Back to Journals » International Journal of Women's Health » Volume 15
Utilization Status and Perceived Barriers Towards Long-Acting Reversible Contraceptives Among Female Youth College Students in Northern Ethiopia: A Mixed-Methods Study
Authors Weldekiros ME, Tamire M, Berhane A, Gufue ZH , Tesfa FH
Received 4 April 2023
Accepted for publication 11 July 2023
Published 18 July 2023 Volume 2023:15 Pages 1107—1123
DOI https://doi.org/10.2147/IJWH.S413425
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Mulu Eyasu Weldekiros,1 Mulugeta Tamire,2 Adugnaw Berhane,2 Zenawi Hagos Gufue,3 Ferehiwot Hailemariam Tesfa1
1Health Education and Promotion Unit, School of Public Health, College of Health Sciences, Mekelle University, Mekelle, Ethiopia; 2Health Education and Promotion Unit, School of Public Health, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 3Department of Public Health, College of Medicine and Health Sciences, Adigrat University, Adigrat, Ethiopia
Correspondence: Mulu Eyasu Weldekiros, Health Education and Promotion Unit, School of Public Health, College of Health Sciences, Mekelle University, Mekelle, Ethiopia, Email [email protected]
Background: In Ethiopia, teenage sexual activity, unintended pregnancy, and unsafe abortions among youth college students have become the most prevalent public health problems. Contraceptive misuse, low use, and a high unmet need for long-acting reversible contraceptives are attributed to the high rate of unintended pregnancy.
Objective: To assess the utilization status of long-acting reversible contraceptives and to explore the perceived barriers among youth female college students in Mekelle City, Northern Ethiopia, in 2019.
Methods: An institutional-based, concurrent, mixed cross-sectional study with quantitative and qualitative components was conducted among four private and two public colleges in Mekelle City from March 1 to April 30, 2019. A total of 580 female youth college students were included in the quantitative study, and six in-depth and four key informant interviews were conducted for the qualitative study. The quantitative data were analyzed using descriptive statistics, frequency, and percentages. The chi-square test was done to assess the crude association between the outcome variable and independent categorical variables. A p-value of < 0.05 was considered a statistically significant difference. In addition, ATLAS.ti qualitative software version 7.5 was used to code and analyze the qualitative data.
Results: With a 93.8% response rate, 544 female youth college students participated, and 177 (32.5%) were sexually active. Seventy-five (42.3%) of students had a history of pregnancy, and of these, 85% of the pregnancies were unplanned. The utilization of long-acting reversible contraceptives among sexually active college students was 7.3%. Qualitatively, the following themes emerged as perceived barriers to the utilization of long-acting reversible contraceptives: knowledge barriers, fear of side effects, misperceptions, health providers’ approach, discrimination, and poor confidentiality.
Conclusion: This study revealed low utilization of long-acting reversible contraceptives among college students. The findings indicate that college students are at high risk of unintended pregnancy, unsafe abortion, and complications.
Keywords: long-acting reversible contraceptives, youths, college students, utilization status, Mekelle
Introduction
Youth constitute the largest part of the world's population, primarily in low- and middle-income countries.1 Those ages consist of a heterogeneous population with different socio-economic, employment, marital, and educational statuses, unique sexual behaviors, multifaceted reproductive health problems, and family planning needs.2
Globally, youth pregnancy and childbirth complications are the leading cause of death among youths, mainly in low-and middle-income countries. Unintended pregnancy drastically affects the health of children, and it is a risk factor for unsafe abortion and its complications, educational disruption, psychological distress, and poor socioeconomic positions.1,2 Even though preventing unintended pregnancy is crucial, it has been challenging until now. About 67% of unsafe abortions occur among women between 15 and 30 years old in developing countries, and 14% have occurred among younger women less than 20 years old.3
Long-acting reversible contraception (LARC) methods, intrauterine contraceptives, and implants are alternative options for women and are effective and convenient. These methods depend less on user compliance and have lower discontinuation rates than other short-acting methods.4 The long-term nature and effectiveness of LARCs can help young women have children at the right time.1,4
In developing countries, youths aged 15–24 years have the highest proportions of contraceptive non-use or misuse, and as a consequence, 43% of unintended pregnancies resulted from incorrect or inconsistent use of contraceptives.5 One of the factors contributing to unintended pregnancy is related to contraceptive choice. Many women choose methods with higher failure rates, such as oral contraceptives (8.7% failure rate) and condoms (17.4% failure rate with typical use).4 Preventing adolescent pregnancy is a key strategy for improving maternal and infant outcomes.6
In Ethiopia, unintended pregnancy and unsafe abortions among college students have become the most prevalent public health problems.7,8 According to the 2014 Ethiopian demographic health survey report, an estimated 28% of all pregnancies in Ethiopia were unintended.9 Meanwhile, numerous unsafe abortions had been performed by female college students.7 Meanwhile, 26% of sexually active unmarried Ethiopian women have an unmet need for family planning.9
In Ethiopia, 58% of sexually active unmarried women use contraceptives; the most popular methods are injectable (35%) and emergency contraception (4%).9 Studies conducted in Debre Berhan10 and Gondar11 towns showed that 23.4% and 20.4% of sexually active college students were using long-acting reversible contraceptives, respectively. LARCs are highly effective, have minimal side effects, require minimal follow-up, and are low-cost.12 In Ethiopian public health facilities, including the study area, LARCs are provided free of charge, but despite this, their uptake by women is limited in Ethiopia. Numerous studies have been done regarding family planning utilization among married reproductive-age women, but there is limited evidence related to LARC utilization among youth college students, particularly in the study area. Then, this study attempts to assess the utilization level of LARCs and explore the perceived barriers among female youth college students in Mekelle City, Northern Ethiopia.
Methods and Materials
Study Area and Period
The study was conducted in Mekelle City, Tigray Regional State, Northern Ethiopia, located 783 kilometers north of Addis Ababa, the capital city of Ethiopia. The health system in Mekelle City consists of both private and public healthcare facilities. Mekelle has one specialized referral hospital, three general hospitals, eight health centers, and more than seventy-four privately owned health facilities.13 Furthermore, there are five public and ten private colleges in the city. According to the 2007 population census, about 300,000 people were residing in the city; over 51% of the population were women.14 Temporarily, 63% of the total population was under 25 years of age.13 The study was conducted in four private and two public colleges and two purposely-selected non-governmental health facilities for the qualitative part. The study was conducted from March 1 to April 30, 2019.
Quantitative Study
Study Design
An institutional-based concurrent mixed cross-sectional study was conducted.
Study Population
All regular undergraduate female students from the selected private and public colleges of Mekelle City.
Eligibility Criteria
All enrolled regular undergraduate female college students in Mekelle City who were willing to participate in the study were included.
Sample Size Determination and Sampling Procedure
The sample size was determined using a single population proportion formula using Epi Info version 7.2.3.1 software.15 Accordingly, the sample size was calculated with the assumptions that the proportion of utilization of long-acting reversible contraceptives among female college students in Debre Berhan town was 23.4%,10 95% confidence interval, the margin of error was 0.04, and the design effect was 1.5. The sample size was 551. After adding a 5% non-response rate, the final sample size was 580.
Mekelle City owns ten private and five public colleges with different programs, of which 10,262 students were enrolled in the academic year 2018/19 in various academic disciplines. The number of female youth college students was 2500. A multistage sampling technique was used to select the study participants. Accordingly, six colleges were selected using a simple random sampling technique, and departments were selected from each college using a simple random sampling (SRS) technique. The number of study participants selected from each college is proportional to the number of students in each department. Students from the selected departments were also randomly selected in proportion to the size of each department, section, or level from the list of students.
Data Collection Tool and Procedure
A structured questionnaire with closed-ended questions was adapted from reviewing different literature and contextualized to the local circumstances. The first part had socio-demographic and socio-economic variables, and the second part had reproductive characteristics. The research tool was first prepared in English and then translated to the local languages Tigrigna and Amharic and back to English by language translators to realize the consistency and understandability of the language. Four trained degree-holder health professionals participated in data collection.
Operational Definition
Utilization of LARC was defined as ever using intrauterine contraceptive devices (IUCD) or implants. Long-acting reversible contraception was defined as modern contraceptive methods that prevent pregnancy for three or more years and are reversible when stopped.16–18 Sexually active was defined as ever having sexual intercourse. The utilization of long-acting reversible contraceptives was used as an outcome variable, whereas socio-demographic characteristics, reproductive history, social factors, and sources of information were used as explanatory variables.
Data Processing and Analysis
The data collection instrument was coded and checked before entry. The data were entered, cleaned, and analyzed using SPSS version 25. Descriptive data for numeric variables were summarized using the mean and standard deviation, and categorical variables were presented in frequency and percentage. To assess the crude association among the categorical variables, a chi-square test was done. A p-value of less than 0.05 is considered a statistically significant difference.
Qualitative Study
Study Design
A phenomenological study design was employed to explore the day-to-day experience of the barriers that female youth college students are facing while utilizing the LARCs.
Eligibility Criteria
Non-governmental clinics that provide sexual and reproductive health services were purposefully identified.
Sample Size and Sampling Procedure
The sample size was determined based on idea saturation. Health professionals for the key informant interview in the selected clinics were selected using a criteria-based purposive sampling technique to obtain an in-depth and yet informed range of perspectives. We identified health professionals who were most closely involved in the provision of sexual and reproductive health services for youth to take part in the key informant interview. Potential participants were asked for their willingness to participate, and verbal informed consent was obtained from all participants. In the interview, healthcare providers were asked to draw on their clinical experience with youth college students at their current organization as well as any previous sexual and reproductive health roles. Six of the interviews were held with health professionals who provide abortion and family planning services.
In-Depth Interview Participants’ Selection Procedure
Female college students were recruited using criteria-based purposive sampling techniques through service providers (KIIs). College students who visit those clinics to receive sexual and reproductive health services were selected. To be eligible for the interview, those college students needed to be young and sexually active. During recruitment, students were verbally informed about the aim of the study and participants’ confidentiality regarding the information they gave. The principal investigator then only invited the female youth student if she was willing and able to give informed consent to participate in the research. Verbal informed consent was received at the time of the interview, and female youth college students were asked about their awareness, attitudes, and risk factors for unintended pregnancy and obstacles to using LARCs.
Data Collection Tool and Procedure
A semi-structured interview guide was prepared for both in-depth interviews and key informant interviews to explore the perceived barriers to LARC methods use. The number of IDIs and KIIs for the qualitative study were determined by information saturation. The principal investigator, with the help of the note-taker, carried out the data collection process, and the interviews were tape-recorded, transcribed, and translated on the same day of the interview.
Data Analysis and Processing
The audio-recorded data was transcribed verbatim, translated, and imported into ATLAS.ti qualitative data analysis software version 7.5 for coding and analysis. Field notes are linked to respective files to assist in analysis. The principal investigator openly coded the data; similar codes were systematically categorized, and unique themes emerged. The data from college students were compared with the data from healthcare professionals, taking careful note of differences and commonalities in themes between the responses of college students and healthcare providers.
Ethics Approval
The study received approval from the institutional review board of the School of Public Health, Addis Ababa University (Ref: SPH/020/2019). Following the receipt of a letter of cooperation from each chosen college and its corresponding departments, the participants in the study were told of its purpose and allowed to give their written informed consent. Those participants who were younger than 18 years old had received parental informed consent. The study complies with the 1964 Declaration of Helsinki, and all participants were made aware of the publication of an anonymous response.
Result
Socio-demographic characteristics
Five hundred forty-four students participated in the study, with a 93.8% response rate. The age of participants was between 16 and 24 years, with a mean (±SD) age of 19.67±1.9 years. Furthermore, 204 (37.5%) participants were first-year students. The great majority of participants, 502 (92.3%), were single in marital status (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Female College Students in Mekelle City, Tigray, Ethiopia, 2019 (n = 544) |
Reproductive Characteristics of Participants
Of the study participants, 177 (32.5%) were sexually active. The mean (±SD) age at first sexual intercourse was 17.1±1.14 with a minimum of 15 and a maximum of 20 years. Among the sexually active students, 75 (13.8%) of them had a history of pregnancy, with the mean (±SD) age at first pregnancy 17.7±1.1 years. Among the pregnancies, 64 (85.7%) were unintended, and 40 (53.3%) ended in abortion (Table 2).
 |
Table 2 Reproductive History of Female College Students in Mekelle City, Northern Ethiopia, 2019 (n = 544) |
Awareness of Female College Students About Contraceptives
Four hundred forty-five (81.8) students had heard of contraceptives; among those, 430 (96.4%) had heard of short-acting modern contraceptives. Additionally, condoms were mostly reported by 380 (88.4%) students, followed by emergency contraceptives by 345 (80.2%). Moreover, 325 (73%) participants have heard of LARC methods, and an implant was mentioned mostly (98.5%). Meanwhile, among the study participants, 117 (36.6%) and 92 (34.3%) of them had information that immediate pregnancy can happen after the removal of the implant and IUCD, respectively (Table 3). According to the college students, 194 (27.8%) and 158 (22.5%) of them cited television and healthcare practitioners as their primary information sources, respectively (Figure 1).
 |
Table 3 Awareness of Female College Students About Contraceptives in Mekelle City, Northern Ethiopia, 2019 (n = 544) |
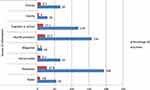 |
Figure 1 Source of information about modern contraceptives, Mekelle, Northern Ethiopia, 2019. |
Factors Associated with Long-Acting Reversible Contraceptive Use
There is no statistically significant difference between the socio-demographic characteristics of participants and LARC utilization except marital status (χ2 = 7.9, df=2, p=0.01). Meanwhile, knowing about the occurrence of immediate pregnancy after removal of IUCD, (χ2= 4.1, df=1, p=0.049), ever using short-acting modern contraceptives (χ2= 4.5, df=1, p=0.035), using television as a source of information (χ2 = 5.6, df=1, p=0.04) and ever encountering planned pregnancy (χ2=7.9, df=1, p=0.043) had a significant difference in the utilization of LARC methods among female college students (Table 2). Whereas, there is no significant difference in living conditions (χ2 = 2.8, df=1, p=0.09), the educational year (χ2 = 0.9, df=1, p=0.75), and partner’s occupation (χ2 = 0.9, df=1, p=0.48) of college girls with the utilization of LARC methods (Table 4).
 |
Table 4 Association of Long-Acting Reversible Contraceptive Utilization with Different Characteristics of Female College Students in Mekelle City, Northern Ethiopia, 2019 (n = 159) |
Result of the Qualitative Part
Four key informant interviews (KII) and six in-depth interviews (IDI) were conducted with purposefully selected participants. The age of the students ranged from 18 to 22 years, and each interview lasted 35 to 90 minutes. The findings are described using themes and sub-themes with continuous text and quotations to support the perceived barriers detailed in further discussion. The themes are, (1) Knowledge barriers; (2) Fear of side effects; (3) Misconceptions; (4) Health providers’ approaches; and (5) Access barriers. The characteristics of participants for the IDI and KIIs were their gender, age, work experience, college year, health institution, or college status (Table 5).
 |
Table 5 Characteristics of Study Participants in the Key Informant and in-Depth Interviews in Mekelle City, Northern Ethiopia, 2019 (n = 10) |
Theme 1: Knowledge Barriers
Poor Knowledge About LARCs
The interview revealed that sexually active female college students were unable to make informed choices due to limited knowledge about LARCs. The participants noted that there is a lack of knowledge and inadequate awareness among college girls. In addition, the service providers mentioned that there are students who do not know what alternative contraceptives are available. This can be the result of the culture that existed in the community because those youths are growing up in a social context in which open discussion about sexual issues is illicit. As a result, the tendency to use LARCs among the 18–24 age groups are almost nonexistent, and there is no trend to know or ask people about modern contraceptives. One student expresses that,
Most college girls who visit our clinic for abortion service said that ‘we heard that LARCs belong to old women only. (KII 1)
A college girl participant mentioned that “…I was 16 when I had sex for the first time. I knew nothing about contraceptives, but after a few days, my boyfriend brought me a tablet and asked me to take it to be safe from pregnancy. After a month, my menstruation stopped. I was so confused and stressed. When I checked up, I got pregnant. That was the worst experience of my life”. (IDI 1)
Parent-to-Child Communication
Healthcare providers stated that poor parent-to-child communication has implications. As they said, some girls put all the contraceptive pill tablets in a plastic tablet bag to convince their families that they were using contraceptives.
…because in our cultural context, youth unmarried girls have no freedom to ask their family any word about sexual and contraceptive issues. For this reason, they may prefer to use short-acting contraceptives secretly…. (KII-1)
Theme-2: Fear of Side Effects
Side Effects
Participants mentioned that side effects are the main reason that deters female college students from using LARC methods. KII participants noted that the possibility of side effects resulting from LARC use contributes to a lack of interest in utilizing them, and there is a weakness among service providers in informing LARC women who are in need about the real side effects of modern contraceptives.
…Actually, health professionals are unconcerned in informing youths about the importance and side effects of modern contraceptives, we just assumed that youths knew about them…. KII-1
The most common side effects expressed by respondents were bleeding, gastritis, depression, and weight gain. A few students also cited hair damage, headaches, and melasma. The college girl said,
I have an implant on my arms for three years. But as you see my face it brings me melasma, that is why I am here to remove it. (IDI-1)
Visibility Concern
Healthcare providers noted the visibility of implants on arms as a possible barrier to LARC use. College girls feel comfortable when they are secure from any visible item in their bodies. They do not want their parents to recognize them as sexually active.
Students hate the visibility of implants on arms because they want to wear shorts. (KII-3)
I remember a girl saying, ‘I would like to use an implant until I finish my education, but I am very close to my brother. When he knew that I had it on my arm, he may have tended to kill me if it was too hard for me. (KII-3)
Theme-3: Misconceptions About LARCs
Misperceptions
Participant students mentioned that receiving mistaken information and bad narratives about LARCs from elders closest to them hinders LARC use among youths. Meanwhile, participant health providers also reported that because LARCs do have side effects, such as vaginal bleeding, the perception of students is that youths help their communities by frequently spreading incorrect information about LARCs. The misperception that IUCD causes cervical cancer was college girls’ most common negative sentiment. Meanwhile, IUCD accumulates blood in the abdomen and moves to the heart, and the implant fuses into the muscle. Having any external material in the body is considered a sin, according to some participants’ misperceptions.
A student participant reported her friend’s experience,
“My friend had an IUCD some years ago while she was living in Jidda”. As she told me; she got ill for a long time, went to holy water, and then the IUCD was found in her heart, as she told me. So how can I use them? “It is terrible”. (IDI-3)
Similarly, KII participants reported that youths perceived having IUCD or implants in their bodies as a sin.
I recall a college girl who tried to remove an implant herself with a sharp stone; later, she came to our clinic for professional help, and when I asked her why she tried to remove it herself, she said, “I went to holy water, and I heard that no one cannot be blessed when we wash holy water while we have implants in the body”. So, I tried to remove it. (KII-3)
Fertility Concerns
The main concern cited by participants was that LARC methods would render a woman infertile. In many cases, this can prevent youth from using LARCs. One college student mentioned that getting pregnant is considered a warrant for her future fertility, so she should get pregnant and abort rather than be safe from pregnancy. She considered it an experiment because she was a fertile woman. As she says,
“To tell you the truth, though I have aborted many times, having a pregnancy makes me hopeful”. That is a merit for me to think that I can have a child in the future. Because I experience that, I can be pregnant. Nevertheless, when you have an implant or IUCD in your body, you never become pregnant, as I heard. “For that reason, I am afraid of having them”. (IDI-2)
Theme-4: Health Providers’ Approach
Discrimination
Student participants reported that they faced discrimination by health professionals when they accessed family planning services, as FP was generally thought to be only for adults and married women. As they stated, there are health providers who do not treat young girls who want sexual and reproductive health services as equally as married women do; rather, they treat them as secondary customers.
“The nurses didn’t listen to us; they blamed us for our mistakes”. They are not willing to give a chance to an unmarried girl who wants family planning services. “They don’t care about the reason behind it”. (IDI-2)
In addition, KII participants noted that there is a need to work on and give emphasis to health providers’ service delivery approaches since there is unequal treatment of clients, especially at governmental health facilities. KII-2 indicated,
“There are health providers who stigmatize young girls who want to use LARCs before marriage. Healthcare providers are not doing a good enough job of disseminating relevant information”. Some health workers themselves don’t believe in LARCs for college students. (KII-1)
“Every woman has the right to know all the information about each modern contraceptive. Most health providers who give FP services for youths, especially at government health facilities, are not well trained or they do not know well about the services they deliver”. (KII-1)
The key informants noted that, though in most health institutions YFS has been introduced, there is a need to improve the system because the health providers who place youth in YFS are at an unmatched age with the service takers (youth). Therefore, it is difficult for youths to express their feelings, and the service providers might not understand the youth girls’ feelings. Now there is a lack of open discussion between health providers and clients, so youths cannot say what they think.
“There is no special center for youths in all health facilities; all kinds of alternatives should be in place for youth college students”. (KII-2)
Mostly the nurses in government health facilities are not early adopters for new technology; rather, they follow the old trend they had before. (KII-1)
Poor Confidentiality
Moreover, college students showed that health providers’ poor confidentiality was a reason for them not to use LARCs. In addition, KIIs noted that female college students are exposed to unintended pregnancy due to the nonuse or misuse of contraceptives, because they do not trust the information and secrecy of health providers.
Some nurses talk to others about patients, particularly unmarried young girls or students, and they gossip about their clients outside of a health facility. (IDI-2)
Youths have no confidence in health providers’ information and skill. (KII-1)
Theme-5: Access Barriers
Cost
The KII respondents mentioned cost as a barrier to the LARC methods’ use; college students may not have a source of income since; they rely on their families for their expenses. For this reason, when they need LARCs, they prefer to go to non-governmental clinics for privacy, but there is payment for the insertion and removal of both IUCDs and implants in non-governmental clinics. Therefore, this might be a big challenge for them.
In our clinic, they are expected to pay 40 and 70 birrs for insertion and removal, respectively. So, for the student, even 5 birrs is too much to pay. (KII-3)
Meanwhile, the health care providers mentioned as the reason for the payment have a sustainability issue, but students argue with this payment as it is too costly for them.
Time
On the other hand, students reported that there is a problem with the long waiting time to get to the service providers. In addition, they noted that the commodities of LARCs are not easily available and that counseling takes longer.
In governmental health facilities, nurses have excess tea time; when you go to a health center, you always wait for hours to get service; it is so tedious. (IDI-1)
Discussion
This study aimed to assess the utilization of long-acting reversible contraceptive methods and explore the perceived barriers among female college students in Mekelle City. The current utilization level of LARC among sexually active female students in this study was 7.3%, similar to a study conducted in Nigeria, which was 10.6% among secondary institution students.19 But the finding was relatively lower compared to study reports done in other parts of Ethiopia, such as Debrebrhan10 and Gondar,11 which were conducted among college students. The reason for this difference might be due to the difference in socio-demographic factors related to the study settings.
Similarly, the study finding of the current study was lower than a study report from Mekelle,20 Harar,21 Nekemte,22 and Uganda23 conducted among reproductive-age women. A possible reason might be the difference in age and marital status. The current study’s participants were youth college students, so maybe they are embarrassed about accessing contraceptives freely. Being young and unmarried might deter them from using LARCs more than married women. Again, the result of this study was lower than the findings from Mexico, which were conducted among adolescents.24 The reason for this difference might be due to the difference in socio-demographic and cultural factors related to the study settings and access to FP services and information.
Among students who used LARC methods, a large proportion of them used implants (84.6%), and 15.4% of them used IUCD. This finding agrees with other studies’ reports that the majority of their respondents used implants.10,11,20 In contrast, a study report from Nigeria showed IUCD was mostly used (60%) for the LARC method.19 The lower rate of IUCD utilization among college students compared to other areas and countries might be explained due to religious and cultural norms.
In developing countries, girls are not expected to have sexual intercourse before marriage.25 For this reason, disclosing private parts to healthcare providers might be difficult for those students. Another reason might be misconceptions about LARCs heard in the community. Qualitatively, the current study found that misconceptions associated with IUCD, such as the fact that it causes cancer, accumulates blood in the abdomen, moves to the head and heart, and involves implants such as implants fused into the muscle, were mentioned as barriers to the use of LARC methods. In Ghana, a study on the myths and misconceptions surrounding IUCD use revealed discomfort after insertion, the male partner feeling it during sex, IUDs breeding infections, and the idea that IUCD can harm the womb.26
Early sexual initiation and low modern contraceptive uptake contribute to teenage unwanted pregnancy and abortion.9 The current study shows that 177 (32.5%) college students were sexually active. Similar findings were noted by studies from Gondar11 (38%) and Nigeria19 (34.5%), but, this finding is slightly greater than a study report from Debre Berhan,10 which was 26%. This difference might be due to socio-cultural differences among the study settings. Meanwhile, this report is less than a study from Uganda, where 51% of female university students were sexually active.27 This difference might be due to the difference in place and population. The study participants in the current study were college girls, whereas the participants in Uganda were university students. So, living on campus may expose university students to sexual intercourse more than college girls.
In the current study, the mean age at first sexual intercourse was found to be 17 years. Similar findings were reported from Debre Berhan,10 Gondar,11 Nigeria,19 and Uganda,27 which were in the age range of 15–19 years. Similarly, the EDHS report showed that the median age at first sexual intercourse among reproductive-age women is 16.6 years, and 62% of women have their first sex before the age of 18 years.9 This emphasizes an important period for the timing of sexual and reproductive health education, including LARCs, which are the most effective and safe methods of modern contraceptives.
Our study points out that among sexually active students, 75 (13.8%) had encountered pregnancy, with a mean age of first pregnancy of 17 years old. This result is almost similar to a finding from Debre Berhan (10.8%).10 This finding is less than a study report from Gondar (24%).11 However, the finding is slightly greater than a study result from Uganda, which was 9%.27 This difference might be due to the differences in access to information and contraceptive services among the study settings. Meanwhile, in the current study, 85% of those pregnancies were unintended; this result is consistent with findings from Gondar11 and Addis Ababa University,28 which were 84.8% and 95%, respectively. However, the finding is greater than a study report from Tanzania (27%).29 This difference might be due to the access and use of effective contraceptive methods in the study settings.
The current study revealed that 40 (53%) pregnancies ended in abortion. This finding is in line with a study report from the 2016 EDHS report, 54%.9 However, the finding is lower than the finding from Gondar (75%).11 However, it was slightly greater than a study report from Arbaminc7 and Debre Berhan10 (43% and 33%, respectively). The possible explanation for the observed differences might be the difference in the study setting. Meanwhile, the result is significantly greater than a finding from Gondar 4%, conducted among women of the reproductive age group.30 A possible reason might be due to economic reasons or marital relationships. Youth college girls were more likely to commit induced abortions than older ones because college students become economically dependent, are in unstable marital relationships, and have not completed their education.
In the current study, television was the main source of information. This result is different from the reports from Debre Berhan,10 Tanzania29 and Mekelle31 in which healthcare providers, public institutions, and friends, respectively, were the main sources of information. This difference might be because of the difference in access to media and health providers’ approaches or counseling skills. The other possible reason might be the difference in age categories. This implies that choosing appropriate channels to deliver health messages to youths related to modern contraceptives might help improve LARC methods use among college students.
Regarding factors associated with marital status, there is a significant difference in the utilization of LARC methods among college female students. This finding is consistent with a study report from Gondar,11 in which marital status was found to be a significant factor in LARC, and a study from Uganda, which found that the prevalence of modern contraceptives was higher among married students.27 Similarly, a study from South Africa showed that marital status was associated with current modern contraceptive use among university students.32 The reason for this might be that married students are exposed to risky sexual encounters, and pregnancy is next door. Therefore, to protect themselves from unplanned pregnancies, especially when they are students, they search for something that keeps them safe. Therefore, LARC methods might be their primary choice.
Findings from the qualitative part of the current study may support this, which shows that unequal treatment and poor confidentiality of health providers are reasons for unmarried college students not to use LARCs. In some cases, as the interview found, there are health providers who do not treat young unmarried girls who want sexual and reproductive health services as equally as married women do; rather, they treat them as secondary customers.
In the developing world, women are not fully authorized and are economically dependent. As a result, partners’ occupations might be a significant factor in LARC use. Women who are economically dependent on their partners might not have the chance to exercise their rights to contraceptive choice. However, this variable was not found to be a significant factor in the current study. In contrast, a study report from Myanmar conducted among married young women revealed that young wives with income were more likely to use modern contraceptives.33 Moreover, an educational year might also be another significant factor that influences LARC use among college girls. As the educational year increases, contraception knowledge and use also increase. However, this variable was not found to be a significant factor in our study. On the contrary, a study report from Uganda showed that the educational year was significantly associated with contraceptive use among university students.27
In the qualitative result of the current study, there was a consensus between youth college students and healthcare providers on the barriers to LARC usage. These barriers included poor knowledge, fear of side effects, concern about visibility, poor health providers’ skills, misconceptions, beliefs, and norms. Overall, those findings were consistent with other literature that has reported that limited knowledge of LARC, familiarity with and normality of OCPs, fear of side effects, and health providers’ knowledge and skill were the major barriers to LARC use.34–37
The finding that poor knowledge prevents college students from using LARC is in line with study reports from Debrebrhan10 and Scotland34 However, this finding was not supported by a study report from Kenya35 among young women, and Uganda27 among university students, which confirms that awareness and knowledge of modern contraceptives do not necessarily translate to the use of contraceptives. This difference might be due to access to reliable information and cultural contexts in the study settings. Moreover, misconceptions and wrong beliefs were also the main barriers to LARC method uptake; this result is similar to study findings from Ghana37 and Zambia.38 The literature revealed that many fears based on myths and misconceptions were formed due to both true side effects and myths learned from their society.
Social stigma and health providers’ bad attitudes are cited by college students as deterrents to their use of LARCs. According to a study report from Zambia, adolescents are unable to utilize contraceptives due to the unfavorable views of healthcare professionals and the possibility that others in the community may find out about their sexual activity. Thus, both adolescents and unmarried users reported being stigmatized when they accessed family planning and contraceptive services, as family planning was normally assumed to be only for adult married women.38
Poor counseling skills among health providers are also mentioned as one reason that prevents college students from using LARC. The KIIs mentioned that most of the time communication in service provision is one-way, but HP should ask the user to check the clarity of the information you provide. After we provide her with the necessary information, she has the full right to choose whatever she likes. This finding was supported by study reports from Jimma that revealed that feeling bored with counseling and the lack of counseling skills of health providers (need-based, privacy, confidentiality, and interaction) were noted as barriers to LARC use among married women.39
Pregnancy as a warranty for fertility was an emerging theme in our study. Some college students perceive getting pregnant as a license for their future fertility, so it is better to get pregnant and abort than be safe from pregnancy. This result is supported by the finding from Nigeria, which showed adolescents’ decision to rely on induced abortion was based on fear of future infertility resulting from adverse side effects of using modern contraceptives other than condoms.40 The possible reason for this misperception might be that we do not know enough about the mechanism of action of modern contraceptives and the side effects of induced abortion. Unsafe abortion is often the result of an unwanted pregnancy resulting from contraceptive non-use or misuse. This trend is most profoundly demonstrated by youth who are single or in school.30 This indicates the need to educate youths about modern contraceptives’ mechanisms of action and the side effects of induced abortion.
Strengths and Limitations of the Study
The study attempts to triangulate the findings qualitatively to explore the depth of perceived barriers that hinder the utilization of LARC methods from the participant’s and service providers’ perspectives. Since the study was institutional-based and the participants were college students, the findings may not be representative of the general youth of Mekelle City. In addition, the quantitative findings were based on the self-report, so it is difficult to prove that the students provided honest answers to these questions. Besides, since there was a very small distribution of outcome variables, we could not apply multivariable logistic regression to identify the strength of associated factors toward LARC utilization among youth college students.
Conclusions
The finding revealed low utilization of LARCs among female youth college students. Qualitatively, some barriers to LARC use were identified. Moreover, the qualitative finding indicates that college students are at high risk of unintended pregnancy, induced abortion, STIs, and HIV/AIDS. Thus, sexual and reproductive health education programs in school are needed for college students. Desirable health providers’ capacity building to improve their skills and approach is required. In addition, healthcare workers and programmers need to scale up awareness-creation programs to change misconceptions and wrong beliefs.
Data Sharing Statement
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
Patient and Public Involvement
Patients and/or the public were not involved in the design, conduct, reporting, or dissemination plans of this research.
Acknowledgments
The authors thank all involved students and healthcare providers who took the time to complete the survey.
Author Contributions
All authors made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed on the journal to which the article will be submitted, gave final approval of the version to be published; and agreed to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. The Health Communication Capacity Collaborative (HC3). Barriers to LARC uptake among youth: highlights from the research. The United States agency for international development; 2014. Available from: https://healthcommcapacity.org/wp-content/uploads/2015/04/Barriers-to-LARC-Uptake-Among-Youth-Brief.pdf.
2. The World Health Organization. Adolescent and young adult health. Geneva, Switzerland: World Health Organization; 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions.
3. Shah I, Ahman E. Age patterns of unsafe abortion in developing country regions. Reprod Health Matters. 2004;12(24 Suppl):9–17. doi:10.1016/S0968-8080(04)24002-2
4. Spies EL, Askelson NM, Gelman E, Losch M. Young women’s knowledge, attitudes, and behaviors related to long-acting reversible contraceptives. Womens Health Issues. 2010;20(6):394–399. doi:10.1016/j.whi.2010.07.005
5. Kavanaugh ML, Jerman J, Ethier K, Moskosky S. Meeting the contraceptive needs of teens and young adults: youth-friendly and long-acting reversible contraceptive services in U.S. family planning facilities. J Adolesc Health. 2013;52(3):284–292. doi:10.1016/j.jadohealth.2012.10.276
6. Chandra-Mouli V, McCarraher DR, Phillips SJ, Williamson NE, Hainsworth G. Contraception for adolescents in low and middle income countries: needs, barriers, and access. Reprod Health. 2014;11(1):1. doi:10.1186/1742-4755-11-1
7. Animaw W, Bogale B. Abortion in university and college female students of Arba Minch town, Ethiopia, 2011. Sex Reprod Healthc. 2014;5(1):17–22. doi:10.1016/j.srhc.2013.12.001
8. Nigatu DT, Seme A, Fituma S, Segni MT. Sexual initiation and associated factors among young women in West Shoa, Ambo Town, Ethiopia: a community-based cross-sectional study. BMC Womens Health. 2018;18(1):76. doi:10.1186/s12905-018-0563-7
9. Central Statistical Agency, Ethiopia and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2016.
10. Birhane K, Tsegaye W, Mulaw A, et al. Utilization of long acting reversible contraceptive methods and associated factors among female college students in Debre Berhan Town, Ethiopia. Adv Appl Sci. 2016;1(1):18–23.
11. Aregay W, Azale T, Sisay M, Gonete KA. Utilization of long acting reversible contraceptive methods and associated factors among female college students in Gondar town, northwest Ethiopia, 2018: institutional based cross-sectional study. BMC Res Notes. 2018;11(1):862. doi:10.1186/s13104-018-3971-8
12. Winner B, Peipert JF, Zhao Q, et al. Effectiveness of long-acting reversible contraception. N Engl J Med. 2012;366(21):1998–2007. doi:10.1056/NEJMoa1110855
13. Giorgi G, Krishnan K Health needs assessment for Mekelle City, Ethiopia. MCI social sector working paper series report number 6; 2009.
14. Population Census Commission. Summary and Statistical Report of 2007 Population and Housing Census. Addis Ababa, Ethiopia: Population Census Commission; 2008.
15. Center for Disease Control and Prevention. Epi Info, a Database and Statistics Program for Public Health Professionals. Atlanta, Georgia, USA: Center for Disease Control and Prevention; 2018.
16. Peipert JF, Zhao Q, Allsworth JE, et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011;117(5):1105–1113. doi:10.1097/AOG.0b013e31821188ad
17. Pearson S, Boerma CJ, McNamee K, Bateson D. Long-acting reversible contraceptives: new evidence to support clinical practice. Aust J Gen Pract. 2022;51(4):246–252. doi:10.31128/AJGP-03-21-5908
18. Committee on Practice Bulletins-Gynecology, Long-Acting Reversible Contraception Work Group. Practice bulletin no. 186: long-acting reversible contraception: implants and intrauterine devices. Obstet Gynecol. 2017;130(5):e251–e269. doi:10.1097/AOG.0000000000002400
19. Eke AC, Alabi-Isama L. Long-acting reversible contraception (LARC) use among adolescent females in secondary institutions in Nnewi, Nigeria. J Obstet Gynaecol. 2011;31(2):164–168. doi:10.3109/01443615.2010.539720
20. Alemayehu M, Belachew T, Tilahun T. Factors associated with utilization of long acting and permanent contraceptive methods among married women of reproductive age in Mekelle town, Tigray region, north Ethiopia. BMC Pregnancy Childbirth. 2012;12:6. doi:10.1186/1471-2393-12-6
21. Shiferaw K, Musa A. Assessment of utilization of long acting reversible contraceptive and associated factors among women of reproductive age in Harar City, Ethiopia. Pan Afr Med J. 2017;28:222. doi:10.11604/pamj.2017.28.222.13475
22. Melka AS, Tekelab T, Wirtu D. Determinants of long acting and permanent contraceptive methods utilization among married women of reproductive age groups in western Ethiopia: a cross-sectional study. Pan Afr Med J. 2015;21:246. doi:10.11604/pamj.2015.21.246.5835
23. Anguzu R, Tweheyo R, Sekandi JN, et al. Knowledge and attitudes towards use of long acting reversible contraceptives among women of reproductive age in Lubaga division, Kampala district, Uganda. BMC Res Notes. 2014;7:153. doi:10.1186/1756-0500-7-153
24. Saavedra-Avendano B, Andrade-Romo Z, Rodriguez MI, Darney BG. Adolescents and long-acting reversible contraception: lessons from Mexico. Matern Child Health J. 2017;21(9):1724–1733. doi:10.1007/s10995-016-2013-1
25. Bearinger LH, Sieving RE, Ferguson J, Sharma V. Global perspectives on the sexual and reproductive health of adolescents: patterns, prevention, and potential. Lancet. 2007;369(9568):1220–1231. doi:10.1016/S0140-6736(07)60367-5
26. Lamptey E, Okunlola MA, Oladokun A. Myths and misconceptions about intrauterine devices: impact on usage. Sci Med J. 2020;2(4):212–218. doi:10.28991/SciMedJ-2020-0204-3
27. Nsubuga H, Sekandi JN, Sempeera H, Makumbi FE. Contraceptive use, knowledge, attitude, perceptions and sexual behavior among female University students in Uganda: a cross-sectional survey. BMC Womens Health. 2016;16:6. doi:10.1186/s12905-016-0286-6
28. Tamire W, Enqueselassie F. Knowledge, attitude, and practice on emergency contraceptives among female university students in Addis Ababa, Ethiopia. Ethiop J Health Dev. 2007;21(2):111–116. doi:10.4314/ejhd.v21i2.10037
29. Somba MJ, Mbonile M, Obure J, Mahande MJ. Sexual behaviour, contraceptive knowledge and use among female undergraduates’ students of Muhimbili and Dar es Salaam Universities, Tanzania: a cross-sectional study. BMC Womens Health. 2014;14:94. doi:10.1186/1472-6874-14-94
30. Oumer M, Manaye A. Prevalence and associated factors of induced abortion among women of reproductive age group in Gondar Town, Northwest Ethiopia. Sci J Public Health. 2019;7(3):66–73. doi:10.11648/j.sjph.20190703.11
31. Gebremichael H, Haile F, Dessie A, Birhane A, Alemayehu M, Yebyo H. Acceptance of long acting contraceptive methods and associated factors among women in Mekelle City, Northern Ethiopia. Sci J Public Health. 2014;2(4):349–355. doi:10.11648/j.sjph.20140204.27
32. Akintade OL, Pengpid S, Peltzer K. Awareness and use of and barriers to family planning services among female university students in Lesotho. S Afr J Obstet Gynaecol. 2011;17(3):72–78.
33. Mon MM, Liabsuetrakul T. Predictors of contraceptive use among married youths and their husbands in a rural area of Myanmar. Asia Pac J Public Health. 2012;24(1):151–160. doi:10.1177/1010539510381918
34. Glasier A, Scorer J, Bigrigg A. Attitudes of women in Scotland to contraception: a qualitative study to explore the acceptability of long-acting methods. J Fam Plann Reprod Health Care. 2008;34(4):213–217. doi:10.1783/147118908786000497
35. Ochako R, Mbondo M, Aloo S, et al. Barriers to modern contraceptive methods uptake among young women in Kenya: a qualitative study. BMC Public Health. 2015;15:118. doi:10.1186/s12889-015-1483-1
36. Okpo E, Allerton L, Brechin S. ‘But you can’t reverse a hysterectomy!’ Perceptions of long acting reversible contraception (LARC) among young women aged 16–24 years: a qualitative study. Public Health. 2014;128(10):934–939. doi:10.1016/j.puhe.2014.08.012
37. Hindin MJ, McGough LJ, Adanu RM. Misperceptions, misinformation and myths about modern contraceptive use in Ghana. J Fam Plann Reprod Health Care. 2014;40(1):30–35. doi:10.1136/jfprhc-2012-100464
38. Silumbwe A, Nkole T, Munakampe MN, et al. Community and health systems barriers and enablers to family planning and contraceptive services provision and use in Kabwe District, Zambia. BMC Health Serv Res. 2018;18(1):390. doi:10.1186/s12913-018-3136-4
39. Tebeje B, Workneh D. Prevalence, perceptions and factors contributing to long acting reversible contraception use among family planning clients, Jimma Town, Oromiya Region, South-West Ethiopia. J Womens Health Care. 2017;6(1):351.
40. Otoide VO, Oronsaye F, Okonofua FE. Why Nigerian adolescents seek abortion rather than contraception: evidence from focus-group discussions. Int Fam Plan Perspect. 2001;27(2):77–81. doi:10.2307/2673818
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
