Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 16
Usefulness of Lung Ultrasound as a Method for Early Diagnosis of Interstitial Lung Disease in Patients with Rheumatoid Arthritis
Authors Santos-Moreno P , Linares-Contreras MF, Rodríguez-Vargas GS, Rodríguez-Linares P , Mata-Hurtado A, Ibatá L, Martínez S, Rojas-Villarraga A, Diaz M, Vicente-Rabaneda EF, Quintero M, Möller I
Received 23 September 2023
Accepted for publication 28 December 2023
Published 17 January 2024 Volume 2024:16 Pages 9—20
DOI https://doi.org/10.2147/OARRR.S441720
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Chuan-Ju Liu
Pedro Santos-Moreno,1 Maria Fernanda Linares-Contreras,1 Gabriel-Santiago Rodríguez-Vargas,2 Pedro Rodríguez-Linares,2 Abdón Mata-Hurtado,3 Linda Ibatá,4 Susan Martínez,4 Adriana Rojas-Villarraga,1,5 Mario Diaz,1 Esther F Vicente-Rabaneda,6 Maritza Quintero,7 Ingrid Möller7
1Rheumatology Department, Biomab IPS, Bogotá, Colombia; 2Research department, Biomab IPS, Bogotá, Colombia; 3Fundación Neumológica Colombiana, Bogotá, Colombia; 4Epidemiology department, Biomab IPS, Bogotá, Colombia; 5Research Institute, Fundación Universitaria de Ciencias de La Salud – FUCS, Bogotá, Colombia; 6Rheumatology, Hospital Universitario La Princesa, Madrid, Spain; 7POAL Rheumatology Institute, Rheumatology, Barcelona, Spain
Correspondence: Pedro Santos-Moreno, Rheumatology department, Biomab IPS, 48th Street #13-86, Bogotá, 110221, Colombia, Tel +57 320 8094232, Email [email protected]
Purpose: To determine the value of lung ultrasound (LUS) compared to high-resolution computed tomography (HRCT) in the early diagnosis of interstitial lung disease (ILD) in patients with rheumatoid arthritis (RA).
Patients and Methods: An observational prospective study was performed. Were included patients with respiratory symptoms or/and, patients with crackles in auscultation during medical consultation. All patients underwent to chest X-rays, LUS, HRCT,and respiratory function tests.
Results: A total of 192 patients with RA were included. Mean disease duration was 16.8 ± 11.1 years. 72% were positive for rheumatoid factor or anti-citrullinated antibodies. Of the total number of subjects, 54.7% had respiratory symptoms. The other patients did not have respiratory symptoms, but they did have had crackles on pulmonary auscultation. B lines > 11.5 on the ROC curve predicted ILD (AUC 0.63; CI 95%: 0.55– 0.71; p < 0.003). A DLCO value of < 7.13 significantly predicted the presence of ILD (AUC 0.61; 95% CI: 0.52– 0.70; p < 0.028).
Conclusion: The findings of this study suggest that LUS is a valuable tool for the early diagnosis of ILD in patients with RA, and together with DLCO, can adequately predict the presence of ILD in this population. LUS also helps to determine which patients with respiratory symptoms and signs suggestive for ILD are undergo to HRCT.
Keywords: rheumatoid arthritis, interstitial lung diseases, respiratory function tests
Introduction
Rheumatoid arthritis (RA) is a progressive systemic autoimmune disorder characterized by joint and extra-articular manifestations. RA-related pulmonary involvement is the most frequent extra-articular manifestation as it occurs in up to 40% of patients with RA.1–3 Lung involvement in RA often occurs within the first five years of the disease.4 Still, it can precede joint symptoms in up to 20% of cases, and respiratory symptoms characterize them it.5–7 Among the pulmonary findings in RA, interstitial lung disease (ILD) stands out.8 The risk increases with the prolonged duration of RA and active joint RA.9
The global incidence of ILD has remained stable despite of the decrease in the frequency of other extra-articular manifestations of RA.10 The prevalence of ILD varies from 10% to 42% or more in different series,11,12 depending on the population studied, clinical, radiographic, and functional criteria to establish the diagnosis.13 On the other hand, clinical significance in ILD is identified in 2% to 10% of RA patients, but reported estimates vary due to the heterogeneity of RA, genetic susceptibility, differences in disease definition, and detection methods.7,14,15
RA associated with ILD (RA-ILD) stands out as the most prevalent extra-articular manifestation of rheumatoid arthritis. It imposes a significant burden on morbidity and mortality, with prognosis varying based on the extent of pulmonary involvement in individual patients. Early identification of this extra-articular manifestation, along with the assessment of risk and progression factors can prove advantageous in light of its considerable impact.16 Thus, in a study conducted by Zhuo J et al,16 which assessed the prevalence and prognostic factors of RA-ILD using data from the Discus Analytics JointMan database spanning from 2009 to 2019, it was found that several key risk factors were associated with RA-ILD. These factors included being older than 65 years, male gender, seropositivity for anti-citrullinated antibodies (anti-CCP) along with moderate disease activity, and elevated C-reactive protein (CRP). The presence of these factors correlated with an increased likelihood of disease, and consequently, a more unfavorable prognosis. In other similar study, identified 3 factors related to disease progression in patients with RA-ILD: age, MMP-13 and CXCL11.17 A multicenter cross-sectional study conducted by Cano-Jiménez et al,18 it was discovered that a delay in diagnosis emerged as an independent predictor of mortality. Age, DLCO levels, and others were also identified as significant predictors of mortality. This underscores the importance of developing tools capable of early disease detection, as such interventions have the potential to enhance outcomes and prevent the mortality associated with this extra-articular manifestation.
For ILD, there are no studies that validate a specific early diagnosis way.19 Chest radiography (CXR) is commonly performed in RA, particularly for the diagnosis of lung disease. Abnormalities have been identified in 79% of CXR in RA patients, and 4.6% have pulmonary abnormalities.20 CXR has a low sensitivity in detecting ILD. Although small reticular and nodular opacities could be seen in the lower lung areas. Radiographic findings are not frequent in the early stages.21 Up to 64% of patients with ILD on high-resolution computed tomography (HRCT) will not present evident interstitial changes on CXR.22
HRCT provides valuable information on ILD, including the pattern and extent of disease, assessment of progression over time, and evaluation of extra-parenchymal abnormalities.23 Pulmonary abnormalities have been reported in 47%–67% of RA patients examined by HRCT.24,25 ILD, respiratory diseases, and bronchiectasis are frequent findings. Although nonnegligible doses of ionizing radiation limit its use, HRCT is accepted as the gold standard in diagnosing ILD in patients with RA.26,27 In addition, HRCT is the reference standard to validate the diagnostic accuracy of other tools in patients with RA.28
Current data have shown that Lung ultrasound (LUS) can be helpful in the detection of ILD by evaluating B lines, the ultrasound marker of pulmonary interstitial syndrome.29 Previous studies have shown that B lines have good diagnostic precision, high sensitivity, and correlate well with HRCT findings, suggesting that LUS is a novel, noninvasive and nonionizing imaging method, less expensive than HRCT.30 The aim of this study is to determine the usefulness of LUS regarding to HRCT in the early diagnosis of ILD in patients with RA, mainly in a local context where is an accessible, and affordable tool that allows the earlier detection of ILD, in order to make a better selection of patients who are candidates for HRCT.
Materials and Methods
Design and Study Population
This observational prospective study was conducted in a single specialized center in RA in Colombia. Adults (age ≥ 18 years) with a diagnosis of RA according to the 2010 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) criteria,31 and respiratory signs and symptoms that might suggest the presence of ILD in RA, who were followed at the center between October 2020 and October 2021 were included. Respiratory symptoms include: shortness of breath, especially with exertion, fatigue and weakness, loss of appetite, nonproductive chronic dry cough, chest discomfort, and shortness of breath (not explained by another condition) with a duration longer than two months. Respiratory signs mainly included the presence of crackles during auscultation at medical appointments. Pregnant women and patients diagnosed with pneumonia in the last month, chronic obstructive pulmonary disease, moderate or severe pleural effusion, atelectasis, or other types of previous pulmonary interstitial involvement due to connective tissue disease were excluded. Patients with a history of COVID-19 infection were also excluded.
Study Outcomes and Procedures
To evaluate the diagnostic usefulness of LUS and CXR against HRCT in the detection of ILD, the results of each test were compared. To characterize the population with ILD and determine the possible association between the patient’s serological status, the onset of the disease and the previous use of methotrexate and the presence of ILD, demographic characteristics, medical history, RA characteristics, use of medications, respiratory symptoms, and physical examination findings were collected. LUS examinations were conducted using a MyLab seven® (Esaote – Italy) equipped with a 2–5-MHz convex transducer. One pulmonologist and one rheumatologist with expertise in LUS performed all examinations. The scanning protocol involved a comprehensive examination of all intercostal spaces, divided in these areas: anterior, posterior and lateral on each side based on Volpicelli protocol.32 Abnormalities, such as B-lines that are define as discrete laser-like vertical hyperechoic reverberation artifacts that arise from the pleural line were documented from each thoracic area.32 In the context of RA-ILD, there no exists standardized quantification for LUS and pathological B-line count. For this study, the following cutoff points were utilized: mild B-line involvement was designated with 6–15 lines, moderate involvement with 16–30 lines, and severe involvement with more than 30 lines. For HRCT, pulmonary involvement was assessed using the Warrick score which combines values assigned to five keys radiological ILD findings (ranging from 0 to 5) and their extent (ranging from 0 to 3). A validated minimum score of 7 identified as the optimal cutoff point for predicting pulmonary disease in ILD.33 Pulmonary function tests were included for evaluations of forced vital capacity (FVC), forced expiratory volume in one second (FEV1) and diffusing capacity of the lungs for carbon monoxide (DLCO). Concerning DLCO measurement, were considered predicted absolute value corrected/adjusted for barometric pressure in Bogota (Colombia), along with factors, such as height, sex, hemoglobin value, and alveolar volume. Furthermore, were taken into account the percentage of predicted values for each corrected/adjusted absolute value. Consequently, there is no specific cut-off point for the absolute value of corrected DLCO, as it varies based on the unique clinical characteristics of each patient for whom DLCO is being corrected.
Information Collection and Monitoring
Patients were recruited consecutively according to the selection criteria and until an estimated sample size was completed. The data collection was carried out in a predetermined case report form (CRF), where the information of the variables of interest and the results of the tests were recorded, completing the data from the medical records. Once the information was collected in the CRF, the data were recorded in an electronic database and validated with the medical records.
Diagnostic images and lung function tests were performed with standard equipment, following ACR criteria, and the recommendations of the American Thoracic Society and European Respiratory Society Technical Statement.34–36 One pneumologist performed the interpretation of the LUS, CXR and HRCT imaging tests in a blinded manner.
Patients diagnosed with ILD continued medical care to receive standard treatment and corresponding follow-up.
Data Analysis
A descriptive analysis was performed, the results of which are presented as the means (± standard deviation [SD]) or medians (with interquartile range [IQR]) for continuous variables, while categorical variables are expressed with frequencies and percentages. Bivariate chi-square analyses were used to determine possible associations between variables and the presence of ILD. Optimal cut-off points for DLCO based on ROC curves and the area under the curve (AUC) were evaluated. Two-tailed p < 0.05 values were considered statistically significant.
Sensitivity and specificity, with their respective 95% confidence intervals (CIs), were calculated for LUS and CXR, with HRCT as the reference standard. False-positive and false-negative rates, predictive values and likelihood ratios were calculated. All statistical analyses will be performed with the R software package.37
The study was carried out in accordance with the Standards for Reporting Diagnostic Accuracy Studies.38 This study was conducted following the principles of the Declaration of Helsinki and was approved by the Research Ethics Committee on Human Beings – Hospital de San José, Bogota, Colombia (Record 0085–2021, February 19th 2021). All patients signed informed consent before the procedures specified by the protocol.
Results
A total of 197 subjects were enrolled in the study; 4 patients did not complete the study due to significant noncompliance, and 1 patient withdrew their consent. Thus, a total of 192 were included (151 women, age: 69 ± 9 years) in whom it was possible to perform all the corresponding imaging tests. The characteristics of the subjects in the cohort are described in Table 1. Most of them tested positive for rheumatoid factor (80%) and anti-CCP (74%). The average evolution of RA was 16.8 ± 11.1 years. The average disease activity measured by DAS28 was 2.5 ± 1.1. A total of 44.3% of the patients had a history of smoking. Regarding treatment with conventional drug modifying rheumatic drugs (csDMARDs), the use of methotrexate (64.6%) and leflunomide (47.9%) were predominating. Among the tumor necrosis factor inhibitors (TNFi) agents, the most frequently prescribed were etanercept (4.7%) and certolizumab (4.7%). The most widely used non-TNFi biologic was abatacept (6.3%).
 |
Table 1 Demographic and Clinical Characteristics of the Study Population |
Evaluation of ILD in the Cohort of Patients with RA
HRCT detected ILD in 117 of 192 (60.9%) subjects in the study cohort. The LUS identified ILD (Lines B) signs in 179 of 192 (93.2%) subjects. The overall agreement between LUS and HRCT was 65.6%. For LUS, the sensitivity concerning HRCT was 98.3%, while the specificity was 14.7%. In patients with positive LUS for ILD, 86.5% showed moderate or severe interstitial involvement, and 93.3% showed irregularity in pleural lines. There were no significant differences in the distribution of all B lines between the categories of the Warrick extension index in the HRCT (p 0.925). On the other hand, the sensitivity and specificity of chest radiography with respect to HRCT were 29.9% and 94.7%, respectively. The overall concordance between the chest radiograph and HRCT was 55.2% (see Table 2). The results of the diagnostic usefulness of LUS and chest radiography in comparison with HRCT in detecting ILD and the description of the imaging findings are presented in Tables 2 and 3.
 |
Table 2 Diagnostic Usefulness of LUS and CXR Compared to HRCT in the Diagnosis of ILD |
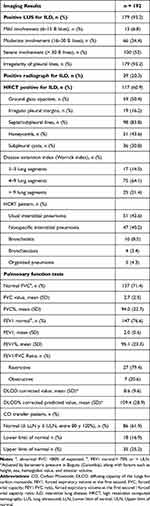 |
Table 3 Imaging Results and Lung Function in the Rheumatoid Arthritis Patients |
In 64 cases, there was no concordance between the LUS and HRCT findings (97% of the discordant cases were false positives in the LUS). The analysis of the characteristics of the false positives, false negatives, true positives and true negatives in the LUS is presented in Table 4. The false positives of the presented a normal CXR in 83.6% of cases. No statistically significant differences were found between the groups in age, BMI, smoking, or symptoms, such as chronic cough or fatigue. The severe involvement in lines B, and the irregularity of pleural lines were associated with true positive diagnosis of ILD in LUS regarding HRCT.
 |
Table 4 Characterization of Subjects with False Positives for Interstitial Lung Disease at Lung Ultrasound |
The analysis of potential associations of different factors with the presence of ILD showed that the findings in the LUS and the corrected DLCO had statistically significant differences between the groups with or without the disease. The corrected DLCO was significantly lower in patients with ILD than those without the disease (6.8 versus 7.7, p < 0.028). Sex, age, time of evolution of RA, use of methotrexate, seropositivity, and smoking history were not significantly related to the presence of ILD (see Supplementary Data).
No statistical analysis was conducted to combine DLCO and LUS for predicting RA-ILD. Instead, the use of ROC curves aimed to identify the optimal cut-off point for each test, assessing their effectiveness in predicting the presence of RA-ILD. Therefore, in ROC curve analysis, the number of total B lines (AUC 0.63; 95% CI: 0.55–0.71; p < 0.003) and the corrected DLCO value (AUC 0.61; CI 95%: 0.52–0.70; p < 0.028) significantly predicted the presence of ILD on HRCT (see Figure 1). The value of 11.5 was identified as the B-line count with the best discriminatory balance, with a sensitivity of 93%. Regarding the corrected DLCO, the value of 7.13 was identified with the best balance of sensitivity (69%) of ILD in subjects with RA.
 |
Figure 1 ROC curves for the prediction of ILD with total B lines and DLCO in subjects with Rheumatoid arthritis. Abbreviation: DLCO, diffusing capacity of the lungs for carbon monoxide. |
Discussion
LUS showed high sensitivity/low specificity for the detection of RA-ILD regarding to the gold standard, which is HRCT. Therefore, being a more accessible technology, it is an assertive method for an initial approach to the diagnosis of RA-ILD. It is worth noting that the number of B lines and the corrected DLCO value allow a better discrimination in the diagnosis of RA-ILD.
In the cohort, 78.6% of the patients with ILD were women. Other reports for this same condition have shown a male/female ratio of 2:1.39,40 Regarding age, patients with ILD had a mean age of 71 years, while other cohorts have reported the onset of lung disease in earlier decades of life (less than 60 years),10 which could suggest a late diagnosis of the disease in this cohort.
As part of the follow-up of RA, patients who show respiratory symptoms should undergo a pulmonary evaluation, which is a challenge due to the various potential causes that can present concomitantly with RA, such as ILD, chronic obstructive pulmonary disease, bronchiectasis, respiratory infections after immunosuppressive therapies, drug-induced pulmonary toxicity, and ischemic heart disease.24,25 Survival in patients with RA has improved in recent years, but patients with ILD associated with RA have a significantly lower survival than patients with RA alone.7,41,42 Therefore, an early diagnosis of ILD by using more affordable radiological techniques and a greater awareness of ILD could offer an earlier diagnosis of RA-ILD, estimated between three and ten years.43,44
In this study, it was observed that 60.9% of the patients with RA had a diagnosis of ILD by HRCT, while by LUS, this figure increased to 93%. The high sensitivity of LUS in ILD is a finding already reported in other studies.45 In the analysis of the ROC curve, the number of total B lines of 11.5 had the best discriminatory balance, with a sensitivity of 93%. With a cut-off point of 10 lines B, it has been documented that ultrasound could be more sensitive than HRCT for the diagnosis of RA-ILD.46,47 This is also shown by other authors who have described a low sensitivity (62.2%) with a cut-off point of 5.5 lines.45
Although a high number of false-positives was evidenced, the concordance between LUS and HRCT was 65.6%, which may guide the use of LUS as a first approach to evaluate the pulmonary parenchyma in patients with suspected RA-ILD. However, the use of HRCT is the gold standard to evaluate interstitial involvement and its extension area throughout the lung parenchyma in patients with suspected ILD.45 In the present study, specificity was influenced by a false positive rate (specificity 14%). Similar findings are reported in other studies,48,49 where specificity is less than 40%. However, the majority of studies report higher specificity.50 It is important to clarify that specificity is not solely affected by false positives but also by the sociodemographic characteristics of populations and the inherent operator-dependent nature of LUS, which can introduce variability in the results.
On the other hand, studies have shown that RA patients who underwent a screening procedure regardless of the presence of respiratory symptoms often had radiological abnormalities on HRCT, called interstitial lung abnormalities. One-third of these patients have subclinical disease with varying degrees of functional impairment.39,51 Therefore, the LUS can be used as a test with lower radiological risk, lower cost and easy availability, although there are still no studies that validate the use of this test within a specific screening way for ILD.19
Studies with CXR have reported a ILD positivity rate of 1% to 6%, while investigations with HRCT report a greater number of cases (5% to 67.3%).52,53 In line with previous studies, this study showed the low sensitivity and high specificity of CXR compared to HRCT, but the high sensitivity of lung ultrasound, evidenced in other studies (89% −97%),46,47 it could suggest the complementary use of these two tests in pulmonary evaluation in patients with RA,54 since the diagnostic criteria to define ILD do not affect the sensitivity but influence the specificity.55
On the other hand, the corrected DLCO value significantly predicted the presence of ILD in the HRCT estimated by the AUC. This predictor variable has also been identified in other studies suggesting DLCO as a tool that can measure the presence and progression of interstitial involvement as well as survival in patients with RA-ILD.23 It is acknowledged that DLCO can serve as a test for evaluating lung function; however, its measurement tends to vary across different populations and measurement sites, despite its widespread use. Various studies, including the present investigation, have endeavored to establish cut-off points for predicting the presence of RA-ILD.56 Nevertheless, additional analyses are warranted in this regard with due consideration given to the diverse characteristics of the population under study. This study has some limitations. First, the study sample excluded patients with other respiratory comorbidities, such as chronic obstructive pulmonary disease, that could be common in clinical practice. Another limitation is inherent in performing ultrasound since the diagnostic accuracy and performance characteristics of LUS depend in part on the examination scheme and the operator. Therefore, this technique has variable performance in clinical practice.57 Although intra- and interobserver reliability requires an evaluation with respect to the variability in the acquisition of the images and not only in their interpretation, they generally place the LUS in the range of good to excellent.55 To minimize this risk, a standardized procedure was established for the LUS diagnosis of ILD, and the professionals were trained in the performance of the specific technique. As strengths, this study included a larger cohort than previous studies, and it was performed in a context with restricted resources.45–47,54
Conclusion
In conclusion, the findings suggest that LUS is a useful tool for the detection of ILD in RA and, together with DLCO, can adequately predict the presence of ILD in patients with RA. However, these tests are not a substitute for HRCT to confirm the diagnosis, quantify the extent, and assess the progression of ILD. Future studies should evaluate larger cohorts, the cost-effectiveness of the test, and the performance of LUS in the follow-up of patients already diagnosed with RA-ILD.
Acknowledgments
The authors would like to thank Fernando Rodríguez-Florido, who help in the figure design.
Disclosure
Dr Pedro Santos-Moreno reports grants, personal fees from Bristol, personal fees, non-financial support from Abbvie, personal fees, non-financial support from Janssen, personal fees, non-financial support from Pfizer, personal fees, non-financial support from Biopas – UCB. Dr Adriana Rojas-Villarraga reports grants from Asociación Colombiana de Reumatología, Fees for conferences from Amgen Fees for conferences and advisory board from Janssen, Fees for conferences from Pfizer, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Yunt ZX, Solomon JJ. Lung disease in rheumatoid arthritis. Rheum Dis Clin North Am. 2015;41(2):225–236. doi:10.1016/j.rdc.2014.12.004
2. Esposito AJ, Chu SG, Madan R, Doyle TJ, Dellaripa PF. Thoracic Manifestations of Rheumatoid Arthritis. Clin Chest Med. 2019;40(3):545–560. doi:10.1016/j.ccm.2019.05.003
3. Turesson C, O’Fallon WM, Crowson CS, Gabriel SE, Matteson EL. Extra-articular disease manifestations in rheumatoid arthritis: incidence trends and risk factors over 46 years. Ann Rheum Dis. 2003;62(8):722–727. doi:10.1136/ard.62.8.722
4. Zamora-Legoff JA, Krause ML, Crowson CS, Ryu JH, Matteson EL. Patterns of interstitial lung disease and mortality in rheumatoid arthritis. Rheumatology. 2017;56(3):344–350. doi:10.1093/rheumatology/kew391
5. O’Dwyer DN, Armstrong ME, Cooke G, Dodd JD, Veale DJ, Donnelly SC. Rheumatoid Arthritis (RA) associated interstitial lung disease (ILD). Eur J Intern Med. 2013;24(7):597–603. doi:10.1016/j.ejim.2013.07.004
6. Singh K, Al-Sadawi M, Ortega RR, et al. Interstitial Lung Disease as the Initial Manifestation of Rheumatoid Arthritis: a Case Report and Review of the Literature. Am J Med Case Rep. 2019;7(12):342–347. doi:10.12691/ajmcr-7-12-10
7. Hyldgaard C, Hilberg O, Pedersen AB, et al. A population-based cohort study of rheumatoid arthritis-associated interstitial lung disease: comorbidity and mortality. Ann Rheum Dis. 2017;76(10):1700–1706. doi:10.1136/annrheumdis-2017-211138
8. Farquhar H, Vassallo R, Edwards AL, Matteson EL. Pulmonary Complications of Rheumatoid Arthritis. Semin Respir Crit Care Med. 2019;40(2):194–207. doi:10.1055/s-0039-1683995
9. Sparks JA, He X, Huang J, et al. Rheumatoid Arthritis Disease Activity Predicting Incident Clinically Apparent Rheumatoid Arthritis-Associated Interstitial Lung Disease: a Prospective Cohort Study. Arthritis Rheumatol. 2019;71(9):1472–1482. doi:10.1002/art.40904
10. Shaw M, Collins BF, Ho LA, Raghu G. Rheumatoid arthritis-associated lung disease. Eur Respir Rev. 2015;24(135):1–16. doi:10.1183/09059180.00008014
11. Habib HM, Eisa AA, Arafat WR, Marie MA. Pulmonary involvement in early rheumatoid arthritis patients. Clin Rheumatol. 2011;30(2):217–221. doi:10.1007/s10067-010-1492-5
12. Dong H, Julien PJ, Demoruelle MK, Deane KD, Weisman MH. Interstitial lung abnormalities in patients with early rheumatoid arthritis: a pilot study evaluating prevalence and progression. Eur J Rheumatol. 2018;6(4):193–198. doi:10.5152/eurjrheum.2019.19044
13. Brito Y, Glassberg MK, Ascherman DP. Rheumatoid Arthritis-Associated Interstitial Lung Disease: current Concepts. Curr Rheumatol Rep. 2017;19(12). doi:10.1007/s11926-017-0701-5
14. Raimundo K, Solomon JJ, Olson AL, et al. Rheumatoid Arthritis-Interstitial Lung Disease in the United States: prevalence, Incidence, and Healthcare Costs and Mortality. J Rheumatol. 2019;46(4):360–369. doi:10.3899/jrheum.171315
15. Zou YQ, Li YS, Ding XN, Ying ZH. The clinical significance of HRCT in evaluation of patients with rheumatoid arthritis-associated interstitial lung disease: a report from China. Rheumatol Int. 2012;32(3):669–673. doi:10.1007/s00296-010-1665-1
16. Zhuo J, Lama S, Knapp K, et al. Epidemiology and clinical characteristics of interstitial lung disease in patients with rheumatoid arthritis from the JointMan database. Sci Rep. 2023;13(1):1–11. doi:10.1038/s41598-023-37452-y
17. Chen J, Chen Y, Liu D, et al. Predictors of long-term prognosis in rheumatoid arthritis-related interstitial lung disease. Sci Rep. 2022;12(1):1–11. doi:10.1038/s41598-021-99269-x
18. Cano-Jiménez E, Vázquez Rodríguez T, Martín-Robles I, et al. Diagnostic delay of associated interstitial lung disease increases mortality in rheumatoid arthritis. Sci Rep. 2021;11(1):1–11. doi:10.1038/s41598-021-88734-2
19. Bendstrup E, Møller J, Kronborg-White S, Prior TS, Hyldgaard C. Interstitial Lung Disease in Rheumatoid Arthritis Remains a Challenge for Clinicians. J Clin Med. 2019;8(12):2038. doi:10.3390/jcm8122038
20. Goggins MR, Conway R, Durcan LJ, Johnston C, Cunnane G. High prevalence of abnormalities on chest radiography in rheumatoid arthritis. Clin Rheumatol. 2019;38(12):3375–3380. doi:10.1007/s10067-019-04717-9
21. Bes C. Comprehensive review of current diagnostic and treatment approaches to interstitial lung disease associated with rheumatoid arthritis. Eur J Rheumatol. 2019;6(3):146. doi:10.5152/eurjrheum.2019.19036
22. Bilgici A, Ulusoy H, Kuru O, Çelenk C, Ünsal M, Danaci M. Pulmonary involvement in rheumatoid arthritis. Rheumatol Int. 2005;25(6):429–435. doi:10.1007/s00296-004-0472-y
23. Nurmi HM, Kettunen HP, Suoranta SK, et al. Several high-resolution computed tomography findings associate with survival and clinical features in rheumatoid arthritis-associated interstitial lung disease. Respir Med. 2018;134:24–30. doi:10.1016/j.rmed.2017.11.013
24. Skare TL, Nakano I, Luiz Escuissiato D, Batistetti R, de Oliveira Rodrigues T, Barreto Silva M. Pulmonary changes on high-resolution computed tomography of patients with rheumatoid arthritis and their association with clinical, demographic, serological and therapeutic variables - PubMed. Revista Brasilera de Reumatologia. 2011;4:325–336.
25. Youssef AA, Machaly SA, El-Dosoky ME, El-Maghraby NM. Respiratory symptoms in rheumatoid arthritis: relation to pulmonary abnormalities detected by high-resolution CT and pulmonary functional testing. Rheumatol Int. 2012;32(7):1985–1995. doi:10.1007/s00296-011-1905-z
26. Biederer J, Schnabel A, Muhle C, Gross WL, Heller M, Reuter M. Correlation between HRCT findings, pulmonary function tests and bronchoalveolar lavage cytology in interstitial lung disease associated with rheumatoid arthritis. Eur Radiol. 2004;14(2):272–280. doi:10.1007/s00330-003-2026-1
27. Li L, Gao S, Fu Q, et al. A preliminary study of lung abnormalities on HRCT in patients of rheumatoid arthritis-associated interstitial lung disease with progressive fibrosis. Clin Rheumatol. 2019;38(11):3169–3178. doi:10.1007/s10067-019-04673-4
28. Manfredi A, Cassone G, Cerri S, et al. Diagnostic accuracy of a velcro sound detector (VECTOR) for interstitial lung disease in rheumatoid arthritis patients: the InSPIRAtE validation study (INterStitial pneumonia in rheumatoid ArThritis with an electronic device). BMC Pulm Med. 2019;19(1). doi:10.1186/s12890-019-0875-x
29. Xie HQ, Zhang WW, Sun DS, et al. A simplified lung ultrasound for the diagnosis of interstitial lung disease in connective tissue disease: a meta-analysis. Arthritis Res Ther. 2019;21(1). doi:10.1186/s13075-019-1888-9
30. Wang YK, Gargani L, Barskova T, Furst DE, Cerinic MM. Usefulness of lung ultrasound B-lines in connective tissue disease-associated interstitial lung disease: a literature review. Arthritis Res Ther. 2017;19(1). doi:10.1186/s13075-017-1409-7
31. Aletaha D, Neogi T, Silman AJ, et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62(9):2569–2581. doi:10.1002/art.27584
32. Volpicelli G, Elbarbary M, Blaivas M, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38(4):577–591. doi:10.1007/s00134-012-2513-4
33. Diot E, Boissinot E, Asquier E, et al. Relationship between abnormalities on high-resolution CT and pulmonary function in systemic sclerosis. Chest. 1998;114(6):1623–1629. doi:10.1378/chest.114.6.1623
34. Writing Committee ACR-SRT-SPR. ACR–SPR–STR Practice Parameter for the Performance of Chest Radiography. Collaborative Practice Parameters, Guidelines and Statements STR. 1–8. 2022.
35. Writing Committee ACR-SRT-SPR. ACR–STR Practice Parameter for the Performance of High Resolution Computed Tomography (HRCT) of the Lungs in Adults. Collaborative Practice Parameters, Guidelines and Statements STR. 1–9. 2020.
36. Graham BL, Steenbruggen I, Barjaktarevic IZ, et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care Med. 2019;200(8):e70–e88.
37. R: the R Project for Statistical Computing. Available from: https://www.r-project.org/.
38. Bossuyt PM, Reitsma JB, Bruns DE, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ. 2015;351.
39. Messina R, Guggino G, Benfante A, Scichilone N. Interstitial Lung Disease in Elderly Rheumatoid Arthritis Patients. Drugs Aging. 2020;37(1):11–18. doi:10.1007/s40266-019-00727-z
40. Brennan-Olsen SL, Cook S, Leech MT, et al. Prevalence of arthritis according to age, sex and socioeconomic status in six low and middle income countries: analysis of data from the World Health Organization study on global AGEing and adult health (SAGE) Wave 1. BMC Musculoskelet Disord. 2017;18(1). doi:10.1186/s12891-017-1624-z
41. Zhang Y, Lu N, Peloquin C, et al. Improved survival in rheumatoid arthritis: a general population-based cohort study. Ann Rheum Dis. 2017;76(2):408–413. doi:10.1136/annrheumdis-2015-209058
42. Lacaille D, Avina-Zubieta JA, Sayre EC, Abrahamowicz M. Improvement in 5-year mortality in incident rheumatoid arthritis compared with the general population-closing the mortality gap. Ann Rheum Dis. 2017;76(6):1057–1063. doi:10.1136/annrheumdis-2016-209562
43. Bongartz T, Nannini C, Medina-Velasquez YF, et al. Incidence and mortality of interstitial lung disease in rheumatoid arthritis: a population-based study. Arthritis Rheum. 2010;62(6):1583–1591. doi:10.1002/art.27405
44. Koduri G, Norton S, Young A, et al. Interstitial lung disease has a poor prognosis in rheumatoid arthritis: results from an inception cohort. Rheumatology. 2010;49(8):1483–1489. doi:10.1093/rheumatology/keq035
45. Mena-Vázquez N, Jimenez-Núñez FG, Godoy-Navarrete FJ, et al. Utility of pulmonary ultrasound to identify interstitial lung disease in patients with rheumatoid arthritis. Clin Rheumatol. 2021;40(6):2377–2385. doi:10.1007/s10067-021-05655-1
46. Cogliati C, Antivalle M, Torzillo D, et al. Standard and pocket-size lung ultrasound devices can detect interstitial lung disease in rheumatoid arthritis patients. Rheumatology. 2014;53(8):1497–1503. doi:10.1093/rheumatology/keu033
47. Moazedi-Fuerst FC, Kielhauser SM, Scheidl S, et al. Ultrasound screening for interstitial lung disease in rheumatoid arthritis. Clin Exp Rheumatol. 2014;32(2):199–203.
48. Hassan RI, Lubertino LI, Barth MA, et al. Lung Ultrasound as a Screening Method for Interstitial Lung Disease in Patients With Systemic Sclerosis. J Clin Rheumatol. 2019;25(7):304–307. doi:10.1097/RHU.0000000000000860
49. Gargani L, Bruni C, Romei C, et al. Prognostic Value of Lung Ultrasound B-Lines in Systemic Sclerosis. Chest. 2020;158(4):1515–1525. doi:10.1016/j.chest.2020.03.075
50. Vicente-Rabaneda EF, Bong DA, Busquets-Pérez N, Moller I. Ultrasound evaluation of interstitial lung disease in rheumatoid arthritis and autoimmune diseases. Eur J Rheumatol. 2022. doi:10.5152/eujrheum.2022.20120
51. Spagnolo P, Lee JS, Sverzellati N, Rossi G, Cottin V. The Lung in Rheumatoid Arthritis: focus on Interstitial Lung Disease. Arthritis Rheumatol. 2018;70(10):1544–1554. doi:10.1002/art.40574
52. Richman NC, Yazdany J, Graf J, Chernitskiy V, Imboden JB. Extraarticular manifestations of rheumatoid arthritis in a multiethnic cohort of predominantly Hispanic and Asian patients. Medicine. 2013;92(2):92–97. doi:10.1097/MD.0b013e318289ce01
53. Norton S, Koduri G, Nikiphorou E, Dixey J, Williams P, Young A. A study of baseline prevalence and cumulative incidence of comorbidity and extra-articular manifestations in RA and their impact on outcome. Rheumatology. 2013;52(1):99–110. doi:10.1093/rheumatology/kes262
54. Vizioli L, Ciccarese F, Forti P, et al. Integrated Use of Lung Ultrasound and Chest X-Ray in the Detection of Interstitial Lung Disease. Respiration. 2017;93(1):15–22. doi:10.1159/000452225
55. Vicente-Rabaneda EF, Bong DA, Castañeda S, Möller I. Use of ultrasound to diagnose and monitor interstitial lung disease in rheumatic diseases. Clin Rheumatol. 2021;40(9):3547–3564. doi:10.1007/s10067-021-05761-0
56. Wang T, Zheng XJ, Liang BM, Liang ZA. Clinical features of rheumatoid arthritis-associated interstitial lung disease. Sci Rep. 2015;5(1):1–7.
57. Salaffi F, Carotti M, Di Carlo M, Tardella M, Giovagnoni A, Adamek M. High-resolution computed tomography of the lung in patients with rheumatoid arthritis: prevalence of interstitial lung disease involvement and determinants of abnormalities. Medicine. 2019;98(38). doi:10.1097/MD.0000000000017088
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
