Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Unpacking the Broad Landscape of Intraoperative Stressors for Clinical Personnel: A Mixed-Methods Systematic Review
Authors Lee A , Torkamani-Azar M , Zheng B, Bednarik R
Received 31 December 2022
Accepted for publication 9 June 2023
Published 17 July 2023 Volume 2023:16 Pages 1953—1977
DOI https://doi.org/10.2147/JMDH.S401325
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ahreum Lee,1 Mastaneh Torkamani-Azar,2 Bin Zheng,3 Roman Bednarik4
1Samsung Electronics Co. Ltd., Suwon, Gyeonggi-do, Republic of Korea; 2University of Eastern Finland, Kuopio, Finland; 3Department of Surgery, University of Alberta, Edmonton, Canada; 4University of Eastern Finland, Joensuu, Finland
Correspondence: Roman Bednarik, University of Eastern Finland, Joensuu, Finland, Email [email protected]
Purpose: The main goals of this mixed-methods systematic review are to identify what types of intraoperative stressors for operating room personnel have been reported in collected studies and examine the characteristics of each intraoperative stressor.
Methods: With a systematic literature search, we retrieved empirical studies examining intraoperative stress published between 2010 and 2020. To synthesize findings, we applied two approaches. First, a textual narrative synthesis was employed to summarize key study information of the selected studies by focusing on surgical platforms and study participants. Second, a thematic synthesis was employed to identify and characterize intraoperative stressors and their subtypes.
Results: Ninety-four studies were included in the review. Regarding the surgical platforms, the selected studies mainly focused on minimally invasive surgery and few studies examined issues around robotic surgery. Most studies examined intra-operative stress from surgeons’ perspectives but rarely considered other clinical personnel such as nurses and anesthetists. Among seven identified stressors, technical factors were the most frequently examined followed by individual, operating room environmental, interpersonal, temporal, patient, and organizational factors.
Conclusion: By presenting stressors as multifaceted elements affecting collaboration and interaction between multidisciplinary team members in the operating room, we discuss the potential interactions between stressors which should be further investigated to build a safe and efficient environment for operating room personnel.
Keywords: intraoperative stressors, team dynamics, communication and teamwork in health care, medical devices and technologies
Introduction
In the operating room (OR), a team ecosystem is built based on the interaction and collaboration between various OR professionals including the main surgeon, assistant surgeons, scrub nurses, circulating nurses, anesthesiologists, and technicians. Under the high-risk and high-demand situations in the OR, all the multi-professional team members do their best to pursue a common goal: patient safety.1,2 While there are various sources that create challenges for the team members, many researchers have focused on intraoperative stress for the OR team members.3–5 Lazarus and Folkman6 define stress as “a particular relationship between the person and the environment” (p.19). In other words, stress leads to psychophysiological changes which are not only provoked by external stimuli from environments but also by individual characteristics.6,7 Stress is generally perceived as an inhibitor of optimal performance that would deter one’s decision-making and cause human errors.8,9 However, in accordance with the Yerkes–Dodson law,10 moderate amounts of tolerable stress are considered beneficial and may contribute to a heightened perceptual performance, better concentration, and improved alertness during surgery.11,12 Likewise, either in a positive or negative way, the stress levels of the team members affect individual and collective performance in the OR.2,4,12,13 Therefore, it is fundamental to identify what factors induce the OR team members’ acute stress during surgery (ie, the intraoperative period14).
Intraoperative Stressors
Previous studies have employed various perspectives to understand stress-inducing factors (from here on referred to as “stressors”) during surgery. Some researchers have focused on external stressors that are created from OR environments such as auditory noise, surgical tools, and the layout of the OR.15–17 For instance, Pluyter et al18 specified the external stressors into two categories: social (eg, music, external staff, phone calls, case-irrelevant talk in the OR) and technological distractions (eg, a non-optimal laparoscopic navigation). These external stressors are referred to “workflow distractions/disruptions”, “interruptions”, or “operating room distractions and interruptions (ORDIs)”.8,19–21 Others have focused on individuals’ characteristics (eg, role, expertise, personality),4,22,23 which are similar to internal stressors that Lazarus and Folkman6 studied. Particularly, when the previous studies looked into which stressors affect individuals in the OR, they focused on the roles of OR personnel and mainly investigated stressors from surgeons’ perspectives.24,25 This is because the surgeon is the main operator who leads surgery and directly interacts with various devices and tools to perform surgery. However, a surgical operation is not done by one person. It is teamwork. The surgeon needs to be supported by all members in the OR to accomplish the most desirable outcome. For example, scrub nurses pass surgical instruments to the surgeon at the right time. Circulating nurses manage all activities outside the sterile field in which the surgeon and scrub nurses cannot directly manage. Anesthesiologists and nurse anesthetists monitor the patients’ vital signs to provide safe anesthesia care during surgery.26,27 In sum, the interaction and collaboration between these various team members is fundamental to perform surgery and provide optimal patient care.28,29 Therefore, it is important to investigate stressors from various OR professionals’ perspectives.30
Beyond understanding the team dynamics in the OR, one also needs to consider surgical technology as another stressor for OR personnel. Whenever new surgical platforms are introduced for better patient recovery and surgical outcome, OR team members need to adjust to a new work environment in the OR quickly and efficiently.31,32 For example, minimally invasive surgery has been preferred to open surgery in terms of patients’ recovery. However, it brings technical challenges that surgeons need to learn and overcome, such as the limited range of motions and fulcrum effect.33,34 New surgical technologies also create a new form of socio-technical process in the OR (eg, communication, teamwork, coordination).32,35,36 In the case of tele-operated robotic surgery, a robot physically replaces a surgeon and reconfigures the operating room where both distributed and collocated teamwork are required.24,37 Therefore, new technologies introduced for the benefit of patients or OR personnel can be another stressor during surgery.31,38,39
Understanding definitions and types of possible stressors in the OR would help to improve awareness of clinical personnel and administrators regarding potential sources of intraoperative stress and assist them with mitigating adverse effects of the stressors on surgical performance and outcomes through training, intervention, and administrative practices. Moreover, human factors researchers and practitioners can examine how the new interventions would affect the existing stressors and what should be proactively evaluated to minimize the potential sources of stress that could be triggered by new interventions in the OR.31 This systematic approach will contribute to designing usable, safe, and effective interventions in the OR, which would be beneficial to all OR team members and patients in the long run.40 While there have been several systematic review papers related to intraoperative stress, they did not fully reflect on the complex OR environments where multiple OR professionals are exposed to various stressors. Two reviews41,42 interpreted stressors only from surgeons’ perspectives. Catanzarite et al42 particularly focused on what stressors cause physical stress during surgery. Other reviews were more interested in the link between intraoperative stressors and surgical performance.21,43,44 On the other hand, Chrouser et al4 demonstrated how emotional, physiological, and behavioral responses to stressors can affect individual and collective performance and surgical outcomes. While they presented a conceptual framework for intraoperative stress, they did not specify what characteristics of stressors were employed to examine intraoperative stress for OR personnel.
Research Goals and Questions
In this work, using the concept of stress,6 we particularly focus on identifying factors causing acute stress for OR personnel during surgery. We define these factors as intraoperative stressors. The main goals of this mixed-methods systematic review are to (1) identify intraoperative stressors for OR personnel that were reported in the previous literature and (2) examine the characteristics of each stressor. For intraoperative stressors, we do not aim to demonstrate or rank stressors in terms of their stress-inducing effects but to cover all possible intraoperative stressors reported in previous literature regardless of their statistical significance. To be more precise, we conduct a mixed-methods systematic review45,46 to address the following research questions:
- How the collected studies have defined problems related to intraoperative stress regarding surgical platforms and study participants
- What types of stressors have been reported in collected studies and what subtypes of stressors were employed to examine intraoperative stress for OR personnel, and
- What should be further investigated to build a safe and efficient environment for OR personnel.
The last research question is not answered in Results, but is instead employed to articulate a research gap that we found in our analysis and to discuss future research directions in Discussion.
Study Selection
In this section, we describe how we collected and selected studies for the mixed-methods systematic review. We firstly address the definition of stress in this paper to clarify our research scope. Then, we present how we apply the definition to collect and screen papers.
Working Definition of Stress
Various terminologies (eg, mental workload, ergonomics, strain, or musculoskeletal pain) are often used interchangeably with stress.4 These terminologies particularly focus on the characteristics of stress-inducing effects in either cognitive or physical ways. However, as noted by Lazarus and Folkman6 and Giannakakis et al,47 stress is a more comprehensive term. The nature of stress involves psychological, physiological, and behavioral processes which is caused by internal and external stimulus from demanding environments. By using the term “stress” as the main search keyword, we aim to collect earlier studies that mentioned “stress” and identify a broad scope of stressors for OR personnel during surgery. To clearly refer to stress that OR professionals experience during surgery, we use a more specific term: “intraoperative stress”.14 In other words, we only consider acute stress that individuals experience during a specific period of time—surgery,48,49 but not chronic stress. Therefore, in this work, we use the term stressors to describe factors inducing acute stress for OR personnel.
Search Strategy
Using the PRISMA methodology,50 we selected three databases: PubMed, Scopus, and ACM Library (see Figure 1). With these databases, we included research papers that explored intraoperative stress from various perspectives such as clinical research, social science, and computer science. The last search was conducted in February 2021, and we limited our search to studies published from 2010 to 2020. This was to differentiate our work from previous review papers that had focused on similar topics in the operating room (ie, distraction,21 surgical stress effects4) and had included papers published before 2016. To narrow down our research interests, we created search queries using combinations of three elements: topic, research contexts, and participants (see Appendix). With these elements, we retrieved the literature that has investigated the intraoperative stress of clinical personnel.
 |
Figure 1 Flow diagram of how articles were searched, selected, and evaluated for inclusion of this mixed-methods systematic review. |
First, we used the term “stress” as our main search keyword. Second, to collect papers examining stress “in the operating room”, we applied keywords describing the study environments such as “surgery”, “operating room”, “operating theater”, and “surgical procedure”. Lastly, we applied keywords to include papers investigating intraoperative stress from “various stakeholders in the OR”. For instance, “surgeon”, “resident”, “trainee”, “intern”, “nurse”, “anesthetist”, “surgical team”, “medical personnel”, and “clinical personnel” were added to the search terms. Additional search limits were applied to collect papers published in English. Using the combinations of these three keyword elements, we initially searched papers from PubMed and Scopus by using the [TITLE-ABS] function which searches for a set of keywords within the titles and abstracts. While we reviewed the titles of retrieved papers, we noted that there were not many papers examining intraoperative stress from technological perspectives. Therefore, we selected ACM Digital Library as an additional database to collect papers in computing fields. We performed another round of literature search in ACM Digital Library with the same search queries. As search functions in ACM Digital Library are different from those of PubMed and Scopus, we applied the [ABS] search function that looks for a set of keywords only within the abstracts.
Screening
We conduct a mixed-methods systematic review45,46 to address the full range of intraoperative stressors that have been reported in both experimental and non-experimental research. In this regard, this review paper does not aim to demonstrate significant effects of the intraoperative stressors. With this purpose, we performed four phases of screening to identify empirical studies reporting intraoperative stressors.
In the first phase, to perform an efficient initial screening process,51 the first author screened the titles of retrieved papers and excluded papers that were not related to intraoperative stress of clinical personnel. Therefore, we excluded studies reporting patients or caregivers stress as well as examining stress of clinical personnel outside the OR. Also, studies using the term “stress” in different contexts such as mechanical stress of tissues52 and stress urinary incontinence53 were excluded. If a paper did not clarify its study goals regarding intraoperative stress in its title, we left them for the next round of screening. After applying the initial screening criteria and removing duplicates from three databases, 645 papers were retrieved.
While conducting the first phase, the first author developed the following inclusion and exclusion criteria to derive the final set of literature included in this review. The inclusion and exclusion criteria were built by considering three different perspectives: formats of papers, the main focus of papers, and research methods used in papers. First, in terms of formats, we only included empirical research written in English but excluded pilot studies, essay, and protocols. Second, we focused on the main topic of papers. In terms of the definition of stress, only studies on acute stress of clinical personnel during surgery or surgical training were included. Therefore, we excluded papers investigating chronic stress (eg, burnout, depression, occupational stress). Furthermore, we excluded papers that did not clearly describe the relevance of their studies to intraoperative stress. For example, if a study only measured the clinical personnel’s satisfaction with surgical tools or interventions (without analyzing stress), it was excluded. Lastly, we only included papers that considered human factors and performed user studies to investigate intraoperative stress in an operating room. Therefore, algorithmic or simulation studies that did not include human participants were excluded.
In the second phase, the first author screened titles of the 645 retrieved papers using these three criteria and derived a total of 226 papers. Before going to the third phase, the first author excluded five papers which were unavailable in the full text. In the third phase, the first author reviewed the abstracts of 226 papers by applying the inclusion and exclusion criteria and selected 103 papers for the last round of screening. In the fourth phase, the first and second authors independently screened full texts of 103 papers with the inclusion and exclusion criteria. During the screening process, the researchers excluded nine papers that focused on occupational stress or job satisfaction (n = 2),54,55 events outside the OR (n = 4),56–59 or, did not include clinical personnel as their participants (n = 3).60–62 If there was any disagreement between the researchers, they had discussions and made final decisions. After four phases of screening, 94 articles were included in the final review.
Analysis
Two different approaches were taken to explore 94 selected studies. First, we delved into the key study information of selected studies followed by a textual narrative synthesis.63 We summarized how each study defined a problem space related to intraoperative stress (eg, surgical platforms and study participants). Then, we conducted a thematic synthesis64 and identified intraoperative stressors that were examined in each study.
Study Characteristics
To categorize the included studies with surgical perspectives, three rounds of analysis were conducted. Initially, the first author reviewed the included studies and labelled surgical procedures if a study specified the procedures. After the first round of coding, the first author noted that the levels of specificity of surgical procedures were varied across the studies and the list of them did not give any concrete information. Therefore, the first author discussed with the third author who specialized in surgery to categorize the studies and ensure the clinical validity. While there were many other ways to categorize the included studies with surgical perspectives such as planned or emergency surgery and daytime or after-hour surgery, the first and third authors decided to categorize the studies into three groups depending on surgical platforms that were considered in the studies: open, laparoscopic, and robot-assisted surgery. This is because previous studies on surgical teams suggested that team behaviors and dynamics are different between open, laparoscopic, and robotic surgery.45,65 Moreover, the categories indicate the surgical practices utilized across a wide range of operations from open to robot-assisted surgery.66,67 Open surgery requires a large incision for reaching the surgical site which is a major cause of postoperative pains and wound infections. Surgeons developed new ways to complete the surgical procedures through small incisions. A special visualization device, the endoscope, was invented in the 1980s which could be inserted to the patient’s body via these small incisions. Together with the use of long-shaft tools, surgeons were able to fulfill surgical goals with minimal trauma to the patients. When performed in the abdominal area, this type of minimally invasive procedure was often called laparoscopic procedure and it was recognized as an evolution of surgical technology.66 While patients prefer to accept laparoscopic surgery rather than open surgery due to less trauma and fast recovery, surgeons encounter more technical difficulties in performing laparoscopic procedures. The challenges came from the poor image qualities, loss of depth perception, difficulties in manipulation of the long instruments, and misalignment between image and manipulation.68–70 Earlier studies reported that surgeons undertaking laparoscopic procedures experienced a higher level of stress than performing open procedures.29,71 To target these drawbacks, robotic surgical platforms were developed which provided a 3D view of the surgical field and allowed surgeons to enhance their precision in manipulation.70,72 Therefore, in this review, we examined stressors in the OR and compared them over the open, laparoscopic, and robotic surgical approaches, aiming to investigate how researchers defined problems related to intraoperative stress regarding different surgical platforms.
Additionally, we categorized the included studies based on study participants. This categorization demonstrated how the existing literature defined the problem related to intraoperative stress from the perspective of various OR professionals. First, we reviewed the included studies based on the consideration of four professional sub-teams in the OR: a surgical team (eg, primary surgeons, assistant surgeons), a nursing team (eg, circulating nurses, scrub nurses), an anesthetic team (eg, anesthesiologists and anesthetic assistants), and a technician team. Therefore, we first labelled what types of OR professionals (eg, surgeons, OR nurses, anesthesiologists) were considered in the studies. Then, we focused on whether studies investigated intraoperative stress from the individual (ie, a single OR professional) or team (ie, a team of OR professionals) perspectives. In sum, each paper was coded with two dimensions, surgical platforms and study participants.
Thematic Synthesis
Before conducting a thematic synthesis,64 we first analyzed the types of research designs employed in the selected studies. This approach was taken to figure out how stressors were incorporated in each study. As a result, we identified 10 exploratory (11%), 9 descriptive (10%), 69 experimental (73%), and 6 mixed-methods (6%) studies. In the case of six mixed-methods research studies,15,73–77 the authors employed both exploratory and experimental research approaches to identify sources of distractions in the OR through observations and to examine the effect of stressors on surgical outcomes. Likewise, depending on research designs applied in each study, the intraoperative stressors were mentioned in different sections of each article. Therefore, we used the research design of each study as an analytical lens to identify intraoperative stressors. For example, in the case of exploratory research articles investigating stressors through observations or interviews, we focused on the methodologies and findings sections because preliminary themes were presented in the methodologies section and new emerging themes derived from observation and interview were described in the findings section. For descriptive research articles, we looked into the methodologies section where survey items were presented. Additionally, in experimental research articles that examined the effects of stressors, we particularly focused on the methodologies section where the authors clarified experimental contexts. We identified stressors by checking independent variables that were applied to induce the intraoperative stress and control variables that were predefined to build experimental contexts. As the main goal of this mixed-methods systematic review paper is to identify intraoperative stressors, we incorporated all stressors that were considered in the included studies regardless of their statistical significance.
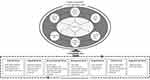
With the considerations of research designs employed in the included studies, a thematic synthesis45,64 was performed. Four phases were rigorously conducted to translate the existing literature about intraoperative stress of clinical personnel by following Pluye and Hong46’s guidance. Initially, depending on the research design employed by each article, the first author immersed herself into the data by delving into the methodologies and results sections. Next, the first author performed a free line-by-line coding in each study and identified all instances of intraoperative stressors regardless of their statistical significance. All codes were recorded in a spreadsheet. Moving forward, the first author organized the initial codes into descriptive themes by considering their similarities and differences. The first, third, and fourth authors reviewed the previous literature4,21,28,78 on intraoperative stressors and refined the descriptive themes. Lastly, to validate the themes, discussions were held among all authors. The third author, an experienced surgeon, also actively engaged in defining and clarifying the themes to apply the challenges in surgical practices. During the discussions, the authors went back and forth from initial codes to the themes. They tried to denote all stressors in the same abstraction level and specified the subtypes of each stressor by presenting the initial codes. After three rounds of discussions between authors, all authors made general agreement on the themes. Then, they denoted seven stressors for OR personnel during surgery and characterized each stressor with its subtypes. In Figure 2, the occurrence of each intraoperative stressor is presented. Since a number of studies examined or identified more than one stressor, they were coded with multiple stressors.
As we derived seven stressors based on the included studies that investigated intraoperative stress by conducting empirical research, our framework cannot cover all possible factors related to intraoperative stress which can be derived from non-empirical research. However, with seven identified stressors, we aimed to address how previous studies had defined and characterized intraoperative stressors for OR personnel. This perspective for our thematic synthesis would help us to further understand challenges of clinical personnel in the OR by an inductive way.
Results
In this section, we first provide a high-level overview of reviewed papers by addressing how the studies defined problems regarding surgical platforms and study participants. Then, we present seven types of stressors and explain how the previous studies defined and examined the intraoperative stressors for OR professionals. A full list of 94 selected studies and results of our textual narrative synthesis and thematic synthesis can be found in https://bit.ly/3rJZg6T.
Overview of Reviewed Papers
Surgical Platforms
Among the 94 studies, 69 studies (74.19%) defined their research scope with surgical platforms (see Table 1). The remaining 25 studies (22.11%) did not specify what surgical platforms they focused on. Therefore, only 69 studies (74.19%) were considered to analyze the types of surgical platforms. Among them, 52 studies focused on a single surgical platform. The rest of the studies (n = 17) examined two or more surgical platforms and compared the effects of different types of the surgical platforms on intraoperative stress, teamwork, and surgical performance. Due to 17 papers considered multiple surgical platforms, the combined percentages of the occurrence of each surgical platform are larger than 100% in Table 1.
 |
Table 1 Types of Surgical Platforms Investigated in the 94 Selected Studies |
The minimally invasive surgery (MIS) (n = 54) was considered more often than open surgery (n = 20) in the included studies. Three studies15,76,91 compared the impact of open surgery and MIS on the workload of clinical personnel in the OR. Most of the MIS studies focused on non-robotic surgeries (eg, laparoscopic/endoscopic surgery, arthroscopic knee surgery) and only 13 studies particularly investigated robot-assisted surgeries. Among 54 studies related to MIS procedures, the laparoscopic surgery (LPS) (n = 44) was the most frequently examined surgical platforms in our collected studies. In addition to the traditional laparoscopic procedures, the researchers applied various types of laparoscopic procedures to examine the impact of different LPS procedures on surgeon’s stress and surgical performance (eg, robot-assisted LPS (n = 11),24,85,99,103,107–109,113,115,118,125 3D LPS (n = 1),100 and hand-assisted LPS (n = 1)85). We also found 10 studies that investigated how different LPS procedures would affect surgeon’s stress and performance. Seven studies99,107,108,113,115,118,125 examined the difference between robot-assisted LPS and traditional LPS. One study100 focused on the differences between 3D and 2D LPS. Moreover, two studies111,145 compared different surgical approaches in LPS by analyzing the impact of four-port and single incision procedures on a surgical team’s workload.
Study Participants
Among the 94 selected studies, we first investigated if the studies focused on a single surgical role or a group of OR professionals. We found that 76 studies investigated intraoperative stress by focusing on a single OR professional. The majority of the selected studies investigated the intraoperative stress from surgeons’ perspective (n = 71), followed by OR nurses (n = 4) (eg, scrub nurse, circulating nurse, and nurse anesthetist), and anesthesiologists (n = 1) (see Table 2). Among the four studies focusing on OR nurses, one study133 explored the nursing team as a whole, but three studies specified the nursing roles. For example, Mitchell et al139 only focused on scrub nurses. Two other studies25,143 applied the nursing roles as a between-subjects factor and compared how different nursing roles would affect the intraoperative stress. For example, Sonoda et al25 investigated scrub nurses and circulating nurses and Tseng and Liu143 focused on the circulating nurses and anesthesia nurses who work in a non-sterile field. On the other hand, 18 studies (19%) addressed intraoperative stress from the OR team perspective. In general, the OR team includes primary and assistant surgeons, trainees, OR nurses, anesthesiologists, and surgical technicians.
 |
Table 2 Types of Participants Investigated in the 94 Selected Studies |
While one study15 explored disruptions in the OR from the whole team perspective, the other 17 studies specified their targeted groups based on their research scope. Specifically, five studies109,117,120,127,144 particularly focused on surgeons and OR nurses (ie, scrub nurse, circulating nurse, nurse anesthetist). The remaining 12 studies included all OR professionals. Hull et al1 categorized OR professionals into three sub-groups: a surgical team (ie, primary operating surgeon and assistant surgeon), a nursing team (ie, scrub nurse and circulating nurse), and an anesthetic team (ie, anesthesiologist and anesthetic assistant). On the other hand, Lowndes et al145 defined two sub-groups by considering whether OR team members work in a sterile field or not.
Seven Intraoperative Stressors for or Personnel
Based on the thematic synthesis, we derived seven intraoperative stressors including Technical, Individual, Operating Room (OR) Environmental, Interpersonal, Temporal, Patient, and Organizational factors. In Table 3, we present the definitions and examples of each stressor. These stressors were identified based on how the selected studies defined or examined factors causing intraoperative stress but not based on their statistical significance effects on intraoperative stress. Therefore, in this section, we aimed to present various characteristics of intraoperative stressors. In this regard, for five stressors including technical, individual, OR environmental, interpersonal, and temporal factors, we further classified them into their subtypes. The subtypes of each stressor were used to present examples of the stressors and organize our findings. However, we did not define subtypes of patient and organizational factors because there were only a few studies that specifically described characteristics of these stressors. Figure 2 demonstrates the distributions of 94 studies across seven stressors. The stacked bar graph represents the proportion of studies that were conducted by four different research designs: experimental, descriptive, exploratory, and mixed-methods research. The types of research designs, stressors, and stressor subtypes that were identified in the collected studies can be found in https://bit.ly/3rJZg6T. Technical factors (n = 54) were the most frequently examined stressors followed by individual (n = 39), OR environmental (n = 31), interpersonal (n = 20), temporal (n = 20), patient (n = 9), and organizational factors (n = 1). As we noticed that some papers examined multiple stressors, we present Table 4 that demonstrates the number of examined stressors. However, we leave room for interpretation of studies employing multiple stressors. These questions will be addressed in the Discussion.
 |
Table 3 Seven Intraoperative Stressors for or Personnel |
 |
Table 4 Categorization of 94 Studies According to the Number of Examined Stressors |
Technical Factors
Technical factors refer to the attributes of procedures that determine technical ease or difficulty in the performance of surgery. Therefore, technical factors include different types of surgical approaches as well as training and technological interventions. We identified 54 studies (57.45%) that investigated technical factors and five subtypes of technical factors (see Table 5). Two studies actually used the term “technical factors” to describe stressful events in the OR that arose from the complexity of surgical approaches.3,129 However, they did not present exact situations or tasks that caused the change of surgical complexity. Therefore, with the rest of the studies (n = 52), we specified how researchers employed the technical factors to understand and investigate intraoperative stress in various contexts. These 52 studies can be categorized into four subtypes based on what variables they used to define the technical factors: multi-tasking conditions (n = 3), surgical approaches (n = 30) (eg, surgical platforms, surgical techniques, and tasks), training interventions (n = 3), and technological interventions (n = 17).
 |
Table 5 Five Subtypes of Technical Factors Identified from 54 Studies |
The first group of studies (n = 3) designed a multi-tasking condition that causes surgical complications in laboratory settings.12,113,116 Specifically, two studies113,116 asked participants to perform case-irrelevant tasks while completing surgical tasks.
The second group of studies (n = 30) applied various surgical approaches by considering their surgical complications. They defined technical challenges by considering different aspects: surgical procedures, surgical platforms, surgical techniques and tasks. Ten studies particularly focused on a single surgical approach (eg, laparoscopic surgery,102,113,126,153 telesurgery,24,127 intracranial aneurysm procedure,87 knee arthroscopy,148 thoracoscopic pulmonary lobectomy,152 natural orifice transluminal endoscopic surgery147). Some of them specified technical issues related to surgical procedures in terms of navigation,102,147 ergonomics,126,147,152 and visualization.102,148
While the aforementioned ten studies addressed a single surgical approach to define technical factors, 20 studies presented at least two different surgical approaches and compared their impacts on stress and performance.76,81,85,89,91,93,97,99,100,103,107,108,111,115,118,125,138,142,145,151 Except one study138 categorizing surgical procedures depending on technical difficulty (ie, easy/intermediate/complex), the remaining 19 studies compared newly introduced surgical approaches with conventional surgical approaches. Twelve studies defined surgical complexity by categorizing surgical approaches based on operative platforms (ie, open surgery, minimally invasive surgery, 2D/3D laparoscopic surgery, robot-assisted surgery).76,85,91,99,100,103,107,108,115,118,125,142 Furthermore, five studies investigated how different surgical techniques would cause mental and physical challenges of OR team members.81,89,111,145,151 Among them, three studies111,145,151 investigated the difference between single and multiple incision techniques in terms of their impact on intraoperative stress for OR team members. They reported that the single incision may provide benefits to patient outcomes but would rather hinder surgical workflow. Another two studies defined the technical difficulty in surgical task levels.93,97 For example, Berg et al97 applied two surgical tasks in laparoscopy which were composed of simple (eg, peg transfer) and complex (eg, intracorporeal) tasks, and examined the impact of heat stress on performance under different levels of complexity.
While the previous two groups of studies focused on technical difficulty in surgical approaches, the last two groups of studies developed interventions that can reduce surgical complications and alleviate OR team member pain points. Three studies evaluated the efficiency of new training interventions (eg, structured training,104 team-based simulation training,146 noise-reduction program16) by measuring surgeons’ stress and performance.
The last group of studies (n = 18) reported technological interventions (eg, surgical instruments and tools) that may alleviate the effect of technical challenges in the OR. Ten studies highlighted the importance of using ergonomic principles in the design of surgical instruments. Except two studies,86,90 eight studies focused on technical difficulty of laparoscopy that caused physical stress and musculoskeletal pain for surgeons. Particularly, three studies focused on laparoscopic tools.94,119,123 For instance, Tung et al123 and Sreekanth et al119 proposed new grip designs that would ease an operator’s physical discomfort and validated the efficiency of the tools by measuring stress and performance. Furthermore, five studies examined technological interventions that can support surgeons posture.105,114,121,124,149 One study124 developed an upper body digital human model to predict an ergonomic height for surgical tables. The remaining four studies examined the benefits of posture-support instruments for laparoscopy such as arm rests,121,149 knee rests,114 and surgical chairs.105,149 Beyond ergonomic interventions, three studies examined other technological interventions that could ease stress for a surgical team by minimizing intraoperative noise17,109 and increasing visibility of surgical fields.96 Furthermore, four studies particularly featured the importance of visual information that can support OR team members’ decision-making in the OR. One study80 explored the feasibility of introducing mixed-reality in the operating room. The remaining three studies focused on image-guided navigation systems.83,84,150
Individual Factors
Individual factors refer to attributes of OR personnel. A total of 39 studies related to the individual factors were identified. Four subtypes of the individual factors were identified: expertise (n = 22), roles of OR personnel (n = 15), specialties (n = 2), and other personal properties (n = 5) (see Table 6).
 |
Table 6 Four Subtypes of Individual Factors Identified from 39 Studies |
Twenty-two studies categorized OR personnel, especially for surgeons, by considering their different levels of expertise. In general, medical students become attending surgeons through post-graduate training programs by beginning as interns and becoming residents and fellows. The different stages of the training also represent varying skills, roles, and responsibilities.154 In this regard, the hierarchy is the most common criteria to determine the expertise of surgeons. While four studies only focused on one targeted group that was composed of surgeons with the same levels of expertise (eg, medical students,18,73 residents,146 attending surgeons74), the rest of studies (n = 18) considered the levels of expertise to categorize participants for a between-subjects design. Among these 18 studies, fifteen studies determined the expertise levels of surgeons by considering different stages of the training program.8,12,28,79,82,88,95,101,104,108,117,122,129,140,147 For instance, four studies79,95,104,129 classified two groups of surgeons depending on their expertise into the trainee group (eg, interns, residents) and expert group (eg, consultants, senior staff surgeons) and compared the impact of interventions on these two groups. Rather than only considering the title of surgeons, six studies determined expertise of surgeons by employing additional variables such as years of experience in surgery,102,122,128,138 surgical volume,102 and the number of specific operating cases.102,122,128,140,147 In addition to the objective measures that define the levels of expertise, one study128 included surgeons’ self-estimation of their expertise in minimally invasive surgery as one of the individual factors. Fifteen studies particularly characterized OR personnel based on their roles in the OR. Particularly, eight studies examined how OR personnel in different professional groups (eg, surgical, nursing, and anesthesia teams) were affected by stressors.117,120,130,134,135,139,144,145 Another seven studies narrowed down their interests to one professional group. Specifically, two studies25,143 focused on the nursing teams and examined how stressors would impact the stress and performance of circulating and scrub nurses who have different roles and responsibilities. The other five studies examined how the surgical roles (eg, primary and assistant roles) would affect surgeons’ stress response.82,85,87,88,126
Surgical specialty of OR personnel (n = 2) was another individual subtype assessed in relation to stressful situations in the OR.76,135 Another five studies considered more about other personal properties like emotional intelligence,28 cognitive styles,18 and personal problems3,75,136 as individual factors.
Besides the aforementioned studies that considered one single subtype of individual factors in their analysis, four studies applied multiple subtypes of individual factors to understand the intraoperative stress.82,88,117,135 One study135 applied both surgical specialties and roles to categorize OR personnel. Two studies examined how surgical roles (ie, primary surgeon and assistant) would differently affect surgeon’s stress depending on surgeons’ levels of expertise.82,88 The last study117 classified a surgical team based on expertise levels of surgeons but categorized a nursing team depending on their roles in their study of associations between intraoperative stress and individual factors.
Operating Room Environmental Factors
Operating room (OR) environmental factors refer to elements that are required to ensure safe and efficient running of operations. These factors include both physical (eg, tools, equipment, operating room layouts) and ambient environments (eg, noise, light, temperature) in the OR. We noted that the OR environmental factors have overlapped with intraoperative sources of “distractions” that the previous literature has investigated.8,19–21 However, we found that the previous literature also included interpersonal interactions (eg, communication between OR personnel) as sources of distractions8,19 which were defined as interpersonal factors in this review paper. By identifying studies considering the physical and ambient environments in the OR, we found 31 studies employing the OR environmental factors. The identified OR environmental factors can be categorized into four subtypes: acoustic noise (n = 24), misarrangement of surgical tools and technical malfunctions of surgical instruments (n = 7), integrated operating room design (n = 2), and other OR environment properties (n = 5) (see Table 7).
 |
Table 7 Four Subtypes of or Environmental Factors Identified from 31 Studies |
Acoustic noise was the most frequent subtype among OR environmental stressors among OR environmental factors (n = 24).3,16,17,26,74,75,77,92,98,101,109,112,113,129–132,136,137,140,141,143,144,155 We found five studies16,17,109,132,143 assessing the impact of intraoperative noise volume on OR personnel’s stress. On the other hand, 12 studies explored types of the acoustic noise that induced the OR team’s stress and even affected their surgical performance. Sources of intraoperative noise mentioned in these studies included phone calls, beepers, pagers, radio, and noises from surgical instruments.3,74,75,77,92,98,113,129–131,136,155
Although the aforementioned acoustic noise is considered as disruptive sources that need to be prevented and minimized in the OR, nine studies considered music as a possible solution to relieve stress of the OR team along with improving surgical performance.17,101,112,136,137,140,141,143,144 While four studies examined the overall impact of music on stress and performance,26,101,137,140 the remaining five studies investigated how OR staff’ stress, performance, and preference are shaped by different volume levels17,143 and music genres (eg, pop, classic, rap).112,141,144
Beyond the acoustic ambience, seven studies15,18,74,77,117,130,131 pinpointed the misarrangement of surgical tools and technical malfunctions of surgical tools as the two main OR work environmental factors that impede the surgical workflow.
Furthermore, two studies106,120 highlighted the needs for building an integrated operating room that can minimize the tensions raised by new surgical platforms. They particularly focused on new working environments driven by laparoscopy and examined the effect of an integrated operating room, equipped with movable monitors and laparoscopy racks, on stress106,120 and teamwork.106,120 We also found other OR environmental properties such as the number of people,76,77,130 illumination,15 and temperature.97
Interpersonal Factors
In the operating room, multiple people with different expertise and skills need to work together to provide an optimal patient care. To coordinate their work and foster an effective team collaboration, it is important to understand interpersonal factors that characterize relationships, interactions, and communication between people in the OR.156 We identified 20 studies investigating interpersonal factors. These studies pinpointed that a successful surgery cannot be done by individuals alone but by a team. Six studies highlighted the importance of working as a team in the OR by using general terms such as team, teamwork, and coordination (Arora et al, 2010a; Bakhsh et al, 2019; Chrouser and Partin, 2019; Holmes et al, 2020; Keller et al, 2020; Sami et al, 2012). In addition to these cases, we identified four subtypes of interpersonal factors that described more specific contexts: communication (n = 9), teaching (n = 5), assistance (n = 4), and relationship (n = 2) (see Table 8).
 |
Table 8 Five Subtypes of Interpersonal Factors Identified from 20 Studies |
The most frequently mentioned interpersonal factor among the collected studies was communication (n = 9). Three studies15,26,136 highlighted the importance of effective communication among team members. Beyond the effectiveness of communication, six studies8,18,74,77,130,131 observed the frequency of occurrence of case-irrelevant communication (CIC) and examined how CIC affects stress and teamwork. They considered CIC as one source of distraction in the OR. While three studies8,18,74 only focused on the type of information shared during interpersonal communication, the remaining three studies77,130,131 classified CIC depending on the initiator of the communication, either OR team members (ie, surgeon, anesthesiologist, nurse) or external staff.
Next, we identified five studies focusing on the interpersonal interactions in teaching and mentoring cases.74–76,88,116 While four studies examined the primary surgeons’ stress levels when they taught or mentored colleagues, students, or assistants during surgery,74–76,88 one study116 focused on trainees’ perspectives in teaching cases. Specifically, Poolton et al116 considered interpersonal interactions during intraoperative teaching as one stressor for trainees who would experience because they had to be evaluated by attending surgeons. Four studies investigated how surgeon’s stress and performance were affected by other team members’ mistakes such as poor role understanding,73 staff mistakes,73 and poor assistance.12,129,136 Lastly, two studies mentioned interpersonal relationship between team members such as team familiarity73 and relationship issues between surgical members (eg, trainees and attending surgeons)129 as potential interpersonal stressors.
Temporal Factors
Temporal factors refer to time-level characteristics of stressful situations in the OR. We identified 20 studies examining temporal factors and further categorized them into three subtypes: time constraints (n = 8), operation time (n = 4), and surgical phases (n = 8) (see Table 9).
 |
Table 9 Three Subtypes of Temporal Factors Identified from 20 Studies |
Eight studies3,9,12,75,113,116,118,129 investigated how time constraints of performing surgery would impact surgeons’ stress and performance. In other words, the difficulty with time management was considered as one stressor for surgeons during surgery.3,75 In this regard, several terminologies such as “time pressure/temporal demand”12,116 and “lack of operation time”75,129 were used to describe the time constraints in the OR. Using simulated scenarios in which surgeons had to manage time constraints during surgery, five studies9,12,113,116,118 investigated the effect of stressful situations on surgical performance and stress. Among them, two studies113,118 employed temporal factors to examine whether new or conventional surgical platforms enabled surgeons to better manage stressful situations during surgery.
Second, four studies reported operation time or procedure duration as temporal factors that would affect stress and surgical performance. Weigl et al76 reported that longer surgical procedures caused more perceived stress for surgeons. Sonoda et al25 also considered the operation start time and anesthesia time to examine factors related to surgical nurses’ stress and team performance. As the duration of operation time affects mental and physical stress, Park et al142 and Engelmann et al98 introduced intraoperative breaks which were identified to alleviate surgeon’s stress and improve performance.
The last group of the studies (n = 8) used surgical phases to measure how one’s stress or performance changes over time.11,82,130,134,135,143,145,150 Kuhn et al82 specified 16 surgical phases by annotating all surgical tasks required to perform cardiac surgery and assessed physiological stress for surgeons during surgery. Tseng and Liu143 defined surgical phases based on specific tasks that nurses performed during surgery. However, other researchers denoted the surgical phases in a simpler way. Two studies analyzed the temporal patterns of episodes when OR team members experienced stress135 and interruptions130 by dividing the whole surgical duration into several phases. The rest of the studies referred to the surgical phases in a conventional way (ie, pre-operative, intraoperative, and post-operative phases) to assess changes in physiological stress11,145,150 and perceived stress and teamwork.134
Patient Factors
Nine studies addressed patient factors as stressors for surgeons. The patient factors refer to patient-level characteristics that can determine the difficulty of performing surgeries such as age,74,117 sex,74,117 Body Mass Index (BMI),74,110,117 past surgical history,74 individual anatomy,73,74 comorbidities,74,117 and patient health status.15,92 However, not all studies explicitly presented a definition or example for the patient factors. Sami et al75 and Arora et al3 performed observations to derive patient factors as one of the stressors and referred them as “patient problems.” They defined the patient problems by describing situations that surgeons need to treat an unwell patient. By setting up a simulated experiment when surgeons must perform surgeries for high-risk patient, two studies12,92 investigated how surgeons’ coping strategies would facilitate their surgical performance under the stressful situation.
Other studies gave more detailed definitions of patient factors. Chrouser and Partin73 defined a patient factor as “an unexpected event, adverse event, difficult case, patient anatomy, surgeon concerned about patient, and high-profile patient.” Jung et al74 addressed a set of patient factors such as age, sex, history of previous abdominal surgery, BMI, and Charlson Comorbidity Index, and examined how these patient factors would affect attending surgeons’ perceived distractions. Liang et al110 particularly examined the impact of patient BMI on surgeon’s physical stress during laparoscopic surgery.
Organizational Factors
Organizational factors refer to structure, process, and climate of hospitals that would affect and shape clinical personnel’s attitude and behavior in the OR. In the selected studies, we only found one study15 identifying the organizational factors along with other stressors (eg, OR environmental, interpersonal, and patient factors). The authors examined the impact of preventable disruptions on operating time for minimally invasive surgery and particularly addressed organizational factors such as hospital protocols or surgery policies.
Discussion
With 94 empirical studies examining intraoperative stress of clinical personnel, we first addressed how each study defined a problem space regarding surgical platforms and study participants. To cover all possible intraoperative stressors for OR personnel, we examine what types of the stressors have been reported in the collected studies regardless of their significant effects on stress. As a result, we identified seven intraoperative stressors for clinical personnel and articulated the characteristics of each stressor. These stressors are determined by various dimensions including technical, individual, interpersonal, OR environmental, temporal, patient, and organizational perspectives. Under these potential stressors, multi-disciplinary team members carry out individual and collective work in the OR. In other words, to pursue patient safety, a team ecosystem needs to adapt to challenges driven by the potential stressors.157,158 Based on the identified stressors and the previous literature on team dynamics,156,159 Figure 3 is presented to illustrate the team ecosystem which is built and managed by the complexity of interactions between the team members.
By reflecting the complex interactions between the team ecosystem and intraoperative stressors in Figure 3, we will discuss what should be further explored to build a safe and efficient environment for OR personnel with the following three questions: What types of research designs have been used to examine intraoperative stress, what should be further investigated to understand intraoperative stress, and how we can interpret studies examining multiple stressors.
What Types of Research Designs Have Been Used to Examine Intraoperative Stress?
Using the insight that various stressors can simultaneously affect the team ecosystem, we further analyzed the types of research designs researchers employed to investigate intraoperative stress. As demonstrated in Figure 2, the majority of the selected studies (n = 69, 73%) employed experimental designs to investigate intraoperative stress. Only 25 studies (27%) applied other types of research designs: 10 exploratory, 9 descriptive, and 6 mixed-methods studies. The skewed trend towards the experimental research was also identified when we cross-tabulated the selected studies and delved into the ratio of the research designs that were applied. Except for interpersonal (35%), patient (33%), and organizational (0%) factors, more than 50% of studies that investigated the technical (85%), individual (64%), temporal (65%), and OR environmental factors (52%) applied experimental research methods. With advanced technologies in healthcare systems, the team ecosystem becomes more complex and is intertwined by various stressors. The performance of the team can no longer be understood by cause–effect relations which are described by linear models in experimental designs.160,161 As shown in Figure 3, a more holistic view is required to understand how the team ecosystem is managed and maintained by interactions between multi-disciplinary members who are affected by multiple stressors.162 We suggest that more exploratory research and mixed-method research are needed to further investigate how one stressor is shaped by another stressor and how the interactions between stressors affect OR team members’ performance and, thereby, the surgical outcomes. Such systematic understanding of stressors will contribute to building a framework that can be utilized to investigate and model the dynamic interactions in the OR (eg, between OR personnel, surgical approaches, and technologies).157
What Should Be Further Investigated to Understand Intraoperative Stress?
While reviewing the included studies, we noted under-investigated research areas that should be further explored to understand intraoperative stress and build a safe and efficient environment for OR personnel. In Results, we identified types of surgical platforms and participants investigated in the selected studies. Among 69 studies clarifying their research scope with surgical platforms, 54 studies focused on minimally invasive surgery (MIS). Compared to laparoscopic surgery (n = 44), few studies (n = 13) examined issues related to intraoperative stress in robot-assisted surgery. These findings reflect the current trends in surgical practice where open surgery is being replaced by MIS163 and robot-assisted surgery is becoming popular.67 Also, it implies the importance of further investigation of robotic-assisted surgery which may generate new subtypes of stressors in the OR.
With the categorization of study participants, we noted that 81% (n = 76) of the selected studies focused on a single OR profession, mainly surgeons (n = 71). The remaining (n = 5) articles tackled the intraoperative stress from other OR professionals’ perspectives (eg, OR nurses, anesthesiologists) (see Table 2). This skewed trend was also found in 39 studies that investigated individual factors. Among the four subtypes of individual factors (ie, clinical expertise, roles, specialties, and other personal properties), the expertise of OR personnel was the most frequently investigated factor; still, this subtype was only applied to determine surgical skill levels of surgeons. Although 38% (n = 15) of studies investigating individual factors considered various OR professions to define the roles of OR team members, only half of these studies (n = 8) investigated the intraoperative stress from the OR team perspective by considering more than one sub-OR team’s roles and responsibilities (eg, a surgical team, a nursing team, and an anesthetic team). The ecosystem of the operating room is not only built on the individual performance but also on the interactions within the OR team (Figure 3). In fact, the collective effort of various OR professionals is required to maintain a safe and effective care environment for patients.25,164 However, as we identified in Interpersonal factors, only 21% of the selected studies examined the interpersonal factors that build teamwork and group dynamics in the OR. This finding calls attention to further investigations on how communication, interactions, and relationships between people in the OR affect their intraoperative stress.
In addition to the interpersonal factors, temporal factors (21%), patient factors (10%), and organizational factors (1%) were the under-represented stressors. This might be because these factors are pre-defined by surgery schedules, patients, and hospitals and cannot be controlled in empirical studies. While the temporal and patient factors determine surgical complexities affecting intraoperative stress, the organizational factors shape work practices and influence how people collaborate with each other and interact with technological interventions in the OR.165,166 The reason for obtaining only one study15 addressing organizational factors may be in line with the inclusion and exclusion criteria of selecting studies. Specifically, we excluded studies that solely focused on OR professionals’ chronic stress (eg, burnout, well-being, depression) which can result from organizational factors in a long term. Moreover, the paucity of studies examining organizational factors is also aligned with what Tomo and De Simone167 identified in their systematic review paper. They also noted that a relatively low number of studies had investigated the well-being of clinical personnel using organizational perspectives. The organizational characteristics are one of the critical factors reconfiguring other stressors such as what interventions are built in the OR (ie, technical factors), how the OR team is coordinated (ie, individual and interpersonal factors), and how the operating room is organized and designed (ie, OR environmental factors).168,169 In this regard, our results highlight the need for researchers to further investigate how the under-represented factors affect the team ecosystem and what should be considered to minimize intraoperative stress for clinical personnel.170
How We Can Interpret Studies Examining Multiple Stressors
Operating room personnel are surrounded by multiple stressors that interact with each other. Therefore, beyond focusing on the characteristics of each stressor, the dynamic OR environments where multiple stressors exist need to be further investigated. While we coded stressors that were investigated in each study, more than half of the selected studies (n = 48, 51%) employed multiple stressors to define contexts in which OR personnel experienced stress and to examine the impact of these stressors on surgical outcomes (see Table 4). To delineate this trend, we categorized the selected studies regarding the types of examined stressors and their co-occurrence. Studies employing a non-technical factor often combined multiple stressors to examine intraoperative stress. In fact, more than 75% of studies that investigated some of the six non-technical factors examined at least two stressors (individual factors: 85%, OR environmental factors: 77%, interpersonal factors: 95%, temporal factors: 90%, patient factors: 89%, organizational factors: 100%). On the other hand, only 44% of studies examining technical factors investigated multiple stressors. Given that technical factors were the most investigated, this finding implies that the potential tensions raised by interactions between technical factors and other stressors are under-explored. Given that 85% of studies examining technical factors applied experimental research approaches, these results might be because of the difficulty of setting up non-technical stressors as another experimental variable to investigate the impact of technical factors on surgical outcomes. However, we need to note that the impact of technical factors can be shaped by various user scenarios: who uses the intervention (individual factors), how the intervention affects interactions between OR personnel (interpersonal factors), and where and when the intervention is being used (OR environmental, organizational, temporal, and patient factors). In this regard, we delved deeper into the 54 studies investigating technical factors among the 94 selected studies.
The subtypes of technical factors can be largely classified into two different groups depending on what causes the technical complexity. While the first group of 34 studies focused on surgical approaches, the second group of 20 studies were related to technological (n = 17) and training (n = 3) interventions developed to alleviate the OR team’s stress. With these two groups, we categorized 54 studies examining technical factors according to the number of stressors (see Table 10); for example, if the number of stressors is three, the study examined two additional stressors in addition to technical factors. With this categorization, we noted that the ratio of studies examining multiple stressors was much higher in studies examining surgical approaches (Group 1: 18 studies, 53%) than in studies investigating technological and training interventions (Group 2: 6 studies, 30%). Likewise, researchers carefully examined the efficiency of various surgical approaches by considering multiple stressors. However, in terms of examining the technological and training interventions, they focused on the efficiency of the interventions on the surgical outcomes (ie, only employing a technical factor). They less so considered how the interaction between newly introduced interventions and other non-technical stressors (ie, individual, OR environmental, interpersonal, temporal, patient, and organizational factors) would affect the team ecosystem and surgical outcomes in the end.31,38,74,171 The adverse effects led by this gap solely go to the individual and collective performance during surgery and could be detrimental to patient safety.45,162 Therefore, to maximize the benefits of the new interventions on the surgical outcomes, it is critical to understand the dynamic interactions between stressors in designing and developing technologies in the OR.15,74,80,172 This effort is fundamental to build a safe and efficient ecosystem in the OR and should be considered as a role and responsibility of human factors practitioners and researchers working in healthcare systems.
 |
Table 10 Categorization of 54 Studies Examining Technical Factors According to the Number of Stressors |
Conclusion
With 94 selected studies published from 2010 to 2020, we present a mixed-methods systematic review on intraoperative stressors. The main goals of this review are to identify intraoperative stressors that have been reported in previous literature and elaborate the characteristics of each stressor. To accomplish the study goals, two analysis approaches are applied. We first perform a textual narrative synthesis to investigate the characteristics of 94 studies in terms of surgical platforms and participants considered in the selected studies. The majority of the selected studies particularly investigated the intraoperative stress from surgeons’ perspectives while rarely addressing the other OR personnel. Also, most studies examined minimally invasive surgery, which is a relatively newer approach than open surgery, and investigated how surgical environments shaped by new surgical approaches would affect intraoperative stress. To present a broad landscape of intraoperative stressors, we conducted a thematic synthesis and identified seven intraoperative stressors: technical, individual, operating room environmental, interpersonal, temporal, patient, and organizational factors. Additionally, we examined the characteristics of each stressor by presenting subtypes of each stressor. By presenting stressors as multifaceted elements affecting the team ecosystem in the operating room, we discuss the potential interactions between stressors which should be further investigated to build a safe and efficient environment for OR personnel. This work brings important insights to a diverse group of stakeholders, such as clinical personnel who work in the OR under potential stressors, managers and directors of healthcare sectors who are in charge of maintaining a safe OR environment, and human factor researchers and practitioners who need to understand stressors to design and develop new interventions in the OR. As we conducted a mixed-methods systematic review, we did not address the significant effects of each stressor on intraoperative stress. To demonstrate the effects of each stressor on intraoperative stress for OR personnel, it is important to extend the current work by performing a meta-analysis. As a future research, seven identified stressors and their subtypes will be employed to conduct a meta-analysis on intraoperative stress for OR personnel.
Funding
The work was partially funded by an Academy of Finland grant [334658] and Emil Aaltonen foundation.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hull L, Arora S, Aggarwal R, Darzi A, Vincent C, Sevdalis N. The impact of nontechnical skills on technical performance in surgery: a systematic review. J Am Coll Surg. 2012;214(2):214–230. doi:10.1016/j.jamcollsurg.2011.10.016
2. Smith-Jentsch KA, Campbell GE, Milanovich DM, Reynolds AM. Measuring teamwork mental models to support training needs assessment, development, and evaluation: two empirical studies. J Organizational Behav. 2001;22(2):179–194. doi:10.1002/job.88
3. Arora S, Hull L, Sevdalis N, et al. Factors compromising safety in surgery: stressful events in the operating room. Am J Surgery. 2010;199(1):60–65. doi:10.1016/j.amjsurg.2009.07.036
4. Chrouser KL, Xu J, Hallbeck S, Weinger MB, Partin MR. The influence of stress responses on surgical performance and outcomes: literature review and the development of the surgical stress effects (SSE) framework. Am J Surgery. 2018;216(3):573–584. doi:10.1016/j.amjsurg.2018.02.017
5. Ng R, Chahine S, Lanting B, Howard J. Unpacking the literature on stress and resiliency: a narrative review focused on learners in the operating room. J Surg Educ. 2019;76(2):343–353. doi:10.1016/j.jsurg.2018.07.025
6. Lazarus RS, Folkman S. Stress, appraisal, and coping. Journal of Behavioral Medicine. 1984;7(4):375–389. doi:10.1007/BF00845271
7. Kim TJ, Seong PH. Influencing factors on situation assessment of human operators in unexpected plant conditions. Ann Nucl Energy. 2019;132:526–536. doi:10.1016/j.anucene.2019.06.051
8. Carr S, McDermott BR, McInerney N, Hussey A, Byrne D, Potter S. Determining the Effect of External Stressors and Cognitive Distraction on Microsurgical Skills and Performance. Front Surgery. 2020;6:77. doi:10.3389/fsurg.2019.00077
9. Modi HN, Singh H, Orihuela-Espina F, et al. Temporal stress in the operating room: brain engagement promotes “coping” and disengagement prompts “choking”. Ann Surg. 2018;267(4):683–691. doi:10.1097/SLA.0000000000002289
10. Yerkes RM, Dodson JD. The Relation of Strength of Stimulus to Rapidity of Habit Formation. J Comparative Neurol Psychol. 1908;18:459–482. doi:10.1002/cne.920180503
11. Phitayakorn R, Minehart RD, Pian-Smith MCM, Hemingway MW, Petrusa ER. Practicality of using galvanic skin response to measure intraoperative physiologic autonomic activation in operating room team members. Surgery. 2015;158(5):1415–1420. doi:10.1016/j.surg.2015.04.009
12. Wetzel CM, Black SA, Hanna GB, et al. The effects of stress and coping on surgical performance during simulations. Ann Surg. 2010;251(1):171–176. doi:10.1097/SLA.0b013e3181b3b2be
13. Anton NE, Howley LD, Pimentel M, Davis CK, Brown C, Stefanidis D. Effectiveness of a mental skills curriculum to reduce novices’ stress. J Surgical Res. 2016;206(1):199–205. doi:10.1016/j.jss.2016.07.019
14. Goodman T, Spry C. Essentials of perioperative nursing. Jones & Bartlett Publishers; 2014.
15. Al-Hakim L. The impact of preventable disruption on the operative time for minimally invasive surgery. Surg Endosc. 2011;25(10):3385–3392. doi:10.1007/s00464-011-1735-9
16. Engelmann CR, Neis JP, Kirschbaum C, Grote G, Ure BM. A noise-reduction program in a pediatric operation theatre is associated with surgeon’s benefits and a reduced rate of complications: a prospective controlled clinical trial. Ann Surg. 2014;259(5):1025–1033. doi:10.1097/SLA.0000000000000253
17. Ukegjini K, Kastiunig T, Widmann B, Warschkow R, Steffen T. Impact of intraoperative noise measurement on the surgeon stress and patient outcomes. A prospective, controlled, single-center clinical trial with 664 patients. Surgery. 2020;167(5):843–851. doi:10.1016/j.surg.2019.12.010
18. Pluyter JR, Buzink SN, Rutkowski A-F, Jakimowicz JJ. Do absorption and realistic distraction influence performance of component task surgical procedure? Surg Endosc. 2010;24(4):902–907. doi:10.1007/s00464-009-0689-7
19. Feuerbacher RL, Funk KH, Spight DH, Diggs BS, Hunter JG. Realistic distractions and interruptions that impair simulated surgical performance by novice surgeons. Arch Surg. 2012;147(11):1026–1030. doi:10.1001/archsurg.2012.1480
20. Koch A, Burns J, Catchpole K, Weigl M. Associations of workflow disruptions in the operating room with surgical outcomes: a systematic review and narrative synthesis. BMJ Qual Saf. 2020;29(12):1033–1045. doi:10.1136/bmjqs-2019-010639
21. Mentis HM, Chellali A, Manser K, Cao CGL, Schwaitzberg SD. A systematic review of the effect of distraction on surgeon performance: directions for operating room policy and surgical training. Surg Endosc. 2016;30(5):1713–1724. doi:10.1007/s00464-015-4443-z
22. Ford DA. Managing Distractions Through Advocacy, Education, and Change. Distracted Doctoring. 2017;3:169–187.
23. Gui JL, Nemergut EC, Forkin KT. Distraction in the operating room: a narrative review of environmental and self-initiated distractions and their effect on anesthesia providers. J Clin Anesth. 2021;68:110110. doi:10.1016/j.jclinane.2020.110110
24. Pelikan HRM, Cheatle A, Jung MF, Jackson SJ. Operating at a distance-how a teleoperated surgical robot reconfigures teamwork in the operating room. Proce ACM Human-Computer Interaction. 2018;2(CSCW):1–28. doi:10.1145/3274407
25. Sonoda Y, Onozuka D, Hagihara A. Factors related to teamwork performance and stress of operating room nurses. J Nurs Manag. 2018;26(1):66–73. doi:10.1111/jonm.12522
26. Kumar M, Dash HH, Chawla R. Communication skills of anesthesiologists: an Indian perspective. J Anaesthesiol Clin Pharmacol. 2013;29(3):372. doi:10.4103/0970-9185.117116
27. Romare C, Enlf P, Anderberg P, Jildenstl P, Sanmartin Berglund J, Skr L. Nurse anesthetists’ experiences using smart glasses to monitor patients’ vital signs during anesthesia care: a qualitative study. PLoS One. 2021;16(4):e0250122. doi:10.1371/journal.pone.0250122
28. Arora S, Russ S, Petrides KV, et al. Emotional intelligence and stress in medical students performing surgical tasks. Acad Med. 2011;86(10):1311–1317. doi:10.1097/ACM.0b013e31822bd7aa
29. Zheng B, Cassera MA, Martinec DV, Spaun GO, Swanstrm LL. Measuring mental workload during the performance of advanced laparoscopic tasks. Surg Endosc. 2010;24(1):45–50. doi:10.1007/s00464-009-0522-3
30. Dias RD, Ngo-Howard MC, Boskovski MT, Zenati MA, Yule SJ. Systematic review of measurement tools to assess surgeons’ intraoperative cognitive workload. Br J Surg. 2018;105(5):491. doi:10.1002/bjs.10795
31. Catchpole K, Bisantz A, Hallbeck MS, et al. Human factors in robotic assisted surgery: lessons from studies ‘in the Wild’. Appl Ergon. 2019;78:270–276. doi:10.1016/j.apergo.2018.02.011
32. Randell R, Honey S, Alvarado N, et al. Embedding robotic surgery into routine practice and impacts on communication and decision making: a review of the experience of surgical teams. Cognition Technol Work. 2016;18(2):423–437. doi:10.1007/s10111-016-0368-0
33. Dalager T, Sgaard K, Bech KT, Mogensen O, Jensen PT. Musculoskeletal pain among surgeons performing minimally invasive surgery: a systematic review. Surg Endosc. 2017;31(2):516–526. doi:10.1007/s00464-016-5020-9
34. Gabrielson AT, Clifton MM, Pavlovich CP, et al. Surgical ergonomics for urologists: a practical guide. Nat Rev Urol. 2021;18(3):160–169. doi:10.1038/s41585-020-00414-4
35. Blom EM, Verdaasdonk EGG, Stassen LPS, Stassen HG, Wieringa PA, Dankelman J. Analysis of verbal communication during teaching in the operating room and the potentials for surgical training. Surg Endosc. 2007;21(9):1560–1566. doi:10.1007/s00464-006-9161-0
36. ElBardissi AW, Sundt TM. Human factors and operating room safety. Surgical Clinics. 2012;92(1):21–35. doi:10.1016/j.suc.2011.11.007
37. Cunningham S, Cao CGL. Spatial communication in robotic surgery. Los Angeles, CA: SAGE Publications; 2012.
38. Lee A, Bednarik R. 3D Exoscopes in Microsurgery: how 3D Exoscopes Reconfigure the Workflow of Assistant Surgeons and Nurses in an Operating Room.
39. Sergeeva AV, Faraj S, Huysman M. Losing touch: an embodiment perspective on coordination in robotic surgery. Organization Sci. 2020;31(5):1248–1271. doi:10.1287/orsc.2019.1343
40. Carayon P, Bass EJ, Bellandi T, Gurses AP, Hallbeck MS, Mollo V. Sociotechnical systems analysis in health care: a research agenda. IIE Trans Healthc Syst Eng. 2011;1(3):145–160. doi:10.1080/19488300.2011.619158
41. Arora S, Sevdalis N, Nestel D, Woloshynowych M, Darzi A, Kneebone R. The impact of stress on surgical performance: a systematic review of the literature. Surgery. 2010;147(3):318–330. doi:10.1016/j.surg.2009.10.007
42. Catanzarite T, Tan-Kim J, Whitcomb EL, Menefee S. Ergonomics in surgery: a review. Female Pelvic Med Reconstr Surg. 2018;24(1):1–12. doi:10.1097/SPV.0000000000000456
43. Gjeraa K, Spanager L, Konge L, Petersen RH, Stergaard D. Non-technical skills in minimally invasive surgery teams: a systematic review. Surg Endosc. 2016;30(12):5185–5199. doi:10.1007/s00464-016-4890-1
44. Oomens P, Fu VX, Kleinrensink GJ, Jeekel J. The effect of music on simulated surgical performance: a systematic review. Surg Endosc. 2019;33(9):2774–2784. doi:10.1007/s00464-019-06868-x
45. Gillespie BM, Gillespie J, Boorman RJ, Granqvist K, Stranne J, Erichsen-Andersson A. The impact of robotic-assisted surgery on team performance: a systematic mixed studies review. Hum Factors. 2021;63(8):1352–1379. doi:10.1177/0018720820928624
46. Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health. 2014;35:29–45. doi:10.1146/annurev-publhealth-032013-182440
47. Giannakakis G, Grigoriadis D, Giannakaki K, Simantiraki O, Roniotis A, Tsiknakis M. Review on psychological stress detection using biosignals. IEEE Transactions Affective Computing. 2019;13(1):440–460. doi:10.1109/TAFFC.2019.2927337
48. Georgiou K, Larentzakis A, Papavassiliou AG. Surgeons’ and surgical trainees’ acute stress in real operations or simulation: a systematic review. Surgeon. 2017;15(6):355–365. doi:10.1016/j.surge.2017.06.003
49. Salas E, Driskell JE, Hughes S. The study of stress and human performance. In: Stress and Human Performance(A 97-27090 06-53). Vol. 1996. Mahwah, NJ: Lawrence Erlbaum Associates, Publishers; 1996:1–45.
50. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34. doi:10.1016/j.jclinepi.2009.06.006
51. Mateen FJ, Oh J, Tergas AI, Bhayani NH, Kamdar BB. s versus titles and abstracts for initial screening of articles for systematic reviews. Clin Epidemiol. 2013;5:89. doi:10.2147/CLEP.S43118
52. Stein-Wexler R, Sanchez T, Roper GE, et al. An interactive teaching device simulating intussusception reduction. Pediatr Radiol. 2010;40(11):1810–1815. doi:10.1007/s00247-010-1764-x
53. Lo K, Marcoux V, Grossman S, Kung R, Lee P. Cost comparison of the laparoscopic Burch colposuspension, laparoscopic two-team sling procedure, and the transobturator tape procedure for the treatment of stress urinary incontinence. J Obstetrics Gynaecol Canada. 2013;35(3):252–257. doi:10.1016/S1701-2163(15)30997-X
54. Aholaakko T-K. Reducing surgical nurses’ aseptic practice-related stress. J Clin Nurs. 2011;20(23–24):3339–3350. doi:10.1111/j.1365-2702.2011.03844.x
55. Vowels A, Topp R, Berger J. Understanding stress in the operating room: a step toward improving the work environment. Ky Nurse. 2012;60(2):5–7.
56. Eslami J, Baghini FK, Moazamfard M, Moazamfard C. The effect of music on the stress severity among the staff of surgery rooms. Int J Pharm Res. 2019;11(2):838–843.
57. Harvey A, Bandiera G, Nathens AB, LeBlanc VR. Impact of stress on resident performance in simulated trauma scenarios. J Trauma Acute Care Surgery. 2012;72(2):497–503. doi:10.1097/TA.0b013e31821f84be
58. Léonore B, Franoise D, Bruno D. Relationship between workload and styles of cooperation developed during medical emergency care. Eur Conf Cognitive Ergonomics. 2014:643.
59. Stevens BS, Royal KD, Ferris K, Taylor A, Snyder AM. Effect of a mindfulness exercise on stress in veterinary students performing surgery. Veterinary Surgery. 2019;48(3):360–366. doi:10.1111/vsu.13169
60. Alam M, Roongpisuthipong W, Kim NA, et al. Utility of recorded guided imagery and relaxing music in reducing patient pain and anxiety, and surgeon anxiety, during cutaneous surgical procedures: a single-blinded randomized controlled trial. J Am Acad Dermatol. 2016;75(3):585–589. doi:10.1016/j.jaad.2016.02.1143
61. Steinhilber B, Seibt R, Reiff F, Rieger MA, Kraemer B, Rothmund R. Effect of a laparoscopic instrument with rotatable handle piece on biomechanical stress during laparoscopic procedures. Surg Endosc. 2016;30(1):78–88. doi:10.1007/s00464-015-4164-3
62. Klein MI, DeLucia PR, Olmstead R. The impact of visual scanning in the laparoscopic environment after engaging in strain coping. Hum Factors. 2013;55(3):509–519. doi:10.1177/0018720812467458
63. Lucas PJ, Baird J, Arai L, Law C, Roberts HM. Worked examples of alternative methods for the synthesis of qualitative and quantitative research in systematic reviews. BMC Med Res Methodol. 2007;7(1):1–7. doi:10.1186/1471-2288-7-4
64. Thomas J, Harden A, Oakley A, et al. Integrating qualitative research with trials in systematic reviews. BMJ. 2004;328(7446):1010–1012. doi:10.1136/bmj.328.7446.1010
65. Zheng B, Fung E, Fu B, Panton NM, Swanström LL. Surgical team composition differs between laparoscopic and open procedures. Surg Endosc. 2015;29:2260–2265. doi:10.1007/s00464-014-3938-3
66. Kelley WE. The evolution of laparoscopy and the revolution in surgery in the decade of the 1990s. JSLS. 2008;12(4):351.
67. Sheetz KH, Claflin J, Dimick JB. Trends in the adoption of robotic surgery for common surgical procedures. JAMA network open. 2020;3(1):e1918911–e1918911. doi:10.1001/jamanetworkopen.2019.18911
68. Nisky I, Huang F, Milstein A, Pugh CM, Mussa-Ivaldi FA, Karniel A. Perception of stiffness in laparoscopy-The fulcrum effect. Stud Health Technol Inform. 2012;173:313.
69. Palep JH. Robotic assisted minimally invasive surgery. J Minim Access Surg. 2009;5(1):1. doi:10.4103/0972-9941.51313
70. Vitiello V, Lee S-L, Cundy TP, Yang G-Z. Emerging robotic platforms for minimally invasive surgery. IEEE Rev Biomed Eng. 2012;6:111–126. doi:10.1109/RBME.2012.2236311
71. Berguer R, Smith WD, Chung YH. Performing laparoscopic surgery is significantly more stressful for the surgeon than open surgery. Surg Endosc. 2001;15(10):1204–1207. doi:10.1007/s004640080030
72. Camarillo DB, Krummel TM, Salisbury JK. Robotic technology in surgery: past, present, and future. Am J Surgery. 2004;188(4):2–15. doi:10.1016/j.amjsurg.2004.08.025
73. Chrouser KL, Partin MR. Intraoperative disruptive behavior: the medical student’s perspective. J Surg Educ. 2019;76(5):1231–1240. doi:10.1016/j.jsurg.2019.04.002
74. Jung JJ, Elfassy J, Grantcharov T. Factors associated with surgeon’s perception of distraction in the operating room. Surg Endosc. 2020;34(7):3169–3175. doi:10.1007/s00464-019-07088-z
75. Sami A, Waseem H, Nourah A, et al. Real-time observations of stressful events in the operating room. Saudi J Anaesth. 2012;6(2):136. doi:10.4103/1658-354X.97026
76. Weigl M, Antoniadis S, Chiapponi C, Bruns C, Sevdalis N. The impact of intra-operative interruptions on surgeons’ perceived workload: an observational study in elective general and orthopedic surgery. Surg Endosc. 2015;29(1):145–153. doi:10.1007/s00464-014-3668-6
77. Wheelock A, Suliman A, Wharton R, et al. The impact of operating room distractions on stress, workload, and teamwork. Ann Surg. 2015;261(6):1079–1084. doi:10.1097/SLA.0000000000001051
78. Healey AN, Sevdalis N, Vincent CA. Measuring intra-operative interference from distraction and interruption observed in the operating theatre. Ergonomics. 2006;49(5–6):589–604. doi:10.1080/00140130600568899
79. Chandra T, Khan P, Khan L. Study to Evaluate Stress Among Ophthalmic Surgeons with Different Levels of Surgical Experience. Clinical Ophthalmology. 2020;14:3535. doi:10.2147/OPTH.S266501
80. Galati R, Simone M, Barile G, De Luca R, Cartanese C, Grassi G. Experimental setup employed in the operating room based on virtual and mixed reality: analysis of pros and cons in open abdomen surgery. J Healthc Eng. 2020;2020:1–11. doi:10.1155/2020/8851964
81. Jackson RS, Sanders T, Park A, et al. Prospective study comparing surgeons’ pain and fatigue associated with nipple-sparing versus skin-sparing mastectomy. Ann Surg Oncol. 2017;24(10):3024–3031. doi:10.1245/s10434-017-5929-9
82. Kuhn EW, Choi Y-H, Schnherr M, et al. Intraoperative stress in cardiac surgery: attendings versus residents. J Surgical Res. 2013;182(2):e43–e49. doi:10.1016/j.jss.2012.11.011
83. Luz M, Manzey D, Modemann S, Strauss G. Less is sometimes more: a comparison of distance-control and navigated-control concepts of image-guided navigation support for surgeons. Ergonomics. 2015;58(3):383–393. doi:10.1080/00140139.2014.970588
84. Manzey D, Luz M, Mueller S, Dietz A, Meixensberger J, Strauss G. Automation in surgery: the impact of navigated-control assistance on performance, workload, situation awareness, and acquisition of surgical skills. Human Factors: The Journal of the Human Factors and Ergonomics Society. 2011;53(6):584–599. doi:10.1177/0018720811426141
85. Marçon B, Sime WN, Guillemin F, et al. An ergonomic assessment of four different donor nephrectomy approaches for the surgeons and their assistants. Res Rep Urol. 2019;11:261. doi:10.2147/RRU.S220219
86. Naresh-Babu J, Arun-Kumar V, Raju DGS. Surgeon’s Neck Posture during Spine Surgeries:“The Unrecognised Potential Occupational Hazard”. Indian J Orthop. 2019;53(6):758–762. doi:10.4103/ortho.IJOrtho_677_18
87. Pimentel G, Rodrigues S, Silva PA, Vilarinho A, Vaz R, Cunha JPS. A wearable approach for intraoperative physiological stress monitoring of multiple cooperative surgeons. Int J Med Inform. 2019;129:60–68. doi:10.1016/j.ijmedinf.2019.05.028
88. Prichard RS, O’Neill CJ, Oucharek JJ, Colinda YH, Delbridge LW, Sywak MS. A prospective study of heart rate variability in endocrine surgery: surgical training increases consultant’s mental strain. J Surg Educ. 2012;69(4):453–458. doi:10.1016/j.jsurg.2012.04.002
89. Roy S, Hammond J, Panish J, Shnoda P, Savidge S, Wilson M. Time savings and surgery task load reduction in open intraperitoneal onlay mesh fixation procedure. Sci World J. 2015;2015:1–8. doi:10.1155/2015/340246
90. Ryland KA, Nelson CA, Hejkal TW. An infant surgical table for laser photocoagulation: ergonomic improvement analysis. J Med Eng Technol. 2010;34(2):124–133. doi:10.3109/03091900903402097
91. Wang R, Liang Z, Zihni AM, Ray S, Awad MM. Which causes more ergonomic stress: laparoscopic or open surgery? Surg Endosc. 2017;31(8):3286–3290. doi:10.1007/s00464-016-5360-5
92. Weigl M, Stefan P, Abhari K, et al. Intra-operative disruptions, surgeon’s mental workload, and technical performance in a full-scale simulated procedure. Surg Endosc. 2016;30(2):559–566. doi:10.1007/s00464-015-4239-1
93. Zhu X, Yurteri-Kaplan LA, Gutman RE, et al. Postural stress experienced by vaginal surgeons. Proceedings of the Human Factors and Ergonomics Society Annual Meeting. 2014;58(1):763–767. doi:10.1177/1541931214581139
94. Alleblas CCJ, Vleugels MPH, Nieboer TE. Ergonomics of laparoscopic graspers and the importance of haptic feedback: the surgeons’ perspective. Gynecol Surg. 2016;13(4):379–384. doi:10.1007/s10397-016-0959-z
95. Andersen LPH, Klein M, Ggenur I, Rosenberg J. Psychological and physical stress among experienced and inexperienced surgeons during laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2012;22(1):73–78. doi:10.1097/SLE.0b013e3182420acf
96. Apollos JR, Lawrence M, Guest RV. A Dual-Valve System to Minimize Loss of Pneumoperitoneum in Laparoscopic Surgery. JSLS. 2015;19(2):
97. Berg RJ, Inaba K, Sullivan M, et al. The impact of heat stress on operative performance and cognitive function during simulated laparoscopic operative tasks. Surgery. 2015;157(1):87–95. doi:10.1016/j.surg.2014.06.012
98. Engelmann C, Schneider M, Kirschbaum C, et al. Effects of intraoperative breaks on mental and somatic operator fatigue: a randomized clinical trial. Surg Endosc. 2011;25(4):1245–1250. doi:10.1007/s00464-010-1350-1
99. de’Angelis N, Alghamdi S, Renda A, Azoulay D, Brunetti F. Initial experience of robotic versus laparoscopic colectomy for transverse colon cancer: a matched case-control study. World J Surg Oncol. 2015;13(1):1–8. doi:10.1186/s12957-015-0708-1
100. Feng X, Morandi A, Boehne M, et al. 3-Dimensional (3D) laparoscopy improves operating time in small spaces without impact on hemodynamics and psychomental stress parameters of the surgeon. Surg Endosc. 2015;29(5):1231–1239. doi:10.1007/s00464-015-4083-3
101. Gao J, Liu S, Feng Q, et al. Quantitative evaluations of the effects of noise on mental workloads based on pupil dilation during laparoscopic surgery. Am Surg. 2018;84(12):1951–1956. doi:10.1177/000313481808401243
102. Gunawardena N, Matscheko M, Anzengruber B, et al. Assessing surgeons’ skill level in laparoscopic cholecystectomy using eye metrics.
103. Hurley AM, Kennedy PJ, O’Connor L, et al. SOS save our surgeons: stress levels reduced by robotic surgery. Gynecol Surg. 2015;12(3):197–206. doi:10.1007/s10397-015-0891-7
104. Khan WF, Krishna A, Roy A, et al. Effect of structured training in improving the ergonomic stress in laparoscopic surgery among general surgery residents. Surg Endosc. 2020;3:1–9.
105. Kim FJ, Sehrt DE, Molina WR, Huh J-S, Rassweiler J, Turner C. Initial experience of a novel ergonomic surgical chair for laparoscopic pelvic surgery. Int braz j Urol. 2011;37:455–460. doi:10.1590/S1677-55382011000400003
106. Klein M, Andersen LPH, Alamili M, Ggenur I, Rosenberg J. Psychological and physical stress in surgeons operating in a standard or modern operating room. Surg Laparosc Endosc Percutan Tech. 2010;20(4):237–242. doi:10.1097/SLE.0b013e3181ed851d
107. Klein MI, Warm JS, Riley MA, et al. Mental workload and stress perceived by novice operators in the laparoscopic and robotic minimally invasive surgical interfaces. J Endourol. 2012;26(8):1089–1094. doi:10.1089/end.2011.0641
108. Klein MI, Mouraviev V, Craig C, et al. Mental stress experienced by first-year residents and expert surgeons with robotic and laparoscopic surgery interfaces. J Robot Surg. 2014;8(2):149–155. doi:10.1007/s11701-013-0446-8
109. Leitsmann C, Uhlig A, Popeneciu IV, et al. The Silent Operation Theatre Optimisation System (SOTOS \copyright) to reduce noise pollution during da Vinci robot-assisted laparoscopic radical prostatectomy. J Robot Surg. 2020;1–9.
110. Liang Z, Gerull WD, Wang R, Zihni A, Ray S, Awad M. Effect of patient body mass index on laparoscopic surgical ergonomics. Obes Surg. 2019;29(6):1709–1713. doi:10.1007/s11695-019-03748-0
111. Lowndes BR, Bingener-Casey J, Hallbeck MS. A preliminary study of surgeon stress measures during randomized controlled trials of 4-port vs. single incision cholecystectomies. Proceedings of the Human Factors and Ergonomics Society Annual Meeting. 2014;58(1):1280–1284. doi:10.1177/1541931214581267
112. Mietzsch S, Bergholz R, Boettcher J, et al. Classical but not rap music significantly improves transferability and long-term acquisition of laparoscopic suturing skills: a randomized controlled trial. Eur J Pediatric Surg. 2020;30(06):541–547. doi:10.1055/s-0039-3401798
113. Moore LJ, Wilson MR, Waine E, McGrath JS, Masters RSW, Vine SJ. Robotically assisted laparoscopy benefits surgical performance under stress. J Robot Surg. 2015;9(4):277–284. doi:10.1007/s11701-015-0527-y
114. Nishimoto W, Kawahira H, Shimomura Y, Nishizawa Y, Ito M. A standing posture support device that reduces laparoscopic surgeons’ occupational lower limb stress. Minimally Invasive Therapy Allied Tech. 2019;28(3):151–156. doi:10.1080/13645706.2018.1491407
115. Niu S, Jin K, Hu Z, Zhang C, Zhao D, Xing Y. Ergonomic evaluation between laparoscopic and robotic surgery based on EMG.
116. Poolton JM, Wilson MR, Malhotra N, Ngo K, Masters RSW. A comparison of evaluation, time pressure, and multitasking as stressors of psychomotor operative performance. Surgery. 2011;149(6):776–782. doi:10.1016/j.surg.2010.12.005
117. Sharma S, Grantcharov T, Jung JJ. Non-technical skills and device-related interruptions in minimally invasive surgery. Surg Endosc. 2020;2:1–7.
118. Singh H, Modi HN, Ranjan S, et al. Robotic surgery improves technical performance and enhances prefrontal activation during high temporal demand. Ann Biomed Eng. 2018;46(10):1621–1636. doi:10.1007/s10439-018-2049-z
119. Sreekanth MP, Ranganathan R, Pugalendhi A. Individual customization strategy accomplished by developing prototype of a laparoscopic forceps handle using additive manufacturing. Rapid Prototyping J. 2020:e64.
120. Stavroulis A, Cutner A, Liao L-M. Staff perceptions of the effects of an integrated laparoscopic theatre environment on teamwork. Gynecol Surg. 2013;10(3):177–180. doi:10.1007/s10397-013-0802-8
121. Steinhilber B, Hoffmann S, Karlovic K, et al. Development of an arm support system to improve ergonomics in laparoscopic surgery: study design and provisional results. Surg Endosc. 2015;29(9):2851–2858. doi:10.1007/s00464-014-3984-x
122. Takayasu K, Yoshida K, Mishima T, Watanabe M, Matsuda T, Kinoshita H. Upper body position analysis of different experience level surgeons during laparoscopic suturing maneuvers using optical motion capture. Am J Surgery. 2019;217(1):12–16. doi:10.1016/j.amjsurg.2018.06.026
123. Tung KD, Shorti RM, Downey EC, Bloswick DS, Merryweather AS. The effect of ergonomic laparoscopic tool handle design on performance and efficiency. Surg Endosc. 2015;29(9):2500–2505. doi:10.1007/s00464-014-4005-9
124. Zhang X, Xue L, Li S, Kim FJ. Digital human modeling for ergonomic evaluation of patient table height. Int J Med. 2013:56.
125. Zihni AM, Ohu I, Cavallo JA, Cho S, Awad MM. Ergonomic analysis of robot-assisted and traditional laparoscopic procedures. Surg Endosc. 2014;28(12):3379–3384. doi:10.1007/s00464-014-3604-9
126. Zihni AM, Cavallo JA, Ray S, Ohu I, Cho S, Awad MM. Ergonomic analysis of primary and assistant surgical roles. J Surgical Res. 2016;203(2):301–305. doi:10.1016/j.jss.2016.03.058
127. Duysburgh P, Elprama SA, Jacobs A. Exploring the social-technological gap in telesurgery: collaboration within distributed or teams.
128. Krüger M, Ackermann J, Osmonov D, et al. Impact of Acoustic and Interactive Disruptive Factors during Robot-Assisted Surgery—A Virtual Surgical Training Model. Sensors. 2020;20(20):5891. doi:10.3390/s20205891
129. Anton NE, Montero PN, Howley LD, Brown C, Stefanidis D. What stress coping strategies are surgeons relying upon during surgery? Am J Surgery. 2015;210(5):846–851. doi:10.1016/j.amjsurg.2015.04.002
130. Antoniadis S, Passauer-Baierl S, Baschnegger H, Weigl M. Identification and interference of intraoperative distractions and interruptions in operating rooms. J Surgical Res. 2014;188(1):21–29. doi:10.1016/j.jss.2013.12.002
131. Aouicha W, Tlili MA, Limam M, et al. Evaluation of the Impact of Intraoperative Distractions on Teamwork, Stress, and Workload. J Surgical Res. 2021;259:465–472. doi:10.1016/j.jss.2020.09.006
132. Arabacı A. The Effect of Noise Levels in the Operating Room on the Stress Levels and Workload of the Operating Room Team. J PeriAnesthesia Nursing. 2021;36(1):54–58. doi:10.1016/j.jopan.2020.06.024
133. Holmes T, Vifladt A, Ballangrud R. A qualitative study of how inter-professional teamwork influences perioperative nursing. Nursing Open. 2020;7(2):571–580. doi:10.1002/nop2.422
134. Hull L, Arora S, Kassab E, Kneebone R, Sevdalis N. Assessment of stress and teamwork in the operating room: an exploratory study. Am J Surgery. 2011;201(1):24–30. doi:10.1016/j.amjsurg.2010.07.039
135. Keller S, Yule S, Smink DS, Zagarese V, Safford S, Parker SH. Episodes of strain experienced in the operating room: impact of the type of surgery, the profession and the phase of the operation. BMC Surg. 2020;20(1):1–11. doi:10.1186/s12893-020-00937-y
136. Lee JY, Lantz AG, McDougall EM, et al. Evaluation of potential distractors in the urology operating room. J Endourol. 2013;27(9):1161–1165. doi:10.1089/end.2012.0704
137. Lies SR, Zhang AY. Prospective randomized study of the effect of music on the efficiency of surgical closures. Aesthetic Surg j. 2015;35(7):858–863. doi:10.1093/asj/sju161
138. Marrelli M, Gentile S, Palmieri F, Paduano F, Tatullo M. Correlation between Surgeon’s experience, surgery complexity and the alteration of stress related physiological parameters. PLoS One. 2014;9(11):e112444. doi:10.1371/journal.pone.0112444
139. Mitchell L, Flin R, Yule S, Mitchell J, Coutts K, Youngson G. Thinking ahead of the surgeon. An interview study to identify scrub nurses’ non-technical skills. Int J Nurs Stud. 2011;48(7):818–828. doi:10.1016/j.ijnurstu.2010.11.005
140. Muhammad S, Lehecka M, Huhtakangas J, Jahromi BR, Niemel E. Meditation music improved the quality of suturing in an experimental bypass procedure. Acta neurochirurgica. 2019;161(8):1515–1521. doi:10.1007/s00701-019-03976-4
141. Padmakumar AD, Cohen O, Churton A, Groves JB, Mitchell DA, Brennan PA. Effect of noise on tasks in operating theatres: a survey of the perceptions of healthcare staff. Br j Oral Maxillofacial Surgery. 2017;55(2):164–167. doi:10.1016/j.bjoms.2016.10.011
142. Park AE, Zahiri HR, Hallbeck MS, et al. Intraoperative “micro breaks” with targeted stretching enhance surgeon physical function and mental focus. Ann Surg. 2017;265(2):340–346. doi:10.1097/SLA.0000000000001665
143. Tseng L-P, Liu Y-C. Effects of noises and music on nurses’ mental workload and situation awareness in the operating room.
144. Yamasaki A, Mise Y, Mise Y, et al. Musical preference correlates closely to professional roles and specialties in operating room: a multicenter cross-sectional cohort study with 672 participants. Surgery. 2016;159(5):1260–1268. doi:10.1016/j.surg.2015.10.031
145. Lowndes BR, Abdelrahman AM, Thiels CA, et al. Surgical team workload comparison for 4-port and single-port laparoscopic cholecystectomy procedures. Appl Ergon. 2019;78:277–285. doi:10.1016/j.apergo.2018.06.005
146. Bakhsh A, Martin GFJ, Bicknell CD, Pettengell C, Riga C. An evaluation of the impact of high-fidelity endovascular simulation on surgeon stress and technical performance. J Surg Educ. 2019;76(3):864–871. doi:10.1016/j.jsurg.2018.10.015
147. James DRC, Orihuela-Espina F, Leff DR, et al. The ergonomics of natural orifice translumenal endoscopic surgery (NOTES) navigation in terms of performance, stress, and cognitive behavior. Surgery. 2011;149(4):525–533. doi:10.1016/j.surg.2010.11.019
148. Opie J, Jaiprakash A, Ploderer B, Crawford R, Brereton M, Roberts J. Understanding the challenges and needs of knee arthroscopy surgeons to inform the design of surgical robots.
149. Statham MM, Sukits AL, Redfern MS, Smith LJ, Sok JC, Rosen CA. Ergonomic analysis of microlaryngoscopy. Laryngoscope. 2010;120(2):297–305. doi:10.1002/lary.20686
150. Theodoraki MN, Ledderose GJ, Becker S, et al. Mental distress and effort to engage an image-guided navigation system in the surgical training of endoscopic sinus surgery: a prospective, randomised clinical trial. Eur Arch Oto-Rhino-Laryngology. 2015;272(4):905–913. doi:10.1007/s00405-014-3194-0
151. Yao J, Chang Z, Zhu L, Fan J. Uniportal versus multiportal thoracoscopic lobectomy: ergonomic evaluation and perioperative outcomes from a randomized and controlled trial. Medicine. 2020;99(42):e22719. doi:10.1097/MD.0000000000022719
152. Yoon S-H, Jung M-C, Park SY. Evaluation of surgeon’s muscle fatigue during thoracoscopic pulmonary lobectomy using interoperative surface electromyography. J Thorac Dis. 2016;8(6):1162. doi:10.21037/jtd.2016.04.16
153. Arora S, Sevdalis N, Aggarwal R, Sirimanna P, Darzi A, Kneebone R. Stress impairs psychomotor performance in novice laparoscopic surgeons. Surg Endosc. 2010;24(10):2588–2593. doi:10.1007/s00464-010-1013-2
154. Green B, Oeppen RS, Da S, Brennan PA. Challenging hierarchy in healthcare teams-ways to flatten gradients to improve teamwork and patient care. Br J Oral Maxillofacial Surgery. 2017;55(5):449–453. doi:10.1016/j.bjoms.2017.02.010
155. Conrad C, Konuk Y, Werner P, et al. The effect of defined auditory conditions versus mental loading on the laparoscopic motor skill performance of experts. Surg Endosc. 2010;24(6):1347–1352. doi:10.1007/s00464-009-0772-0
156. Wakeman D, Langham MR. Creating a safer operating room: groups, team dynamics and crew resource management principles. Seminars in Pediatric Surgery. 2018;27(2):107–113. doi:10.1053/j.sempedsurg.2018.02.008
157. Hollnagel E, Wears RL, Braithwaite J. From Safety-I to Safety-II: a white paper. The Resilient Health Care Net: Published Simultaneously by the University of Southern Denmark, University of Florida, USA, and Macquarie University, Australia. 2015:565.
158. Lyng HB, Macrae C, Guise V, et al. Balancing adaptation and innovation for resilience in healthcare-a metasynthesis of narratives. BMC Health Serv Res. 2021;21(1):1–13. doi:10.1186/s12913-021-06592-0
159. Berry JC, Davis JT, Bartman T, et al. Improved safety culture and teamwork climate are associated with decreases in patient harm and hospital mortality across a hospital system. J Patient Saf. 2020;16(2):130–136. doi:10.1097/PTS.0000000000000251
160. Göras C, Nilsson U, Ekstedt M, Unbeck M, Ehrenberg A. Managing complexity in the operating room: a group interview study. BMC Health Serv Res. 2020;20:1–12. doi:10.1186/s12913-020-05192-8
161. Tsai MH, Sanford JA, Black IH, et al. Operating room management at the edge of order and chaos. J Med Pract Manage. 2017;32:250–255.
162. Leach LS, Myrtle RC, Weaver FA. Surgical teams: role perspectives and role dynamics in the operating room. Health Services Manag Res. 2011;24(2):81–90. doi:10.1258/hsmr.2010.010018
163. Tsui C, Klein R, Garabrant M. Minimally invasive surgery: national trends in adoption and future directions for hospital strategy. Surg Endosc. 2013;27(7):2253–2257. doi:10.1007/s00464-013-2973-9
164. Schmutz JB, Meier LL, Manser T. How effective is teamwork really? The relationship between teamwork and performance in healthcare teams: a systematic review and meta-analysis. BMJ open. 2019;9(9):e028280. doi:10.1136/bmjopen-2018-028280
165. Greenwood BN, Agarwal R, Agarwal R, Gopal A. The role of individual and organizational expertise in the adoption of new practices. Organization Sci. 2019;30(1):191–213. doi:10.1287/orsc.2018.1246
166. Rydenfält C. Teamwork in the Operating Room-The Role of Organizational Design and Implications for Patient Safety. Vol. 50. Lund University; 2014.
167. Tomo A, De Simone S. Exploring factors that affect the well-being of healthcare workers. Int J Business Management. 2017;12(6):49–61. doi:10.5539/ijbm.v12n6p49
168. Flin R, Winter J, Sarac C, Raduma M. Human factors in patient safety: review of topics and tools. World Health. 2009;2(10):67.
169. Tawfik DS, Profit J, Webber S, Shanafelt TD. Organizational factors affecting physician well-being. Curr Treatment Options Pediatrics. 2019;5(1):11–25. doi:10.1007/s40746-019-00147-6
170. Keroack MA, Youngberg BJ, Cerese JL, Krsek C, Prellwitz LW, Trevelyan EW. Organizational factors associated with high performance in quality and safety in academic medical centers. Acad Med. 2007;82(12):1178–1186. doi:10.1097/ACM.0b013e318159e1ff
171. Cresswell KM, Blandford A, Sheikh A. Drawing on human factors engineering to evaluate the effectiveness of health information technology. J R Soc Med. 2017;110(8):309–315. doi:10.1177/0141076817712252
172. Carayon P, Hundt AS, Karsh BT, et al. Work system design for patient safety: the SEIPS model. BMJ Qual Saf. 2006;15(suppl 1):i50–i58. doi:10.1136/qshc.2005.015842
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.