Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
Utility of Alpha-Fetoprotein and Ultrasound in the Diagnosis and Prognosis of Patients with Hepatocellular Liver Cancer
Authors Huang D, Zhang J, Xu J, Niu Q, Zhou D
Received 10 November 2023
Accepted for publication 4 April 2024
Published 23 April 2024 Volume 2024:17 Pages 1819—1826
DOI https://doi.org/10.2147/JMDH.S449276
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Dongfang Huang,1– 3 Jianhuai Zhang,3 Jianbo Xu,3 Qiang Niu,2 Dinghua Zhou2
1Department of Hepatobiliary Surgery, Medical College of Soochow University, Suzhou, People’s Republic of China; 2Department of Hepatobiliary Surgery, PLA Rocket Force Characteristic Medical Center, Beijing, People’s Republic of China; 3Department of Hepatobiliary Surgery, The Affiliated Huaian No.1 People’s Hospital of Nanjing Medical University, Huaian, People’s Republic of China
Correspondence: Dinghua Zhou, Department of Hepatobiliary Surgery, PLA Rocket Force Characteristic Medical Center, No. 16 Xinjiekou Outer Street, Xicheng District, Beijing, 100088, People’s Republic of China, Tel +86 010-66343003, Fax +86 010-66343055, Email [email protected]
Objective: To investigate the utility of alpha-fetoprotein (AFP) and ultrasound in the diagnosis and prognosis of patients with hepatocellular liver cancer (HCC).
Methods: Using retrospective convenience sampling, 401 patients with HCC who underwent transarterial chemoembolisation at the Department of Oncology of The Affiliated Huaian No.1 People’s Hospital of Nanjing Medical University between June 2015 and January 2020 were recruited and assigned to the case group. Simultaneously, patients matched to the case group in terms of gender and age but excluded for HCC were enrolled at a 1:1 ratio and classified as the control group. Relevant parameters were collected from both groups for comparison.
Results: Both AFP levels and ultrasound results demonstrated diagnostic value for patients with HCC (P < 0.05). Their combined use exhibited the highest diagnostic accuracy for the cancer, with an area under the curve of 0.896 (95% confidence interval [CI]: 0.876, 0.923), a sensitivity of 67.65% and a specificity of 91.22%. In terms of overall survival (OS), statistically significant differences in the OS rates were observed between the low-AFP (L-AFP) group and high-AFP (H-AFP) group as well as between the low-tumour-diameter (LTD) group and high-tumour-diameter (HTD) group (81.31% vs 52.22% and 85.11% vs 63.41%, respectively; P < 0.05). Regarding the progression-free survival (PFS), significant differences in the PFS rates were also noted between the L-AFP and H-AFP groups and between the LTD and HTD groups (81.31% vs 52.22% and 85.11% vs 63.41%, respectively; P < 0.05).
Conclusion: Ultrasound and AFP display notable distinctions when used in the diagnosis of HCC. The sensitivity of ultrasound as a standalone diagnostic tool surpasses that of AFP alone. However, their combined use results in much higher specificity than the use of either test individually. In addition, both techniques hold predictive value for patients’ OS and PFS, enabling timely prognostic assessment.
Keywords: alpha-fetoprotein, hepatocellular liver cancer, ultrasound, survival analysis, prognosis
Introduction
Hepatocellular liver cancer (HCC) is the fourth most prevalent tumour and the third leading cause of cancer mortality in China.1 Furthermore, China accounts for over 50% of new liver cancer cases globally annually, with this percentage steadily increasing.2 Every year, approximately 360,000 new cases of HCC and 350,000 related deaths occur in China.3 This clearly underscores the persistent and pressing public health concern posed by HCC in the country. Given the scarcity of liver sources for transplant, the prevailing treatment for liver cancer in China involves resection followed by postoperative chemotherapy despite a relatively high post-surgery recurrence rate. Relevant studies4 have reported a one-year survival rate of 84.3%, a three-year survival rate of 69.5%, a five-year survival rate of 39.4% and a median survival time of 50.14 months in patients with liver cancer post-surgery. Symptoms of HCC, particularly in its early stages, often lack specificity, leading many patients to seek medical care during the middle to late stages. To improve the early diagnosis rates of HCC, international liver disease prevention, diagnosis and treatment guidelines recommend that high-risk groups, including patients with chronic hepatitis and cirrhosis, undergo liver ultrasonography and serum alpha-fetoprotein (AFP) examinations at least once every six months for early HCC screening.
Currently, abdominal ultrasound is used as a routine method for liver cancer examination in hospitals, offering the advantages of affordability, convenience, non-invasiveness and minimal radiation exposure for clinical staff.5 However, this method can be easily affected by the operator’s skill level as well as machine sensitivity, lesion size and patient obesity.5 Conventional ultrasound has reported accuracy, specificity and sensitivity rates of 41%, 25% and 49%, respectively, in diagnosing HCC.6
Serum tumour marker examinations offer unique advantages, such as minimal invasiveness, cost-effectiveness, easy sampling and patient acceptability. Apart from its association with pathological grading, disease progression and prognosis regarding liver cancer,7,8 serum AFP also plays a confirmed role in the early screening and diagnosis of HCC,9 although its specificity and sensitivity remain suboptimal. Increased serum AFP levels can also result from active hepatitis and cirrhosis,10 which is a primary reason for AFP’s decreased specificity in screening high-risk groups for HCC. In addition, more than one-third of liver cancer cases have negative serum AFP levels, posing a negative impact on its sensitivity in early HCC screening. At present, there are varied views on the clinical value of serum AFP as an early screening indicator for HCC, both in China and abroad.
To enhance screening accuracy, some researchers have suggested integrated multi-marker screening approaches. For instance, if a patient has serum AFP levels of ≥400 μg/L and if common conditions such as pregnancy, chronic or active liver disease, gonadal embryonal tumours or digestive tract tumours are ruled out, there is a high probability of liver cancer. In cases of mildly elevated serum AFP, additional measures, such as imaging or dynamic monitoring, combined with liver function assessments, can be incorporated for the final diagnosis.11 However, there is a lack of conclusive evidence regarding the specific accuracies of ultrasound and AFP in detecting liver cancer and whether the combination of these methods is more accurate than using either individually. Therefore, this study aims to explore the epidemiological characteristics of serum AFP in liver cancer and the utility of combining AFP and ultrasound for early HCC screening and diagnosis. The findings from this study will contribute to the refinement of screening criteria and clinical applications.
Research Subjects and Methods
Subjects
A retrospective convenience sampling method was used to select 401 patients with HCC who underwent transarterial chemoembolisation (TACE) at the Department of Oncology of The Affiliated Huaian No.1 People’s Hospital of Nanjing Medical University between June 2015 and January 2020. These patients were enrolled in the case group. Simultaneously, patients who received ultrasound and AFP examinations during physical examinations or treatments at the hospital and were excluded for HCC based on clinical or pathological diagnosis were enrolled in the control group at a 1:1 ratio, matched with the case group by gender and age (within a two-year range). The inclusion criteria were (1) patients meeting the diagnostic criteria for HCC, which was confirmed by pathological examination; (2) no history of prior chemotherapy or radiotherapy; and (3) All patients needed to have been examined with the same instruments. The exclusion criteria were (1) hematologic diseases and/or (2) refusal of participation and (3) a history of other tumour diseases. This study was approved by the Ethics Committee of The Affiliated Huaian No.1 People’s Hospital of Nanjing Medical University with the ethics number JS-P-2015-023-01. Informed consent was obtained from all study subjects, and all enrolled patients provided written informed consent.
Methods
AFP testing: Fasting venous blood (4 mL) was collected, allowed to stand for 30 minutes and then centrifuged at 4000 rpm for 10 minutes to isolate the serum for storage at –25°C. Quantitative AFP detection based on chemiluminescence was performed using the Roche E411 analyser (Roche Group, Basel, Switzerland) along with matching Roche reagents, calibrators and quality control methods, with strict adherence to the operational instructions for the instrument and reagent kit.11
Ultrasound examination: Ultrasonography was performed using the GE LOGIQ 400 Pro Series black-and-white ultrasound system (United States) with a probe frequency of 2.0–5.0 MHz. Patients were examined in supine position on an empty stomach, maintaining this position throughout the examination. Longitudinal, oblique and transverse scans were performed using the left lateral probe, continuously sliding between the xiphoid process, right intercostal space and right subcostal region. Upon discovery of a lesion, the location, shape, size, internal echo intensity and various specific ultrasound features of the mass were documented.
Treatments: TACE: Following local anaesthesia, selective hepatic arteriography was conducted through the femoral artery. Once the tumour-feeding artery was identified, a mixture of iodised oil and pirarubicin was injected into the selected artery through a microcatheter. Gelatin sponge particles were used for selective embolisation of the feeding artery until complete occlusion of blood flow was achieved. Targeted immunotherapy: Patients were initially administered oral sorafenib once daily (with a starting dose of 12 mg for patients weighing ≥60 kg and 8 mg for patients <60 kg). After they had been taking sorafenib for 1–2 weeks, patients received the first TACE treatment (sorafenib was stopped three days prior). They resumed taking sorafenib three days after treatment. Intravenous infusion of 200 mg of camrelizumab was administered one week after TACE, followed by subsequent doses every two weeks (administered on day 1 of each cycle, with 14 days comprising one cycle).
Data Collection
The data collected included information on the patients’ gender, age, tumour diameter, tumour type, family history, drinking history, jaundice, ascites, cirrhosis, portal vein tumour thrombus, hepatitis virus presence, alanine aminotransferase (ALT) levels, Child–Pugh stage, AFP levels and ultrasound findings.
The follow-up procedures involved both telephone interviews and a review of medical records. For patients with complete clinical follow-up data, a comprehensive examination of their medical records was conducted to extract relevant clinical follow-up information from various admission times, ensuring that it met the study’s follow-up period requirements. In cases of patients with incomplete clinical follow-up data, the contact information was accessed from the baseline data to conduct follow-up telephone surveys and determine their survival status.
The information collected via follow-up mainly included the cause and time of death for deceased patients and information regarding local recurrence or distant metastasis, including the timing of such events for patients who survived.
The follow-up outcomes were categorised into recurrence/metastasis and death. The follow-up period was calculated from the day after surgery, where the progression-free survival (PFS) was defined as the time from postoperative day 1 to the first progression event and the overall survival (OS) as the time from day 1 to either the date of death or the date of the last follow-up. Patients who were lost to follow-up were censored at the date of the missed follow-up. The main prognostic indicators included 36-month OS and PFS rates.
Statistical Analysis
The statistical analysis was performed using SPSS 26.0. Normality was assessed using the K–S method. Normally distributed measurement data were expressed as the mean ± SD, and comparisons between the two groups were examined using the independent samples t-test. Count data were expressed as the frequency (n) or rate (%), and comparisons were assessed using the chi-squared test. The diagnostic value of AFP and ultrasound for HCC was evaluated by constructing ROC curves. Survival curves were generated using the Kaplan–Meier method, and Log rank tests were applied for comparisons. A significance level of α = 0.05 was used to determine statistical significance.
Results
Correlation Between Alpha-Fetoprotein and Characteristics of Hepatocellular Liver Cancer Cases
In total, 401 patients with HCC were enrolled in this study. Follow-up was completed for all 401 patients, with a follow-up period ranging from 5 to 36 months (median: 23.01 ± 6.52 months). Among the 300 AFP-positive cases, there were 167 males and 133 females, with a mean age of 45.38 ± 5.42 years and a mean tumour diameter of 5.12 ± 1.23 cm. Among the 101 AFP-negative cases, there were 54 males and 47 females, with a mean age of 46.78 ± 5.55 years and a mean tumour size of 3.31 ± 1.36 cm. Significant differences existed between the two groups regarding the tumour diameter (5.12±1.23 vs 3.31±1.36, t = 4.561, P < 0.001), ALT levels (53.51 ± 2.33 vs 48.41 ± 3.24, t = 3.452, P = 0.033), proportion with Child–Pugh grade C (29.67% vs 11.88%, χ2 = 15.340, P < 0.001) and proportion with viral hepatitis (48.33% vs 12.87%, χ2 = 39.797, P < 0.001). Conversely, no significant differences were observed between the two groups regarding gender, age, tumour type, family history, drinking history, jaundice, ascites, cirrhosis or portal vein tumour thrombus, and HCC staging (P > 0.05). See Table 1.
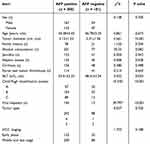 |
Table 1 Correlation Between AFP and Clinicopathological Characteristics of Primary Liver Cancer Cases |
Diagnostic Value of Alpha-Fetoprotein and Ultrasound for Hepatocellular Liver Cancer
The diagnostic value of AFP and ultrasound for HCC was evaluated using diagnostic results as the gold standard. The results showed that AFP and ultrasound have certain diagnostic value for patients (P < 0.05). When predicting the occurrence of HCC, ultrasound had an area under the curve (AUC) of 0.722 (95% confidence interval [CI]: 0.689, 0.756), with a sensitivity of 64.01%, a specificity of 73.82%, a positive predictive value (PPV) of 71.23, a negative predictive value (NPV) of 64.84 and a cutoff of 3.12 cm. The AFP levels had an AUC of 0.745 (95% CI: 0.723, 0.788), with a sensitivity of 31.32%, a specificity of 90.05%, a PPV of 75.84, an NPV of 56.77 and a cutoff of 368.87 ng/mL. The combined use of both ultrasound and AFP demonstrated the highest diagnostic value, with an AUC of 0.896 (95% CI: 0.876, 0.923), a sensitivity of 67.65%, a specificity of 91.22%, a PPV of 85.46 and an NPV of 59.49. See Table 2.
 |
Table 2 Diagnostic Value of AFP and Ultrasound for Primary Liver Cancer |
Effect of Alpha-Fetoprotein and Ultrasound Use on Overall Survival
The patients were categorised as follows according to the optimal cutoff values: the low AFP (L-AFP) group (<368.87 ng/mL) and the high AFP (H-AFP) group (≥368.87 ng/mL) as well as the low-tumour-diameter (LTD) group (<3.12 cm) and the-high-tumour diameter (HTD) group (≥3.12 cm). With recurrence as the endpoint, survival curves were constructed using the Kaplan–Meier method, and the Log rank test was employed to analyse differences in the recurrence rate across different indicator categories. In the case of AFP, a statistically significant difference in the OS rate was observed between the L-AFP and H-AFP groups (81.31% vs 52.22%, respectively; P < 0.05; see Figure 1A). In terms of ultrasound, there was a statistically significant difference in the OS rate between the LTD and HTD groups (85.11% vs 63.41%, respectively; P < 0.05; see Figure 1B).
 |
Figure 1 Effect of AFP and ultrasound on OS (A) OS curves of L-AFP and H-AFP groups. (B) OS curves of LTD and HTD groups. |
Effect of Alpha-Fetoprotein and Ultrasound Use on Progression-Free Survival
With recurrence as the endpoint, survival curves were constructed using the Kaplan–Meier method, and the Log rank test was employed to analyse differences in the recurrence rate across different indicator categories. For AFP, a statistically significant difference in the PFS rate was identified between the L-AFP group and the H-AFP group (81.31% vs 52.22%, respectively; P < 0.05; see Figure 2A). Regarding ultrasound, there was a statistically significant difference in the PFS rate between the LTD group and the HTD group (85.11% vs 63.41%, respectively; P < 0.05; see Figure 2B).
 |
Figure 2 Effect of AFP and ultrasound on PFS (A) PFS curves of L-AFP and H-AFP groups. (B) PFS curves of LTD and HTD groups. |
Discussion
Selective transcatheter arterial chemoembolisation (TACE) is a minimally invasive surgery, and is the first choice for treatment of advanced liver cancer that cannot be surgically removed. This treatment method involves percutaneous puncture of arterial blood vessels. After the target blood vessels of a liver tumour are selected with a catheter, chemotherapy drugs are infused through the catheter, and the blood supply of the tumour is blocked with embolic substances. This is an interventional therapy technique for “starving” tumour cells.12 As an important method for the clinical treatment of liver cancer, TACE mainly blocks the blood supply of the tumour by embolising its blood-supply artery, leading to tumour ischemia and hypoxia, inhibiting tumour growth, and promoting tumour cell necrosis and apoptosis. The whole process of TACE treatment is guided and monitored by imaging equipment, and the lesion can be accurately and directly reached through small wounds. Therefore, it has the advantages of being “minimally invasive, accurate, safe and efficient”.13,14
The primary diagnostic methods for HCC fall into three categories, as follows: cross-sectional imaging, serological diagnosis and pathological diagnosis. Imaging diagnosis comprises ultrasound, computed tomography (CT) and magnetic resonance imaging. These techniques not only hold crucial diagnostic value but can also assist in tumour grading and treatment plan evaluation.15 Ultrasonography, a common clinical screening and diagnostic method, offers real-time, repeatable, non-invasive, radiation-free (for patients) and cost-effective advantages.16 The principle of this technique is based on the fact that different fibrous tissues in the liver lead to varied ultrasound pulse absorption, attenuation and reflection, ultimately producing distinct images that aid in determining the benign or malignant nature of liver tumours.17 For patients with HCC, the average diameter of space-occupying lesions in the liver, as observed through ultrasound, is approximately 3.53 ± 1.88 cm, with 3.1-cm lesions being of the utmost diagnostic significance. A study by Ren et al also found that the average diameter of HCC is approximately 3.10 ± 1.70 cm, with HCC lesions measuring less than 3 cm constituting 67.7% of all cases.18 This observation highlights that a small lesion diameter on ultrasound does not rule out the possibility of HCC. The results of this study showed that relying solely on the diameter values generated from ultrasound displayed a relatively low diagnostic sensitivity. Several studies have confirmed that the sensitivity of HCC diagnosis using ultrasound alone is as low as 32.0%.19 In this study, the use of space-occupying liver lesion diameter from ultrasound for diagnosis had a sensitivity of 64.01%, aligning with the findings of other research works. This suggests that using lesion diameter obtained from ultrasound alone may offer a more advantageous approach to the diagnosis of HCC.
Alpha-fetoprotein is the most widely used tumour screening marker globally and serves as a primary indicator for screening HCC. When serum AFP levels exceed 200 ng/mL, there is a very high probability of a positive diagnosis as cirrhosis progresses to hepatic tumours.20 In this study, there were statistically significant differences between AFP-positive and AFP-negative patients in terms of tumour diameter (45.38 ± 5.42 vs 46.78 ± 5.55, respectively; t = 4.561, P < 0.001), ALT levels (53.51 ± 2.33 vs 48.41 ± 3.24, respectively; t = 3.452, P = 0.033), the proportion of patients classified as Child–Pugh grade C (29.67% vs 11.88%, respectively; χ2 = 15.340, P < 0.001) and the proportion of patients with viral hepatitis (48.33% vs 12.87%, respectively; χ2 = 39.797, P < 0.001). These findings suggest an association between the severity of a patient’s condition and the level of AFP. However, it is important to note that AFP alone is not a very strong diagnostic indicator. While AFP has a specificity of 90.0%, not all patients with HCC have increased AFP levels, and elevations are also observed in those with chronic liver disease.21 In addition to AFP, several other tumour markers have been identified as being significantly elevated in patients with HCC, including AFP-L3 fragments (which could be used to enhance the diagnostic specificity of AFP)22 and des-gamma-carboxy prothrombin (which could improve the accuracy of HCC diagnosis).23 In terms of cost and practicality, AFP is better suited for disease screening. In general, if a patient with chronic liver disease maintains a continuous AFP level exceeding 400 ng/mL for more than eight weeks, attention should be paid to the potential development of their condition, even if ultrasound or CT scans do not clearly indicate the presence of liver cancer. Monitoring dynamic changes in AFP levels, especially persistent elevations and recurring fluctuations, could benefit the early detection of HCC.11
Currently, AFP and ultrasound examinations are the most commonly used periodic screening methods for HCC. Franca et al pointed out that the ideal frequency of AFP and ultrasound examinations is either once every six months or once every three months after tumour discovery24 and that the both of results are highly complementary to each other. In the present study, the ultrasound and AFP results differed significantly and had poor consistency, indicating that the combined use of both could offset individual limitations. Moreover, some studies have proposed that combining ultrasound examination and AFP measurement could greatly aid the early detection of HCC development.25 In this study, only lesion diameter under ultrasound and levels of AFP were used in combination in the diagnosis of HCC, with a specificity of 96.3%. Several studies have suggested a relationship between AFP levels and tumour size under ultrasound, with larger tumours indicating a higher frequency of greater AFP levels and greater diagnostic value.26 Based on these findings, the combined use of both tumour diameter and AFP may become an important method in the field of early screening for HCC in the future. At the same time, this study demonstrated statistically significant differences in the OS and PFS between the L-AFP (<368.87 ng/mL) and H-AFP groups (≥368.87 ng/mL) and between the LTD (<3.12 cm) and HTD groups (≥3.12 cm) (all P < 0.05), indicating that ultrasound and AFP are valuable predictors of postoperative survival.
It should be noted that this study has limitations. To start, due to the limited source and small sample size, the results may lack representativeness for further extrapolation. This could be addressed through large multi-centre prospective cohort studies examining AFP changes in HCC. In addition, given the incidence of liver cancer, most of the liver cancer cases included in this study were HCC, with very few representing other types of liver cancer. Finally, this study did not explore the molecular mechanisms and clinical significance of AFP in HCC development, progression and diagnosis, warranting future investigation into AFP’s molecular functions.
Conclusions
In summary, ultrasound and AFP have significantly different results when used for the diagnosis of HCC. The sensitivity of ultrasound alone for diagnosis is higher than that of AFP alone. Notably, these techniques offer significantly greater specificity when used in combination than when used individually. In addition, both techniques hold predictive value for patients’ OS and PFS, enabling timely prognostic assessment.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of the Affiliated Huaian No.1 People’s Hospital of Nanjing Medical University (JS-P-2015-023-01).
Funding
2012 Science and Technology Support Program of Huai’an Science and Technology Bureau: Combining with public health information platform to carry out research on secondary prevention of liver cancer (No. HAS2012014).
Disclosure
All of the authors had no any personal, financial, commercial, or academic conflicts of interest separately for this work.
References
1. Xia C, Dong X, Li H, et al. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin Med J. 2022;135(5):584–590. doi:10.1097/CM9.0000000000002108
2. Liu SS, Ma XF, Zhao J, et al. Association between nonalcoholic fatty liver disease and extrahepatic cancers: a systematic review and meta-analysis. Lipids Health Dis. 2020;19(1):118. doi:10.1186/s12944-020-01288-6
3. Poon D, Anderson BO, Chen LT, et al. Management of hepatocellular carcinoma in Asia: consensus statement from the Asian Oncology Summit 2009. Lancet Oncol. 2009;10(11):1111–1118. doi:10.1016/S1470-2045(09)70241-4
4. Zhao HB. Application of medical imaging in liver cancer diagnosis. Imaging Research and Medical Application. 2019;3(4):56–57.
5. Chiang JK, Chih-Wen L, Kao YH. Effect of ultrasonography surveillance in patients with liver cancer: a population-based longitudinal study. BMJ Open. 2017;7(6):e015936. doi:10.1136/bmjopen-2017-015936
6. Pocha C, Dieperink E, McMaken KA, et al. Surveillance for hepatocellular cancer with ultrasonography vs. computed tomography -- a randomised study. Aliment Pharmacol Ther. 2013;38(3):303–312. doi:10.1111/apt.12370
7. Bai DS, Zhang C, Chen P, et al. The prognostic correlation of AFP level at diagnosis with pathological grade, progression, and survival of patients with hepatocellular carcinoma. Sci Rep. 2017;7(1):12870. doi:10.1038/s41598-017-12834-1
8. Xie QS, Chen ZX, Zhao YJ, et al. Systematic review of outcomes and meta-analysis of risk factors for prognosis after liver resection for hepatocellular carcinoma without cirrhosis. Asian J Surg. 2021;44(1):36–45. doi:10.1016/j.asjsur.2020.08.019
9. Choi J, Tayob N, Lim YS. Detecting early hepatocellular carcinoma in patients with chronic hepatitis B using longitudinal α-fetoprotein screening. Clin Gastroenterol Hepatol. 2023;21(6):1590–1597. doi:10.1016/j.cgh.2022.08.018
10. Yen YH, Kee KM, Li WF, et al. Stationary trend in elevated serum alpha-fetoprotein level in hepatocellular carcinoma patients. Cancers (Basel). 2023;15(4):1222. doi:10.3390/cancers15041222
11. Hanif H, Ali MJ, Susheela AT, et al. Update on the applications and limitations of alpha-fetoprotein for hepatocellular carcinoma. World J Gastroenterol. 2022;28(2):216–229. doi:10.3748/wjg.v28.i2.216
12. Hatanaka T, Arai H, Kakizaki S. Balloon-occluded transcatheter arterial chemoembolization for hepatocellular carcinoma. World J Hepatol. 2018;10(7):485–495. doi:10.4254/wjh.v10.i7.485
13. Liu X, Xie Y, Qi X, Xu K. Transcatheter arterial chemoembolization (TACE) with iRGD peptide in rabbit VX2 liver tumor. J Cancer Res Ther. 2020;16(7):1703–1709. doi:10.4103/jcrt.JCRT_1411_20
14. Zhao W, Xu J, You Y, et al. Thermoresponsive hydrogel for transcatheter arterial chemoembolization of hepatocellular carcinoma. Chem Commun. 2023;59(61):9352–9355. doi:10.1039/d3cc02257a
15. Wang CH, Wey KC, Mo LR, et al. Current trends and recent advances in diagnosis, therapy, and prevention of hepatocellular carcinoma. Asian Pac J Cancer Prev. 2015;16(9):3595–3604. doi:10.7314/apjcp.2015.16.9.3595
16. Tanaka H. Current role of ultrasound in the diagnosis of hepatocellular carcinoma. J Med Ultrason. 2020;47(2):239–255. doi:10.1007/s10396-020-01012-y
17. Jia PF, Gao WP. Malignant liver cancer ultrasonic image processing and analysis based on MATLAB. Tissue Engineering Research and Clinical Rehabilitation. 2009;13(43):8523–8526. doi:10.3969/j.issn.1673-8225.2009.43.026
18. Ren FY, Piao XX, Jin AL. Efficacy of ultrasonography and alpha-fetoprotein on early detection of hepatocellular carcinoma. World J Gastroenterol. 2006;12(29):46564659. doi:10.3748/wjg.v12.i29.4656
19. Demirtas CO, Gunduz F, Tuney D, et al. Annual contrast-enhanced magnetic resonance imaging is highly effective in the surveillance of hepatocellular carcinoma among cirrhotic patients. Eur J Gastroenterol Hepatol. 2020;32(4):517–523. doi:10.1097/MEG.0000000000001528
20. Wang X, Zhang Y, Yang N, et al. Evaluation of the combined application of AFP, AFP-L3%, and DCP for hepatocellular carcinoma diagnosis: a meta-analysis. Biomed Res Int. 2020;2020:5087643. doi:10.1155/2020/5087643
21. Yu M, Huang L, Zhang S, et al. Follow-up value of serum AFP and aminotransferases in chronic hepatitis B progression. Front Cell Infect Microbiol. 2023;13:1082390. doi:10.3389/fcimb.2023.1082390
22. Zhao Y, Liu Q, Qin Y, et al. Ordered labeling-facilitated electrochemical assay of alpha-fetoprotein-L3 ratio for diagnosing hepatocellular carcinoma. ACS Appl Mater Interfaces. 2023;15(5):6411–6419. doi:10.1021/acsami.2c19231
23. Zhang X, Wu LN, Li XQ, et al. Whether the Golgi protein 73 could be a diagnostic serological marker in hepatocellular carcinoma: a meta analysis. BMC Gastroenterol. 2023;23(1):85. doi:10.1186/s12876-023-02685-8
24. Bureau of Medical Administration, National Health Commission of the People’s Republic of China. [Standardization for diagnosis and treatment of hepatocellular carcinoma (2022 edition)]. Zhonghua Gan Zang Bing Za Zhi. 2022;30(4):367–388. Chinese. doi:10.3760/cma.j.cn501113-20220413-00193
25. Urhuț MC, Săndulescu LD, Ciocâlteu A, et al. The clinical value of multimodal ultrasound for the differential diagnosis of hepatocellular carcinoma from other liver tumors in relation to histopathology. Diagnostics. 2023;13(20):3288. doi:10.3390/diagnostics13203288
26. Zhou JM, Wang T, Zhang KH. AFP-L3 for the diagnosis of early hepatocellular carcinoma: a meta-analysis. Medicine. 2021;100(43):e27673. doi:10.1097/MD.0000000000027673
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
