Back to Journals » Infection and Drug Resistance » Volume 15
Utility of Human Neutrophil Lipocalin as a Diagnosing Biomarker of Prosthetic Joint Infection: A Clinical Pilot Study
Received 1 January 2022
Accepted for publication 29 April 2022
Published 2 May 2022 Volume 2022:15 Pages 2393—2400
DOI https://doi.org/10.2147/IDR.S355180
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Hanjiang Liu,1,* Yali Yu,1,* Yanli Niu2
1Department of Clinical Laboratory, Zhengzhou Orthopaedics Hospital, Zhengzhou, Henan, 450000, People’s Republic of China; 2School of Basic Medical Science, Henan University, Kaifeng, Henan, 475004, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yanli Niu, School of Basic Medical Science, Henan University, Kaifeng, Henan, 475004, People’s Republic of China, Email [email protected]
Purpose: The discrimination of prosthetic joint infection (PJI) from aseptic failure is regarded as a major clinical challenge. The key function of human neutrophil lipocalin (HNL) in regulating bacterial infection rationalizes its potential as a biomarker to diagnose PJI. This work evaluated the accuracy of serum human neutrophil lipocalin as a biomarker to diagnose PJI.
Methods: This prospective cohort study enrolled altogether 58 patients suffering from miserable knee or hip arthroplasty and receiving revision surgery from 2018 to 2020. Related laboratory and clinical information of these patients were retrieved. Following the Musculoskeletal Infection Society (MSIS) criteria, the diagnosis of PJI was conducted. Collecting preoperative blood samples, we measured HNL by the standard assay. Thereafter, plotting the receiver-operating characteristic curve (ROC), the area under the curve (AUC) values were calculated to analyze the diagnosis accuracy.
Results: According to the MSIS criteria, 38 cases (65.5%) were classified into the PJI group, while 20 (34.5%) into the aseptic loosening group, with age ranging from 38 to 87 (median, 66.9) years. The median serum HNL level of the PJI patients was 199.01 (range, 85.34– 357.79) ng/mL, significantly higher as compared with that of 64.81 (range, 20.73– 157.89) ng/mL of the aseptic loosening group. Using the Youden index, the optimal threshold value was 105.1ng/mL, while the specificity, sensitivity, and AUC were 85.0%, 81.6%, and 0.919, respectively.
Conclusion: Serum HNL is the creditable test that can be employed as the laboratory biomarker to screen PJI. The threshold HNL level is 105.1 ng/mL, which may distinguish PJI from aseptic failure.
Keywords: prosthetic joint infection, human neutrophil lipocalin, biomarker, arthroplasty
Introduction
The severe complication secondary to total joint arthroplasty (TJA) is periprosthetic joint infection (PJI) which may lead to catastrophic results, like limb loss, revision surgery, and even death.1–3 Nonetheless, it is still not easy to diagnose PJI and often gets delayed, in particular in the presence of low-degree or chronic infections, because of the absence of any “gold standard” examinations available and the existing diagnostic approaches fail to achieve high accuracy.4–6
Standard tests, including erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), are unable to achieve satisfactory diagnostic value.7,8 Therefore, many efforts are made to elucidate novel approaches to effectively detect PJI, such as circulating cytokine analysis, molecular approaches, and implant sonication.9–11 Nonetheless, such novel diagnostic approaches are expensive, time-consuming, and need special equipment, restricting their clinical application. This necessitates the development of highly sensitive, specific, cost-effective markers or marker panels for diagnosis so as to rapidly diagnose and differentiate disease under varied clinical conditions.
Human neutrophil lipocalin (HNL) can also be referred to as neutrophil gelatinase-associated lipocalin (NGAL) and lipocalin 2.12,13 Neutrophil granulocytes reflect the major HNL source, while the main site for protein generation in some conditions is epithelial cells.14–16 HNL was frequently associated with tumor size, stage, and invasiveness. These characteristics thus make it a potential biomarker for malignancy.17 Carlson et al reported HNL served as a unique marker of neutrophil inflammation in ulcerative colitis and proctitis.18 Immunoassays estimating HNL/NGAL in different body fluids suggested escalation of its concentration in urine and blood among cases suffering from acute kidney injury (AKI) and those having bacterial infections, respectively.19,20 Thus, serum HNL level is presumed to distinguish viral from bacterial infections, which can achieve high likelihood, and negative (NPV) and positive (PPV) predictive values (NPV) in the N90% distinction.21 As verified by other articles, the potent discrimination of serum HNL content on adults and children indicates that measuring serum HNL level can be the potential biomarker to differentiate viral from acute bacterial infections.22–24 The joint fluid HNL has also proved the existence of closed correlations between PJI and aseptic loosening.25–27 Deirmeingian et al were the first to predicted HNL in synovial fluid with 100% sensitivity and specificity,26 and Vergara et al reported 86% sensitivity and 77% specificity applying MSIS definition.25 Thirdly, Dijkman reported synovial fluid HNL 92% sensitivity and 83% specificity when applying the MSIS criteria.27 Based on the above findings, the HNL level has been recognized as the potential diagnostic factor to diagnose postoperative prosthesis infection. Nonetheless, there is no available article demonstrating HNL’s function in blood as the candidate biomarker to diagnose PJI. Thus, this single-center study mainly focused on the significance of serum HNL in distinguishing between aseptic failure and PJI.
Methods
Study Design, Patient Inclusion, and Exclusion Criteria
This single-centered prospective cohort study was conducted in one medical university hospital. The Board Review Committee of Zhengzhou Orthopaedics Hospital approved our study protocols. Each partaker provided informed consent for participation. This work included cases who underwent knee or hip arthroplasty revision between 2018 and 2020 in our institution. Patients conforming to the following criteria were enrolled: those undergoing total knee or hip arthroplasty to treat osteoarthritis and those who were about to receive revision due to aseptic loosening and suspected infection. The exclusion criteria involved cases who took antibiotics for a long time (>7 days) in 2 weeks prior to admission, cases who had other sites of infections (including urinary or respiratory tract infection), acute or chronic renal function injury patients, chronic renal insufficiency, and patients with active malignant disease. Moreover, cases with heavy smoking (≥20 cigarettes per day) or those with obesity (body mass index (BMI) >35 kg/m2) were also eliminated from this study.
PJI diagnosis was defined according to the MSIS definition.28 We determined the need for revision in patients due to aseptic causes (like wear, aseptic loosening, malalignment, instability) or PJI. Preoperative blood was sampled to determine ESR, CRP, D-dimer, PCT (Procalcitonin), and HNL.
Bacterial Culture
Synovial fluids after collection in the operating room were cultured in BD BACTEC aerobic/anaerobic/fungal and acid-fast bacilli vials for 14 days (35 °C). Intraoperative periprosthetic tissue samples were homogenized for 1min using BHI broth (3mL). Thereafter, the as-obtained homogenate was further cultured on Columbia blood agar containing selective medium, chocolate agar and 5% sheep blood for 7 days at 35 °C both anaerobically and aerobically. The same amount of homogenate (1mL) was inoculated into BD BACTEC aerobic/anaerobic/fungal and acid-fast bacilli bottles for 14 days.
Measurement of Serum HNL Levels
HNL levels in heparinized blood or EDTA-plasma were determined using the double monoclonal ELISA kit (Diagnostics Development, Uppsala, Sweden) following the specific protocols. In the ELISA assay, the <6% CV imprecision was allowed. HNL levels within whole blood samples were analyzed based on the previous description.
Statistical Analysis
Results were expressed in the form of medians. The data obtained from diagnostic tests were compared using Fisher’s exact test and independent-sample t-test. Meanwhile, this study plotted receiver-operating characteristic (ROCs) curves to present HNL-index within the blood, CRP, ESR, PCT, and D-dimer levels, respectively, which were subsequently adopted for establishing the best thresholds to diagnose PJI based on Youden’s J statistic. The specificity, sensitivity, as well as area under the curve (AUC) values were evaluated with the help of the MedCalc 13.2.2 Software (MedCalc, Ostend, Belgium). Further, this study also adopted SPSS24.0 (SPSS, Chicago, Illinois, USA) for statistical analysis. P<0.05 represented statistical significance.
Results
General Characteristics and Comorbidities of Patients
This study enrolled a total of 58 patients for revision knee or hip arthroplasty from 2018 to 2020. The MSIS criteria on PJI categorized 38 patients into the PJI group, while 20 were into the aseptic group (Figure 1). The study population comprised 35 (57.4%) males and 26 (42.6%) females, yielding the ratio of male to female of 1.3. The mean age was 66.4 ±6.7 years and 67.3 ±8.2 years for the PJI and non-PJI groups, respectively. Preoperative blood was obtained from the hip in 7 (17.2%) and knee in 51 (82.8%) cases. Patient baseline features and underlying diseases are detailed in Table 1.
 |
Table 1 Demographic Data for the Study Population |
 |
Figure 1 Flowchart of patient inclusion. |
The Diagnostic Accuracy and ROC Curve of PJI Diagnosis by Using Serum HNL
Relative to the aseptic group, the PJI group manifested significantly high serum PCT, ESR, and HNL levels (Figure 2). However, blood CRP and D-dimer levels failed to demonstrate significant differences between both groups, respectively (p = 0.204, p = 0.414). The median serum HNL level was 199.01 ng/mL (ranging from 85.34 to 357.79) among patients with PJI compared to 64.81 ng/mL (20.73 to 157.89) among those with no PJI (p < 0.001). Meanwhile, the PJI group revealed the median level of PCT of 0.52 mg/L (0.22–1.34) relative to that of 0.27 mg/L (0.04–0.45) for the non-PJI group (p = 0.000). Moreover, the median CRP level was 22.27 mg/L (1.03–89.26) in the PJI group, whereas 15.99 mg/L (3.01–50.40) in the non-PJI group (p = 0.204). As evident from Table 2, the median ESR and median D-dimer of the PJI group were 41.63 mm/H (9.00–80.00) and 1.58 mg/L (0.19–3.38), respectively, while those in the non-PJI group were 13.70 mm/H (3.00–25.00) and 1.39 mg/L (1.87–2.05), respectively (p = 0.000, p = 0.414).
 |
Table 2 Sensitivity, Specificity, Positive Predictive Value, Negative Predictive Value, and Accuracy of Inflammatory Markers |
To analyze the discriminating ability of these inflammatory parameters of PJI versus non-PJI groups, ROC curves regarding the serum parameters were plotted (Figure 3). Results revealed the AUC value for serum CRP was 0.531 (95% CI 0.429–0.719), while that for D-dimer was 0.579 (95% CI 0.384–0.678). The PJI and non-PJI groups could be well discriminated by the serum HNL, ESR, and PCT, and their AUC values were 0.919 (95% CI 0.851–0.987), 0.878 (95% CI 0.773–0.982), and 0.856 (95% CI 0.678–0.913), respectively. Table III narrates the comprehensive features of serum CRP, ESR, PCT, D-dimer, and HNL in diagnosis. To distinguish aseptic failure from PJI, the best threshold for serum HNL was 105.15 ng/mL, and the maximal specificity and sensitivity were 85.00% (95% CI 74.6–96.9%) and 81.6% (95% CI 71.0–93.0%), respectively. To detect PJI, PCT at level of 0.32 mg/L reflected the specificity and sensitivity of 90.0% (95% CI 85.4–99.1%) and 78.9% (95% CI 65.7–85.8%), separately; those for CRP level (19.2 mg/L) were 80.0% (95% CI 71.1–89.7%) and 57.9% (95% CI 43.5–67.1%), separately. ESR demonstrated a specificity of 76.3% (95% CI 62.3–82.2%) and a sensitivity of 93.5% (95% CI 88.8–100.0%) at the 24.5 mm/H threshold; D-dimer at level of 2.13 mg/L highlighted the specificity and sensitivity of 100.0% (95% CI 95.0–100.0%) and 31.6% (95% CI 21.8–40.7%), separately.
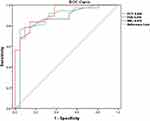 |
Figure 3 ROC curves for diagnostic indicators with an AUC >0.7, which included PCT, ESR, HNL. |
Microbiological Findings
All of these patients had ≥2 positive culture specimens with the same organism. Totally, 27 (27/38, 71.1%) cultures were positive in diagnosed PJI patients. S. epidermidis (12/27, 42.9%) and S. aureus (5/27, 21.4%) were the most commonly cultured bacteria, followed by fungal (3/27), Mycobacterium tuberculosis (2/27), Pseudomonas aeruginosa (2/27), Escherichia coli (2/27) and Brucella (1/27). There were no polymicrobial culture results. Five out of 11 patients with PJI are negative cultures.
Discussion
Despite recent advancements in exploring the approaches to diagnose PJI, it is still not easy to definitely detect PJI prior to surgical treatment. More efforts are warranted to develop novel strategies to timely and correctly diagnose PJI.
A degranulation product of neutrophils, HNL, is found to be expressed at a low level in the kidney, lung, stomach, colon, and prostate under normal physiological conditions. HNL expression escalates when inflammation stimulates neutrophil activation or epithelial cell injury.29 Research findings substantiate the close association of HNL to inflammation, signal transduction, immune response, and the occurrence and development of tumors. The HNL begins to rise at 6–8 h following infection and reaches the peak at 24–48 h. Recent results predict a more rapid release time of HNL. Thus, alterations in serum HNL levels are beneficial in detecting acute infection.
The results of this study emphasized that differences in PCT, HNL, and ESR were of statistical significance between the PJI and non-PJI groups. Meanwhile, serum D-dimer and CRP levels did not reveal any differences between both groups.
ROC curve is the most commonly employed method to estimate the diagnostic value. It takes the 1-specificity (misdiagnosis rate or false-positive rate) corresponding to different cutoff points as the abscissa and the sensitivity (true-positive rate) as the ordinate to connect the obtained operating points into a curve. The diagnostic value of the diagnostic test is determined by the ROC AUC, typically 0.5≤AUC≤1. A higher AUC value reflects a higher diagnostic value. Analyzing the ROC curves of the five indicators, the AUC of HNL and ESR were all higher than 0.90 with no significant difference, but HNL exhibited the highest diagnostic value. In the diagnosis of bacterial infectious diseases, the cutoff values of HNL, ESR, and PCT were 105.1 ng/mL, 24.5 mm/h, and 0.32 ng/mL, respectively. The cutoff values of ESR and PCT in the diagnosis of bacterial infectious diseases differed from those in other studies, which may be attributed to the differences in disease patterns, regions, populations, reagents, instruments, etc. Further investigation will greater sample size will help to identify the most accurate cutoff value to provide relevant data for clinical diagnosis.
In conclusion, HNL, ESR, PCT, CRP, and D-dimer are all increasing at PJI, but the sensitivity, specificity, and accuracy of HNL, ESR, CRP, D-dimer, and PCT in the diagnosis of PJI varied. The sensitivity of HNL was the highest, with 85.1% sensitivity. To our knowledge, this is the first study evaluating serum HNL as diagnostic biomarker for PJI. Deirmeingian et al were the pioneer to detect synovial fluid HNL, demonstrating 100% for both sensitivity and specificity based on the MSIS criteria.27 Subsequently, the sensitivity and specificity of synovial fluid HNL detected by Vergara et al demonstrated 86% sensitivity and 77% specificity, respectively.25 Dijkman then reported 92% sensitivity and 83% specificity when applying the MSIS criteria, and sensitivity 95% and specificity 95% when according to the pro-Implant criteria.26 Notably, their cut-off values (2.2 μg/mL, 0.152 μg/mL and 0.7355 μg/mL, respectively) were distinguished from the values our analysis revealed (199.01 ng/mL=0.199μg/mL, MSIS criteria), which could potentially result from using of different analyzers and type of sample. HNL was detected by an Enzyme-linked immunosorbent assay in our study. At present, Shahi et al described the benefits of D-dimer in the diagnosis of PJI, with a sensitivity of 89% and a specificity of 93%.30 In our study, D-dimer was presented the highest specificity (100%), but less sensitivity (31.6%) to distinct between PJI and non-PJI. Serum PCT is also not a good adjunct in diagnosing PJI in other study.31 The reason may be a different detection methods and reagents used and different cutoff for infection in the present study.32 Fjaertoft et al24 also believed that the process of bacterial infection could be better reflected by HNL than CRP and PCT tests. Hemodynamic studies of HNL and CRP revealed that CRP still maintained a high level after the elimination of bacterial infection, while HNL was consistent with the degree of disease recovery.24 These findings justified the application of HNL as a detection indicator to guide use more effectively and avoid the irrational use of antibiotics. To offer the foundation of rapid diagnosis of PJI in the clinic, the research group will further explore the sensitivity, specificity, and accuracy of the combined diagnosis of multiple detection indicators.
Several limitations of this study included: Firstly, although MSIS criteria are well-accepted at present, the gold-standard test to detect PJI is lacking for the time being. In this regard, the criteria selected in the present work might misclassify the PJI or non-PJI patients. Secondly, the small sample size of this study might affect the NPV/PPV of the indicators. Furthermore, underlying diseases in certain cases might affect the HNL level. Moreover, the present single-center study only enrolled Asian patients. Thus, to eliminate biases of race and researcher, more multicenter studies are required.
Conclusion
This work confirmed the remarkably higher serum HNL levels in PJI cases with high specificity and sensitivity in diagnosis. Serum HNL was identified as the candidate diagnostic biomarker for PJI, which might be incorporated in the diagnostic algorithm of MSIS criteria.
Abbreviations
PJI, periprosthetic joint infection; HNL, human neutrophil lipocalin; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; BMI, body mass index; PCT, procalcitonin.
Ethics Approval and Consent to Participate
The study protocol was approved by the Institutional Review Board of Zhengzhou Orthopaedics Hospital (202203). This study was conducted in accordance with the declaration of Helsinki and patient data were kept confidential.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare that there are no conflicts of interest in this work.
References
1. Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev. 2014;27(2):302–345. doi:10.1128/CMR.00111-13
2. Goswami K, Parvizi J, Maxwell Courtney P. Current recommendations for the diagnosis of acute and chronic PJI for hip and knee-cell counts, alpha-defensin, leukocyte esterase, next-generation sequencing. Curr Rev Musculoskelet Med. 2018;11(3):428–438. doi:10.1007/s12178-018-9513-0
3. Maale GE, Eager JJ, Srinivasaraghavan A, Mohammadi DK, Kennard N. The evolution from the two stage to the one stage procedure for biofilm based periprosthetic joint infections (PJI). Biofilm. 2020;2:100033. doi:10.1016/j.bioflm.2020.100033
4. Aynardi MC, Plöger MM, Walley KC, Arena CB. What Is the definition of acute and chronic Periprosthetic Joint Infection (PJI) of Total Ankle Arthroplasty (TAA)? Foot Ankle Int. 2019;40(1_suppl):19S–21S. doi:10.1177/1071100719859527
5. Kalbian IL, Goswami K, Tan TL, et al. Treatment outcomes and attrition in gram-negative periprosthetic joint infection. J Arthroplasty. 2020;35(3):849–854. doi:10.1016/j.arth.2019.09.044
6. Abad CL, Haleem A. Prosthetic joint infections: an update. Curr Infect Dis Rep. 2018;20(7):15. doi:10.1007/s11908-018-0622-0
7. Iannotti F, Prati P, Fidanza A, et al. Prevention of Periprosthetic Joint Infection (PJI): a clinical practice protocol in high-risk patients. Trop Med Infect Dis. 2020;5(4):186. doi:10.3390/tropicalmed5040186
8. Saleh A, George J, Faour M, Klika AK, Higuera CA. Serum biomarkers in periprosthetic joint infections. Bone Joint Res. 2018;7(1):85–93. doi:10.1302/2046-3758.71.BJR-2017-0323
9. Izakovicova P, Borens O, Trampuz A. Periprosthetic joint infection: current concepts and outlook. EFORT Open Rev. 2019;4(7):482–494. doi:10.1302/2058-5241.4.180092
10. Gallo J, Raska M, Dendis M, Florschütz AV, Kolár M. Molecular diagnosis of prosthetic joint infection. A review of evidence. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2004;148(2):123–129. doi:10.5507/bp.2004.022
11. Heim CE, Bosch ME, Yamada KJ, et al. Lactate production by Staphylococcus aureus biofilm inhibits HDAC11 to reprogramme the host immune response during persistent infection. Nat Microbiol. 2020;5(10):1271–1284. doi:10.1038/s41564-020-0756-3
12. Venge P, Eriksson AK, Douhan-Håkansson L, Pauksen K. Human neutrophil lipocalin in activated whole blood is a specific and rapid diagnostic biomarker of bacterial infections in the respiratory tract. Clin Vaccine Immunol. 2017;24(7):e00064–17. doi:10.1128/CVI.00064-17
13. Venge P. Human neutrophil lipocalin (HNL) as a biomarker of acute infections. Ups J Med Sci. 2018;123(1):1–8.
14. Cai L, Rubin J, Han W, Venge P, Xu S. The origin of multiple molecular forms in urine of HNL/NGAL. Clin J Am Soc Nephrol. 2010;5(12):2229–2235. doi:10.2215/CJN.00980110
15. Nielsen BS, Borregaard N, Bundgaard JR, Timshel S, Sehested M, Kjeldsen L. Induction of NGAL synthesis in epithelial cells of human colorectal neoplasia and inflammatory bowel diseases. Gut. 1996;38(3):414–420. doi:10.1136/gut.38.3.414
16. Zughaier SM, Tangpricha V, Leong T, Stecenko AA, McCarty NA. Peripheral monocytes derived from patients with cystic fibrosis and healthy donors secrete NGAL in response to Pseudomonas aeruginosa infection. J Investig Med. 2013;61(6):1018–1025. doi:10.2310/JIM.0b013e31829cbd14
17. Lippi G, Meschi T, Nouvenne A, et al. Neutrophil gelatinase-associated lipocalin in cancer. Adv Clin Chem. 2014;64:179–219. doi:10.1016/b978-0-12-800263-6.00004-5
18. Carlson M, Raab Y, Sevéus L, et al. Human neutrophil lipocalin is a unique marker of neutrophil inflammation in ulcerative colitis and proctitis. Gut. 2002;50(4):501–506. doi:10.1136/gut.50.4.501
19. Mårtensson J, Xu S, Bell M, Martling CR, Venge P. Immunoassays distinguishing between HNL/NGAL released in urine from kidney epithelial cells and neutrophils. Clin Chim Acta. 2012;413(19–20):1661–1667. doi:10.1016/j.cca.2012.05.010
20. Mishra J, Dent C, Tarabishi R, et al. Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet. 2005;365(9466):1231–1238.
21. Xu SY, Petersson CG, Carlson M, Venge P. The development of an assay for human neutrophil lipocalin (HNL)–to be used as a specific marker of neutrophil activity in vivo and vitro. J Immunol Methods. 1994;171(2):245–252.
22. Yu Z, Jing H, Hongtao P, et al. Distinction between bacterial and viral infections by serum measurement of human neutrophil lipocalin (HNL) and the impact of antibody selection. J Immunol Methods. 2016;432:82–86. doi:10.1016/j.jim.2016.02.014
23. Venge P, Xu S. Diagnosis and monitoring of acute infections with emphasis on the novel biomarker human neutrophil lipocalin. J Appl Lab Med. 2019;3(4):664–674. doi:10.1373/jalm.2018.026369
24. Fjaertoft G, Foucard T, Xu S, Venge P. Human neutrophil lipocalin (HNL) as a diagnostic tool in children with acute infections: a study of the kinetics. Acta Paediatr. 2005;94(6):661–666. doi:10.1111/j.1651-2227.2005.tb01961
25. Vergara A, Fernández-Pittol MJ, Muñoz-Mahamud E, et al. Evaluation of lipocalin-2 as a biomarker of periprosthetic joint infection. J Arthroplasty. 2019;34(1):123–125. doi:10.1016/j.arth.2018.09.047
26. Dijkman C, Thomas AR, Koenraadt KLM, Ermens AAM, van Geenen RCI. Synovial neutrophilic gelatinase-associated lipocalin in the diagnosis of periprosthetic joint infection after total knee arthroplasty. Arch Orthop Trauma Surg. 2020;140(7):941–947. doi:10.1007/s00402-020-03427-1
27. Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Parvizi J. Diagnosing periprosthetic joint infection: has the era of the biomarker arrived? Clin Orthop Relat Res. 2014;472(11):3254–3262. doi:10.1007/s11999-014-3543-8
28. Parvizi J, Zmistowski B, Berbari EF, et al. New definition for periprosthetic joint infection: from the workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res. 2011;469(11):2992–2994. doi:10.1007/s11999-011-2102-9
29. Schmidt-Ott KM, Mori K, Li JY, et al. Dual action of neutrophil gelatinase-associated lipocalin. J Am Soc Nephrol. 2007;18(2):407–413. doi:10.1681/ASN.2006080882
30. Shahi A, Kheir MM, Tarabichi M, Hosseinzadeh HRS, Tan TL, Parvizi J. Serum D-dimer test is promising for the diagnosis of periprosthetic joint infection and timing of reimplantation. J Bone Joint Surg Am. 2017;99(17):1419–1427. doi:10.2106/JBJS.16.01395
31. Guerreiro FD, Mumith A, Saeed K. Serum procalcitonin as an adjunct in diagnosing prosthetic joint infection in total knee replacement and total hip replacement. Infez Med. 2020;28(1):6–10.
32. Riley RS, Gilbert AR, Dalton JB, Pai S, McPherson RA. Widely used types and clinical applications of D-dimer assay. Lab Med. 2016;47(2):90–102. doi:10.1093/labmed/lmw001
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

