Back to Journals » Infection and Drug Resistance » Volume 17
Unraveling Key Chloroquine Resistance-Associated Alleles Among Plasmodium falciparum Isolates in South Darfur State, Sudan Twelve Years After Drug Withdrawal
Authors Magboul AM, Nour BY, Tamomh AG , Abdul-Ghani R, Albushra SM, Eltahir HB
Received 13 September 2023
Accepted for publication 17 January 2024
Published 24 January 2024 Volume 2024:17 Pages 221—227
DOI https://doi.org/10.2147/IDR.S439875
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Abdalmoneim M Magboul,1 Bakri YM Nour,2 Abdelhakam G Tamomh,1 Rashad Abdul-Ghani,3,4 Sayed Mustafa Albushra,5 Hanan Babiker Eltahir6
1Department of Parasitology & Medical Entomology, Faculty of Medical Laboratory Sciences, University of El Imam El Mahdi, Kosti, Sudan; 2Department of Parasitology, Faculty of Medical Laboratory Sciences, University of Gezira, Wad Madani, Sudan; 3Department of Medical Parasitology, Faculty of Medicine and Health Sciences, Sana’a University, Sana’a, Yemen; 4Tropical Disease Research Center, Faculty of Medicine and Health Sciences, University of Science and Technology, Sana’a, Yemen; 5Department of Internal Medicine, Faculty of Medicine, University of Gezira, Wad Madani, Sudan; 6Department of Biochemistry, Faculty of Medicine, University of El Imam El Mahdi, Kosti, Sudan
Correspondence: Abdelhakam G Tamomh, Email [email protected]; [email protected]
Background: Due to the increasing resistance of Plasmodium falciparum to chloroquine (CQ) in Sudan, a shift from CQ to artesunate combined with sulfadoxine/pyrimethamine as a first-line treatment for uncomplicated falciparum malaria was adopted in 2004. This study aimed to determine the frequency distribution of K76T and N86Y mutations in P. falciparum chloroquine resistance transporter (pfcrt) and P. falciparum multidrug resistance 1 (pfmdr1) genes as key markers of resistance to CQ among P. falciparum isolates from patients in Nyala district of South Darfur state, west of Sudan.
Methods: A descriptive, cross-sectional study was conducted among 75 P. falciparum isolates from Sudanese patients diagnosed with falciparum malaria mono-infection. Parasite DNA was extracted from dried blood spots and amplified using a nested polymerase chain reaction (PCR). Then, restriction fragment length polymorphism (RFLP) was used to detect the genetic polymorphisms in codons 76 of pfcrt and 86 of pfmdr1. PCR-RFLP products were analyzed using 1.5% gel electrophoresis to identify the genetic polymorphisms in the studied codons. The wild-type (pfcrt K76 and pfmdr1 N86), mutant (pfcrt 76T and pfmdr1 86Y) and mixed-type (pfcrt K76T and pfmdr1 N86Y) alleles were expressed as frequencies and proportions.
Results: The wild-type pfcrt K76 allele was observed among 34.7% of isolates and the mutant 76T allele among 20% of isolates, while the mixed-type K76T allele was observed among 45.3% of isolates. On the other hand, 54.7% of isolates harbored the wild-type pfmdr1 N86 allele and 5.3% of isolates had the mutant 86Y allele, while the mixed-type N86Y allele was observed among 40% of isolates.
Conclusion: The key molecular markers associated with CQ resistance (pfcrt 76T and pfmdr1 86Y) are still circulating in high frequency among P. falciparum isolates in South Darfur state, about twelve years after the official withdrawal of the drug as a treatment for uncomplicated falciparum malaria.
Keywords: chloroquine, drug resistance, molecular markers, pfcrt, pfmdr1, Sudan
Introduction
Sudan accounted for an estimated 41% of the malaria cases in the Eastern Mediterranean Region (EMR) of the World Health Organization (WHO) in 2022,1 with about 8 million suspected cases and 1.4 million confirmed cases. Malaria in the country is predominantly caused by Plasmodium falciparum (80.5%), followed by Plasmodium vivax (9.2%).1 The entire population is at risk of malaria, with approximately 87% being at high risk.1 Malaria endemicity is primarily low to moderate in the country’s northern, eastern and western states.2 According to the last Malaria Indicator Survey (MIS) in 2016, the overall malaria prevalence in Sudan is 5.9%.3 The prevalence varies across different regions of the country. In the states of Khartoum, Red Sea, Northern and River Nile, it is less than 1%, while it exceeds 20% in Central Darfur state.3 The prevalence is around or above 10% in the states of South and West Darfur, Blue Nile and South Kordofan.3 In South Darfur state, malaria transmission is largely mesoendemic, with pockets of hyperendemicity.4
Chloroquine (CQ) has been used for treating falciparum malaria for more than four decades.5 In the late 1970s, CQ sensitivity was reported among more than 99% of Sudanese patients infected with P. falciparum.6 However, P. falciparum was resistant to CQ in 42% of patients in an in-vivo study in eastern Sudan in the late 1980s.7 Since then, CQ resistance has been reported from different parts of Sudan.8–13 In response to the growing problem of P. falciparum resistance to CQ, the National Malaria Control Programme in Sudan transitioned from CQ monotherapy to artemisinin-based combination therapy (ACT) for treating uncomplicated falciparum malaria in 2004.5,14
Resistance of P. falciparum to CQ is a complex trait involving multiple genes, with initial resistance often linked to mutations occurring in a specific gene called P. falciparum CQ resistance transporter (pfcrt) that encodes the PfCRT in the membrane of its digestive vacuole.15–17 The mutation at codon 76 in PfCRT (K76T), which leads to the substitution of lysine (K) with threonine (T), is critical for CQ resistance, serving as a key marker of resistance in vitro and treatment failure in vivo.18–20 However, mutations in other codons of pfcrt can be associated with CQ resistance.15,21
The P. falciparum multidrug resistance 1 (pfmdr1) gene encodes the PfMDR1 transporter protein, which is likely to regulate drug accumulation in its digestive vacuole.22 In vitro studies have shown that the mutation at codon 86 in PfMDR1 (N86Y), which leads to the substitution of asparagine (N) with tyrosine (Y), was found to be partially associated with resistance to CQ among field isolates and laboratory lines of P. falciparum.20,23–26 The role of pfmdr1 N86Y in CQ treatment failure is supported by a meta-analysis, though the association was weak.27
Molecular markers of resistance provide an effective means of monitoring resistance, often serving as reliable alternatives to in vitro and in vivo studies in many instances. These markers are particularly useful in detecting the emergence of resistance before treatment failure and monitoring resistance patterns following drug withdrawal.28,29 As the intensity of CQ pressure has diminished compared to previous decades, mutations in these genes can offer valuable insights into the genetic trends of CQ resistance. After the withdrawal of CQ, several reports have shown a decline in resistant genotypes.30–36 However, there are reports on the persistence of high resistance-associated mutations in some countries after the withdrawal of CQ as a treatment for falciparum malaria.37,38
Given that CQ has been officially discontinued as a treatment for falciparum malaria for the past decade, this study aimed to determine the frequency distribution of the genetic polymorphisms in pfcrt K76T and pfmdr1 N86Y as key markers of CQ resistance among P. falciparum isolates from patients in South Darfur state, Sudan.
Methods
Study Design and Sample Collection
A cross-sectional study was conducted among P. falciparum isolates from 75 conveniently selected Sudanese patients (41 males and 34 females) in Nyala district, South Darfur state, west of Sudan (Figure 1) in 2016. The median age (interquartile range) of patients was 22 years (11), with an age range of 2–65). These patients were diagnosed with P. falciparum mono-infection using microscopy by two expert microscopists or rapid diagnostic tests (RDTs) (SD Bioline® Malaria Antigen Pf/Pan test (Standard Diagnostics, Inc., Kyonggi, Korea) in the Malaria Laboratory in South Darfur state. Patients of both sexes and aged 2–65 years were included after obtaining written informed consent. Patients who were negative for falciparum malaria by microscopy or RDTs or who were co-infected with other Plasmodium species were excluded. Finger-prick blood was collected and spotted onto Whatman 3MM filter papers (Whatman International, Ltd., Maidstone, UK) for the collection of dried blood spots (DBS) for molecular study.
 |
Figure 1 Map of Sudan showing the locations of Nyala district and South Darfur state. |
Detection of Pfcrt K76T and pfmdr1 N86Y Polymorphisms
The Chelex® 100 technique was used to extract parasite DNA from DBS, following the protocol described by Warhurst et al.39 To identify the pfcrt K76T and pfmdr1 N86Y polymorphisms in P. falciparum isolates, nested polymerase chain reaction (PCR) was performed using the primer sequences and amplification cycles outlined by Shrivastava et al.20 PCR amplifications were performed in Techne thermocycler (Techne, Staffordshire, UK) in the Molecular Biology Laboratory, Faculty of Medical Laboratory Sciences, Sudan University of Science and Technology in Khartoum. The amplified products of nested PCR were subsequently subjected to digestion with the Apo I restriction enzyme (New England Biolabs, UK) for restriction fragment length polymorphism (RFLP) analysis, as described by Shrivastava et al.20 Amplicons and RFLP patterns were analyzed on 1.5% agarose gels, which were stained with ethidium bromide and visualized using an ultraviolet illuminator.
Ethical Considerations
The study protocol was reviewed and approved by the Ethics Committee of the Faculty of Medical Laboratory Sciences, University of Gezira, Wad Madani, Sudan. Written informed consent was obtained from patients or their parents. This study was conducted in compliance with the Declaration of Helsinki for medical studies involving human subjects.
Statistical Analysis
Data were analyzed using IBM SPSS Statistics, Version 21 (IBM Corp., Armonk, NY, USA). Genetic polymorphisms were expressed as the frequencies and proportions of wild-type, mutant and mixed-type alleles of pfcrt and pfmdr1.
Results
All 75 P. falciparum isolates investigated in this study were successfully characterized for codons 76 of pfcrt and 86 of pfmdr1. Table 1 shows that 34.7% of isolates harbored the wild-type pfcrt K76 allele and 20% of isolates had the mutant 76T allele, while the mixed-type K76T allele was observed among 45.3% of isolates. On the other hand, Table 2 shows that 54.7% of isolates harbored the wild-type pfmdr1 N86 allele and 5.3% of isolates had the mutant 86Y allele, while the mixed-type N86Y allele was observed among 40% of isolates.
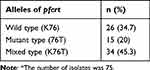 |
Table 1 Frequency Distribution of Pfcrt K76T Alleles Among P. Falciparum Isolates from Patients in Nyala District of South Darfur State, Sudan (2016)* |
 |
Table 2 Frequency Distribution of pfmdr1 N86Y Alleles Among P. Falciparum Isolates from Patients in Nyala District of South Darfur State, Sudan (2016)* |
Discussion
Following the widespread and intense global use of CQ starting in the late 1940s, the first documentation of chloroquine-resistant P. falciparum emerged in Cambodia and at the Cambodia-Thailand border approximately a decade later.40 During the 1960s and 1970s, drug-resistant strains originating from these regions began to disseminate progressively across South America, Southeast Asia and India.40 In the late 1970s, resistance to CQ was introduced into East Africa through a selective sweep originating from Southeast Asia.17,41 Subsequently, within a decade, resistant strains of P. falciparum rapidly spread across the entire African continent.40 Sudan was one of the African countries where the emergence of CQ-resistant falciparum malaria was first reported in the late 1970s.6
CQ was officially withdrawn from Sudan malaria treatment policies about twelve years before the implementation of the present study. However, the key molecular markers associated with its resistance are still circulating among P. falciparum isolates from patients in Nyala district of South Darfur state in the west of the country. The present study revealed the presence of wild-type alleles of pfcrt K76 and pfmdr1 N86 among approximately one-third and one-half of parasite isolates, respectively. However, the remaining isolates harbored either the mutant alleles (76T and 86Y) or mixed-type alleles (K76T and N86Y). The pfcrt 76T and pfmdr1 86Y mutations were reported to be associated with high-level CQ resistance among P. falciparum isolates from Asar village in eastern Sudan in the early 2000s, when CQ was recommended for treating uncomplicated falciparum malaria.25 In 2003, the pfcrt 76T but not the pfmdr1 86Y was reported to be associated with the in-vivo efficacy of CQ against P. falciparum in the Upper Nile state of South Sudan.42
Compared to the frequency of the mutant alleles in the present study, the mutant pfcrt 76T and pfmdr1 86Y alleles were detected among 63% (63/100) and 31% (31/100) of P. falciparum isolates, respectively, collected in 2002 before CQ withdrawal from Akuem village of Bahr El Gazal province in South Sudan.43 A study conducted three years after official CQ withdrawal showed that the mutant types pfcrt 76T and pfmdr1 86Y were present among 72.7% (144/198) and 55.5% (110/198) of P. falciparum isolates, respectively, in central and eastern Sudan.2 In 2015, pfcrt 76T and pfmdr1 86Y mutant alleles were detected among 75% (30/40) and 59.5% (22/37) of P. falciparum isolates, respectively, in Wad Madani district of Gezira State in central Sudan.44 During 2015–2017, pfcrt 76T and pfmdr1 86Y mutant alleles were detected among 71.8% (153/213) and 53.6% (104/194) of P. falciparum isolates, respectively, in Khartoum, New Halfa, Gezira and North Kordofan.45 A higher frequency of 80% (16/20) was reported for the mutant pfcrt 76T allele among P. falciparum isolates from Khartoum in 2018.46 Lower frequencies of pfcrt 76T (25.8%; 31/120) and pfmdr1 86Y (21.7%; 25/115) have been recently reported among parasite isolates from Blue Nile State, Southeast Sudan.47
After the withdrawal of chloroquine and the subsequent absence of its selective pressure, susceptible strains tend to dominate, allowing for the potential recovery of chloroquine efficacy.33,48 Nevertheless, it seems that this restorative outcome has not been attained in Sudan. Despite the withdrawal of CQ from Sudan’s malaria treatment policies more than ten years ago, the persistence of high frequencies of pfcrt 76T and pfmdr1 86Y mutant alleles among P. falciparum isolates in the present study is concerning. This finding highlights the ongoing presence and potential impact of drug-resistant strains in this region in western Sudan, emphasizing the need for continued vigilance and the implementation of effective alternative antimalarial strategies. The high frequency of pfcrt 76T and pfmdr1 86Y mutant alleles in the present study indicates that CQ is still prescribed in the country for treating uncomplicated falciparum malaria. For instance, a survey in 15 states of the country showed that CQ is available at 5% of 244 public health facilities.49 Moreover, the impact of self-medication and the irrational prescription of antimalarial drugs by community pharmacists could not be ruled out. In line with the present study, the persistence of high resistance-associated mutations after withdrawal of CQ as a treatment for falciparum malaria has been reported from India and elsewhere.37,38 However, several reports have shown a decrease in resistant genotypes after CQ withdrawal, suggesting the likelihood of its efficacy reversal, including in Malawi, Kenya, Tanzania, Senegal and China.30–36,50
The present study is limited by the small sample size of isolates investigated for the molecular markers of resistance to CQ and the convenience sampling of study subjects because of financial and logistic constraints. However, the findings of the study provide insights into the high circulation of parasite isolates harboring mutant alleles associated with CQ resistance years after its official discontinuation for treating falciparum malaria. Therefore, large-scale studies are recommended to investigate the molecular markers associated with CQ resistance. Furthermore, antimalarial drug prescribing practices need to be studied to assess the use of CQ monotherapy for treating falciparum malaria and the level of adherence of physicians and other healthcare providers to the guidelines of the national treatment policy.
Conclusion
The key molecular markers associated with CQ resistance (pfcrt 76T and pfmdr1 86Y) are still circulating in high frequency among P. falciparum isolates in Nyala district of South Darfur state, west of Sudan, about twelve years after the official withdrawal of the drug as a treatment for uncomplicated falciparum malaria. The sustained circulation of these resistant alleles indicates that the local malaria parasite population is still under the selective pressure that favors the survival and spread of CQ-resistant parasites. Consequently, reintroducing CQ as a treatment option for falciparum malaria in the near future is not feasible.
Acknowledgments
We thank Dr. Salah Jumaa, Dr. Mohammed Siddig and Dr. Ghada Hag Ali from the Faculty of Medical Laboratory Sciences at the University of Gezira for their support for data acquisition. Also, we thank the administration and staff of the Faculty of Medical Laboratory Sciences at the University of Gezira for their kindness and support. Special thanks are due to the volunteers and teams of the Malaria Laboratory in South Darfur state for their cooperation and collection of specimens. We also thank the research laboratory staff of the Faculty of Medical Laboratory Sciences, Sudan University for Science and Technology for their technical assistance.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. World Malaria Report 2023. Geneva: WHO; 2023.
2. Menegon M, Talha AA, Severini C, et al. Frequency distribution of antimalarial drug resistance alleles among Plasmodium falciparum isolates from Gezira State, central Sudan, and Gedarif State, eastern Sudan. Am J Trop Med Hyg. 2010;83(2):250–257.
3. Federal Ministry of Health. Sudan Malaria Indicator Survey, 2016. Khartoum: Communicable and Non-communicable Disease Control Directorate/Federal Ministry of Health; 2017.
4. Noor AM, ElMardi KA, Abdelgader TM, et al. Malaria risk mapping for control in the Republic of Sudan. Am J Trop Med Hyg. 2012;87(6):1012–1021.
5. Malik EM, Mohamed TA, Elmardi KA, et al. From chloroquine to artemisinin-based combination therapy: the Sudanese experience. Malar J. 2006;5:65.
6. Omer AH. Response of Plasmodium falciparum in Sudan to oral chloroquine. Am J Trop Med Hyg. 1978;27(5):853–857.
7. Bayoumi RA, Babiker HA, Ibrahim SM, et al. Chloroquine-resistant Plasmodium falciparum in eastern Sudan. Acta Trop. 1989;46(3):157–165.
8. Ibrahim AM, Ali FR, Ali ME. Assessment of chloroquine resistance of Plasmodium falciparum in children of Wad Medani (Central Sudan). J Trop Pediatr. 1992;38(4):162–166.
9. Elkheir HK, Elkarim EF, Eltayeb IB, Elkadaru AE, Babiker HA, Ibrahim AM. Efficacy of sulphadoxine and pyrimethamine, doxycycline and their combination in the treatment of chloroquine resistant falciparum malaria. Saudi Med J. 2001;22(8):690–693.
10. Abdel-Hameed AA, El-Jak IE, Faragalla IA. Sentinel posts for monitoring therapeutic efficacy of antimalarial drugs against Plasmodium falciparum infections in the Sudan. Afr J Med Med Sci. 2001:30. Suppl:1-5
11. Adam I, Osman ME, Elghzali G, Ahmed GI, Gustafssons LL, Elbashir MI. Efficacies of chloroquine, sulfadoxine-pyrimethamine and quinine in the treatment of uncomplicated, Plasmodium falciparum malaria in eastern Sudan. Ann Trop Med Parasitol. 2004;98(7):661–666.
12. van den Broek IV, Gatkoi T, Lowoko B, Nzila A, Ochong E, Keus K. Chloroquine, sulfadoxine-pyrimethamine and amodiaquine efficacy for the treatment of uncomplicated Plasmodium falciparum malaria in Upper Nile, South Sudan. Trans R Soc Trop Med Hyg. 2003;97(2):229–235.
13. Stivanello E, Cavailler P, Cassano F, et al. Efficacy of chloroquine, sulphadoxine-pyrimethamine and amodiaquine for treatment of uncomplicated Plasmodium falciparum malaria in Kajo Keji county, Sudan. Trop Med Int Health. 2004;9(9):975–980.
14. Malik EM, Ali EM, Mohamed TA, et al. Efforts to control malaria in Sudan - case study of the National Malaria Control Programme, 2001-2005. Italian J Trop Med. 2006;11(3–4):56.
15. Fidock DA, Nomura T, Talley AK, et al. Mutations in the P. falciparum digestive vacuole transmembrane protein PfCRT and evidence for their role in chloroquine resistance. Mol Cell. 2000;6(4):861–871.
16. Plowe CV. Monitoring antimalarial drug resistance: making the most of the tools at hand. J Exp Biol. 2003;206(Pt 21):57.
17. Ecker A, Lehane AM, Clain J, Fidock DA. PfCRT and its role in antimalarial drug resistance. Trends Parasitol. 2012;28(11):504–514.
18. Lakshmanan V, Bray PG, Verdier-Pinard D, et al. A critical role for PfCRT K76T in Plasmodium falciparum verapamil-reversible chloroquine resistance. EMBO j. 2005;24(13):2294–2305.
19. Tagelsir N, Ibrahim Z, Medani A, et al. High frequency of Plasmodium falciparum PfCRT K76T and PfpghN86Y in patients clearing infection after chloroquine treatment in the Sudan. Acta Trop. 2006;97(1):19–25.
20. Shrivastava SK, Gupta RK, Mahanta J, Dubey ML. Correlation of molecular markers, Pfmdr1-N86Y and Pfcrt-K76T, with in vitro chloroquine resistant Plasmodium falciparum, isolated in the malaria endemic states of Assam and Arunachal Pradesh, Northeast India. PLoS One. 2014;9(8).
21. Bray PG, Martin RE, Tilley L, Ward SA, Kirk K, Fidock DA. Defining the role of PfCRT in Plasmodium falciparum chloroquine resistance. Mol Microbiol. 2005;56(2):323–333.
22. Ecker A, Lehane AM, Fidock DA. Molecular markers of Plasmodium resistance to antimalarials. In: Staines HM, Krishna S, editors. Treatment and Prevention of Malaria: Antimalarial Drug Chemistry, Action and Use. Basel: Springer; 2012:245–280.
23. Mu J, Ferdig MT, Feng X, et al. Multiple transporters associated with malaria parasite responses to chloroquine and quinine. Mol Microbiol. 2003;49(4):977–989.
24. Adagu IS, Warhurst DC. Plasmodium falciparum: linkage disequilibrium between loci in chromosomes 7 and 5 and chloroquine selective pressure in Northern Nigeria. Parasitology. 2001;123(Pt 3):219–224.
25. Babiker HA, Pringle SJ, Abdel-Muhsin A, Mackinnon M, Hunt P, Walliker D. High-level chloroquine resistance in Sudanese isolates of Plasmodium falciparum is associated with mutations in the chloroquine resistance transporter gene pfcrt and the multidrug resistance gene pfmdr1. J Infect Dis. 2001;183(10):1535–1538.
26. Duraisingh MT, Cowman AF. Contribution of the pfmdr1 gene to antimalarial drug-resistance. Acta Trop. 2005;94(3):181–190.
27. Picot S, Olliaro P, de Monbrison F, Bienvenu AL, Price RN, Ringwald P. A systematic review and meta-analysis of evidence for correlation between molecular markers of parasite resistance and treatment outcome in falciparum malaria. Malar J. 2009;8:89.
28. Hastings IM, Watkins WM, White NJ. The evolution of drug-resistant malaria: the role of drug elimination half-life. Philos Trans R Soc Lond B Biol Sci. 2002;357(1420):505–519.
29. Guerra AP, Olivera MJ, Cortés LJ, Chenet SM, Macedo de Oliveira A, Lucchi NW. Molecular surveillance for anti-malarial drug resistance and genetic diversity of Plasmodium falciparum after chloroquine and sulfadoxine-pyrimethamine withdrawal in Quibdo, Colombia, 2018. Malar J. 2022;21(1):306.
30. Kublin JG, Cortese JF, Njunju EM, et al. Reemergence of chloroquine-sensitive Plasmodium falciparum malaria after cessation of chloroquine use in Malawi. J Infect Dis. 2003;187(12):1870–1875.
31. Mita T, Kaneko A, Lum JK, et al. Recovery of chloroquine sensitivity and low prevalence of the Plasmodium falciparum chloroquine resistance transporter gene mutation K76T following the discontinuance of chloroquine use in Malawi. Am J Trop Med Hyg. 2003;68(4):413–415.
32. Wang X, Mu J, Li G, et al. Decreased prevalence of the Plasmodium falciparum chloroquine resistance transporter 76T marker associated with cessation of chloroquine use against P. falciparum malaria in Hainan, People’s Republic of China. Am J Trop Med Hyg. 2005;72(4):410–414.
33. Laufer MK, Thesing PC, Eddington ND, et al. Return of chloroquine antimalarial efficacy in Malawi. N Engl J Med. 2006;355(19):1959–1966.
34. Mwai L, Ochong E, Abdirahman A, et al. Chloroquine resistance before and after its withdrawal in Kenya. Malar J. 2009;8:106.
35. Wurtz N, Fall B, Pascual A, et al. Prevalence of molecular markers of Plasmodium falciparum drug resistance in Dakar, Senegal. Malar J. 2012;11:197.
36. Gharbi M, Flegg JA, Hubert V, et al. Longitudinal study assessing the return of chloroquine susceptibility of Plasmodium falciparum in isolates from travellers returning from West and Central Africa, 2000-2011. Malar J. 2013;12:35.
37. Das S, Tripathy S, Chattopadhayay S, et al. Progressive increase in point mutations associates chloroquine resistance: even after withdrawal of chloroquine use in India. Int J Parasitol Drugs Drug Resist. 2017;7(3):251–261.
38. Ocan M, Akena D, Nsobya S, et al. Persistence of chloroquine resistance alleles in malaria endemic countries: a systematic review of burden and risk factors. Malar J. 2019;18(1):76.
39. Warhurst DC, Awad El Kariem FM, Miles MA. Simplified preparation of malarial blood samples for polymerase chain reaction. Lancet. 1991;337(8736):303–304.
40. Payne D. Spread of chloroquine resistance in Plasmodium falciparum. Parasitol Today. 1987;3(8):241–246.
41. Campbell CC, Chin W, Collins WE, Teutsch SM, Moss DM. Chloroquine-resistant Plasmodium falciparum from East Africa: cultivation and drug sensitivity of the Tanzanian I/CDC strain from an American tourist. Lancet. 1979;2(8153):1151–1154.
42. Ochong EO, van den Broek IV, Keus K, Nzila A. Short report: association between chloroquine and amodiaquine resistance and allelic variation in the Plasmodium falciparum multiple drug resistance 1 gene and the chloroquine resistance transporter gene in isolates from the upper Nile in southern Sudan. Am J Trop Med Hyg. 2003;69(2):184–187.
43. Anderson TJ, Nair S, Jacobzone C, Zavai A, Balkan S. Molecular assessment of drug resistance in Plasmodium falciparum from Bahr El Gazal province, Sudan. Trop Med Int Health. 2003;8(12):1068–1073.
44. Nour BY, Mohamadani AA, Saeed OK, Schallig H. Molecular markers assessment of chloroquine resistance to Plasmodium falciparum isolates in Wad Medani district, Gezira State, Sudan. N M J. 2015;3(17):576.
45. Hussien M, Abdel Hamid MM, Elamin EA, et al. Antimalarial drug resistance molecular makers of Plasmodium falciparum isolates from Sudan during 2015-2017. PLoS One. 2020;15(8):34.
46. Abdulla Mohammed WS, Yasin K, Mahgoub NS, Abdel Hamid MM. Cross sectional study to determine chloroquine resistance among Plasmodium falciparum clinical isolates from Khartoum, Sudan. F1000Res. 2018;7:208.
47. Mohamed AO, Hussien M, Mohamed A, et al. Assessment of Plasmodium falciparum drug resistance molecular markers from the Blue Nile State, Southeast Sudan. Malar J. 2020;19(1):78.
48. Lu F, Zhang M, Culleton RL, et al. Return of chloroquine sensitivity to Africa? Surveillance of African Plasmodium falciparum chloroquine resistance through malaria imported to China. Parasit Vectors. 2017;10(1):355.
49. Abdelgader TM, Ibrahim AM, Elmardi KA, et al. Progress towards implementation of ACT malaria case-management in public health facilities in the Republic of Sudan: a cluster-sample survey. BMC Public Health. 2012;12:11.
50. Mohammed A, Ndaro A, Kalinga A, et al. Trends in chloroquine resistance marker, Pfcrt-K76T mutation ten years after chloroquine withdrawal in Tanzania. Malar J. 2013;12:415.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
