Back to Journals » Infection and Drug Resistance » Volume 14
Unfavorable Treatment Outcome and Its Predictors Among Patients with Multidrug-Resistance Tuberculosis in Southern Ethiopia in 2014 to 2019: A Multi-Center Retrospective Follow-Up Study
Authors Bogale L , Tsegaye T , Abdulkadir M, Akalu TY
Received 7 January 2021
Accepted for publication 16 March 2021
Published 8 April 2021 Volume 2021:14 Pages 1343—1355
DOI https://doi.org/10.2147/IDR.S300814
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Lemlem Bogale,1 Tewodros Tsegaye,1 Mohamed Abdulkadir,1 Temesgen Yihunie Akalu2
1Department of Internal Medicine, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 2Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Temesgen Yihunie Akalu
Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Po Box 196, Gondar, Ethiopia
Tel +251 929390709
Email [email protected]
Background: According to the 2017 global report, Ethiopia is among the top 30 high tuberculosis (TB) and multidrug-resistant tuberculosis (MDR-TB) burden countries. However, studies on MDR-TB treatment outcomes in Southern Ethiopia was very limited. Therefore, the study was aimed at determining the unfavorable treatment outcome and its predictors among patients with multidrug-resistant tuberculosis in Southern Ethiopia MDR-TB treatment centers.
Subjects and Methods: A retrospective follow-up study was conducted in Southern Ethiopia MDR-TB treatment initiating centers. Three hundred sixty-three patients were included in the study. Kaplan–Meier failure curve, median time, and Log rank test were used to present the descriptive findings. Then, a Cox regression analysis was used to identify predictors of unfavorable treatment outcome. The strength of the association was reported using an adjusted hazard ratio (AHR) and a 95% confidence interval (CI). Finally, the Cox Snell residual test was used to check the goodness of fit.
Results: For the entire cohort, the unfavorable treatment outcome was 23.68% (19.29, 28.09). Hospitalization for care (AHR = 2.07; 95% CI = 1.21, 3.63), male sex (AHR = 1.85; 95% CI = 1.002, 3.42), attending tertiary education (AHR = 0.31; 95% CI = 0.11, 0.91), and those with low hemoglobin (AHR = 2.89; 95% CI = 1.55, 5.38) were predictors for unfavorable treatment outcome.
Conclusion: The unfavorable treatment outcome was higher compared with the national goal of END-TB by 2020. Hospitalizations for care, male sex, and low hemoglobin level increased the hazard of the unfavorable treatment outcome. On the other hand, attending territory education decreased the hazard of the unfavorable treatment outcome.
Keywords: multidrug-resistant tuberculosis, unfavorable treatment outcome, Southern Ethiopia
Background
Multidrug-resistant tuberculosis, defined as tuberculosis (TB) resistant to at least isoniazid and rifampicin, the two most powerful anti-TB drugs. It results from either primary infection or may develop in the course of a patient’s treatment.1 The treatment outcome of MDR-TB could be cured, completed, treatment failure, lost to follow-up (LTFU), died, and extensively drug-resistant tuberculosis (XDR-TB). Treatment failure, death, and LTFU were considered unfavorable treatment outcomes.2
According to the 2017 global report, 558,000 people developed active TB. Of these, 3.6% of new cases and 17% of previously treated cases developed MDR-TB. Nearly half of the global MDR/RR-TB cases were from the three countries: India (24%), China (13%), and the Russian Federation (10%).1 Ethiopia is one of the 30 high TB and MDR-TB burden countries. It has an annual incident of 5500 MDR/RR-TB cases in 2017. Of these, an estimated 2.7% and 14% of MDR/RR-TB cases were new and previously treated, respectively.3 In Ethiopia, the treatment success rate of MDR/RR-TB cases was 75% in 2015. However, the national TB strategic plan towards achieving the END-TB 90–90-90 targets set for 2020 is to reduce the unfavorable treatment outcome to <10%.1,4
The unfavorable treatment outcome would result in transmitting a drug-resistant form of TB to the community, which increases the burden of TB. Also, it increases the risk of acquiring additional resistance, cost of TB treatment, and loss of productivity.5 The presence of medical complications, drug side effects, human immunodeficiency virus (HIV) co-infection, underweight, presence of anemia, being a farmer, older age, treatment delay, male gender, abuse of alcohol, and smear positivity at diagnosis were significantly affect the unfavorable treatment outcome among MDR-TB patients.6–15 Non-governmental organizations and the Federal Ministry of Health did in collaboration to improve a good treatment outcome. However, the end TB 90–90-90 target is still not achieved. Hence, the current study was aimed at determining the unfavorable treatment outcome and its predictors in Southern Ethiopia.
Subjects and Methods
Study Design and Setting
A retrospective follow-up study design was conducted between September 2014 and September 2019. Multidrug-resistant TB treatment was started at Saint Peter TB Specialized Hospital by the end of 2009. Then the service was expanded to selected regional referral hospitals. Eight public Hospitals are providing MDR-TB treatment in Southern nation: Arbaminch, Yirgalem, Hosanna, Butajira, Mizan Tepi, Jinka, Dilla, and Sawla Hospitals. About 427 MDR-TB patients were enrolled from the inauguration. Of all, more than 95% were enrolled in Yirgalem General Hospital, Wachamo University Queen Elleni Mohamed Memorial Referral Hospital, Butajira General Hospital, and Dilla University Specialized Referral Hospital.
Yirgalem General Hospital and Wachamo University Queen Elleni Mohamed Memorial Referral Hospital initiated treatment for MDR-TB at the end of 2013. Then Butajira General Hospital and Dilla University Specialized Referral Hospital initiated MDR-TB treatment in 2017 and 2018, respectively.
Population and Sample
All MDR-TB patients who initiated treatment at the four treatment initiating centers (TICs) found in Southern Ethiopia were the source population. All MDR-TB patients who were found in the four TICs and enrolled between September 2014 and September 2019 were the study population. All MDR-TB patients enrolled in the Southern nation and nationality peoples’ region (SNNPR) between September 2014 and September 2019 were included in the study. Patients with an incomplete date of entry, exit, and treatment outcome were excluded. The sample size was estimated using Stata 14.1. The following assumptions; 80% Power, 5% significant level, effect size (Hazzard ratio), and 10% lost to follow-up were used (Table 1).
 |
Table 1 Estimated Sample Size for Treatment Outcomes and Its Predictors at TIC in Southern Ethiopia, 2014 to 2019 |
Variables of the Study
The dependent variable, unfavorable treatment outcome, was defined as a patient who is died, lost to follow-up, and/or treatment failure during the treatment course. Time to unfavorable treatment outcome: measured in months from the start of MDR-TB treatment to the occurrence of the unfavorable treatment outcome. Independent variables including socio-demographic characteristics: TIC, baseline age, sex, residence, occupation, marital status, and educational status, behavioral characteristics: baseline alcohol drinking, smoking, and chat chewing history, clinical characteristics: duration of illness before diagnosis, treatment delay, body mass index (BMI), previous TB treatment, diagnosis methods, site of MDR-TB, HIV status, other comorbidities, baseline sputum smear/culture grade, presence of CXR finding, baseline hemoglobin, creatinine, alanine transaminase (ALT), aspartate transaminase (AST), serum potassium (K), thyroid-stimulating hormone (TSH), treatment regimen, adverse drug reaction, types of drug resistance, treatment support, and adherence.
Good adherence: was defined as a patient taking the drug according to instructions given by the providers and an estimated adherence level of ≥ 85%. A major adverse drug event: was defined as when a patient developed at least one (nephrotoxicity, hepatotoxicity, hypokalemia, hypothyroidism, and hematologic abnormalities). Hepatotoxicity: was defined as an elevation of serum transaminases >3 times the normal upper limit with symptoms or elevation of serum bilirubin >2 times the normal upper limit with symptoms or elevation of serum transaminases or serum bilirubin >5 times of the normal upper limit with or without symptoms. Anemia: was defined as when hemoglobin level was <11g/dl. Hypokalemia: was defined as when a patient had at least one serum potassium value < 3.5 mmol/l. Hypothyroidism: was defined as when a patient had at least one measure of serum thyroid-stimulating hormone greater than 5.0 mIU/L. Nephrotoxicity: was defined as when a patient had an elevation of at least one serum creatinine value greater than 133 mmol/l. Censored: was defined as when a patient does not develop an event (cured, completed, and transfer out). Cured: was defined as when a patient completed treatment according to the national recommendation without evidence of failure and three or more consecutive cultures taken at least 30 days apart are negative after the intensive phase. Death: was defined when a patient dies for any reason during TB treatment. Duration of illness before diagnosis: was defined from the date of a patient having symptoms (duration of complaint in association with TB) plus a duration of a patient diagnosed with MDR after seeking medical care (the days between the date of seeking care and MDR-TB confirmation). Lost to follow up: was defined when a patient started anti-TB treatment and interrupted for 2 or more consecutive months. Previous TB treatment: was defined as a patient who was treated for TB at least for one month. Sputum smear grade: Negative (no AFB/100 high-power fields [HPF]), scanty (1–9 AFB/100 HPF), 1+ (10–99 AFB/100 HPF), 2+ (1–9 AFB/HPF), and 3+ (>9 AFB/HPF). Treatment completed: Treatment completed according to national recommendation without evidence of failure but no record that three or more consecutive cultures taken at least 30 days apart are negative after the intensive phase. Treatment delay: was defined as the median time from the duration in days between the date of MDR-TB confirmation and the date of treatment initiation. Treatment failure: Treatment terminated or need for permanent regimen change of at least two anti-TB drugs because of lack of conversion by the end of the intensive phase, or bacteriological reversion in the continuation phase after conversion to negative after intensive phase, or evidence of additional acquired resistance to fluoroquinolones or second-line injectable drugs, or adverse drug reactions.
Sputum culture grade: No growth (none), record actual number (1–9 colonies), 1+ (10–100 colonies), 2+ (>100–200 colonies), 3+ (>200 colonies), positive for other mycobacteria (other mycobacterial growth), contaminated (contaminated), and positive for MTB and contamination. Successful treatment outcome: was defined when a patient became cured or completed the treatment.
Data Collection Tools and Procedures
Data was collected using a structured checklist from patient medical charts and registration books. One supervisor (senior BSc nurse) and two data collectors (BSc nurses) were enrolled for each selected TIC in the data collection process. Patient information including socio-demographic characteristics such as age, sex, residence, education, and occupation; behavioral characteristics such as baseline smoking, alcohol drinking and chat chewing history; clinical variables such as duration of illness before diagnosis, treatment delay, BMI, treatment outcomes, duration of therapy, previous TB treatment history, way of diagnosis, site of MDR, smear and culture results, HIV status, other comorbidities, CXR finding, adverse drug event, drug regimen, types of DR, and laboratory investigations; as well as adherence, treatment support and mode of care were obtained from MDR-TB medical records and the registration book. Body mass index is measured by using patient weight (kg) and height (M), then dividing weight by height square. Hemoglobin is measured as total hemoglobin and the result is expressed in grams (gm) per deciliter (dl) of whole blood, a deciliter being 100 milliliters.
Data Quality Control
Appropriate training and supervision of data collectors were given to ensure the data quality. A two days training on how to extract data from patient medical charts and registration books was given to data collectors and supervisors. The principal investigator made the overall supervision. The pre-test was done on 5% of the sample in Yirgalem General Hospital and Wachamo University Queen Elleni Mohamed Memorial Referral Hospital.
Data Processing and Analysis
Data was entered into Epi-data version 3.1 and exported to Stata 14 for analysis. Data cleaning, coding, and recoding were made. Descriptive findings were summarized using counts and percentages. The presence of influential outliers, multicollinearity, and the proportional hazard assumption were checked. The median time with Interquartile range (IQR) was used to present the continuous variables. Life table was constructed to estimate the probability of unfavorable treatment outcome at different time intervals. Kaplan–Meier’s failure curve was used to compare the different groups. Besides, a Log rank test was used to test the presence of differences in the incidence of unfavorable treatment outcome among the groups. A bivariate Cox regression model was used at p-value <0.2 and variables significant in the bivariate analysis were entered in the final multivariable Cox regression model.
The Cox proportional hazard assumption was assessed graphically using log-log survival curves and Schoenfeld residual statistical tests. The goodness of fit of the final model was checked by Nelson Aalen’s cumulative hazard function against the Cox-Snell residual. The finding was presented using the adjusted hazard ratio (AHR) and the 95% confidence interval (CI).
Results
Socio-Demographic Characteristics of MDR-TB Patients
A total of 381 patients were registered from September 2014 to September 2019. Among these, 18 (4.72%) were excluded from the study due to incomplete records on the date of treatment outcome and unknown outcome status. Thus, a total of 363 (95.28%) participants were included in the study. Of all, 220 (60.61%) participants were male. About one-third (36.91%) participants were from the Sidama region. About a quarter (24.53%) participants were students (Table 2).
 |
Table 2 Sociodemographic Characteristics of Patients with Multidrug-Resistance Tuberculosis in Southern Ethiopia, from 2014 to 2019 |
Behavioral Characteristics of MDR-TB Patients
Three-hundred-fifty-three (97.25%) patients had no baseline smoking history. Nearly 13% patients had a history of alcohol drinking (Table 3).
 |
Table 3 Behavioral Characteristics of Patients with Multidrug-Resistant in Southern Ethiopia, from 2014 to 2019 |
Clinical Characteristics of MDR-TB Patients
The median duration of illness among MDR-TB patients before the diagnosis was 91 (51–161) days. Almost all, 98.35% of MDR-TB patients had pulmonary tuberculosis. Baseline sputum culture and smear were positive for 69.97% and 71.35% patients, respectively. The majority, 93.9% of patients were diagnosed by gene-expert. Most of the patients, 80.44% were put on a long-term drug regimen. About a quarter, 27 (7.44%) of MDR-TB patients were reactive for HIV. Nineteen (5.33%) of MDR-TB patients had other co-morbidities. About 15.43% of MDR-TB patients had developed adverse drug events. Of these, had a hematologic disorder (41.07%), nephrotoxicity (26.78%), hypokalemia (23.21%), hepatotoxicity (7.14%), and hypokalemia (1.78%) (Table 4).
 |  |  |
Table 4 Clinical Characteristics of Patients with Multidrug-Resistance Tuberculosis in Southern Ethiopia, from 2014 to 2019 |
Treatment Outcome of MDR-TB Patients
The overall median time was 19.23 (IQR: 9.53 to 20.73) months with a total of 5511.39 person-months observation. Two-hundred-fifty-one (69.15%) of MDR-TB patients had favorable treatment outcome. The remaining 23.68% (19.29%, 28.09%) of MDR-TB patients had unfavorable treatment outcome (Figure 1).
 |
Figure 1 Treatment outcome of patients with multidrug-resistant tuberculosis in Southern Ethiopia, from 2014 to 2019. |
Based on the treatment initiation centers about half (50.14%) of MDR-TB patients were from Yirgalem general hospital (Figure 2).
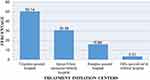 |
Figure 2 The percentage of multidrug-resistance tuberculosis patients in treatment initiation centers of Southern Ethiopia, from 2014 to 2019. |
Survival Status of MDR-TB Patients
The overall cumulative failure of the unfavorable treatment outcome was 8%, 19%, and 27% at the end of 6, 12, and 24 months, respectively (Figure 3).
 |
Figure 3 The plot of the overall estimate of the Kaplan–Meier failure function of MDR-TB patients in Southern Ethiopia, from 2014 to 2019. |
Hospitalized MDR-TB patients had a higher hazard of unfavorable treatment outcome compared with ambulatory care patients (Figure 4).
 |
Figure 4 The plot of Kaplan–Meier failure function of MDR-TB patients based on the model of care in Southern Ethiopia, from 2014 to 2019. |
Log Rank Test for the Equality of Survival Function
The Log rank test indicates that there is statistically a significant difference in survival experience among groups of smokers at baseline, alcohol drinkers at the baseline, the presence of co-morbidity, other adverse drug events, and model of care at a 5% level of significance (Table 5).
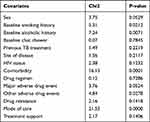 |
Table 5 Results of the Log Rank Test for the Categorical Variables of Patients with Multidrug-Resistance Tuberculosis in Southern Ethiopia, from 2014 to 2019 |
Model Diagnostics and Goodness of Fit of the Final Model
The Schoenfeld residual global test showed that the proportional hazard assumption was met (P-value = 0.098). The hazard function follows the 45 degree line very closely except for large values of the time. It is very common for models with censored data to have some wiggling at large values of the time and it is not something which should cause much concern. Overall, we could conclude that the final model fits the data very well (Figure 5).
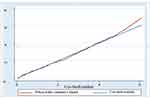 |
Figure 5 Cumulative hazard plot of the Cox-Snell residuals of the proportional hazard against the Nelson-Aalen cumulative hazard function. |
Factors Affecting Unfavorable Treatment Outcome Among MDR-TB Patients
Sex, educational status, baseline smoking history, baseline alcohol drinking history, treatment delay, HIV status, co-morbidity, baseline sputum culture, baseline hemoglobin, baseline creatinine, baseline ALT, baseline potassium, major adverse drug event, other adverse drug events, mode of care and treatment support were fitted in multivariable analysis for unfavorable treatment outcome. Being male, attending tertiary education, low hemoglobin, and hospitalization for MDR-TB were predictors of the unfavorable treatment outcome.
The hazard of developing unfavorable treatment outcome among male MDR-TB patients was 85% higher than female MDR-TB patients. Attending tertiary education decreased the hazard of unfavorable treatment outcome by 69% compared to patients’ attending primary education. The hazard of an unfavorable treatment outcome among MDR-TB patients with low baseline hemoglobin was 2.89 times that of normal baseline hemoglobin. The hazard of developing unfavorable treatment outcome among hospitalized patients was 2.07 times that of ambulatory patients (Table 6).
 |
Table 6 Bivariate and Multivariable Cox Proportional Hazards Regression Analysis of Time to Unfavorable Treatment Outcome in Southern Ethiopia, from 2014 to 2019 |
Discussion
The objective of this study was to assess unfavorable treatment outcome and its predictors among patients with multidrug-resistant tuberculosis. In this study, 86 (23.69%) of MDR-TB patients had unfavorable treatment outcome. This finding is in line with a study conducted from Shanghai, Pakistan, India, Tanzania, Gabon, and a systematic and meta-analysis study.1,16–21 Besides, it is in agreement with the studies done in different regions of Ethiopia including the Amhara region, Southern region, and Oromia region.8,10,22
Unfavorable treatment outcome is lower compared with studies done in Ukraine, Armenia, Uzbekistan, China, Western India, and Morocco.7,9,23–25 This could be in the current study there is an improvement of care on MDR-TB treatment. Moreover, the introduction of a short-term drug regimen will cause a lower unfavorable treatment outcome in the current study. Furthermore, the addition of Bedaqulline and linezolid which are powerful ant-MDR-TB drugs in the recent study could cause the lower incidence of unfavorable treatment outcome.
On the other hand, this finding was still higher compared with our national target of 2020 which showed only < 10% should have unfavorable treatment outcome.5 The increasing number of unfavorable treatment outcome could put the community in danger for the transmission of resistant forms of tuberculosis in addition to poverty. The median time to unfavorable treatment outcome was 7.6 months which was similar to the study done in the Oromia region.22
In the current study, hospitalization for care increases the hazards of unfavorable treatment outcome. This finding is in line with a study done in Uzbekistan that showed that more favorable treatment outcomes occurred for those on ambulatory care than on hospitalized care.26 This could be because hospitalized patients were more debilitated, have concomitant infections, and could develop adverse drug events from the MDR-TB treatment or other treatment. Hence, this finding suggested that it is better to provide better attention to hospitalized patients.
In this study being male increased the hazard of developing unfavorable treatment outcome. This finding was in agreement with a study done in India.19 This could be due to the working behavior of males that may compromise drug compliance and nutrition. As a result, it is highly recommended to give enhanced counseling and provide strict follow-up by health professionals for better treatment outcomes.
Those attending tertiary education decreased the hazard of unfavorable treatment outcome. This finding is similar to the finding in Western India.7 This could be due to the increased level of education that would cause better nutrition, information to initiate treatment early, and good adherence to treatment. Hence, it is valuable to educate the community to reduce unfavorable treatment outcome.
Low hemoglobin level was a predictor of unfavorable treatment outcome. This finding is comparable to the study done in Northwest Ethiopia.10 This could be due to poor nutrition, chronicity of illness, and other concomitant infections. Therefore, clinicians need to give better attention to patients with low hemoglobin levels to minimize the burden of unfavorable treatment outcome.
As per our knowledge, it is the first study that was conducted on predictors of unfavorable treatment outcome in Southern Ethiopia. Secondly, it incorporated new variables like duration of illness before diagnosis and drug regimen (short-term or long-term). However, the study has some limitations. Firstly; it was entirely secondary and data on important variables were missing. Secondly, patient-related factors, health system-related factors, and drug-related factors are needed to further analyze the determinants of unfavorable treatment outcome and to reach solid national decisions for a successful treatment outcomes.
This study will be helpful to policy-makers, planners, and decision-makers to provide timely evidence. Besides, the study will be valuable to clinicians in their day to day activities. Finally, the study will be important to researchers as a baseline information.
Conclusion
This study showed that the unfavorable treatment outcome was higher compared with the national goal of END-TB by 2020. Being male, higher education, low hemoglobin, and hospitalization were significant predictors with unfavorable treatment outcome. Hence, it is appropriate to give more attention to patients with low hemoglobin levels and hospitalized patients.
Abbreviation
ART, Antiretroviral Therapy; BMI, Body Mass Index; CD4, A cluster of Differentiation 4; CI, Confidence Interval; CP, Continuation Phase; CXR, Chest X-ray; DM, Diabetes Mellitus; DOT, Directly Observed Therapy; DR, Drug-Resistance; DST, Drug Susceptibility Test; GHC, Global Health Commute; HR, Hazard Ratio; HIV, Human Immunodeficiency Virus; IP, Intensive Phase; IQR, Interquartile Range; IRB, Institutional Review Board; KM, Kaplan–Meier; LTFU, Loss To Follow Up; MDR, Multidrug-Resistant; RR, Rifampicin Resistance; SCC, Sputum Culture Conversion; SHR, Sub Hazard Ratio; SLD, Second Line Drug; SNNPR, Southern Nation, Nationalities, and People’s Region; TIC, Treatment Initiation Centers; TB, Tuberculosis; TF, Treatment Failure; TSH, Thyroid Stimulating Hormone; USA, United States of America; WHO, World Health Organization; XDR, Extensively Drug-Resistance.
Data Sharing Statement
Data will be made available from the primary author upon a reasonable request.
Ethical Approval and Consent to Participate
Ethical clearance and permission were obtained from the University of Gondar institutional review board (IRB) with Reference number. SOM/1734/2019 and permission was secured from SNNPR health departments. Informed consent was not taken from the study participants directly as it is entirely secondary but permission was requested for each hospital for their patients. Besides, the information obtained from the patients was waived by the University of Gondar because of inability to collect information directly from the participants. The checklist was de-identified and kept securely in locked cabinets and the database was password protected to keep the confidentiality of the patients. The study was conducted in accordance with the Declaration of Helsinki.
Consent for Publication
Not applicable.
Acknowledgments
We would like to thank the Amhara region health bureau for its minimal financial support. We are also grateful to Hossana, Butajira, Dilla, and Yirgalem hospital staff members for their kind cooperation in the data collection process. Last but not least, we would like to thank data collectors and supervisors for their kind support and without them, the study cannot be materialized.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Amhara region health bureau provided minimal financial support. The funder had no role in the conception, design, analysis, interpretation, and decision on publication.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. World Health Organization; 2018. Global tuberculosis report 2018. World Health Organization. Available from: https://apps.who.int/iris/handle/10665/274453.
2. Alipanah N, Jarlsberg L, Miller C, et al. Adherence interventions and outcomes of tuberculosis treatment: a systematic review and meta-analysis of trials and observational studies. PLoS Med. 2018;15(7):e1002595. doi:10.1371/journal.pmed.1002595.
3. WHO. Treatment guidelines for drug-resistant tuberculosis; 2016.
4. WHO. The end TB strategy; 2014:1–25.
5. F D. National Programmatic management of Drug resistant TB in Ethiopia Participant’s manual; 2017.
6. JP KE C, Van Der Walt M, Brand J, et al. Multidrug-resistant tuberculosis treatment outcomes in relation to treatment and initial versus acquired second-line drug resistance. Clin Infect Dis. 2015;62(4):418–430. doi:10.1093/cid/civ910
7. Patel SVNK, Alpesh PB, Shukla LK, et al. Treatment outcome among cases of multidrug-resistant tuberculosis (MDR TB) in Western India: a prospective study. J Infect Public Health. 2016;9(4):478–484. doi:10.1016/j.jiph.2015.11.011
8. Girum T, Tariku Y, Dessu S. Survival Status and Treatment Outcome of Multidrug Resistant Tuberculosis (MDR-TB) among Patients Treated in Treatment Initiation Centers (TIC) in South Ethiopia: a Retrospective Cohort Study. Ann Med Health Sci Res. 2017;7(5):331–336.
9. O BM A, Krasiuk V, Rybak N, et al. Risk factors for poor multidrug-resistant tuberculosis treatment outcomes in Kyiv Oblast, Ukraine. BMC Infect Dis. 2017;17(1):1–7. doi:10.1186/s12879-016-2122-x
10. Alene KA, Viney K, McBryde ES. Clements ACA Treatment outcomes in patients with multidrug-resistant tuberculosis in north-west Ethiopia. Trop Med Int Health. 2017;22(3):351–362. doi:10.1111/tmi.12826
11. Ep H, Garcia-Prats AJ, Law S, et al. Treatment and outcomes in children with multidrug-resistant tuberculosis: a systematic review and individual patient data meta-analysis. PLoS Med. 2018;15(7):1–26.
12. Htun YM, Khaing TMM, Aung NM, et al. Delay in treatment initiation and treatment outcomes among adult patients with multidrug-resistant tuberculosis at Yangon Regional Tuberculosis Centre, Myanmar: a retrospective study. PLoS One. 2018;13:12. doi:10.1371/journal.pone.0209932
13. Samuels JPSA, Campbell JR, Ahmad Khan F, Johnston JC. Comorbidities and treatment outcomes in multidrug resistant tuberculosis: a systematic review and meta-analysis. Sci Rep. 2018;8(1):1–13.
14. Gualano G, Musso M, Mosti S, et al. Putting in harm to cure: drug related adverse events do not affect outcome of patients receiving treatment for multidrug-resistant Tuberculosis experience from a tertiary hospital in Italy. PLoS One. 2019;14(2):1–14.
15. Tefera KT, Reta MM, Sisay MM, Tamirat KS, Akalu TY. Treatment delay and associated factors among adults with drug resistant tuberculosis at treatment initiating centers in the Amhara regional state. Ethiop BMC Infect Dis. 2019;19(1):1–8.
16. Bélard S, Bootsma S, Janssen S, et al. Tuberculosis treatment outcome and drug resistance in lambaréné. Gabon Prospective Cohort Study. 2016;95(2):472–480.
17. Li DGE, Shen X, Wei X. Risk factors of treatment outcomes for multi-drug resistant tuberculosis in Shanghai, 2009–2012. Procedia Environ Sci. 2016;36:12–19. doi:10.1016/j.proenv.2016.09.003
18. Kibret KT, Memiah P, Biadgilign S. Treatment outcomes for multidrug-resistant tuberculosis under DOTS-Plus: a systematic review and meta-analysis of published studies. Infect Dis Poverty. 2017;6(1):1–8.
19. Nair D, Kannan T, Tripathy JP, Harries AD, Natrajan M, Swaminathan S. Predictors of unfavourable treatment outcome in patients with multidrug-resistant tuberculosis in India Public Health Action. Public Health Action. 2017;7:1.
20. Javaid A, Masud H, Basit A, et al. Predictors of poor treatment outcomes in multidrug-resistant tuberculosis patients: a retrospective cohort study. Clin Microbiol Infect. 2018;24(6):612–617. doi:10.1016/j.cmi.2017.09.012
21. Leveri TH, Mollel E, Lyamuya F, Kilonzo K. Predictors of treatment outcomes among multidrug resistant tuberculosis patients in Tanzania; 2019.
22. Woldeyohannes D, Aman R, Tekalegn Y, Hailemariam Z. Predictors of time to unfavorable treatment outcomes among patients with multidrug resistant tuberculosis in Oromia region. Ethiop PLoS One. 2019;14:10. doi:10.1371/journal.pone.0224025
23. Bastard M, Hewison C, Hayrapetyan A, et al. Effects of treatment interruption patterns on treatment success among patients with multidrug-resistant tuberculosis in Armenia and Abkhazia. J Infect Dis. 2015;211(10):1607–1615. doi:10.1093/infdis/jiu551
24. Alene KA, Viney K, McBryde ES, et al. Treatment outcomes of patients with multidrug-resistant and extensively drug resistant tuberculosis in Hunan Province, China. BMC Infect Dis. 2017;17(1):1–11. doi:10.1186/s12879-017-2662-8
25. El Hamdouni M, Bourkadi JE, Benamor J, Hassar M, Cherrah Y, Ahid S. Treatment outcomes of drug resistant tuberculosis patients in Morocco: multi-centric prospective study. BMC Infectious Diseases. 2019;19(1):1–7.
26. Kalandarova L, Parpieva N, Saidova S, et al. Treatment outcomes and adverse reactions in patients with multidrug-resistant tuberculosis managed by ambulatory or hospitalized care from 2010–2011 in tashkent, uzbekistan. Public Health Panorama. 2016;2(1):1–116.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
