Back to Journals » OncoTargets and Therapy » Volume 10
Validation of a novel prognostic scoring system using inflammatory response biomarkers in patients undergoing curative thoracoscopic esophagectomy for esophageal squamous cell carcinoma
Authors Hirahara N, Fujii Y, Yamamoto T, Hyakudomi R, Hirayama T , Taniura T, Ishitobi K, Tajima Y
Received 13 October 2016
Accepted for publication 9 December 2016
Published 13 January 2017 Volume 2017:10 Pages 363—370
DOI https://doi.org/10.2147/OTT.S124556
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Geoffrey Pietersz
Noriyuki Hirahara, Yusuke Fujii, Tetsu Yamamoto, Ryoji Hyakudomi, Takanori Hirayama, Takahito Taniura, Kazunari Ishitobi, Yoshitsugu Tajima
Department of Digestive and General Surgery, Shimane University Faculty of Medicine, Shimane, Japan
Background: Systemic inflammatory markers, including the lymphocyte-to-monocyte ratio, neutrophil-to-lymphocyte ratio, and platelet-to-lymphocyte ratio have been shown to predict postoperative recurrence and survival in various types of cancer. However, their role in esophageal cancer has yet to be determined. This study aimed to evaluate the prognostic significance of an inflammatory response biomarker (IRB) score, independent of conventional clinicopathological criteria, in patients with esophageal cancer undergoing curative resection.
Patients and methods: We retrospectively reviewed a database containing the medical records of 147 consecutive patients who underwent curative esophagectomy for esophageal squamous cell carcinoma. The IRB score was determined as follows: a low lymphocyte-to-monocyte ratio (<4), a low neutrophil-to-lymphocyte ratio (<1.6), and a high platelet-to-lymphocyte ratio (>147), which were each scored as 1, with all remaining values scored as 0. The scores were added together to produce the IRB score (range: 0–3).
Results: An IRB score of 2–3 (hazard ratio: 6.023, 95% confidence interval: 1.675–13.078; P<0.01) was identified as an independent poor prognostic factor of cancer-specific survival (CSS) in a multivariate logic regression analysis. The 5-year CSS rates in patients with the IRB scores of 0-1, 2, and 3 were 37.8%, 67.8%, and 72.5%, respectively. As determined by Kaplan–Meier analysis and the log-rank test, these differences were significant (P<0.001).
Conclusion: The IRB score can predict the systemic inflammatory response as accurately as conventional tumor markers and is useful for determining CSS in patients with esophageal cancer undergoing curative thoracoscopic esophagectomy.
Keywords: esophageal squamous cell carcinoma, prognosis, inflammatory response biomarker score, IRB score, lymphocyte-to-monocyte ratio, neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio
Introduction
Tumor biology and host-related factors, such as performance status, weight loss, smoking, drinking, and comorbidity, play an important well-recognized role in the outcome of patients with cancer. It is clear that a genetic basis underlies cancer development and host inflammatory response to the tumor plays a key role in carcinogenesis, cancer development, progression, and metastasis. Colaprico et al1 showed interesting networks of pathways that could regulate target genes in breast cancer, including stem cell pluripotency, coagulation, and hypoxia pathways and microRNAs (miRNAs). Moreover, these networks could be potential biomarkers for diagnostic, prognostic, and therapeutic developments in breast cancer. Recent studies have demonstrated an association between the preoperative systemic inflammatory response (SIR) and a poorer postoperative survival, owing to its involvement in tumor development, cell survival, and angiogenesis that can lead to metastasis.2,3 Based on this, a number of inflammatory-based prognostic markers have been identified, such as the Glasgow Prognostic Score (GPS), modified GPS (mGPS), and Prognostic Nutritional Index (PNI), in esophageal cancer.4–6 However, only a few studies have evaluated the utility of lymphocyte-to-monocyte ratio (LMR), neutrophil-to-lymphocyte ratio (NLR), and platelet-to-lymphocyte ratio (PLR) for assessing the prognosis of patients with esophageal cancer.7–9 Previous studies revealed that high LMR and NLR, and low PLR are the strong predictors of postoperative survival in several types of cancer.7–9 In addition, these parameters are routinely measured by automated hematology analyzer in daily medical practice and are easily available and inexpensive, which is one of the major advantages of their clinical application. However, their prognostic significance in esophageal cancer has yet to be determined.7,10,11 Therefore, a prognostic scoring system that combines the ratios of all three inflammatory markers (ie, the inflammatory response biomarker [IRB] score) could more accurately predict survival in patients with esophageal cancers, including esophageal squamous cell carcinoma (SCC). Identification of those patients who are most at risk of developing postoperative recurrence is important because it facilitates the personalization of each patient’s treatment plan according to the risk of recurrence.
In this study, we aimed to evaluate the prognostic significance of the IRB score in patients with esophageal SCC after curative resection.
Patients and methods
Patients
We retrospectively reviewed a database containing the medical records of 147 consecutive patients who underwent curative esophagectomy with R0 resection for histologically confirmed esophageal SCC between January 2006 and February 2015 at Shimane University Hospital (Shimane, Japan). R0 resection was defined as complete resection in the absence of microscopic resection margin involvement. Video-assisted or thoracoscopic subtotal esophagectomy with three-field lymph node dissection was performed in all patients, followed by laparoscopic gastric surgery. These procedures involved elevating the gastric conduit to the neck through a posterior mediastinal or retrosternal approach and end-to-end anastomosis of the remnant cervical esophagus and fundus of the gastric conduit.
The patients’ clinicopathological features, laboratory data, and treatment strategies were collated from medical records. None of the patients exhibited preoperative clinical signs of infection or systemic inflammatory conditions. Cancer-specific survival (CSS) rates were evaluated with the cause of death determined from case notes or computerized clinical records.
Ethical approval
The retrospective design of this study was approved by the Ethical Review Board committee of Shimane University Faculty of Medicine (Shimane, Japan). Research was conducted in accordance with the 1964 Declaration of Helsinki and its later amendments. All study participants provided written informed consent.
Blood sample analysis
Preoperative complete blood cell (CBC) counts were retrospectively extracted from patient medical records. Only patients for whom preoperative CBC and blood differential data were available were included in this study. All white blood cell (WBC) and differential counts were obtained within 1 week prior to surgery. CBC counts obtained from ethylenediaminetetraacetic acid-treated blood were analyzed using an XE-5000 Automated Hematology Analyzer (Tao Medical Electronics Co., Ltd., Kobe, Japan). Absolute lymphocyte, monocyte, and platelet counts were obtained from the CBC analysis.
Calculation of the LMR, NLR, and PLR
The LMR was calculated by dividing the absolute lymphocyte count by the absolute monocyte count in a routine preoperative blood count. Analysis of the WBC count was performed in the general routine laboratory of our hospital. The NLR was calculated by dividing the absolute neutrophil count by the absolute lymphocyte count in the differential WBC count. The PLR was calculated by dividing the absolute platelet count by the absolute lymphocyte count in the differential count.
Receiver operating characteristic curve analysis was used to determine the optimal cutoff values for the LMR, NLR, and PLR using the statistical software JMP (version 11 for Windows; SAS Institute, Cary, NC, USA). For the LMR, the area under the curve and the optimal cutoff value for the prediction of CSS were 0.69 and 4.0, respectively, with a sensitivity of 62.5% and a specificity of 71.3%. For the NLR, the area under the curve and the optimal cutoff value for the prediction of CSS were 0.58 and 1.6, respectively, with a sensitivity of 57.5% and a specificity of 66.3%. For the PLR, the area under the curve and the optimal cutoff value for the prediction of CSS were 0.65 and 147.0, respectively, with a sensitivity of 59.6% and a specificity of 68.4%. Measurements exceeding the optimal cutoff values were regarded as being high.
Calculation of the IRB score
The IRB score was determined as follows: a high LMR (>4), a high NLR (>1.6), and a low PLR (<147), which were each scored as 1, with all remaining values scored as 0. The scores were added together to produce the IRB score (range: 0–3).
Staging
The pathological classification of the primary tumor, the degree of lymph node involvement, and the presence or absence of organ metastasis were determined according to the TNM classification system.12
Statistical analyses
Mean and standard deviation were calculated, and differences between the study groups were evaluated using the Student’s t-test. Differences between the clinicopathological features were analyzed using a chi-square test. CSS rates were calculated using the Kaplan–Meier method, and differences were assessed using the log-rank test. Prognostic factors associated with a shorter CSS rate were identified using Cox regression analyses.
Univariate analyses were performed to identify variables associated with CSS. Potential prognostic factors of esophageal cancer included age (<70 vs≥70 years), gender (female vs male), pathological TNM stage (I–II vs III), tumor size (<3 vs ≥3 cm), operation time (<600 vs ≥600 min), intraoperative blood loss (<500 vs ≥500 mL), LMR (<4 vs ≥4), NLR (<1.6 vs ≥1.6), PLR (<147 vs ≥147), serum SCC antigen level (<1.5 vs ≥1.5 ng/mL), and IRB score (2–3 vs 0–1). Variables with a P-value of <0.05 in the univariate analyses were included in a multivariate logistic regression analysis.
All statistical analyses were conducted using the JMP software for Windows, version 11. A P-value of <0.05 was considered statistically significant.
Results
Relationships between the LMR, NLR, and PLR, and patients’ clinicopathological features
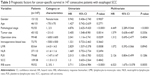
Relationships between the LMR, NLR, and PLR, and the clinicopathological features of 147 consecutive patients with esophageal SCC are presented in Table 1. The LMR was significantly correlated with lymphocyte count (P<0.001), monocyte count (P<0.001), tumor size (P<0.05), tumor depth (P<0.001), and pathological TNM stage (P<0.001). The NLR was significantly correlated with WBC (P<0.05), neutrophil count (P<0.001), lymphocyte count (P<0.001), and tumor depth (P<0.01). The PLR was significantly correlated with lymphocyte count (P<0.001), platelet count (P<0.001), and tumor location (P<0.05). It is notable that the LMR, but not the NLR or PLR, was significantly correlated with a more advanced pathological TNM stage.
Relationships between the IRB score and patients’ clinicopathological features
Relationships between the IRB score and the clinicopathological features of 147 consecutive patients with esophageal SCC are presented in Table 2. Given that the number of patients with an IRB score of 0 was small, we compared patients with an IRB score of 0–1 with those with an IRB score of 2–3.
The IRB score was significantly correlated with age (P<0.05), lymphocyte count (P<0.001), monocyte count (P<0.01), platelet count (P<0.01), tumor depth (P<0.05), tumor location (P<0.01), LMR (P<0.001), NLR (P<0.001), and PLR (P<0.001). Conversely, however, there was no significant association between the IRB score and the pathological TNM stage.
Prognostic factors for CSS in patients with esophageal SCC
From the univariate analysis, pathological TNM stage (P<0.001), tumor size (P<0.01), operation time (P<0.05), a low LMR (P<0.001), a high PLR (P<0.05), and an IRB score of 2–3 (P<0.001) were identified as significant risk factors for CSS (Table 3). Pathological TNM stage (hazard ratio: 4.449, 95% confidence interval: 2.289–9.044; P<0.001) and an IRB score of 2–3 (hazard ratio: 6.023, 95% confidence interval: 1.675–13.078; P<0.01) were confirmed as independent poor prognostic factors in the multivariate logistic regression analysis (Table 3).
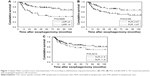
Postoperative CSS according to the LMR, NLR, and PLR in patients with esophageal cancer
Patients with a low vs high LMR (P<0.001; Figure 1A) or a high vs low PLR (P<0.05; Figure 1B) were associated with a significantly poorer CSS rate. Conversely, patients with a low vs high NLR have a slight tendency to be poor prognosis, but no significant differences in CSS rates were observed (P=0.321; Figure 1C).
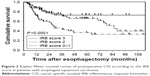
Postoperative CSS according to the IRB score in patients with esophageal cancer
The 5-year CSS rates were 37.8%, 67.8%, and 72.5% for patients with IRB scores of 0–1, 2, and 3, respectively (Figure 2). As determined by Kaplan–Meier analysis and the log-rank test, these differences were statistically significant (P<0.0001).
Discussion
Interest in the host SIR has developed in recent years, owing to its ability to promote angiogenesis, DNA damage-related cancer development, and tumor progression and metastasis by upregulating the expression of proinflammatory cytokines.13,14 Accumulating evidence suggests that host immune responses are important prognostic indicators, and several inflammation-based postoperative prognostic scoring systems have been described.15 Cancer-related inflammation suppresses antitumor immunity through the recruitment of regulatory T cells and the activation of chemokines that result in tumor progression and metastasis.16
In the past decade, a number of studies have confirmed the clinical utility of systemic inflammation-based prognostic scores for predicting postoperative survival in patients with various types of solid tumors.15–17 Although the LMR, NLR, and PLR can predict the prognosis of patients with various types of cancer, their prognostic value and the optimal cutoff points in patients with esophageal cancer remain to be determined.7,10,18 In this study, we generated receiver operating characteristic curves to determine the optimal cutoff values for predicting CSS in patients with esophageal cancer. These were 4.0, 1.6, and 147 for the LMR, NLR, and PLR, respectively. We also evaluated the prognostic significance of the IRB score that incorporated all three ratios in patients with esophageal SCC. These patients did not receive any neoadjuvant or adjuvant therapy, because systemic chemotherapy and radiation therapy may affect systemic inflammation.
In this study, we evaluated the relationships between the LMR, NLR, PLR, and IRB score and various clinicopathological features in patients with esophageal SCC. Univariate analyses identified SIR-related characteristics (eg, the LMR, PLR, and IRB score) and tumor-related characteristics (eg, pathological TNM stage and tumor size) as significant risk factors for CSS. A multivariate logistic regression analysis subsequently confirmed the IRB score and pathological TNM stage as independent poor prognostic factors in these patients. Moreover, Kaplan–Meier analysis using the log-rank test revealed that patients with a preoperative IRB score of 0–1 had a significantly poorer prognosis compared to patients with a preoperative IRB score of 2 and 3 (P<0.0001). Remarkably, the IRB score was unrelated to the levels of classical tumor markers, such as SCC antigen, tumor size, lymph node metastasis, pathological TNM stage, and other tumor characteristics. The levels of conventional tumor markers are not elevated in many patients with esophageal cancer, not even in advanced cases. Therefore, the IRB score could represent an excellent biomarker for the postoperative surveillance of these patients.
Interleukin-6 (IL-6) is a multifunctional inflammatory cytokine that triggers the proliferation and differentiation of a variety of cell types, including immune competent cells and hematopoietic cells. IL-6 induces not only neutrophil proliferation but also the differentiation of megakaryocytes to platelets, and these events are similar to those underlying the SIR.19,20 Theoretically, dynamic changes in the SIR arising from tumor–host interactions are best determined by directly measuring serum IL-6 levels. However, routine assessment of IL-6 levels in cancer patients in a clinical setting is both expensive and inconvenient. The LMR, NLR, and PLR, on the other hand, are based on blood cell components whose levels are regulated by cytokines, most notably IL-6. These blood cell components proliferate and differentiate immediately after inflammatory cytokine release.21 Moreover, the measurement of the LMR, NLR, and PLR is easy, convenient, and cost-effective and, therefore, can be performed routinely. Hence, we assessed the ability of the IRB score to predict the SIR, because IRB score was a novel prognostic system based on the IRBs’ score system that calculates the LMR, NLR, and PLR. Our results demonstrate that the IRB score can predict the SIR as accurately as existing tumor markers and is useful for determining long-term survival outcomes in patients with esophageal cancer.
The limitations of our study include its retrospective, single-institution design, the small sample sizes, and short follow-up durations. We did not observe any changes in terms of IRB score and prognostic features with respect to gender difference in the patients with esophageal SCC, because the total number of female patients was small. In addition, we excluded patients who had received adjuvant chemotherapy and/or radiation therapy. Thus, large prospective randomized controlled trials are needed to confirm our preliminary findings. However, despite these limitations, our study has demonstrated that the preoperative IRB score is a potentially promising independent prognostic factor for CSS in patients undergoing curative resection for esophageal SCC. The IRB score is easy and inexpensive to derive and could facilitate the risk stratification and treatment planning of patients with esophageal cancer undergoing curative thoracoscopic esophagectomy. Further investigation should clarify the relationship with the cytokines, classical tumor marker, and IRB score. In addition, larger prospective studies are still required to elucidate the precise mechanisms that relate IRB score with survival in patients with esophageal cancer. Furthermore, it is important to identify patients who are most at risk of developing postoperative recurrence, which enables us to customize management strategies for individual patients according to the risk of recurrence.
Disclosure
The authors report no conflicts of interest in this work.
References
Colaprico A, Cava C, Bertoli G, Bontempi G, Castiglioni I. Integrative analysis with Monte Carlo cross-validation reveals miRNAs regulating pathways cross-talk in aggressive breast cancer. Biomed Res Int. 2015;2015:831314. | ||
Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004;21(2):137–148. | ||
Hoffmann TK, Dworacki G, Tsukihiro T, et al. Spontaneous apoptosis of circulating T lymphocytes in patients with head and neck cancer and its clinical importance. Clin Cancer Res. 2002;8(8):2553–2562. | ||
Vashist YK, Loos J, Dedow J, et al. Glasgow Prognostic Score is a predictor of perioperative and long-term outcome in patients with only surgically treated esophageal cancer. Ann Surg Oncol. 2011;18(4):1130–1138. | ||
Xiao Y, Ren YK, Cheng HJ, Wang L, Luo SX. Modified Glasgow prognostic score is an independent prognostic factor in patients with cervical cancer undergoing chemoradiotherapy. Int J Clin Exp Pathol. 2015;8(5):5273–5281. | ||
Chenyue Zhang C, Wang H, Ning Z, et al. Prognostic nutritional index serves as a predictive marker of survival and associates with systemic inflammatory response in metastatic intrahepatic cholangiocarcinoma. Onco Targets Ther. 2016;9:6417–6423. | ||
Deng Q, He B, Liu X, et al. Prognostic value of pre-operative inflammatory response biomarkers in gastric cancer patients and the construction of a predictive model. J Transl Med. 2015;13:66. | ||
Huang Y, Feng JF. Low preoperative lymphocyte to monocyte ratio predicts poor cancer-specific survival in patients with esophageal squamous cell carcinoma. Onco Targets Ther. 2015;8:137–145. | ||
Feng JF, Huang Y, Chen QX. A new inflammation index is useful for patients with esophageal squamous cell carcinoma. Onco Targets Ther. 2014;7:1811–1815. | ||
Huang Y, Liu JS, Feng JF. Combination of neutrophil lymphocyte ratio and platelet lymphocyte ratio is a useful predictor of postoperative survival in patients with esophageal squamous cell carcinoma. Onco Targets Ther. 2013;6:1605–1612. | ||
Ying HQ, Deng QW, He BS, et al. The prognostic value of preoperative NLR, d-NLR, PLR and LMR for predicting clinical outcome in surgical colorectal cancer patients. Med Oncol. 2014;31(12):305. | ||
Sobin LH, Gospodarowicz MK, Wittekind C. TNM Classification of Malignant Tumours. 7th ed. New York, NY: John Wiley & Sons; 2011. | ||
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–444. | ||
Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357(9255):539–545. | ||
Hirahara N, Matsubara T, Hayashi H, Takai K, Fujii Y, Tajima Y. Impact of inflammation-based prognostic score on survival after curative thoracoscopic esophagectomy for esophageal cancer. Eur J Surg Oncol. 2015;41(10):1308–1315. | ||
Bhatti I, Peacock O, Lloyd G, Larvin M, Hall RI. Preoperative hematologic markers as independent predictors of prognosis in resected pancreatic ductal adenocarcinoma: neutrophil-lymphocyte versus platelet-lymphocyte ratio. Am J Surg. 2010;200(2):197–203. | ||
McMillan DC. The systemic inflammation-based Glasgow prognostic score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013;39(5):534–540. | ||
Shimada H, Takiguchi N, Kainuma O, et al. High preoperative neutrophil-lymphocyte ratio predicts poor survival in patients with gastric cancer. Gastric Cancer. 2010;13(3):170–176. | ||
Imai T, Koike K, Kubo T, et al. Interleukin-6 supports human megakaryocytic proliferation and differentiation in vitro. Blood. 1991;78(8):1969–1974. | ||
Ruscetti FW. Hematologic effects of interleukin-1 and interleukin-6. Curr Opin Hematol. 1994;1(3):210–215. | ||
Ohsugi Y. Recent advances in immunopathophysiology of interleukin-6: an innovative therapeutic drug, tocilizumab (recombinant humanized anti-human interleukin-6 receptor antibody), unveils the mysterious etiology of immune-mediated inflammatory diseases. Biol Pharm Bull. 2007;30(11):2001–2006. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.