Back to Journals » Clinical Interventions in Aging » Volume 17
Validation of Abbreviated Form of the Multidimensional Prognostic Index (MPI): The BRIEF-MPI Project
Authors Cella A, Veronese N, Custodero C, Castagna A, Cammalleri LA, Capitano WM, Solimando L, Carruba L, Sabbà C, Ruotolo G, Barbagallo M, Pilotto A
Received 10 January 2022
Accepted for publication 10 March 2022
Published 12 May 2022 Volume 2022:17 Pages 789—796
DOI https://doi.org/10.2147/CIA.S355801
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Alberto Cella,1 Nicola Veronese,2 Carlo Custodero,3 Alberto Castagna,4 Lisa A Cammalleri,1 Walter M Capitano,2 Luisa Solimando,2 Luca Carruba,2 Carlo Sabbà,3 Giovanni Ruotolo,4 Mario Barbagallo,2 Alberto Pilotto1,3
1Department of Geriatric Care, Orthogeriatrics and Rehabilitation, E.O. Ospedali Galliera, Genova, Italy; 2Geriatric Unit, Department of Internal Medicine and Geriatrics, University of Palermo, Palermo, Italy; 3Department of Interdisciplinary Medicine, University of Bari “Aldo Moro”, Bari, Italy; 4Geriatrics Unit, “Pugliese Ciaccio” Hospital, Catanzaro, Italy
Correspondence: Alberto Pilotto, Via delle Mura Capuccine, 14, Genova, 16128, Italy, Tel +39 010 5634400, Fax +39 010 5634400, Email [email protected]
Purpose: To screen multidimensional frailty in older people, using a comprehensive geriatric assessment (CGA) tool such as the multidimensional prognostic index (MPI), is a public health priority. Unfortunately, the screening tools available are not able to capture multidimensional frailty. In this work, we aimed to evaluate in a population of hospitalized and ambulatory older patients, the agreement between an abbreviated form of the MPI (ie, BRIEF-MPI) and the standard/full version.
Participants and Methods: All participants included in the study completed both versions of the MPI, brief and full, which share the following domains: 1) basic and 2) instrumental activities of daily living, 3) mobility/risk of pressure sores, 4) cognition, 5) nutrition, 6) comorbidity, 7) social and 8) number of medications. The agreement between the two instruments was reported using either the mean comparisons with a t-test matched sample, a simple correlation analysis and the Bland–Altman methodology.
Results: The study sample included 110 participants (mean age=83.2 years, 51.8% women). The mean difference was statistically and clinically irrelevant (mean difference=0.01± 0.10; p=0.27). The correlation between brief and full MPI versions was optimal (R=0.82, p< 0.0001). Using the Bland–Altman methodology, we observed that only three participants over 110 (=2.73%) were outside the limits of agreement. The accuracy of BRIEF-MPI in predicting multidimensional frailty, as full MPI> 0.66, was optimal (area under the curve=0.92, p< 0.0001). A BRIEF-MPI value of 0.59 yielded the highest sensitivity and specificity in predicting multidimensional frailty.
Conclusion: BRIEF-MPI had a good agreement with the full/standard version of the MPI, making this tool as ideal for the screening of multidimensional frailty in older people.
Keywords: multidimensional prognostic index, screening, frailty, agreement
Introduction
The growing population of aging imposes a broader diffusion of traditional geriatric assessment, also outside the more classic geriatric settings (ie, geriatric ward, ambulatory activity, nursing home).1 The COVID-19 pandemic further increased this need, with clinicians often struggling for instruments able to help in the case-finding of older adults more at risk of negative outcomes.2 To date simple case-finding tools include judgement-based measures such as the Clinical Frailty Scale (CFS),3 physical performance-based measures such as gait speed,4 the frailty phenotype,5 and questionnaire-based measures such as the PRISMA-76 which, however, unlikely capture the different spectrum of geriatric disorders and serve as prognostic tools.
These concepts indicate the need to stratify older adults according to their prognosis based upon instrument derived from Comprehensive Geriatric Assessment (CGA), the gold standard in the evaluation of older adults.7 Several multicenter studies demonstrated that the multidimensional prognostic index (MPI), a CGA derived tool had excellent accuracy and calibration in predicting the clinical outcomes typical of older people, such as hospitalization, institutionalization, need for homecare services and mortality.8,9 Nowadays, the MPI has been validated in over 54,000 older adults suffering from the most common chronic and acute age-related diseases associated with high mortality in over 50 international studies.10 Unfortunately, in some settings (eg, emergency departments, intensive care units, general practitioners’ ambulatory, or surgical wards), it could be perceived time-consuming, even if the MPI may require approximately 15–25 minutes.8
Therefore, it could be useful developing an abbreviated version of MPI that, following the same concept of “multidimensional frailty” and preserving the prognostic accuracy of the original tool, may serve as screening tool to support individuals who are not trained in CGA to move the assessment and management plan forward.
Given this background, we aimed to evaluate, for the first time, in a population of hospitalized older patients the agreement between an abbreviated form of the MPI (ie, BRIEF-MPI) and the standard/full version of the MPI.
Participants and Methods
Participants
Participants were consecutively enrolled at two Italian hospitals (Palermo, Genova) and one center enrolling older outpatients (Catanzaro) participating in the project between 01st and 31st October 2021. As inclusion criteria we used only an age more than 65 years and the capacity to understand the project; we excluded older people who did not want to participate in the project.
This project falls within the aims of the MULTIPLAT-AGE, approved by the Ethical Committee of the Liguria Region (protocol: 176/2021) on 17 May 2021. The study complies with the Declaration of Helsinki.
Multidimensional Prognostic Index (Full Version)
The Multidimensional Prognostic Index (MPI) is a prognostic tool based on a standardized CGA which allows to predict short- and long-term mortality and other negative health outcomes11 in older subjects.8 MPI includes eight domains as follows:
1) Activities of daily life (ADL - Activities of Daily Living);12
2) Instrumental activities of daily living (IADL - Instrumental Activities of Daily Living);13
3) Short Portable Mental Status Questionnaire (SPMSQ):14 composed of 10 questions which assessed the patient’s cognitive status;
4) Exton-Smith Scale (ESS):15 composed of 5 items for assessing the risk of developing pressure sores;
5) Nutritional Assessment (MNA, Mini-Nutritional Assessment) -short form:16 it consists of 6 items to assess the patient’s nutritional status through three different types of assessments;
6) Cumulative Illness Rating Scale (CIRS):17 consisting of 14 items to describe the pathologies present at the time of patient recruitment, identifying their severity by calculating the comorbidity and severity index respectively;
7) Number of drugs in use;
8) Cohabitation status.
To each domain is assigned a score corresponding to a risk, ie, low (value of 0), moderate (value of 0.5), and high (value of 1). The MPI is expressed as a continuous value from 0.0 (lowest risk of mortality) to 1.0 (highest risk of mortality), identifying three groups at different risk of mortality MPI-1: mild risk (MPI values from 0.0 to 0.33); MPI-2: moderate risk (MPI values from 0.34 to 0.66); MPI-3: severe risk (MPI values from 0.67 to 1.0).8
The calculation of the final MPI was made through the software application available for free at the https://multiplat-age.it/index.php/en/tools.
The BRIEF-MPI
To develop the BRIEF-MPI, we selected functional and clinical items available in the full standard MPI according to a clinical-driven CGA-based assessment of the older subject.
In developing the BRIEF-MPI, we preserved the multidimensional structure of the original version, including the same domains and the structure, according to the three prognostic categories of the MPI. In detail, we considered: 1) to avoid repetitions of the items in the different scales (eg, incontinence); 2) gender differences (eg, some IADLs are distributed according to gender); 3) to better underline the role of mobility, as we made in the MPI-InChianti study;18 4) the hierarchy in the progression of loss of functions, particularly for ADLs and IADLs. Finally, to assess the nutritional status, we included the three cornerstones of the nutritional assessment, ie, body mass index, weight loss, change in food intake. The other domains, ie comorbidities, number of drugs and co-habitation status, were not modified.
Thus, the abbreviated version of MPI (BRIEF-MPI) explore the same eight domains of the standard/full MPI preserving the multidimensional concept of frailty assessment, but reducing the evaluation to only 18 the items to collect, as reported in Supplementary Table 1:
1) Activities of daily life derived from ADL test12 included three items with dichotomous answer (yes/no) to evaluate the independence in dressing and feeding and self-control over urination and defecation;
2) Instrumental activities of daily living derived from IADL test13 including three items with dichotomous answer (yes/no) to evaluate the independence in using the telephone, taking medications, and shopping;
3) Cognition evaluated using three items of the SPMSQ14 assessing temporal and personal orientation, and computation ability;
4) Mobility, based on the Barthel mobility scale, evaluated inquiring about the abilities to transfer from bed to chair or wheelchair, walking and going up and down the stairs.18 The ability of doing these activities will be categorized as yes (1 point) or no (0 point);
5) Nutritional Assessment assessing with dichotomous answer (yes/no) three items from MNA-short form:16 BMI (<21 or ≥ 30 kg/m2), loss of appetite in the last three months, and weight loss in the last three months;
6) Comorbidities using the CIRS derived from SELFY-MPI19 and expressed as number of health diseases requiring drug therapies across 13 health areas;
7) Number of drugs in use as for standard MPI;
8) Cohabitation status as for standard MPI.
Similarly, to the full MPI, as shown in Supplementary Table 2, to each domain was assigned a score corresponding to a risk (0, 0.5, or 1) and expressed as a continuous value from 0.0 (lowest risk of mortality) to 1.0 (highest risk of mortality). Appropriate validated cut-off (ie, 0.33 and 0.66) were used for categorizing BRIEF-MPI in three categories (Supplementary Table 2). The BRIEF-MPI requires in mean 5 (SD=1.5) minutes for the execution, with a range between 1 to 10 minutes.
Statistical Analysis
Main findings were summarized using means and standard deviation [SD] for continuous variables and absolute numbers and percentages for categorical variables.
The agreement between the brief and full versions of the MPI was assessed using several approaches, including: 1. Mean comparisons with a t-test matched sample; 2. Simple correlation analysis; 3. The Bland–Altman (BAP) methodology. The BAP methodology provides an objective measure (95% limits of agreement) and a visual representation (plot of the difference vs the mean of the two measures) of the level of agreement between two different measures.20
The accuracy of BRIEF-MPI in predicting the presence of multidimensional frailty, as a full MPI>0.66, was analyzed using the area under the curve (AUC). The best point of BRIEF-MPI, in terms of sensitivity and specificity, was then reported.
We reported two-tailed probabilities, and a p-value of 0.05 was adopted to define nominal statistical significance. All analyses were conducted using the software STATA (version 14.2; StataCorp., College Station, TX) and SPSS 20.0.
Results
Altogether, 110 participants in hospital (Palermo and Genova) and partly in a geriatric ambulatory (Catanzaro), were enrolled. Only three participants, previously contacted, decided to not participate in the study. The mean age was 83.2±6.9 years (range: 65–101) and the participants were mainly females (=51.8%), as reported in Table 1. The main causes of hospitalization in Palermo and Genova’s hospital were heart failure and pneumonia and chronic obstructive pulmonary disease exacerbation.
 |
Table 1 Baseline Characteristics of the Participants Included |
The mean MPI value, using the full version, was 0.53±0.18 (range: 0.13 to 0.88) having 10 participants in MPI-1 (=9.1%), 67 in MPI-2 (=60.9%), and 33 in MPI-3 (=30.0%). Table 2 shows the mean difference between full and brief versions of MPI, including their domains. Overall, the full and the brief versions of the MPI were not significantly different (mean difference=0.01±0.10; p=0.27). Among the domains included, ADL (p=0.40) and mobility items (p=0.16) did not significantly differ between brief and full versions. The linear correlation between full and BRIEF-MPI was optimal, as shown in Figure 1 (R=0.82, p<0.0001). Finally, using the BAP methodology, we observed that only three participants over 110 (=2.73%) were outside the limits of agreement (Figure 2).
 |
Table 2 Comparison Between Full and BRIEF Multidimensional Prognostic Index |
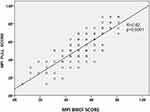 |
Figure 1 Linear correlation between full and BRIEF Multidimensional Prognostic Index. |
 |
Figure 2 Bland–Altman plot for the agreement between BRIEF and full Multidimensional Prognostic Index. |
Figure 3 shows the accuracy of BRIEF-MPI in predicting multidimensional frailty, as full MPI>0.66. The area under the curve was 0.92 (p<0.0001) indicating an optimal accuracy and a value of BRIEF-MPI of 0.59 had a sensitivity in identifying multidimensional frailty was 82% and a specificity of 88%.
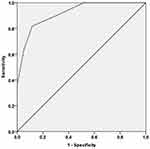 |
Figure 3 Accuracy of BRIEF Multidimensional Prognostic Index in predicting the presence of frailty using full Multidimensional Prognostic Index. |
Discussion
In this work, including 110 older in and outpatients, we found that the abbreviated form of the MPI, ie, BRIEF-MPI, had a good agreement with the standard/full version. Using the Bland-Altman plot, we found that only a very small part of older people felt outside the limits of agreement and that the accuracy of BRIEF-MPI in predicting multidimensional frailty was therefore optimal. Altogether, these findings indicate that an abbreviated version of the MPI can be used as a screening tool in settings in which time is limited.
The instruments for the screening frailty are several but limited to the identification of physical frailty or as frailty defined as accumulation of health deficits. For the identification of physical frailty, for example, the FRAIL scale is based on five simple questions predicting the presence of frailty according to the frailty phenotype.21 Similarly, the CFS can be used as a screening tool for detecting frailty in older people even if, unfortunately, during COVID-19 this screening tool was used as a diagnostic tool22 while CFS is not able to capture the different spectrum of geriatric problems and the complexity of older person.23 In an interesting new study of 100 Danish older people,23 CFS and MPI showed a fair and equal efficiency to predict 90-day mortality, but these two tools can have different roles in geriatric assessment: CFS may be more appropriately used in the ED screening patients for frailty,24 whilst MPI can be recommended to better understand the complex physical and mental health needs in older patients, particularly for the clinical decision making.23
With the current work, we tried to formulate an abbreviated form of the MPI in order to give an easy screening tool for detecting multidimensional frailty, a condition that is highly present in older people25 and it is associated with several negative outcomes in older individuals.26 Of importance, multidimensional frailty seems to be more accurate than physical frailty in predicting mortality both in hospital27 and in community-dwelling settings.28 Therefore, our current work can further highlight the importance of having a specific tool for quickly identifying older individuals that can be considered frail using a CGA derived tool. In particular, a BRIEF-MPI more than 0.59 identifies with a good accuracy and with good specificity/sensitivity, older people that could be frail from a multidimensional point of view and then needing a CGA evaluation of their needs and problems.
Finally, we found an important difference in the completion time between the full and the brief version of the MPI. The standard MPI, in fact, may require 15–25 minutes,8 whilst the BRIEF-MPI only five minutes, making the BRIEF-MPI ideal for the screening of frailty in older people, across different settings.
The findings of this study must be interpreted within its limitations. First, the cohort enrolled was relatively small, consisting of 110 included participants. However, we plan to use in bigger samples and in different contexts in which geriatric patients are present. Moreover, the population included was quite frail, since only 10/110 of patients were categorized as MPI 1, probably explaining the lower agreement observed in MPI 1 category and probably indicating the presence of a proportional bias in our findings. These considerations further stress the need to further validate the BRIEF-MPI not only in different settings, bur also in a less frail population. Second, some domains are significantly different between full and brief version of the MPI: in particular, the IADL and MNA seem to be underestimated by the BRIEF-MPI, whereas the CIRS seems to be overestimated by the BRIEF MPI, compared to the full version, finally suggesting that more research is needed. Finally, the majority of the people was included from hospital setting, whilst the application of BRIEF-MPI could be more useful in other settings such as emergency department or primary care.
Conclusion
BRIEF-MPI had a good agreement with the full/standard version of the MPI, making this tool as ideal for the screening of multidimensional frailty in older people. Further studies are needed to verify the validity of BRIEF-MPI in other settings in which the geriatrician is currently involved.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. Lancet. 2019;394(10206):1376–1386. doi:10.1016/S0140-6736(19)31785-4
2. Polidori MC, Maggi S, Mattace-Raso F, Pilotto A. The unavoidable costs of frailty: a geriatric perspective in the time of COVID-19. Geriatric Care. 2020;6(1):8989. doi:10.4081/gc.2020.8989
3. Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–495. doi:10.1503/cmaj.050051
4. Cesari M. Role of gait speed in the assessment of older patients. JAMA. 2011;305(1):93–94. doi:10.1001/jama.2010.1970
5. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol a Biol Sci Med Sci. 2001;56(3):M146–56. doi:10.1093/gerona/56.3.m146
6. Raiche M, Hebert R, Dubois MF. PRISMA-7: a case-finding tool to identify older adults with moderate to severe disabilities. Arch Gerontol Geriatr. 2008;47(1):9–18. doi:10.1016/j.archger.2007.06.004
7. Turner G, Clegg A; British Geriatrics S, Age UK, Royal College of General P. Best practice guidelines for the management of frailty: a British Geriatrics Society, Age UK and Royal College of general practitioners report. Age Ageing. 2014;43(6):744–747. doi:10.1093/ageing/afu138
8. Pilotto A, Ferrucci L, Franceschi M, et al. Development and validation of a multidimensional prognostic index for one-year mortality from comprehensive geriatric assessment in hospitalized older patients. Rejuvenation Res. 2008;11(1):151–161. doi:10.1089/rej.2007.0569
9. Cruz-Jentoft AJ, Daragjati J, Fratiglioni L, et al. Using the Multidimensional Prognostic Index (MPI) to improve cost-effectiveness of interventions in multimorbid frail older persons: results and final recommendations from the MPI_AGE European project. Aging Clin Exp Res. 2020;32(5):861–868. doi:10.1007/s40520-020-01516-0
10. Pilotto A, Custodero C, Maggi S, Polidori MC, Veronese N, Ferrucci L. A multidimensional approach to frailty in older people. Ageing Res Rev. 2020;60:101047. doi:10.1016/j.arr.2020.101047
11. Pilotto A, Veronese N, Daragjati J, et al. Using the multidimensional prognostic index to predict clinical outcomes of hospitalized older persons: a prospective, multicenter, international study. J Gerontol. 2019;74(10):1643–1649. doi:10.1093/gerona/gly239
12. Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. 1970;10(1):20–30. doi:10.1093/geront/10.1_part_1.20
13. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. doi:10.1093/geront/9.3_Part_1.179
14. Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433–441. doi:10.1111/j.1532-5415.1975.tb00927.x
15. Bliss MR, McLaren R, Exton-Smith AN. Mattresses for preventing pressure sores in geriatric patients. Mon Bull Minist Health Public Health Lab Serv. 1966;25:238–268.
16. Kaiser MJ, Bauer JM, Ramsch C, et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13(9):782–788. doi:10.1007/s12603-009-0214-7
17. Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc. 1968;16(5):622–626. doi:10.1111/j.1532-5415.1968.tb02103.x
18. Pilotto A, Veronese N, Siri G, et al. Association between the multidimensional prognostic index and mortality over 15 years of follow-up in the Inchianti Study. J Gerontol a Biol Sci Med Sci. 2020. doi:10.1093/gerona/glaa237
19. Pilotto A, Veronese N, Quispe Guerrero KL, et al. Development and validation of a self-administered multidimensional prognostic index to predict negative health outcomes in community-dwelling persons. Rejuvenation Res. 2019;22(4):299–305. doi:10.1089/rej.2018.2103
20. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. doi:10.1016/S0140-6736(86)90837-8
21. Morley JE, Malmstrom T, Miller D. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601–608. doi:10.1007/s12603-012-0084-2
22. Pranata R, Henrina J, Lim MA, et al. Clinical frailty scale and mortality in COVID-19: a systematic review and dose-response meta-analysis. Arch Gerontol Geriatr. 2020;93:104324. doi:10.1016/j.archger.2020.104324
23. Verholt AB, Gregersen M, Gonzalez-Bofill N, et al. Clinical presentation and outcomes of COVID-19 in older hospitalised patients assessed by the record-based multidimensional prognostic index, a cross-sectional study. Eur Geriatr Med. 2021;12:1–11.
24. Dent E, Morley J, Cruz-Jentoft A, et al. Physical frailty: ICFSR international clinical practice guidelines for identification and management. J Nutr Health Aging. 2019;23(9):771–787. doi:10.1007/s12603-019-1273-z
25. Veronese N, Custodero C, Cella A, et al. Prevalence of multidimensional frailty and pre-frailty in older people in different settings: a systematic review and meta-analysis. Ageing Res Rev. 2021;72:101498. doi:10.1016/j.arr.2021.101498
26. Pilotto A, Cella A, Pilotto A, et al. Three decades of comprehensive geriatric assessment: evidence coming from different healthcare settings and specific clinical conditions. J Am Med Dir Assoc. 2017;18(2):
27. Pilotto A, Rengo F, Marchionni N, et al. Comparing the prognostic accuracy for all-cause mortality of frailty instruments: a multicentre 1-year follow-up in hospitalized older patients. PLoS One. 2012;7(1):e29090. doi:10.1371/journal.pone.0029090
28. Cella A, Veronese N, Pomata M, et al. Multidimensional frailty predicts mortality better than physical frailty in community-dwelling older people: a Five-Year Longitudinal Cohort Study. Int J Environ Res Public Health. 2021;18(23):12435. doi:10.3390/ijerph182312435
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
