables that are not registered for the miscarriages (Apgar score, parity, birth weight, etc). Pregnancy characteristics and complications are integrated in DMBR. The DMBR includes all live births irrespective of gestational age and stillbirth from 22 weeks of gestation. This division is based on the WHO’s universally adopted definition of a live birth as delivery of a fetus that subsequently shows any signs of life, such as movement, heartbeat, or pulsation of the umbilical cord, for however brief a time.21 Fetal deaths before 22 weeks are regarded miscarriages and recorded in DNPR.
In the registries, we identified women hospitalized in Denmark with the diagnosis of miscarriage or spontaneous delivery in week 16–27 during 1997–2012, no prior deliveries, and a subsequent miscarriage/delivery after 16 weeks of gestation (Figure 1). Multiple pregnancies were included. Records with unregistered gestational age and birth weight <1,200 g (n=58) were included in the cohort by the calculated gestational age.22
  | Figure 1 Flowchart of selection for validation. |
Medical records for validation of information on the first pregnancy were retrieved from a total of 13 hospitals. We selected the four largest tertiary hospitals from the five regions in Denmark (the fifth region does not have a tertiary hospital and all extremely preterm deliveries are therefore referred to another region). We randomly selected between one and three secondary hospitals from each of the five regions without knowledge of specific local routines or registration procedures. From the selected hospitals we retrieved the following samples from the registries: 1) second trimester spontaneous delivery/miscarriage in both first and second pregnancy beyond 16 weeks of gestation (n=88) and 2) second trimester spontaneous delivery/miscarriage in first pregnancy beyond 16 weeks and third trimester delivery in second pregnancy beyond 16 weeks (n=652).
The review of medical records included ultrasound and surgical descriptions, autopsy reports, blood samples and the birth chart with admission history, description of the delivery, and the outcome. For each record, we decided whether a diagnosis of spontaneous second trimester delivery could be confirmed. Data were collected from the records using Epidata Data Entry (EpiData Association, http://www.epidata.dk) by one of the authors (KS).
Validation of the diagnoses related to the first spontaneous second trimester delivery/miscarriage was carried out with the knowledge of the outcome of subsequent pregnancy, sometimes at the same hospital. However, the criteria for categorization by pathway to delivery (spontaneous vs caregiver-initiated) were explicit, and when in doubt the case was discussed with a second reviewer (n=25).
A spontaneous onset of delivery was defined by the presence of initial signs of delivery (contractions, bleeding, preterm premature rupture of membranes [PPROM], or painless cervical dilation), but contractions may be augmented and delivery may be by cesarean section. The definitions and ICD-10 codes were as follows: Spontaneous onset of delivery (DO800–DO809, DO840–DO842, DO821B/C, DO843B/C in the absence of the Danish code of induction of labor, BKHD2) and miscarriage (DO030–DO039) combined with the Danish codes for gestational week 16+0–27+6 (DU16D1–DU27D6). Duration of gestation was calculated from the 1st day of last period or estimated by an early ultrasound. From 2004, gestational age has been routinely measured by ultrasound screening at 11–13 weeks. Gestational age was evaluated in two categories: ±1 week and ±2 weeks of gestational age recorded in the medical records. We defined a correct diagnosis of second trimester delivery as a gestational age within weeks 16–27 regardless of errors in gestational age within this period.
Information regarding risk factors was collected until the date of the second delivery. In women with recurrent second trimester deliveries, data collection continued until a first third trimester delivery. Cerclage was placed either in the nonpregnant woman (prepregnancy abdominal cerclage) or in second pregnancy (vaginal cerclage, postconceptional abdominal cerclage). For vaginal cerclages we used the gestational age at the time of placement to distinguish between elective vaginal cerclage (applied before 16 weeks of gestation) and urgent cerclage (applied ≥16 weeks of gestations). Definitions and ICD-10 codes or Danish procedure codes of risk factors, pregnancy complications, and procedures of cerclage are presented in Table S1.
Statistical analysis
We compared the primary diagnoses in the registries with those obtained by review of the medical records (the gold standard). The main outcome was positive predictive value (PPV), defined as the proportion of patients with a diagnosis of second trimester preterm birth in the registries that had the diagnosis verified by medicals records. We calculated PPV with 95% confidence intervals (CI). PPV was calculated for the whole study population and stratified by registrations as miscarriage (DNPR) or birth (DMBR). Distributions in the registries were compared with the Fisher’s exact test. We proceeded with 2×2 cross tables calculating specificity, sensitivity, and PPV for each of the diagnoses related to spontaneous second trimester delivery. Sensitivity is the proportion of patients with a true diagnosis captured by the registry. We calculated sensitivity as (+patient registry + records)/[(+patient registry + records) + (−patient registry + records)]. Specificity is the proportion of patients without a registered diagnosis, who truly do not have the diagnosis. We calculated specificity as (−patient registry − records)/[(−patient registry − records) + (+patient registry − records)]. Sensitivity and specificity were calculated with 95% CI. Sensitivity and specificity were calculated for the following risk factors, pregnancy complications, and types of cerclage: congenital uterine anomalies, uterine fibroids, thrombophilia, cervical conizations, cervical insufficiency, chorioamnionitis, antepartum fetal death, multiple pregnancies, congenital fetal anomalies, placental insufficiency/intrauterine growth retardation (IUGR), placental abruption, PPROM, antepartum bleeding, and cervical cerclage. Cohen’s kappa was estimated as a measure of agreement between the validated and the register-based diagnoses.23
We used SPSS software (Version 22.0; IBM Corporation, Armonk, NY, USA). The study was approved by the Danish Data Protection Agency (journal number 2008-58-0028) and The Danish Health and Medicines Authority (journal number 3-3013-185/1/).
Results
Among 441,904 women with a first pregnancy progressing beyond 16 weeks in Denmark during 1997–2012, 3,489 (0.8%) had a spontaneous delivery or miscarriage before week 28 and 2,358 had a subsequent pregnancy ≥16 weeks (Figure 1). In the sample of 740 registry records from DNPR and DMBR, 682 (92.2%) were available in the hospital achieves. Records were unavailable in eleven of the 13 hospitals.
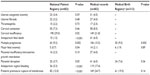
For the second trimester miscarriage/spontaneous delivery diagnoses, we examined gestational age and pathway to delivery independently and in combination (Table 1). A spontaneous pathway to delivery occurring between 16 weeks and 27 weeks of gestation was observed in 621 cases resulting in an overall PPV of 91.1% (95% CI: 88.6–93.0; Table 1). The PPVs were similar in DMBR and DNPR (P=0.08). The level of agreement of gestational age within 2 weeks between registries and medical records were 97.6% for DNPR and 97.7% for DMBR. Among the 61 women in whom the registry diagnosis was not confirmed, 38 were recorded in DNPR. Three women had an early miscarriage, and 37 had induced labor due to fetal or maternal conditions (antepartum fetal death [n=28], malformations [n=3], IUGR [n=2], or maternal conditions [n=2]). Of the 23 women whose registry diagnosis was not confirmed in DMBR, 15 women had induced labor due to antepartum fetal death (n=5), fetal malformations (n=2), and preeclampsia (n=8) and eight women had erroneous gestational recordings (seven term deliveries and one preterm delivery). We found no difference in PPV in tertiary hospitals compared to secondary hospitals.
Table 2 lists frequencies of risk factors and pregnancy complications. No difference was detected in frequencies of risk factors recorded in DNPR and medical records. Cervical insufficiency had a higher frequency in DNPR compared to the records (29.0% vs 21.8%, P=0.02). All other pregnancy complications except placental insufficiency/IUGR were underreported in DNPR (up to 70%).
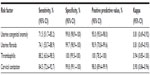
Sensitivities, specificities, and PPVs of pregnancy complication are presented in Table 3. The 2×2 tables of diagnoses in registries and medical records are available in Tables S2 and S3. Most sensitivities of pregnancy complications recorded in DNPR were <50% in miscarriages and 65%–90% in deliveries. Generally, strength of agreements between registries and medical records described by kappa coefficients was “fair” to “moderate” for miscarriages (kappa coefficients 0.21–0.60) and “good” for births (kappa coefficients 0.61–0.80). Specificity was >90% for all diagnoses except cervical insufficiency (81%–86%). The diagnoses of cervical insufficiency had “moderate” kappa coefficients for both miscarriages and deliveries (0.55–0.57). We found no difference in sensitivity of variables available in both registries.
Table 4 lists sensitivities, specificities, and PPVs of risk factors of spontaneous second trimester delivery. The number of diagnoses recorded in DNPR and medical records are available in 2×2 tables in Table S4. Most of the kappa values showed good agreement (≥0.6) between each registry and the medical record.
  | Table 4 Sensitivity, specificity, positive predictive value, and kappa scores of risk factors of spontaneous second trimester delivery/miscarriage |
Sensitivity, specificity, PPVs, and kappa scores of the cervical cerclage are summarized in Table 5. The 2×2 tables of diagnoses in registries and medical records are available in Table S5. All kappa scores were >0.80, corresponding to a “very good” agreement between registry and medical records. Distinguishing between elective and urgent vaginal cerclage by gestational age at cerclage placement (cutoff was 16 weeks) resulted in a decrease in sensitivity, specificity, PPV, and kappa score.
  | Table 5 Sensitivity, specificity, positive predictive value, and kappa scores of different types of cervical cerclage |
Discussion
Medical records confirmed 91% of register-based spontaneous second trimester deliveries. The PPVs were similar in DMBR and DNPR. Kappa coefficients for risk factors associated with second trimester deliveries were ≥0.61, indicating good agreement. Most pregnancy complications in second trimester miscarriage were underreported in DNPR, resulting in low sensitivities and poor to moderate kappa values. The diagnosis of cervical insufficiency had a “moderate” kappa value of 0.55.
This validation study is the first on spontaneous second trimester miscarriages and deliveries described by risk factors and pregnancy complications. We examined a representative segment of the population from hospitals in each of the five Danish regions without knowledge of specific local routines or registration procedures. We have no reason to believe that registration practice in selected hospitals was different from that in other hospitals. Therefore, we assume that the results are generalizable. Unavailable or missing records were less likely to bias the results, as they were missing in small numbers in most of the selected hospitals.
A prior study validated the diagnosis of miscarriage in the DNPR and found a PPV of 97.4%.24 In contrast to our study, the authors used the same code for missed abortions and miscarriages arguing that the two are different presentations of the same conditions. In this study, we have chosen to distinguish between the two diagnoses, as we consider miscarriages and intrauterine fetal death in the absence of symptoms of delivery as different entities.
By using Danish medical registries, we found an incidence of 0.8% of spontaneous second trimester delivery/miscarriage in first time pregnancies beyond 16 weeks, which is comparable to the rates presented in previous publications.6–9,25 We did not search for spontaneous second trimester deliveries among induced deliveries, pregnancy terminations, and miscarriages with unrecorded gestational age, which is a limitation. Our findings of high PPVs indicate that the DNPR and DMBR can be used to identify spontaneous second trimester deliveries/miscarriages for the purpose of register-based cohort studies.
The gestational age registered in DMBR has been evaluated in a previous study.26 Kristensen et al compared a review of medical records of 1,662 preterm deliveries with registry information and found a large number of errors in the length of gestational age. We found agreement between DMBR and medical records within 1 week of 89.4% and within 2 weeks of 97.7%. Implausible combinations of gestational age and birth weight may identify errors in gestational age, but it can be difficult to determine which measure is reliable.
We used a cutoff at 16 gestational weeks to distinguish between elective and urgent vaginal cerclage. Since 30% of miscarriages had at least 1 week difference in gestational age in the medical records compared to the register, some elective cerclages might have been recorded as urgent/emergency, and vice versa.
According to WHO definitions, presence of signs of life at delivery/miscarriage determines whether a delivery of a fetus <22 weeks will be recorded as a miscarriage in DNPR or a delivery in DMBR. There are several problems related to this definition. It may be difficult to distinguish stillborn infants from liveborn infants who are extremely preterm, asphyxiated, or neurologically depressed and who die soon after birth. Even if the fetus is clearly stillborn, it is not possible in registries to distinguish peripartum fetal deaths caused by the preterm delivery from antepartum fetal death. In 2004, in Denmark, the gestational age classifying intrauterine fetal deaths as births was lowered from 28 weeks to 22 weeks. Recent studies, however, have suggested similar causes and risk factors in miscarriages at 16–19 weeks and births at 22–25 weeks.
There is no agreement about the definition of cervical insufficiency.27,28 Traditionally, the diagnosis has been made based on an obstetric history of recurrent second trimester delivery following painless cervical dilation.28 In the absence of recurrence, the term can be applied to a single event with painless cervical dilation after exclusions of other possible causes of preterm delivery.16 The main problem of the diagnosis of cervical insufficiency is that it is not associated with specific symptoms and that there are no diagnostics tests. A low specificity, as observed in this study, indicates that the diagnosis may be applied to a variety of patients that do not suffer from cervical insufficiency. Some use the diagnosis of cervical insufficiency in women with a short cervix measured by ultrasound. For a correct diagnosis of cervical insufficiency, a classification system based on objective components would be beneficial. In particular, we need information on cervical length, dilation, and clinical presentation at admission to hospital in the second trimester.
Placental abruption, PPROM, multiple pregnancies, major fetal anomalies, and antepartum bleeding in miscarriages were underreported DNPR. Without information on pregnancy characteristics and complications, we risk lumping together different phenotypes of second trimester deliveries. A recently published series of clinical opinions described the purpose, challenges, and considerations for a preterm birth classification system.3,4,29 The authors emphasize that precise classification of subtypes of preterm delivery from gestational week 16 will improve understanding of causes of preterm delivery and improve research in treatment and preventive interventions.
Data on three pregnancy complications (placental abruption, PPROM, and fetal anomaly) and multiplicity were available in both DNPR and DMBR and there were no difference in sensitivity, specificity, and kappa coefficients. DMBR is superior due to the readily accessible structure and the linkage between pregnancy characteristics, complications, neonatal outcomes, and maternal demographic data.
Conclusion
In conclusion, we found acceptable diagnostic validity of Danish medical registries in spontaneous second trimester deliveries and miscarriages. Kappa values were good for risk factors for second trimester miscarriage/delivery and cervical cerclage. The diagnosis of cervical insufficiency had “moderate” kappa coefficients for both miscarriages and deliveries (0.55–0.57). Most other pregnancy complications in miscarriages were underreported, resulting in low incidences, sensitivities, and kappa scores compared to cases recorded as deliveries. DNPR and DMBR were equally accurate regarding pregnancy complications in deliveries, but the advantages of DMBR are the readily accessible structure and linkage between pregnancy characteristics, maternal demographic data, and neonatal outcomes. We recommend improved data collection to the national birth registries with detailed information on pregnancies ending after the first trimester – operationally after ultrasound scan showing live fetus at 12 weeks scan. For now, we can use combined data from the Danish patient and the birth registers to identify spontaneous second trimester deliveries and miscarriages. In order to obtain valid information about the etiology based on pregnancy characteristics and complications, we need to retrieve medical records.
Disclosure
The authors report no conflicts of interest in this work.
References
Mohangoo AD, Blondel B, Gissler M, Velebil P, Macfarlane A, Zeitlin J. International comparisons of fetal and neonatal mortality rates in high-income countries: should exclusion thresholds be based on birth weight or gestational age? PLoS One. 2013;8(5):e64869. | |
Patel RM, Kandefer S, Walsh MC, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Causes and timing of death in extremely premature infants from 2000 through 2011. N Engl J Med. 2015;372(4):331–340. | |
Kramer MS, Papageorghiou A, Culhane J, et al. Challenges in defining and classifying the preterm birth syndrome. Am J Obstet Gynecol. 2012; 206(2):108–112. | |
Goldenberg RL, Gravett MG, Iams J, et al. The preterm birth syndrome: issues to consider in creating a classification system. Am J Obstet Gynecol. 2012;206(2):113–118. | |
Barros FC, Papageorghiou AT, Victora CG, et al; International Fetal and Newborn Growth Consortium for the 21st Century. The distribution of clinical phenotypes of preterm birth syndrome: implications for prevention. JAMA Pediatr. 2015;169(3):220–229. | |
Langhoff-Roos J, Kesmodel U, Jacobsson B, Rasmussen S, Vogel I. Preterm delivery in primiparous women at low risk: Preterm birth or delivery? Study authors suggest new terms. BMJ. 2006;332(7547):937–939. | |
Ellett K, Buxton EJ, Luesley DM. The effect of ethnic origin on the rate of spontaneous late mid-trimester abortion. Ethn Dis. 1992;2(1):84–86. | |
Ammon Avalos L, Galindo C, Li D-K. A systematic review to calculate background miscarriage rates using life table analysis. Birth Defects Res A Clin Mol Teratol. 2012;94(6):417–423. doi: 10.1002/bdra.23014. | |
Mercer B, Milluzzi C, Collin M. Periviable birth at 20 to 26 weeks of gestation: proximate causes, previous obstetric history and recurrence risk. Am J Obstet Gynecol. 2005;193(3 pt 2):1175–1180. | |
Jeve Y, Davies W. Evidence-based management of recurrent miscarriages. J Hum Reprod Sci. 2014;7:159. | |
Heller DS, Moorehouse-Moore C, Skurnick J, Baergen RN. Second-trimester pregnancy loss at an urban hospital. Infect Dis Obstet Gynecol. 2003;11(2):117–122. | |
Dukhovny S, Zutshi P, Abbott JF. Recurrent second trimester pregnancy loss: evaluation and management. Curr Opin Endocrinol Diabetes Obes. 2009;16(6):451–458. | |
Michels TC, Tiu AY. Second trimester pregnancy loss. Am Fam Physician. 2007;76(9):1341–1346. | |
Chan YY, Jayaprakasan K, Tan A, Thornton JG, Coomarasamy A, Raine-Fenning NJ. Reproductive outcomes in women with congenital uterine anomalies: a systematic review. Ultrasound Obstet Gynecol. 2011;38(4):371–382. doi: 10.1002/uog.10056. | |
Easterday L, Reid DE. The incompetent cervix in repetitive abortion and premature labor. N Engl J Med. 1959;260:687–690. | |
Lotgering FK. Clinical aspects of cervical insufficiency. BMC Pregnancy Childbirth. 2007;7(Suppl 1):S17. doi: 10.1186/1471-2393-7-S1–S17. | |
Owen J. Cervical insufficiency. Queenan’s Manag High-Risk Pregnancy Evidence-Based Approach Sixth Ed. 2012;85(48):271–279. | |
Hassan SS, Romero R, Vidyadhari D, et al; PREGNANT Trial. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: a multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2011;38(1):18–31. | |
Rode L, Langhoff-Roos J, Andersson C, et al. Systematic review of progesterone for the prevention of preterm birth in singleton pregnancies. Acta Obstet Gynecol Scand. 2009;88:1180–1189. | |
Nickelsen TN. Data validity and coverage in the Danish National Health Registry. A literature review. Ugeskr Laeger. 2001;164(1):33–37. | |
World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 10th Revision. Geneva, Switzerland: World Health Organization; 1993:129. | |
Honarvar M, Allahyari M, Dehbashi S. A simple estimated fetal weight equation for fetuses between 24 and 34 weeks of gestation. Int J Gynaecol Obstet. 1999;67(2):67–74. | |
Altman D. Practical Statistics for Medical Research. London: Chapman and Hall/CRC; 1991:396–439. | |
Lohse SR, Farkas DK, Lohse N, et al. Validation of spontaneous abortion diagnoses in the Danish National Registry of Patients. Clin Epidemiol. 2010;2:247–250. | |
Chauhan SP, Ananth CV. Periviable births: epidemiology and obstetrical antecedents. Semin Perinatol. 2013;37(6):382–388. | |
Kristensen J, Langhoff-Roos J, Skovgaard LT, Kristensen FB. Validation of the Danish Birth Registration. J Clin Epidemiol. 1996; 49(8):893–897. | |
Brown R, Gagnon R, Delisle MF, et al; Maternal Fetal Medicine Committee, Society of Obstetricians and Gynaecologists of Canada. Cervical insufficiency and cervical cerclage. J Obstet Gynaecol Can. 2013;35(12):1115–1127. | |
American College of Obstetricians and Gynecologists. ACOG practice bulletin No.142: cerclage for the management of cervical insufficiency. Obstet Gynecol. 2014;123(2 pt 1):372–379. | |
Villar J, Papageorghiou AT, Knight HE, et al. The preterm birth syndrome: a prototype phenotypic classification. Am J Obstet Gynecol. 2012;206(2):119–123. | |
Nell S, Wijngaarde CA, Pistorius LR, et al. Fetal Diag Ther. 2013; 33(4):235–240. |
Supplementary materials
  | Table S1 Definitions and codes of risk factors, pregnancy complications, and cerclage |
  | Table S2 Diagnoses recorded in The Danish National Patient Registry (DNPR) by the presence of the condition in medical records |
  | Table S3 Diagnoses recorded in The Danish Medical Birth Registry (DMBR) by the presence of the condition in medical records |
  | Table S4 Diagnoses recorded in the Danish National Patient Registry (DNPR) by the presence of the risk factor/surgical intervention observed in medical records |
  | Table S5 Diagnoses recorded in The Danish National Patient Registry (DNPR) by the presence of the procedure in medical records |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.