Back to Journals » International Journal of General Medicine » Volume 16
Utilization of HIV Pre-exposure Prophylaxis and Associated Factors Among Female Sex Workers in Bahir Dar City, North-West Ethiopia, Cross-sectional Study, 2022
Authors Ademe B, Bogale EK , Anagaw TF
Received 17 October 2023
Accepted for publication 13 December 2023
Published 21 December 2023 Volume 2023:16 Pages 6015—6024
DOI https://doi.org/10.2147/IJGM.S443477
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mihajlo Jakovljevic
Bezza Ademe,1 Eyob Ketema Bogale,2 Tadele Fentabil Anagaw2
1Department of Nursing, Tibebe Ghion Specialized Hospital, Bahir Dar University, Bahir Dar, Ethiopia; 2Department of Health Promotion and Behavioral Science, School of Public Health, College of Medicine and Health Science, Bahir Dar University, Bahir Dar, Ethiopia
Correspondence: Tadele Fentabil Anagaw, Department of Health Promotion and Behavioral Science, School of Public Health, College of Medicine and Health Science, Bahir Dar University, PoBox:079, Bahir Dar, Ethiopia, Tel +251-927692916, Email [email protected]
Objective: This study aimed to assess the utilization of HIV pre-exposure prophylaxis and associated factors among commercial female sex workers in Bahir Dar City, Northwest Ethiopia, in 2022.
Methods: An institution-based cross-sectional study was conducted in Bahir Dar City from November 1 to 30, 2022. The random sampling technique was used to select 396 commercial female sex workers. Kobo Collector was used to gather the data, which was then exported to STATA 14 for analysis. In bivariate regression analysis, all variables with a P-value of < 0.2 were entered into multivariable logistic regression. Multivariable logistic regression variables with P-values ≤ 0.05 at a 95% confidence interval were declared to be significantly linked with the utilization of HIV pre-exposure prophylaxis.
Results: In this study, 183 (46.2%) (95%CI: 41.33– 51.16) of respondents utilized HIV pre-exposure prophylaxis. Educational status: secondary and above (AOR: 2.18, 95%CI: 1.05– 4.53). Age of sex workers 26– 36 (AOR: 0.20, 95%CI: 0.17– 0.84); experience of sex work 3– 5 years (AOR: 0.25, 95%CI: 0.24– 0.83); and having good knowledge (AOR: 4.98, 95%CI: 3.90– 10.65) were significantly associated with the utilization of HIV pre-exposure prophylaxis.
Conclusion: In this study, HIV pre-exposure prophylaxis was not widely used by commercial female sex workers. Therefore, social and behavioral change communication strategies focus on creating awareness and building knowledge on HIV pre-exposure prophylaxis utilization.
Keywords: pre-exposure prophylaxis, HIV pre-exposure prophylaxis, female sex workers, Ethiopia
Introduction
Human immunodeficiency virus (HIV) is an infection that targets the immune system of the body, in particular the CD4 cells of the white blood cells. HIV kills these CD4 cells, which weakens the immune system and makes people more susceptible to opportunistic infections.Sex workers, users of injectable drugs, men who have sex with men, transgender persons, and their sexual partners worldwide are responsible for the high risk of HIV infections.2 Those who are more likely to contract HIV should undergo thorough and efficient HIV infection prevention, testing, and treatment programs. Pre-exposure prophylaxis (PrEP) has gained popularity as a legitimate method of preventing HIV infection among the high-risk population, such as female sex workers (FSWs).3
In 2012, the World Health Organization first recommended PrEP for a number of populations, including serodiscordant couples (SDCs), transgender women who have sex with men, and men who have sex with men.4 The first HIV pre-exposure began in 2013 with tenofovir (TDF).5
The WHO recommended in 2015 that PrEP be made available to all population groups with a high incident risk of infection (defined as ≥3%).6 Every individual at considerable risk of HIV should be offered oral PrEP with tenofovir disoproxil fumarate (TDF) as an alternative prevention option, according to the WHO guidelines issued in September 2015.7 Since 2017, PrEP drugs have been included in the WHO Essential Drugs List, including TDF/FTC and TDF/3TC.8
According to the UN program on HIV/AIDS, there was a reduction reduction of 75% in 2020 and different fast-track strategies were used to end the global epidemic by the end of 2030. One of the effective strategies to tackle this epidemic is PrEP 9.
For the well-being of high-risk population groups HIV preventive measures such as PrEP are crucial. It has been demonstrated that pre-exposure prophylaxis using anti-retroviral medications effectively lowers the risk of HIV infection.10
Pre-exposure prophylaxis (PrEP) has become a viable HIV prevention strategy for groups most at risk of contracting the virus.11 TDF/FTC is an effective HIV prevention strategy that is recommended for use as PrEP by those who are at high risk for HIV.12 The Ethiopian Federal Ministry of Health and development partners have committed to meeting the 2030 UNAIDS targets of 95–95 to end HIV transmission by that year by adopting PrEP in addition to other preventive strategies.13
Worldwide, in 2021, 38.4 million people will be positive for HIV. Of these, 1.5 million have newly contracted HIV. Significant demographic groups, including transgender individuals and their sexual partners, men who have sex with men, users injecting drugs, and sex workers and their clients, were responsible for 70% of HIV infections in 2021.14
Six out of every seven new HIV infections among teenagers in Sub-Saharan Africa between the ages of 15 and 19 are female. Women and girls accounted for 63% of all new HIV infections in 2021.14
Global studies have revealed that there is a low willingness to use PrEP. A relatively low degree of awareness or understanding about PrEP among FSW is seen in studies on the interest in PrEP among female bar workers in Tanzania (5%), China (15.1%), and Baltimore (21%).15–17 Drug safety, potential drug-to-drug interactions, elevated risk of other STDs, FSW pregnancy, stigma, efficacy, and cost, reduced risk perceptions, worries about the effectiveness of PrEP, and side effects are all factors that have been identified as potential barriers to PrEP uptake.15–18
Sociostructural hurdles to PrEP use in FSW include stigma, discrimination, criminalization, violence, and financial insecurity.15–18 Many FSWs are misinformed about the safety and adverse effects of PrEP, and there is widespread mistrust of the medication’s efficacy and cost.15–17,19,20
There are certain crucial logistical elements involved in the implementation of PrEP. This entails initial testing for HIV to establish HIV-negative status, continuing testing to make sure that HIV status is not changing, and monitoring for kidney health.21 Successful implementation and scale-up of PrEP will require these components, and it will also pose challenges such as repeat HIV testing, blood draws, and regular client follow-up. In addition, for PrEP to become mainstream as an intervention, communities need to become familiar with and accept the concept.21
Ethiopia is one of the nations where the HIV epidemic is most prevalent. According to the Ethiopian Demographic Health Survey (EDHS) conducted in 2016, the adult HIV prevalence rate was 0.9%, with women being more likely to contract the disease than men.22 Female sex workers (FSWs) have an HIV acquisition rate that is 30 times higher than that of the overall female population.23 In Ethiopia, 690,000 people were living with HIV in 2018, and 1% of adults were infected, which is higher than the global average report.24
FSWs are at higher risk of acquiring the HIV virus. However, developing countries like Ethiopia pay minimal attention to HIV-related care for sex workers.25 According to the research done in 2020, HIV prevalence in FSWs was 18.7% in Ethiopia and 28.2% in Bahir Dar city.23 The national comprehensive HIV prevention guideline was endorsed from 2018–2020 in Ethiopia.26 However, no evidence exists on the level of utilization toward HIV PrEP in female commercial sex workers in Ethiopia. Therefore, the aim of this study was to determine the utilization of HIV PrEP and associated factors among female sex workers.
Methods and Materials
Study Area and Period
The study was conducted at two nongovernmental organizations, the Networked HIV Positive Association and Development (NAPAD) and the Family Guidance Association of Ethiopia (FGAE), in Bahir Dar City. Bahir Dar city is in the Northwestern part of Ethiopia, 557 km from Addis Ababa. There are six administrative sub-cites. According to the EDHS 2021 population projection, Bahir Dar has 344,964 residents.25 Both NAPAD and FGAE organizations focus on HIV/AIDS prevention, care, and support for PLHIV, SRH services, peer sessions, condom distribution, family planning services, antenatal care services, HIV counseling and testing, sexually transmitted infection screening and intervention, hygiene support (modes, soap, showering), and others that target HIV-prone populations, mainly female sex workers, through community-based outreach and integrated HIV testing and counseling intervention approaches. The estimated number of female commercial sex workers in NAPAD and FGAE in Bahir Dar city is 6,557 and 3,000, respectively.26,27 The study was carried out from November 1 to 30, 2022.
Study design: An institution-based cross-sectional study design was used.
Source of population: all female sex workers who live in Bahir Dar city and are registered at NAPAD and FGAE.
Study population: Selected commercial female sex workers ≥18 years of age who were registered with NAPAD and FGAE during the data collection period.
Inclusion criteria: female sex workers ≥18 years of age registered with NAPAD and FGAE.
Exclusion criteria: Female sex workers who were critically ill during the data collection period and HIV-positive female sex workers were excluded.
Sample Size Determination
By employing a single proportion formula and a 50% proportion of PrEP with a 5% margin of error or precision, the sample size was determined. 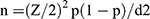 =384. By using the correction formula since the total population is less than 10,000. nf = final sample size; n=total number of female sex workers in NAPAD and FGAE, which was 9,557.
=384. By using the correction formula since the total population is less than 10,000. nf = final sample size; n=total number of female sex workers in NAPAD and FGAE, which was 9,557.
 = 369, the total sample size with 10% rate of nonresponse was added and then the final sample size of n = 406
= 369, the total sample size with 10% rate of nonresponse was added and then the final sample size of n = 406
Sampling technique: A simple sampling technique was used to select CFSWS who are registered in NAPAD (6,557) and FGAE (3,000) and had follow-up. During the last three months before the data collection period, we followed up at NAPAD (960) and FGAE (390). After proportionally allocating based on the registered numbers at NAPAD (278) and FGAE (128) and then using a random number table to recruit each study participant.
Study Variables
Dependent variables: HIV PrEP utilization (yes or no).
Independent variables: sociodemographic: age, marital status, religion, income, education, residence, experience of sex work, knowledge, and attitude, and drug-related factors, side effects of the PrEP, and availability of the PrEP.
Data Collection Tool and Procedures
A structured interviewer-administered Amharic version questionnaire was used. The tool for this study contains four sections: sociodemographic factors, knowledge, attitude, and utilization variables. Four female BSC nurse data collectors and one supervisor a BSc nurse. One-day training was given on the content of the questionnaire, Kobo Collect, and the data collection procedures. Kobo Collect is an open-source Android application for collecting survey data. It is a free flat form that can be used for humanitarian data collection. PrEP utilization was assessed with three questions.
Operational Definition
HIV PrEP utilization is measured using one “yes/no” question for current status: “Are you currently taking pre-exposure prophylaxis?” If yes, it is currently utilized, and if no, it is not utilized.28
Commercial female sex work: reported having had sex in exchange for money, goods, or services at any point in their lives.20
Knowledge: Participants’ knowledge was assessed using 11 yes/no questions about PrEP, with respondents scoring ≥50% to have good knowledge and those scoring ˂50% to have poor knowledge.18
Attitude: Measured using 16 items on a 5-point Likert scale from strongly disagree to strongly agree and summed to get the score. Participants who scored ≥50% had a favorable attitude, and those who scored <50% had an unfavorable attitude.18
Data Processing and Management
The data collected by Kobo Collect was transferred to the data manager (computer) and downloaded. The data were then exported to XLS and imported into STATA version 14 for analysis. Before analysis, data cleaning, coding, and recoding were performed. Descriptive statistics were used to characterize the sociodemographic status of the study participants. Bivariable and multivariable logistic regression analyses were done to identify predictors of utilization of HIV PrEP Independent variables with a P-value <0.2 in the bivariate analysis were entered into the multivariable logistic regression to control the possible effect of confounders using the forward likelihood variable selection method. The goodness of fit of the final models was checked using the Hosmer and Lemeshow test with a P-value of 0.25, which revealed that the model was fitted. Multicollinearity was checked using the variance inflation factor 1.23. The internal consistency of attitude items was checked for reliability using Cronbach’s alpha, which was 0.83.
A multivariable logistic regression factor with a P-value <0.05 was considered statistically significant and declared by the adjusted odds ratio (AOR) at a 95% confidence interval.
Data Quality Control
All data collectors and the supervisor were given one day training about data collection tools and procedures A pretest was done on 5% of the total sample before the real data collection period. Throughout the time of data collection, the supervisor reviewed the information gathered to ensure its accuracy and completeness.
Ethical Clearance
The Institutional Review Board (IRB) of the College of Medicine and Health Science at Bahir Dar University granted ethical approval under protocol number 553/2022. Participants were told of the study’s objectives, that participation was voluntary and open to withdraw or refuse at any time, and that the data was used for research purposes. Written informed consent was obtained from each study participant.
Results
Sociodemographic Characteristics
From the total sample size of 406, 396 respondents completed the study, making a response rate of 97.5%. The average age of the respondents was 26.46 years, with a standard deviation of ±4.60. The minimum age of the study participants was 18 years and the maximum age was 36 years (Table 1).
 |
Table 1 Sociodemographic Characteristics of Respondents Toward HIV Pre-exposure Prophylaxis Among Female Sex Workers at Bahir Dar City, Northwest Ethiopia, 2022 (n=396) |
Utilization of HIV Pre-exposure Prophylaxis
Among respondents, only 183 (46.21%) (95%CI: 41.33–51.16) used pre-exposure prophylaxis as an HIV prevention measure (Table 2).
 |
Table 2 HIV Pre-exposure Prophylaxis Utilization Among Female Sex Workers at Bahir Dar City, 2022 (n=396) |
Knowledge on HIV Pre-exposure Prophylaxis
The overall level of good knowledge among female sex workers was 202 (51%, 95%CI: 45.82–55.67). Among the total participants, 390 (98.48%) know that pre-exposure prophylaxis is a drug that is not given to HIV-positive people after they have been tested.
Attitude Toward HIV Pre-exposure Prophylaxis
The overall level of favorable attitudes among respondents was 41%, with a 95%CI: 95%CI of 36.14–45.84. More than half, 265 (66.92%) of the participants agreed that sex workers are likely to consistently use pre-exposure prophylaxis; 304 (76.77%) participants agreed that PrEP is an important measure for HIV prevention; and 138 (34.85%) participants agreed that pre-exposure prophylaxis is likely to have serious side effects. Of respondents, 147 (37.12%) agreed that taking PrEP is safe, 268 (67.68%) agreed that PrEP is effective in HIV prevention, and 267 (67.42%) agreed that everyone should have access to pre-exposure prophylaxis. Only 15 (2.78%) respondents agreed that if sex workers are taking PrEP, they will stop using condoms altogether (Table 3).
 |
Table 3 Attitude Toward Pre-exposure Prophylaxis Among Female Sex Workers in Bahir Dar City, 2022 (n=396) |
Factors Associated with HIV PrEP Utilization
To identify factors associated with HIV PrEP utilization among female sex workers, both bivariable and multivariable logistic regressions were performed. In the bivariable analysis, age, religion, marital status, education, reason for entering sex work, years of experience in sex work, knowledge, and attitude were all eligible for multivariable analysis.
In multivariable binary logistic regression analysis, only age, years of experience in sex work, education, and knowledge were significantly associated with HIV PrEP utilization among female sex workers.
Commercial female sex workers aged 26–36 years old were 75% less likely to utilize PrEP compared to age 18–21 year old female sex workers (AOR: 0.25; 95%CI: 0.17–0.84). Commercial female sex workers educational status: female sex workers who have secondary education and above were 2.18 times (AOR: 2.18; 95%CI: 1.05–4.35) more likely to use HIV PrEP compared to those who are unable to read and write.
Commercial female sex workers who had 3–5 years of sex work experience were 75% less likely to utilize HIV PrEP compared to those who had <3 years of sex work experience (AOR: 0.25; 95%CI: 0.24–0.82). Commercial female sex workers who had good knowledge were 4.98 times (AOR: 4.98; 95%CI: 3.90–10.65) more likely to utilize HIV PrEP compared to those who had poor knowledge (Table 4).
 |
Table 4 Multivariable Logistic Regression of Variables for HIV PrEP Utilization Among Female Sex Workers in Bahir Dar City, Northwest Ethiopia, 2022 (n=396) |
Discussion
In this study’s findings, 183 (46.21%) (95%CI: 41.33–51.16) female sex workers utilize HIV pre-exposure prophylaxis. This result is higher than the studies in New York and Portugal, which showed that only 17.4% and 0.4% of participants received a pre-exposure prophylaxis prescription.20,27 The possible reason might be due to differences in the study period, sociocultural differences between study participants, and perceptions of disease severity.
However, this study was lower than the studies done in Kenya (72%) and Ghana (53.99%), which were taking PrEP, respectively.18,27 Southern Arizona showed that 87% of participants utilized pre-exposure prophylaxis16, and another study in the US showed that 69.7% of participants were currently pre-exposure prophylaxis users.29 This difference might be because a prevention tool that requires less attention, pre-exposure prophylaxis, could benefit sex workers who have difficulty using it regularly.
Study design, and most likely because the study participants in this study were already attending reproductive health clinics and had access to pre-exposure prophylaxis.
Female sex workers in the age group of 26–36 years old were 0.2 times (AOR: 0.2; 95%CI: 0.17–0.84) less likely to utilize HIV PrEP compared to those aged 18–21 years. This finding was in line with studies in the US and Ghana. PrEP use was more commonly reported by those aged 18–29 years and <25 years (42.4%), 79.65% of whom use PrEP, respectively.18,29 Also, this was almost similar to the study conducted in New York, which was higher among participants aged 27 or older (22.8%).30
In this study, participants with a secondary education and above were 2.18 times (AOR: 2.18, 95%CI: 1.02–4.53) more likely to use HIV PrEP compared to those who are unable to read and write. This finding is comparable with a study conducted in the USA that revealed that higher education levels were significantly and positively associated with using pre-exposure prophylaxis (28.1%).30 sex workers who were educated may have awareness about PrEP, and they might have a positive perception toward using PrEP as a prevention measure.
In this study’s findings, those living in sex work who had 3–5 years’ experience were 0.25 times (AOR: 0.25, 95%CI: 0.24, 0.82) less likely to use HIV PrEP compared to those who were living in sex work for less than three years. This finding is consistent with a study conducted in Uganda, which found that people who worked in sex for <5 years were more likely to use PrEP than people who worked in sex for a long time.31
In this study, female sex workers who had good knowledge were 4.98 times (AOR: 4.98, 95%CI: 3.90–10.65) more likely to utilize HIV PrEP compared to those who had poor knowledge.
This is almost similar to a study done in Zimbabwe, which revealed that more knowledge about pre-exposure prophylaxis moderately increased the likelihood of pre-exposure prophylaxis use.28
The possible explanation for this similarity might be that people who are more knowledgeable have a better understanding of pre-exposure prophylaxis and have increased the probability of pre-exposure prophylaxis uptake.
Strengths and Limitations of the Study
The strength of the study was the use of Kobo Toolbox software for data collection, and an appropriate statistical test was done. A limitation of the study is that it was a cross-sectional. Cross-sectional studies limit causal explanations due to the temporal nature of exposure-outcome relationships. Social desirability bias is one of the limitations of this study due to the nature of the data collection technique being administered by the interviewer.
Conclusion
In this study, below half of female sex workers utilize HIV pre-exposure prophylaxis. Factors affecting utilization related to pre-exposure prophylaxis, including educational status, age, experience of sex work, and knowledge level, were statistically significantly associated with HIV pre-exposure prophylaxis utilization among female sex workers. Therefore, policymakers and stakeholders working on HIV/AIDS prevention should focus on strategic social and behavioral change communication to create awareness and build knowledge on HIV pre-exposure prophylaxis.
Data Sharing Statement
Data is available within the manuscript.
Ethical Considerations
Ethical clearance was obtained from the Institutional Board of Review of Bahir Dar University College of Medicine and Health Science, with an IRB reference number of 553/2022. Written informed consent was obtained from each study participant. This study was conducted in accordance with the Declaration of Helsinki.
Acknowledgment
We express our gratitude to the Department of Health Promotion and Behavioral Sciences, School of Public Health, and College of Medicine and Health Sciences, Bahir Dar University. We also thank the nongovernmental organizations NAPAD and FGAE head office, as well as all data collectors and study participants, for their cooperation and devoting their time.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, data collection, quality control, analysis and interpretation of results, and preparation of the manuscript; critically reviewing the manuscript; giving final approval of the version to be published; agreeing to the journal to which the article has been submitted; and agreeing to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. WHO Case Definitions of HIV for Surveillance and Revised Clinical Staging and Immunological Classification of HIV-Related Disease in Adults and Children. World Health Organization, 2007.
2. HIV/AIDS JUNPo. Global AIDS Update: Fact Sheet. Geneva: UNAIDS Global Statistics, 2019:6.
3. Abou Ghayda R, Hong SH, Yang JW, et al. A review of pre-exposure prophylaxis adherence among female sex workers. Yonsei Med J. 2020;61(5):349. doi:10.3349/ymj.2020.61.5.349
4. Van der Elst EM, Mbogua J, Operario D, et al. High acceptability of HIV pre-exposure prophylaxis but challenges in adherence and use: qualitative insights from a Phase I trial of intermittent and daily PrEP in at-risk populations in Kenya. AIDS Behav. 2013;17(6):2162–2172. doi:10.1007/s10461-012-0317-8
5. World Health Organization. Guidelines on When to Start Antiretroviral Therapy and Pre-Exposure Prophylaxis for HIV. World Health Organization, 2015.
6. Nhamo D, Duma SE, Ojewole EB, Chibanda D, Cowan FM, Sharifi H. Factors motivating female sex workers to initiate pre-exposure prophylaxis for HIV prevention in Zimbabwe PLoS One. 2022;17(7):e0264470. doi:10.1371/journal.pone.0264470
7. World Health Organization. Health Worker Role in Providing Safe Abortion Care and Post-Abortion Contraception. World Health Organization, 2015.
8. Hodges-Mameletzis I, Dalal S, Msimanga-Radebe B, Rodolph M, Baggaley R. Going global: the adoption of the World Health Organization’s enabling recommendation on oral pre-exposure prophylaxis for HIV. Sexual Health. 2018;15(6):489–500. doi:10.1071/SH18125
9. Masyuko S, Mukui I, Njathi O, et al. Pre-exposure prophylaxis rollout in a national public sector program: the Kenyan case study. Sexual Health. 2018;15(6):578–586. doi:10.1071/SH18090
10. Tanner MR, Miele P, Carter W, et al. Preexposure prophylaxis for prevention of HIV acquisition among adolescents: clinical considerations, 2020. MMWR Recommendations Rep. 2020;69(3):1. doi:10.15585/mmwr.rr6903a1
11. Beymer MR, Weiss RE, Sugar CA, et al. Are centers for disease control and prevention guidelines for preexposure prophylaxis specific enough? Formulation of an a personalized HIV risk score for pre-exposure prophylaxis initiation. Sexually Transmitted Diseases. 2017;44(1):49–57. doi:10.1097/OLQ.0000000000000535
12. Pines H, Strathdee S, Hendrix C, et al. Oral and vaginal HIV pre-exposure prophylaxis product attributes and preferences among female sex workers in the Mexico-US border region. Int J STD AIDS. 2019;30(1):45–55. doi:10.1177/0956462418793038
13. Haile T, Lamessa A, Mekonnen Y, Ifa M. HIV prevalence and associated factors among high-risk individuals recruited through social network strategies in the Oromia region of Ethiopia: a Retrospective retrospective study. Int J HIV/AIDS Prev Educ Behav Sci. 2022;8(1):1–7.
14. Global H. AIDS statistics—2020 fact sheet; 2020. 2021.
15. Harling G, Muya A, Ortblad KF, et al. HIV risk and pre-exposure prophylaxis interest among female bar workers in Dar es Salaam: a cross-sectional survey. BMJ open. 2019;9(3):e023272. doi:10.1136/bmjopen-2018-023272
16. Ye L, Wei S, Zou Y, et al. HIV pre-exposure prophylaxis interest among female sex workers in Guangxi, China. PLoS One. 2014;9(1):e86200. doi:10.1371/journal.pone.0086200
17. Tomko C, Park JN, Allen ST, et al. Awareness and interest in HIV pre-exposure prophylaxis among street-based female sex workers: results from a US context. AIDS Patient Care STDS. 2019;33(2):49–57. doi:10.1089/apc.2018.0182
18. Guure C, Afagbedzi S, Torpey K. Willingness to take and ever use pre-exposure prophylaxis among female sex workers in Ghana. Medicine. 2022;101(5). doi:10.1097/MD.0000000000028798
19. Mantsios A, Muraleetharan O, Donastorg Y, et al. “She is the one who knows”: a qualitative exploration of oral and injectable PrEP as part of a community empowerment approach to HIV prevention among female sex workers in the Dominican Republic and Tanzania. PLOS Glob Public Health. 2022;2(9):e0000981. doi:10.1371/journal.pgph.0000981
20. Ucsf A. South African Health Monitoring Study (SAHMS), Final Report: The Integrated Biological and Behavioural Survey Among Female Sex Workers, South Africa 2013–2014. San Francisco, CA: UCSF, 2015.
21. Eakle R, Venter F, Rees H. Pre-exposure prophylaxis (PrEP) in an era of stalled HIV prevention: can it change the game? Retrovirology. 2018;15(1):1–10. doi:10.1186/s12977-018-0408-3
22. Abubeker FA, Fanta MB, Dalton VK. There is an unmetneed for contraception among HIV-positive women attending HIV care and treatment services at Saint Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia. Int J Reprod Med. 2019;1–7. doi:10.1155/2019/3276780
23. Abdella S, Demissie M, Worku A, Dheresa M, Berhane Y. HIV prevalence and associated factors among female sex workers in Ethiopia, East Africa: a cross-sectional study using a respondent-driven sampling technique. EClinicalMedicine. 2022;51:101540. doi:10.1016/j.eclinm.2022.101540
24. Alemu GH, Gidebo DD, Ali MM. The magnitudeof HIV infection and associated factors among female sex workers in Hawassa, Ethiopia. Ethiop J Health Sci. 2022;32(2):261–268. doi:10.4314/ejhs.v32i2.6
25. Park CJ, Taylor TN, Gutierrez NR, Zingman BS, Blackstock OJ. Pathways to HIV pre-exposure prophylaxis among women prescribed PrEP at an urban sexual health clinic. J Assoc Nurses AIDS Care. 2019;30(3):321–329. doi:10.1097/JNC.0000000000000070
26. Amogne MD, Sanders EJ, Belihu WB, Sundewall J, Agardh A. Condom failure and pre-exposure prophylaxis use experience among female sex workers in Ethiopia: a qualitative study. BMC Public Health. 2022;22(1):1–10. doi:10.1186/s12889-022-13468-3
27. Litiema E, Orago A, Muia D. Correlations associated with adherence among female sex workers to HIV pre-exposure prophylaxis in Nairobi City County, Kenya. J Health Med Nurs. 2021;7(3):29–40. doi:10.47604/jhmn.1401
28. Mudzviti T, Dhliwayo A, Chingombe B, et al. Perspectives on oral pre-exposure prophylaxis use amongst female sex workers in Harare, Zimbabwe. S Afr J HIV Med. 2020;21(1):1-6. doi:10.4102/sajhivmed.v21i1.1039
29. Kota KK, Mansergh G, Stephenson R, Hirshfield S, Sullivan P. Sociodemographic characteristics of HIV pre-exposure prophylaxis use and reasons for nonuse among gay, bisexual, and other men who have sex with men from three US cities. AIDS Patient Care STDS. 2021;35(5):158–166. doi:10.1089/apc.2020.0261
30. Zarwell M, John SA, Westmoreland D, et al. PrEP uptake and discontinuation among a US US national sample of transgender men and women. AIDS Behav. 2021;25(4):1063–1071. doi:10.1007/s10461-020-03064-0
31. Kawuma R, Ssemata AS, Bernays S, Seeley J. Women at high risk of HIV infection in Kampala, Uganda, and their candidacy for PrEP. SSM Popul Health. 2021;13:100746. doi:10.1016/j.ssmph.2021.100746
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
