Back to Journals » Journal of Multidisciplinary Healthcare » Volume 15
Understanding the Nature and Sources of Conflict Among Healthcare Professionals in Nigeria: A Qualitative Study
Authors Mohammed ENA, Onavbavba G , Wilson DO , Adigwe OP
Received 10 May 2022
Accepted for publication 25 July 2022
Published 7 September 2022 Volume 2022:15 Pages 1979—1995
DOI https://doi.org/10.2147/JMDH.S374201
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Elijah N A Mohammed,1 Godspower Onavbavba,2 Diana Oyin-Mieyebi Wilson,2 Obi Peter Adigwe2
1Office of the Registrar, Pharmacists Council of Nigeria, Abuja, Federal Capital Territory, Nigeria; 2Office of the Director General, National Institute for Pharmaceutical Research and Development, Abuja, Federal Capital Territory, Nigeria
Correspondence: Elijah N A Mohammed, Office of the Registrar, Pharmacists Council of Nigeria, Abuja, Federal Capital Territory, Nigeria, Email [email protected]
Introduction: Inter-professional conflict in the Nigerian health sector is a concept that is as old as modern medical practice and has resulted in disruption of health care delivery, with the overall impact bearing down on patients.
Purpose: This study aimed to provide an in-depth understanding and a clearer insight into the causes of conflict in the Nigerian health sector.
Methods: A qualitative strategy was employed using a semi-structured interview approach. Data were obtained from health practitioners from diverse backgrounds in various healthcare facilities.
Results: The phenomenon of conflict was reported as a long existent and trans-generational strain on inter-professional relationships occurring in all sectors of health practice, primarily between the physicians and other health care professionals. Inter-professional conflict was reported to emanate primarily from lapses in leadership, remuneration structure, role description, communication and emotional intelligence. This has affected the effectiveness of the Nigerian healthcare system and has contributed to hindrance in the provision of high-quality care in the country.
Conclusion: Evidence from this study can help in developing contextual policy in addressing inter-professional conflict in the health sector, and this will consequently improve health care delivery in the country.
Keywords: inter-professional, rivalry, health sector, conflict, patient, practice
Introduction
Team work and effective collaboration are important factors necessary for the advancement of various sectors; however, the human propensity for conflict is inevitable when groups of people with diverse backgrounds, professions and orientations are brought together to achieve a common goal.1,2 Conflict is an indispensable phenomenon experienced in every facet of human interaction and remains essential for innovation and creativity in the work place.3 Its presence has, however, plagued organisations, including the health sector with retardation in growth and altered team dynamics.4,5
Conflict in the healthcare system is not a new phenomenon considering the intricate complexities of inter-professional relationships with time pressure, critical life and death decisions, as well as enormous workloads in the sector.6,7 In contrast to centuries back where patient care was manned by only a few professionals, the multiplicity of roles in modern healthcare has amplified interdependent relationships, consequently resulting in frictions, disagreements or discord between members of the healthcare team.8,9 Conflict is therefore attributable to an enduring power struggle, competition for limited resources, unclear job boundaries, inadequate communication, as well as incompatibilities in personality and value systems.10,11 More so, team disagreement left to fester can be deleterious due the tendency to create conflict, psychological tension, violence and interpersonal discords.12
Following this trend, the extent of conflict in the health sector has been expressed as grossly complicated and widespread among the different teams in multidisciplinary healthcare practice.13 A quantitative study undertaken among 128 nurses in private and government hospitals in Jordan revealed that moderate levels of conflict are experienced by nurses, mostly in the form of intra-group conflict and disruptions from physicians.14 In the United States, conflict is perceived to occur on a weekly basis, and previous findings show that about 20% of resident doctors reported serious conflict with other staff members, and close to half of surgeons indicated experiencing conflict about postoperative goals of care.15
Conflict in the health sector has been attributed to patient ownership, better disease management opinions, better patient-drug tussle, or the trust in inter-professional capabilities.16 Although this disharmony is primarily prevalent in tertiary institutions, the complexity of inter-professional conflict in the health sector has been spread towards the primary and secondary health settings where there are fewer workforce and less structural complexity.9 To a large extent, this is prominently reflected in the Nigerian health system and has, in turn, relayed deleterious implications on high-quality health service delivery in the country.16 Healthcare services in Nigeria are provided by both the private sector and the three tiers of government in the country. The public health sector is structured in such a way that the Federal Government superintends over the management of tertiary health facilities, the State Governments has the responsibility of running the secondary health facilities, and primary health facilities are operated by the Local Governments.17 Despite this segmentation in the healthcare sector to improve access to healthcare services, the system has remained daunted by various challenges, such as poor infrastructural development,18 suboptimal quality of care,19 lack of Medicines’ Security,20 and regular strikes by healthcare workers among other factors.21
In a typical Nigerian system, the foundations upon which conflict among healthcare professionals thrives include challenges of leadership structure in the practice environment, inconsistencies in government policies on the roles and welfare of practitioners, labour matters, professional hierarchies, as well as cultural diversity.22–25, A review of extant literature revealed that the idealization of team work and collaborative practice has not been supported thus far in the Nigerian health system and this is displayed in the form of dysfunctional conflicts.16,23,26,27
Unhealthy and counterproductive incidents have been reported between physicians, nurses and other professionals involved in patient care at both local and national levels and have resulted in poor patient management, reduced motivation among health workers, as well as a reduced operational efficiency.26 This has caused a clamor for description in the clinical hierarchy and the acknowledgement of inter-group professional expertise and experiences.25 The consideration of such long-term strife among professionals in Nigerian health institutions, which has impeded healthcare delivery, has made it critical to assess the sources and nature of conflict in the health sector.
A number of studies have been undertaken in the area of inter-professional conflict among healthcare professionals in Nigeria,28–32 and a national study on causes of disharmony among healthcare workers that was previously reported was based on quantitative method.32 There is a need for a robust national study that will holistically assess the nature and source of conflict among health care practitioners in Nigeria. It is against this backdrop that this study therefore follows through with a qualitative approach, in a bid to provide a more detailed understanding of this phenomenon and to produce findings not arrived at by quantitative statistical analysis methods.33 The study aimed at providing clear insights and an in-depth understanding of the nature and sources of conflict in the Nigerian health care sector by employing a qualitative approach in assessing the views and experiences of health personnel. This can in turn reveal areas for potential improvement in collaboration among professionals, as well as improving healthcare delivery in the country.
Methods
Study Design
A review of the relevant literature guided the generation of an invariant methodological approach that was best fit to explore the human phenomena. To gain a deeper understanding of the nature and sources of conflict, a qualitative approach using content analysis was employed. A qualitative approach was the best method suited to generate understanding of the concepts of disharmony in Nigerian health sector since it describes the “lived experiences” of the respondents and helps to understand the activity in context of the everyday life.34,35 Moreover, a qualitative research produces findings not arrived at by quantitative procedures.33
Sampling
A criterion and purposive sampling strategy was employed. In this manner, health practitioners were sampled to gain insights on the level of their knowledge and experience on the phenomenon. Samples were selected based on their diversity in sections of practice and their abilities to provide, reflect, and articulate rich information on the topic.35,36 A total of 22 participants (Doctors, Nurses, Pharmacists, Medical Laboratory Scientist, and Dental Therapists) were included in the study, and this was considered ideal for research of this nature.37 However, saturation was also a critical determinant of the sample size used in the study.
Inclusion criteria of participants in the study were based on their availability and willingness to contribute to the subject matter, as well as their professional licensure with at least 3 years of work experience in government or private health facilities within Nigeria. Healthcare practitioners who did not meet these criteria were excluded from the study.
Data Collection Instrument
Following the qualitative approach, data were obtained using a semi-structured interview guide (Appendix 1). This structure was selectively chosen in order to explore already existent information about the said topic. The interview guide comprised open-ended questions such as:
can you give me an idea of your views and experiences about inter-professional conflict in Nigerian healthcare sector; what do you think is the cause of conflict among healthcare workers in Nigeria?
The questions were structured to obtain demographic information of the respondents and to explore general ideas and reflective perspectives on the subject matter. Interviews unfolded in a manner that gave participants the chance to explore issues they feel are important to the subject matter as well as express their candid thoughts without influences on their anonymity or confidentiality.38 Respondents were allowed to tell their story in their own words so as to provide unique insights into the nature and sources of conflict in the Nigerian healthcare sector.
Data Collection Procedure
Interviews were conducted online via Zoom, which lasted an average of 30 minutes per participant; this encouraged the participation of each interviewee and richness in data was quickly attained. Prior to the interview, consent to be recorded during the session was sought from each participant. All interviews were recorded through an external recorder as well as via Zoom. At the 18th interview, no new theme emerged, and subsequent data collection followed a pattern that paid more attention to addressing the already emergent themes. At the 20th interview saturation was judged to have been achieved, however, two other interviews were further conducted to affirm this.
A reflective journal was kept for note taking during the course of the interviews, so as to capture researchers' observations, interpretations and feelings. All interviews were conducted in English language and were afterwards transcribed verbatim. Files were saved on a portable computer and encrypted for safety and confidentiality.
Data Analysis
A content analysis approach was adopted to analyse data derived from the interviews. Transcripts were scanned to identify emergent codes, themes and categories.39 The data from the transcripts and field notes generated in the course of the interview were coded and compared with the themes that emerged in a bid to validate the invariant constituents. These were also compared using the constant comparison method with the literature review to crosscheck for accuracy and a clear representation of information as well as to enhance information synthesis into more cogent themes. “Memoing” was done to provide reflective identification and writing of ideas or assumptions generated in relation to the entire analysis process. The emergent findings as well as other relevant attributes, such as their frequency of emergence, were recorded in tables and noted as key concepts. Themes that addressed similar issues were eventually clustered accordingly to form two core categories. Each category emerged as a dominant area of interest, showing significant relationships with some of the identified themes. The categories were considerable enough to explain the essence of the phenomenon in a manner that resonated with the synthesised information that made up the results.
Ensuring Quality
Throughout the study, trustworthiness was ensured through the following means:
- Interviews were transcribed verbatim, and a reflective journaling system was adopted following each interview. The researchers were reflexive enough to acknowledge their place of bias in the study and setting them aside before and during the processes of data collection as well as analysis. The subjectivity statements of the researchers were constantly referred to in order to help clarify the researchers position.
- A triangulation strategy was also employed to affirm validity. The strategy for triangulation involved obtaining analysis from multiple perspectives. The data obtained in the course of interviews were analyzed by two independent individuals in a bid to eliminate researchers' bias. The results obtained were in close similitude depicting that findings from the study were not influenced by predetermined ideas of the researchers.
- Furthermore, the critical appraisal skills program (CASP) checklist (2018) was used to validate the entirety of the study. This tool asserts the value of qualitative evidence for informing health policy and practice.40 Using the CASP checklist, every aspect of the study was validated for quality and credibility by appropriately checking all questions on the list.
Ethics Consideration
Ethical approval was obtained from the National Health Research Ethics Committee of Nigeria prior to the commencement of data collection, as they are responsible for granting approval for studies involving participants from multiple health facilities (Approval number: NHREC/01/01/2007-01/03/2021). Respondents were contacted formally to provide details of the study to them, as well as information on confidentiality and anonymity before undertaking the interviews. Participation of the respondents in the study was solicited at this stage, and informed consents were obtained which included publication of anonymised responses. There was no potential risk for taking part in the study and participation was entirely voluntary. All information provided was kept safe and used solely for the purpose of this research. Confidentiality, anonymity and highest ethical standards were maintained throughout the course of the study.
Results
Demography
Table 1 shows the demographic characteristics of 22 participants who participated in the study based on the information they provided in the course of the interviews. The demography represents 5 doctors, 5 pharmacists, 5 nurses, 6 medical laboratory scientists and 1 dental therapist who have experienced one or more incidents of conflict at different times of practice.
 |
Table 1 Demography of Health Professionals |
Findings
The analysis revealed two core categories. These include nature and sources of inter-professional conflict in the Nigerian health sector. The categories and sub-categories that emerged from the coding comprised 3 levels. Findings from the study indicate that conflict in the health sector has existed for a long time. Data provided views on the nature of these conflicts and the various sources from which they emanate. Five sub-categories emerged as sources of inter-professional conflict which include poor job description and clarity of roles, leadership, emotional intelligence, poor communication frameworks and disparity in remuneration. Predominant among these was leadership, where nearly all participants indicated that leadership was a critical cause of rancor across various settings of healthcare. A summary of the various categories that emerged from this study is presented in Figure 1.
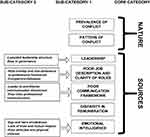 |
Figure 1 Flow diagram showing categories and sub-categories of findings. |
Nature of Conflict in the Health Sector
Considering the prevalence and long-lasting history of conflict in the Nigerian health setting, every professional seemed to have a perceived notion with regard to the inter-professional conflict in the health sector. Clearly enough, inter-professional conflict was envisaged by quite a number of the respondents prior to practice and was eventually experienced within the course of work. This category explores the existence of conflict in the health sector.
Prevalence of Conflict
The concept of conflict among different health care practitioners was observed to be a recurrent trend in the Nigerian setting. Health workers experience conflict on a daily basis in mild or confrontational patterns, thus creating room for inefficient patient management.
… yes, there is a lot of conflict among health workers. it is something that sometimes it could be all vast. like confrontational output. But at times it could be something that you don’t often come out to see …. the conflict situation. But you know that it is there and it is an ongoing thing …. (Practitioner 6, Male, Pharmacist with 9 years work experience in a tertiary health facility)
… where will I start? It is so much, a vast topic that I will be very unbiased. I have been practicing for the past 28 years, if I tell you the truth about the professional conflicts or inter-professional war that is going on, I will say that it is not a cordial one …. (Practitioner 7, Male, Nurse with 28 years work experience in a tertiary health facility)
Pattern of Conflict
Considering the long existence of conflict, it is possible that strategies have been long implemented to curb the existing menace. Sadly, the practice of inter-professional rivalry seems to be unabating. Young professionals are fueled right from the processes of training on the disharmony in the health sector and enter into practice to continue the long-standing tradition of conflict exhibited by senior colleagues.
… as I said, I came in as a student, around 2001, 2002. And since then from student level, we were told of the problem on ground, and till now, in my little years of practice, the problem have been there …. (Practitioner 1, Male, Medical Laboratory Scientist with 13 years work experience in a tertiary health facility)
… the inter-professional conflicts that is domiciled in the health care system in Nigeria in my perception is long standing and had been passed on from one generation to another over the past decades. I believe this has been in the hearts and minds of new entrance into the health care team even before induction. They already see their co- practitioners as threats, so, that already sows a seed of conflict before they even get to the field where they are actually required to save lives and contribute their own quota in ensuring quality healthcare delivery …. (Practitioner 17, Male, Pharmacist with 4 years work experience in a private health facility)
However, the pattern seemed to be more domicile between the physicians and other healthcare professionals.
… it was as if the people in the lab are against the doctors, and the other people are against one another … … if you are following very well, it’s like the doctors are on one side and all other health professionals are on the other side. ….So they form a Coalition, they call it JOHESU, they are like on the other side against the doctors. The doctors against the other people. So, there is a fight going on … … (Practitioner 2, Male, Medical Doctor with 15 years work experience in a tertiary health facility)
… there is always conflict between doctors and nurses, doctors and lab scientists, doctors and radiographers, virtually all other professions are having conflict with the doctors …. (Practitioner 7, Male, Nurse with 28 years work experience in a tertiary health facility)
… it’s very common between nurses and the doctors, between doctors and pharmacists. But between nurses and pharmacists, it looks as if it is not so common because they are not really having much to do together …. (Practitioner 9, Male, Nurse)
Sources of Conflict in the Health Sector
From the interviews, it became prominent that leadership and remuneration were major causes of conflict in Nigerian healthcare system. Consequently, other prominent themes emerged that focused on emotional intelligence, clarity of roles, and communication as a major barrier to collaboration and team work in the practice setting.
Leadership
Sub-categories that emerged from leadership as a cause of conflict include leadership struggle, leadership inadequacy, bias in governance, lack of professional autonomy and poor work environment. In practice, it seemed more likely that many professionals are aggrieved by the pattern of leadership and governance in the health sector. Conflict in the health sector has been primarily centered on who should be the head of the sector, fairness and bias of leadership, as well as the poor provision or implementation of a working system.
Lopsided Leadership Structure
The Nigerian healthcare system is faced with challenges of leadership. Currently, the leadership structure of the system is lopsided, thereby creating tension and struggle where other healthcare professionals feel marginalised. Furthermore, hierarchy is often inherent to medical and clinical decision-making. Some groups of health care professionals have fostered a culture of hierarchical power structure, which has a tendency to cause inter-professional conflict. Based on this, some of the participants were of the opinion that the current leadership structure is not the best for effective service delivery and opined that clinical competence does not equal the administrative prowess required to manage diverse health professionals in the field of healthcare practice.
… instead we are just after supremacy; who will be head of this, who will be head of that. So, the main essence actually, it’s supposed to be a multi-disciplinary work. There is nothing wrong in being a pathologist or being a medical lab scientist if our goal is to serve the patients. And if our goal is to get the quality, you will find out that the space is very big enough for all of us to actually work together if quality is actually our watch ward …. (Practitioner 18, Male, Medical Laboratory Scientist with 8 years work experience in a tertiary health facility)
… firstly, I have always been of the opinion that being the head of the healthcare team does not directly qualify you to be the head of hospital. If you look down at our systems, you will observe that the training of the medical doctor, for instance does not involve him being trained administratively on the do’s and don’ts of administration hence he lacks the required knowledge he needs aforetime, from the beginning, right from when he is inducted into the medical profession on how to run an hospital …. Let a medical doctor focus more on his training because the training does not train him to be a CMD … (Practitioner 17, Male, Pharmacist with 4 years work experience in a private hospital)
… lack of either leadership or technicalities in the management of those professionals actually lead to a lot of conflict … (Practitioner 18, Male, Medical laboratory scientist with 8 years work experience in tertiary healthcare facility).
Professionals are continuously involved in the tussle for leadership and governance where every practitioner is believed to be competent enough to attain an administrative position in the health sector. It emerged that the solitary leadership by physicians and lack of widespread administrative authority among other healthcare workers had a considerable impact on the conflict.
… the leadership should not be limited to one profession. Imagine in the leadership team, you are having just one voice. Only one profession is there. You will see that, when they are making decisions, they will always make a decision that will favour just members of the profession they are coming from. But in a situation whereby you have a leadership team where different members of the team make up the leadership, it means that, whenever you are making decisions, the decision will be such that it favours every member of the team and at the same time the interest of the patient …. (Practitioner 19, Male, Medical Laboratory Scientist with 5 years work experience)
… I think, most of the professionals in the health sector are actually not happy that they are not given an opportunity to reach the peak of their career. There is no reason why a pharmacist, a medical lab scientist that reaches a director cannot head the health sector. Why must it be a doctor always? So, I think this particular thing, the civil service rule does not limit, but we limit it from the context of the hospital set up which is one of the key problems why the other professionals feel aggrieved to a larger extent …. (Practitioner 18, Male, Medical Laboratory Scientist with 8 years work experience in a tertiary health facility)
Contesting the hierarchy in the health system goes much further beyond administrative authority but also on clinical authorities. The continuous tussle for patient ownership sets the pace for undue disagreements which eventually takes its toll on patient care.
… had been a time where several years back, where we need to fight over who is the real owner of the patient. You go to the ward and the nurse says this patient is my patient, and the doctor says, this patient is my patient, so, the fight over who really owns the patient … …. (Practitioner 2, Male, Medical Doctor with 15 years work experience in a tertiary health facility)
More so, professional autonomy was seen as a factor influencing conflict. This was attributed to role infringements and encroachment into a territory which other professionals consider their responsibility.
… we have conflicts of who should be the head, and who should not be the head. We also have issues of … you know, like me, I said I am a medical laboratory scientist. So, who should sign out results, who should not sign out results. Who should vet results, who should not vet results. All those things, we have them in the course of my practice …. (Practitioner 16, Male, Medical Laboratory Scientist with 27 years work experience in a tertiary institution)
… also, there is this issue of headship of the lab. In other climes of the world, even down Ghana, where there is professional autonomy. As a medical laboratory scientist, you are supposed to head at least your department. Although we have the pathology department. …. Well, we have the office of the pathologist and they are distinct, so, medical laboratory science should also be recognised as a distinct profession where people should be able to head their department and rise to the pinnacle of their profession … …. (Practitioner 15, Male, Medical Laboratory Scientist with 9 years work experience in a research institute)
Bias in Governance
It appears that if professional autonomy is not achieved and leadership remains one sided, nepotism and undue favoritism will continue, and the leadership style will be channeled to favour a group of professionals over others. Participants were of the opinion that bias in the current leadership structure was a major hindrance to harmony and efficiency in patient management, hence resulting in a lack of motivation to work effectively.
… one, if you do not pay attention to what your people are telling you … if you are biased per se, if you have some sort of favouritism towards one group of health practitioners than the others, this is significant. I think it is significant enough. … …. (Practitioner 12, Male, Medical Doctor with 8 years work experience in a tertiary health facility)
Bias in governance was perceived as providing support, structure and sponsorship for the training and professional development of a particular group of professionals, whilst denying all other members of the healthcare team these same rights and privileges. Bias could also be said to emanate in the form of policies that favour one group as opposed to the other in terms of welfare.
… yes, the policy of the country has given us the right to all these training and retraining but somehow, it appears it’s only resident doctors that are entitled to training. I have trained myself at MSc level, I have undergone other trainings and certifications but I sponsored myself. But there are people that we are working with that can access funds in order for them to get higher knowledge … (Practitioner 18, Male Medical Laboratory Scientist with 8 years work experience in tertiary health facility)
… as we always observe, in most of our teaching hospitals especially here in Delta state, the teaching hospital at Oghara, the FMC at Asaba. you will see medical doctors being provided accommodation during their housemanship training. The pharmacists, the lab scientists, the nurse are told ‘go and look for accommodation outside the hospital’ … (Practitioner 17, Male, Pharmacist with 4 years work experience in a private health facility)
… can I tell you the truth sir? We went on strike, for almost 3 months. That is all other members of the health team apart from the doctors, that was 2018, I think. We spent 2 months plus, and the government brought a policy that no work no pay …. by the time doctors went on strike, they spent the same number of months we also spent - 2 months …. at the end of the day, the government knowing that they have already said they were not going to pay them, they came up and said they are going to pay the money …. (Practitioner 7, Male, Nurse with 28 years work experience in a tertiary health facility)
… that is where I am blaming the government, I think the structure is also not balanced. It gives more power to certain people and it makes them get away with a lot of things … … (Practitioner 10, Male, Pharmacist with 7 years work experience in a tertiary health facility)
… and you are bragging about because at the top managerial level, you have the backing and you have a policymaker that that seems to support you …. (Practitioner 1, Male Medical Laboratory Scientist with 13 years work experience in a tertiary health facility).
Poor Job Description and Clarity of Roles
Due to advancement and emerging new areas of healthcare, there have been role overlaps without clear distinction in the performance of some functions. This has also resulted in encroachment in some aspects with some practitioners not adhering to the scope of their practice.
Role Overlap and Non-Adherence to Professional Framework
Contemporary healthcare practices have resulted in a vast array of knowledge and advancements in job descriptions that have in one way or another promoted co-dependency and certain similarities in professional practices. Health practitioners become oblivious of the submergence of roles and may be said to have practiced beyond their scope
… is poor understanding about individual roles to be played by each cadre of worker and that actually brings conflict because if we do not understand our roles or the roles we are supposed to play in the setting, then it is likely going to bring friction between the healthcare workers which is what has been seen … …. (Practitioner 21, Male, Medical Doctor with 7 years work experience in a secondary health facility)
… if you come to the area where I am, the lab, we have some professional misunderstanding. A pathologist is a licensed doctor that is supposed to interpret results to his colleagues – the clinicians – in the clinic, but he happens to find himself in the lab where he is not licensed to practice as a medical laboratory scientist. We are all guided by rules and protocols, our curriculum in the universities and our educational curriculum are quite explicit, but when you come down to practice, you find that there is a lot of false task shifting where people think that they have the right to take care of, or to take other professional work irrespective of whether they are licensed or whether they are qualified to do that …. (Practitioner 18, Male Medical Laboratory Scientist with 8 years work experience in a tertiary health facility)
… now, after graduating from school, we noticed that some institutions will say no, the setting of intravenous line is the primary assignment of the doctors and on no account should a nurse do it. Some places will say no, a nurse can set line, and the doctors can as well set the line. Assuming there is a law that has stated clearly that, setting of intravenous line is the primary duty of the doctors, nurses acts based on that. If you say giving of injection is the basic duty of the nurse, there will not be conflict between nurses and doctors at nurses giving injections.…. (Practitioner 9, Male, Nurse, works in secondary health facility)
Compartmentalization
One aspect of conflict arising from poor job description is the idea of compartmentalization. Groups of professionals are segmented into different sections of healthcare setting and are oblivious to the roles or practices of the other.
…. we don’t know the roles of one another. It seems that the whole system is very compartmentalized so to say. Everybody is in his own compartment and he doesn’t really know much what is happening at the other end. So, there is room for misunderstanding. Either you are of getting into my work, or you are trying to bring me down. That is one of the things. So, understanding the role in which the other team member plays is one of the things that is actually lacking …. (Practitioner 6, Male, Pharmacist with 9 years work experience in a tertiary health facility)
Poor Communication Framework
Clear communication is considered the sine qua non of effective teamwork. Potentiation of errors can arise from messages lost in translation or lack of idea sharing. Communication patterns among health professionals have not been regarded as cordial. This theme is centered on communication disconnect or message lost in translation.
Leaders-to-Practitioners Communication Disconnect
Information dissemination in the flow of hierarchy has been regarded as dysfunctional and requires adjustment. This is expressed as a preference in communication dissemination that likely leaves other groups behind. This can be seen within the different areas of practice.
… the issue of communication is not very cordial …. Locally, you will see sometimes in disseminating information, doctors are being considered first, maybe they feel they need to have a first-hand information in some things …. (Practitioner 16, Male Medical Laboratory Scientist with 27 years work experience in a tertiary health facility)
… I think in my own view, for every system that wants to grow, communication is quite key and strategies have to be put in place to move information from the grassroots to the top management and the top management down to the grassroots. Once there is clarity and understanding of clear objectives of establishments, then you will find out that there will be smooth running of any activity and in a well-coordinated manner …. (Practitioner 18, Male Medical Laboratory Scientist with 8 years work experience in a tertiary health facility)
More so, government and management policies have been expressed as being implemented without proper communication and understanding of what is attainable at the practice level.
… we have a management that is not sensitive to what his health care workers are going through. It is also very important. If we have poor communication from the management, inappropriate or lack of responsibility or impact to your staff, then this could also contribute significantly to conflict among healthcare workers …. (Practitioner 12, Male, Medical Doctor with 8 years work experience in a tertiary health facility)
Poor Inter-Professional Communication
More evident in this setting is the lack of communication among individuals where professionals may have dissimilar goals in patient management or otherwise. This could also emanate from proof of showmanship and intellect, thereby causing disregard for the professional opinions of others.
… a situation whereby the doctor will make a prescription and the pharmacist will see it and say ‘ no! no! this thing is wrong’ and he is not saying it is wrong for you to correct it, but you are saying it is wrong to show that at least, in this your profession you are better than the other person. This should not be our view. Our view should be a collective effort gearing towards our patients …. (Practitioner 9, Male, Nurse working in a secondary health facility)
… the genesis of this problem, looking at it will be lack of communication in a way. Communication is a key thing that fuels this crises and this communication comes in the fact that, within us, we are not communicating. The communication happening at the individual level such as within the nurses, they have their own medium of communication. What they are saying to themselves is like we must protect ourselves, we must do this, and then it becomes like everybody is on his own even though we are supposed to be working together …. (Practitioner 2, Male, Medical Doctor with 15 years work experience in a tertiary healthcare facility)
… factors that could affect the employee could simply be maybe lack of communication. Maybe you do not communicate appropriately with someone and then your idea are lost in translation …. (Practitioner 12, Male, Medical Doctor with 8 years work experience in a tertiary institution)
Disparity in Remuneration
The disparity in resource allocations, such as salary, allowances and other welfare packages, was identified as a cause of conflict among healthcare professionals. The discrepancies in salary allocation were perceived as unfair by many healthcare professionals, thus demanding equity in resource distribution among each member of the healthcare team. The differences in salary allotment on the basis of entry levels and salary scale turned out as a major source of conflict in the healthcare space.
… they give you a percentage of your salary which are not equal, which the salaries are not the same, yet their percentage in the hospital is highest and they bring down other people’s percentage. Irrespective of how small their salary is. This is not a fair deal for the health system and if this continue, there will continue to be a rancor in the system …. (Practitioner 20, Male, Nurse with 10 years work experience in a tertiary health facility)
Owing to the differences in years of training, many professionals seem to note the difference in remuneration as normal; however, they were dissatisfied with the large margin and demanded equity rather than equality.
… other health professionals that spent five years in the university happens to have a very wide gap with others that spent six years. The disparity of one year actually is not supposed to be that wide. Even though there should be gap, we are not talking about equality, we are talking about equity. There should be equity in division of remuneration and welfare in the health sector …. (Practitioner 18, male, Medical Laboratory Scientist with 8 years experience in a tertiary health facility)
Some others opined that salary and wages should be allotted based on working hours and not on professional background.
… come to the area of salary, it can only happen in Nigeria where you will see a doctor who is on call, for probably a couple of hours in the week, his take-home will be more than the nurse who was on duty for five days in a week and had only two days off. By the time you see their take-home you cannot even compare it. Unlike in the developed countries, whereby you will be paid per hour depending on what you do. You will work and you will be paid base on that. But here, they will just know that oh because you are a pharmacist, because you are a medical doctor, because this person is a nurse, you just place them on different salary scale. In as much as the doctors are still earning the highest salary, of course every other people behind him that are not earning up to him you will see them as a subordinate …… (Practitioner 9, Male, Nurse working in a secondary health facility)
The struggle for resources have emerged in a manner such that different groups of professionals presume they are better deserving of higher remuneration and allowances due to their work schedule.
… still on the interest of members of this team, each group who make up this team are saying that, they are supposed to be more rewarded than others, because of this, the problem goes on …. (Practitioner 19, Medical Laboratory Scientist)
Emotional Intelligence
The fact that individuals are of different backgrounds, opinions and professional upbringing is a leading cause of conflict in the health sector. Due to the diversity in cultures, traditions and religions in Nigeria, vast differences occur in views, communication patterns and perception.
… yes the other thing will be, the human ego that we all carry. Most times as a lab scientist you begin to look like this doctor is younger to you in terms of age, so why should he be the one telling you that we need to do this and all of that. So, the human ego part of it is also one of the key things I also see …. (Practitioner 2, Male, Medical Doctor with 15 years work experience in a tertiary health facility)
Also expressed in this theme are the concepts of ego, hero mindedness, lack of mutual respect, poor attitudes, lack of trust, physical violence and assault, as well as unappreciated roles.
Ego and Hero Mindedness
Diversity in professional training and orientations can breed conflicts in the health system. The feeling of egoism and superiority was expressed severally as some sources of conflict in the health sector.
It starts right from school whereby, the student of one profession see themselves to be better than students of the other professions rather than working as a team …. (Practitioner 19, Medical Laboratory Scientist)
… for me, I feel it is ego …. You will always hear them saying that doctors are superior over every other person. And so, because they are superior over every other person or every other health professional, they feel they should also head every other health professional, but it is not so …. (Practitioner 16, Medical Laboratory Scientist)
Some of these notions seemed to have been generated right from the training institutions and are replicated among a particular set of professionals. This can ultimately cause morbidity or inefficient service delivery to patients due to the fact that it represents the inability to take suggestions or corrections, the perception of superiority, or the feeling of being heroic and better than others.
… my worst personal experience as a pharmacist came on board last year October to be precise when a prescription came from one of the hospitals nearby, and after screening the prescription, I noticed that there were lots of unnecessary drugs and immediately, I tried to contact the physician in a polite way to discuss my discrepancies. However, he was unable to admit his fault and though, I did not dispense the drug, but he was like, he is a medical doctor and he knows it all. And it should not be so, we are professionals, we should be working towards achieving a common goal towards our patient …. (Practitioner 3, Male, Pharmacist practicing in a community pharmacy with 6 years experience)
… from my experience, I have seen a doctor, to be specific, make a mistake. And because ego, and existing conflict between the doctor and the nurse, has given an overdose of promethazine injection to a patient. He administered it and the rest they say is history. Although the patient … no fatality was recorded, but other things had to be done to arrest the situation I believe if that ego was not existent, that conflict was not there …. (Practitioner 17, Male, Pharmacist working in private facility with 4 years practice experience)
Lack of Trust and Mutual Respect
These aspects of egoism can rob team members of respect for each other. In further light, there is an exhibition of lack of respect for intellect, professional contributions to patient care or an outright neglect of professional boundaries.
….well, I think that could be true partly. Because some physicians can actually tell you, what is your role in this place? You are just like an attachment, an accessory. You don’t really have a key role to play. So, if you already have that kind of mindset, how do you give the best? It is almost impossible …. (Practitioner 6, Male, Pharmacist with 9 years experience in a tertiary health facility)
… most times a group thinks that they own the patient in the hospital. And they do not allow other professionals to give their best just because they feel that they own the patients and their decision is final concerning the patients. …. One of the pharmacist undergoing training in the West African Postgraduate College of Pharmacist was supposed to go for ward rounds in a particular ward, and then the physician in charge of that ward tried to walk them out and said ‘what are they doing with his patients folder’ that led to exchange or banters. He got angry and pharmacists were angry, and he went to report to his other colleagues that the pharmacist were challenging him concerning the patients folder. The pharmacist had to take it up with the management. Unfortunately, the management did not handle it well …. (Practitioner 8, Female, Pharmacist with 22 years experience in tertiary health facility)
Such level of attitudes breeds anger, unaccommodating behaviour, and lack of trust in the competence of other groups in achieving the desired patient outcome
… when they come to the lab, we will tell them the result is genuine, it has been done. When they go back to them there, they will tell them, this result is fake, they cannot work with this. So, at the end of the day, they will either refer the patient to another hospital or refer the patient to another lab, or sometimes they just handle the patient, maybe treat the patient based on what they think. So, that is really affecting the patient seriously …. (Practitioner 16, Male, Medical Laboratory Scientist with 27 years experience in a tertiary health facility)
Poor Attitudes and Physical Violence
Poor attitudes to work, patient care, or inter-personal relationships were given as one of the prominent reasons for conflict in healthcare settings. Professionals sometimes exhibit conducts that are ill and improper, such as physical assault and negative attitudes.
… you know, you are asking for something and the way you ask even the tone of your voice goes a long way to know if you will get results or not. So, emotional intelligence has a very big role to play … … and then it also boils down to this Nigerian thing where anything public does not work, it is always being destroyed by one thing or the other. So, when somebody comes that knows one person or the other, they do whatever they want to do and they get away with it …. (Practitioner 2, Male, Medical doctor with 15 years work experience in a tertiary health facility)
… I feel as humans, we know what is right, but people in our side of the world they do what they like. When they go to other places where things are organised, these same people behave well. So, I think when people see loop holes in a place, they try to take advantage … …. (Practitioner 10, Male, Pharmacist with 7 years work experience in a tertiary health facility)
Discussion
A clear portrayal of the existence of inter-professional conflict presents itself throughout the course of this study and has revealed that conflict among healthcare practitioners is a phenomenon experienced regularly within the health sector.
Findings from this study indicate a high level of conflict within every area of the healthcare system, which could be deleterious to both professionals and patients. Doctors, nurses, pharmacists, medical laboratory scientists and other health professionals reported incidents of inter-professional conflict within their practice settings, thereby mirroring previous findings that indicated a high prevalence of conflict in the Nigerian healthcare sector.41,42 The implication of this is the negative impact of healthcare delivery due to these unhealthy practices. Findings in this study also suggest that inter-professional conflict in the healthcare sector is predominantly between the physicians against other practitioners, and this corroborates earlier findings.31
Conflict in the sector was seen as trans-generational. Participants in the study expressed rivalry as a phenomenon passed on from older generations to young professionals just coming into healthcare practice. They attested to their fore knowledge of conflict before entering into the practice setting, which was eventually translated into one or more experiences. This shows that almost every health professional has had at least one experience of conflict in the course of practice,43 and this can ultimately result in poor service delivery.
Conflict has been reported at all levels of the healthcare system from primary to tertiary healthcare facilities, and therefore implies that, in addressing conflict, all aspects of the health sector must be considered irrespective of the size of the institution or the workforce.30,44
In this study, leadership structure was identified as one of the sources of inter-professional conflict in the healthcare sector. Participants attributed some of the causes of conflict to bias and lopsided appointments in leadership, suggesting the need for urgent reforms in the current administrative structure. This finding further corroborates previous reports,22,32 whilst also revealing a clear gap between the management of healthcare system in Nigeria and other developed climes where leadership is based on competence and expertise rather than professional background.45 A critical look into the administrative process of Nigerian health institutions reflects that physicians have maintained a sovereign hierarchy in the health system.46 Leadership positions are dominated by the medical doctors without emphasis on administrative competence.47 Several practitioners in this study were of the opinion that clinical prowess is not equivalent to administrative skills, and this further validates previous findings which reported that being a better physician does not automatically translate to making a good leader.48 To address the issue of poor leadership structure, participants supported the need for policies that incorporate a competent health administrator or a mode that spreads leadership across the different health professions. For government and policymakers, it is important to develop contextual strategy underpinned by these findings so as to conform to international best practices and reduce conflict in the sector.
From the perspective of the medical laboratory scientists in this study, professional autonomy was seen a primary source of conflict, and they described the idea of dominance by physician as an infringement, whilst opining that this situation can prevent them from contributing their best to patient management. Owning to this, medical dominance has been cited as a cause for power tussle thereby depicting that the extent of conflict in any health institution is related to the extent of power tussle and resistance to dominance.49 This has contributed greatly to rivalry in the health sector irrespective of the professional backgrounds, with a defective implication on loss of job satisfaction and professional inefficiency if not properly managed.50
In contrast to other health professionals, physicians were less likely to communicate leadership as a source of conflict but have rather hinged on the reasons such as improper communication, poor attitude to work, low emotional intelligence and undue competitiveness in the health sector. This could be attributed to the trend in the current leadership structure which is in favour of the medical doctors.27
However, other healthcare professionals had also clamored for sovereignty in power similar to the physicians in such a manner that they can also administer management within and outside their respective departments. This implies that there is a need for headship of hospitals to be made attainable to all healthcare professionals on the basis of expertise and competence. This will eventually give room for effective leadership structure such that, the positions of the Minister of Health, Minister of State for Health, Chief Medical Directors or Chairman of the Medical Advisory Committee can be held by different professional groups in order to diversify management opinions, reduce bias, make policies that can be favourable to all members of the team and give room for excellent service delivery to patients. A confrontation of hierarchy among health care professionals in Nigeria can potentially reduce bias and improve efficiency.46 However, there have been counter-resolutions that the leadership by physicians has been efficient but faced with professional, economic or social attempts that try to deviate attention from the main essence of healthcare.48
Furthermore, non-clarity of roles was revealed as a source of inter-professional conflict. Health practitioners indicated encroachment of responsibilities, and role overlap as one of the factors responsible for conflict in the sector, thereby validating previous findings.51 With respect to the inculcation of specialisation and multiplicity of practices in modern medicine, conflict rather than efficiency in patient care delivery has ensued, showing an unclear distribution of responsibilities, encroachment and consequent disunity in patient management. Practitioners fight to maintain boundaries when they perceive a breach of the legal framework of practice by others. It is important to develop a robust framework with clearly defined roles and scope of practice for all healthcare professionals. The generation of such a framework will clarify boundaries and greatly limit rivalry that can emanate from the blurring lines of inter-professional responsibilities in the health sector.52
Another emergent cause of conflict was poor communication framework in the health sector. Findings suggest that a lack of proper communication structure can result to practitioners encroaching beyond their scope of practice whilst being oblivious to the disposition of other professionals.53 In similitude to other reports,54 compartmentalization was seen to have resulted in poor communication and a consequent lapse in patient care. A defunct inter-professional communication or deficit in leader to member communication channel has been shown to breed conflict in different sectors of healthcare practice. Messages can be lost in translation, or not communicated at all, thus ultimately affecting the patient. The findings from this study therefore suggest a need to promote interdependency in practice as well as improve communication mechanism in a manner that will promote inter-professional collaboration so as to reduce compartmentalization in the system. As asserted, this strategy can aid in proper communication in practice settings and will eventually lead to efficient patient care.28
The issue of remuneration and salary scale were also predominant as sources of conflict in the health sector. Other healthcare professionals were of the opinion that remuneration pattern in the healthcare sector is in favour of medical doctors, and this was seen to have played a key role in inter-professional conflict, thereby validating previous reports.32,55 The wide disparity in salary and entry level into public service between physicians and other healthcare workers shows a margin that is far higher in comparison to the one-year difference in training. This is quite different from what is obtainable in developed settings and has caused uproar for equity.56,57 This finding suggests the need for harmonisation of salary structure and welfare allocation among healthcare professionals in Nigeria.
Furthermore, the findings of this study suggest that the large disparity in emoluments and mode of training has led to a poor emotional intelligence in collaborative health service delivery. The perception of superiority, egoistic attitudes and belittling of inter-professional efficiency has caused conflict in the health sector. This is similar to other studies where poor attitudes and lack of mutual respect between professionals were identified as causes of conflict.25,26 Professionals irrespective of age, professional background, sector of practice or years of experience are expected to maintain high level of emotional intelligence and mutual respect for the competence of one another in order to promote harmony in the health sector.
Limitation of this study can be associated with the recruitment process of participants which did not take into account various union leaders as well as headship of various departments in healthcare facilities who may have different perspectives on the phenomenon of conflict in Nigerian health sector. This is, however, mitigated by various strengths of the study, which include recruiting participants across different professions, as well as practice settings, and with diverse years of practice experience.
Conclusion
Findings from this study suggest conflict is prevalent in the Nigerian health sector. This phenomenon is experienced by different groups of professionals. There is a need for team work to be promoted among healthcare workers.
Whilst patient care is perceived to be most affected by inter-professional conflict, this study also showed that conflict can lead to a lack of satisfaction in professional career. Practitioners are therefore more likely to exhibit characteristics that impede the necessary collaboration for patient care and management, which in turn decreases efficiency in the health system and ultimately patient management.
Poor leadership structure, lack of clarity roles, as well as poor communication were linked to sources of conflict in the Nigerian health sector. Also, disharmony in the sector was attributed to government’s poor attitude in addressing the needs of the sector which has subsequently caused a strain on the workers and the system. Inter-professional conflict in the healthcare sector may not only hinder access to high quality of healthcare to the populace but can also result in wastage of resources, for both the healthcare system and patients. There is, however, no better time than now to articulate strategies for mitigating and preventing disharmony in the Nigerian healthcare system.
Findings from this study can provide a guide in developing a robust and comprehensive policy for addressing conflict in the Nigerian healthcare industry. It has also emerged that there is an urgent need for leadership reforms in the healthcare sector, as this approach can go a long way in repositioning the healthcare system for effective service delivery. The introduction of rotational leadership system among different healthcare professionals or the use of health administrators as headship of healthcare facilities would be of importance in reducing conflict in the sector. Furthermore, it is important for government to develop contextual strategy that can promote collaboration among different professional groups. In addition, a comprehensive review of salary structure will be invaluable in reducing conflict in the sector.
Acknowledgement
The authors sincerely appreciate Mr. Charles Balogun for his technical assistance whilst undertaking the interview of participants in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Obiekwe O, Mobolade GO, Akinade ME. Team building and teamwork in organizations: implications to managers and employers in work places. IJMSSPCS. 2021;4(1):261–274.
2. Cheng AS, Kruger LE, Daniels SE. “Place” as an integrating concept in natural resource politics: propositions for a social science research Agenda. Soc Nat Resour. 2003;16(2):87–104. doi:10.1080/08941920309199
3. Rahim A, Bonoma TV. Managing Organizational conflict: a model for diagnosis and intervention. Psychol Rep. 1979;44(suppl 3):1323–1344. doi:10.2466/pr0.1979.44.3c.1323
4. Jehn KA. Enhancing effectiveness: an investigation of advantages and disadvantages of value-based intragroup conflict. Int J Conflict Manag. 1994;5(3):223–238. doi:10.1108/eb022744
5. Tekleab AG, Quigley NR, Tesluk PE. A longitudinal study of team conflict, conflict management, cohesion, and team effectiveness. Group Organ Manag. 2009;34(2):170–205. doi:10.1177/1059601108331218
6. Haraway DL, Haraway WM. Analysis of the effect of conflict management and resolution training on employee stress at a healthcare organization. Hosp Top. 2005;83(4):11–17. doi:10.3200/HTPS.83.4.11-18
7. Almost J, Doran D, Hall L, Laschinger H. Antecedents and consequences of intra-group conflict among nurses. J Nurs Manag. 2010;18(8):981–992. doi:10.1111/j.1365-2834.2010.01154.x
8. Ramsay MAE. Conflict in the health care workplace. J Health Care L Pol’y. 2001;14(2):138–139. doi:10.1080/08998280.2001.11927749
9. Brown J, Lewis L, Ellis K, Stewart M, Freeman T, Kaperski MJ. Conflict on inter-professional primary health care teams – can it be resolved? J Interprof Care. 2011;25(1):4–10. doi:10.3109/13561820.2010.497750
10. Malik ME, Nawab S, Naeem B, Danish QR. Job satisfaction and organizational commitment of university teachers in public sector of Pakistan. Int J Bus Manag. 2010;4(6):17–26.
11. Lukes S. Moral Conflict and politics. Clarendon press. Available from: https://www.philpapers.org/red/LUKMCA/.
12. Wokoma CU. The effects of industrial conflicts and strikes in Nigeria: a socio economic analysis. Int J Dev Manag Rev. 2011;6(1):32–40.
13. Liberati EG, Gorli M, Scaratti G. Invisible walls within multidisciplinary teams: disciplinary boundaries and their effects on integrated care. Soc Sci Med. 2016;150:31–39. doi:10.1016/j.socscimed.2015.12.002
14. Higazee MZ. Types and levels of conflicts experienced by nurses in the hospital setting. Health Sci J. 2015;9(6):1–6.
15. Olson PJ, Brasel KJ, Redmann AJ, Alexander GC, Schwarze ML. Surgeon-reported conflict with intensivists about postoperative goals of care. JAMA Surg. 2013;148(1):29–35. doi:10.1001/jamasurgery.2013.403
16. Nwobodo EO, Nwadinigwe UC, Anyehie UB, et al. Inter-professional conflict among healthcare teams in Nigeria: implications on quality of patient care. Res Sq. 2021. doi:10.21203/rs.3.rs-904216/v1
17. Oyibocha EO, Irinoye O, Sagua EO, Ogungide-Essien OT, Edeki JE, Okome OL. Sustainable healthcare system in Nigeria: vision, strategies and challenges. J Financ Econ. 2014;5(2):28–39.
18. Ademiluyi IA, Aluko-Arowolo SO. Infrastructural distribution of healthcare services in Nigeria: an overview. J Geogr Reg Plan. 2009;2(5):104–110.
19. Ephraim-Emmanuel BC, Adigwe A, Oyeghe R, Ogaji DS. Quality of health care in Nigeria: a myth or a reality. Int J Res Med Sci. 2018;6(9):2875–2881. doi:10.18203/2320-6012.ijrms20183621
20. Adigwe OP. Stakeholders’ perspective of role of policy and legislation in achieving medicines’ security. IJWPDS. 2020;6(66):66–73. doi:10.32861/ijwpds.66.66.73
21. Oleribe OO, Udofia D, Oladipo O, Ishola TA, Taylor-Robinson SD. Healthcare workers’ industrial action in Nigeria: a cross-sectional survey of Nigerian physicians. Hum Resour Health. 2018;16(1):1. doi:10.1186/s12960-018-0322-8
22. Oleribe OO, Ezieme IP, Oladipo O, Akinola EP, Udofia D, Taylor-Robinson SD. Industrial action by healthcare workers in Nigeria in 2013–2015: an inquiry into causes, consequences and control—a cross-sectional descriptive study. Hum Resour Health. 2016;14(1):1–10. doi:10.1186/s12960-016-0142-7
23. Adeloye D, David R, Olaogun A, Iseolorunkanmi A. Health workforce and governance: the crisis in Nigeria. Hum Resour Health. 2017;15(32):1–8. doi:10.1186/s12960-017-0205-4
24. Mohammed E. Perceptions of public sector pharmacists regarding their beliefs, attitudes towards teamwork. Walden Dissertations and Doctoral Studies; 2020. Available from: https://scholarworks.waldenu.edu/dissertations/8407.
25. Adeniji FO. Group-think among health workers; the Nigerian perspective. Researcher. 2010;2(5):1–4.
26. Lorngurum MT, Godowoli AH. The nature of competition and conflicts among healthcare professionals in Nigeria. Nig Hosp Pract. 2008;2(2):42–48. doi:10.4314/nhp.v2i2.41430
27. Mayaki S, Stewart M. Teamwork, professional identities, conflict, and industrial action in Nigerian healthcare. J Multidiscip Healthc. 2020;13:1223–1234. doi:10.2147/JMDH.S267116
28. Ukonu IO, Emerole GA. Conflict management and alternative dispute resolution mechanisms in the health sector: a case of University of Abuja Teaching Hospital. Int J Lit Lang Linguist. 2013;6:51–57.
29. Osaro E, Charles AT. Harmony in health sector: a requirement for effective healthcare delivery in Nigeria. Asian Pac J Trop Med. 2014;7(suppl1):51–55. doi:10.1016/S1995-7645(14)60196-6
30. Omisore AG, Adesoji OR, Abioye-Kuteyi EA. Inter-professionals rivalry in Nigeria’s health sector: a comparison of doctors and other health workers’ views at a secondary care center. Int Q Community Health Educ. 2017;38(1):9–16. doi:10.1177/0272684X17748892
31. Olajide A, Asuzu MC, Obembe T. Doctor-nurse conflict in Nigerian hospitals: causes and modes of expression. Br J Med Res. 2015;9(10):1–12. doi:10.9734/BJMMR/2015/15839
32. Mohammed ENA. Knowledge, causes, and experience of inter-professional conflict and rivalry among healthcare professionals in Nigeria. BMC Health Serv Res. 2022;22(1):320. doi:10.1186/s12913-022-07664-5
33. Streubert HJ, Carpenter DR. Qualitative Research in Nursing: Advancing the Humanistic Imperative.
34. Plager K. Interpretive phenomenology: embodiment, caring, and ethics in health and illness. In: Hermeneutic Phenomenology. Vol. 17. Thousand oaks: Sage; 1994:65–83.
35. Patton MQ. Qualitative Evaluation and Research Methods.
36. Moser A, Kortsjens I. Series: practical guidance to qualitative research. Part 3: sampling, data collection and analysis. Eur J Gen Pract. 2018;24(1):9–18. doi:10.1080/13814788.2017.1375091
37. Mason M. Sample size and saturation in Phd studies using qualitative interviews. Forum Qualitative Research Sozialforschung. Qual Soc Res. 2010;11(3):
38. Longhurst R. Semi-structured interviews and focus groups. In: Clifford N, Cope M, Gillespie T, French S, editors. Key Methods in Geography.
39. Colaizzi PF. Psychological research as the phenomenologist views it. In: Ronald SV, Mark K, editors. Existential-Phenomenological Alternatives for Psychology. Oxford University Press; 1978: 6 Available from: https://philpapers.org/rec/COLPRA-5.
40. Long AH, French DP, Brooks JM. Optimizing the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res Meth Med Health Sci. 2020;1(1):31–42. doi:10.1177/2632084320947559
41. Chinawa AT, Ndu AC, Arinze-Onyia SU, et al. Prevalence of psychological workplace violence among employees of a public tertiary health facility in Enugu, Southeast Nigeria. Niger J Clin Pract. 2020;23(1):103–109. doi:10.4103/njcp.njcp_160_19
42. Olaopa O, Adebayo O, Adufe I, et al. Conflict and conflict resolutions experienced in the Nigerian health sector: a qualitative report. Med Unvi. 2020;3(2):79–85. doi:10.2478/medu-2020-0009
43. Cassels A. Health sector reforms: key issues in less developed countries. J Int Dev. 1995;7(3):329–347. doi:10.1002/jid.3380070303
44. Alenoghena I, Aigbiremolen AO, Abejegah C, Eboreime E. Primary health care in Nigeria: strategies and constraints in implementation. Int J Community Res. 2014;3(3):74–79.
45. Ham C, Clark JM, Spurgeon P, Dickinson H, Armit K. Medical chief executives in the NHS: facilitators and barriers to their career progress. Coventry: Institute for Innovation and Improvement and the Academy of Medical Royal Colleges; 2010. Available from: https://research.birmingham.ac.uk/en/publications/medical-chief-executives-in-The-nhs-facilitators-and-barriers-to-.
46. Badejo O, Sagay H, Seye A, Van Belle S. Confronting power in low places: historical analysis of medical dominance and role-boundary negotiation between health professions in Nigeria. BMJ Glob Health. 2020;5(9):e003349. doi:10.1136/bmjgh-2020-003349
47. Isibor E, Kanmodi K, Adebayo O, et al. Exploring issues and challenges of leadership among early career doctors in Nigeria using a mixed-method approach: CHARTING Study. Eur J Investig Health Psychol Educ. 2020;10(1):441–454. doi:10.3390/ejihpe10010033
48. Berwick MD, Nolan TW. Physicians as leaders in improving healthcare. Ann Intern Med. 1998;128(4):289–292. doi:10.7326/0003-4819-128-4-199802150-00008
49. Alubo O, Hunduh V. Medical dominance and resistance in Nigeria’s health care system. Int J Health Serv. 2016;47(4):778–794. doi:10.1177/0020731416675981
50. Lasebikan OA, Ede O, Lasebikan NN, Anyaehie UE, Oguzie GC, Chukwujindu ED, Job satisfaction among health professionals in a federal tertiary hospital in Nigeria. Niger J Clin Pract. 2020;23:3. 371–375. doi:10.4103/njcp.njcp_292_19
51. Walt G, Gilson L. Reforming the health sector in developing countries: the central role of policy analysis. Health Policy Plan. 1994;9(4):353–370. doi:10.1093/heapol/9.4.353
52. Adeleye OA, Ofili AN. Strengthening intersectoral collaboration for primary health care in developing countries: can the health sector play broader roles? J Environ Public Health. 2010;2010:1–6. doi:10.1155/2010/272896
53. Wald HS. Optimizing resilience and wellbeing for healthcare professions trainees and healthcare professionals during public health crises–Practical tips for an ‘integrative resilience’ approach. Med Teach. 2020;42(7):744–755. doi:10.1080/0142159X.2020.1768230
54. Belrhiti Z, Van-Belle S, Criel B. How medical dominance and inter-professional conflicts undermine patient-centred care in hospitals: historical analysis and multiple embedded case study in Morocco. BMJ Glob Health. 2021;6(7):e006140. doi:10.1136/bmjgh-2021-006140
55. McCoy S, Bennett S, Witter S, et al. Salaries and incomes of health workers in sub-Saharan Africa. Lancet. 2008;371(9613):675–681. doi:10.1016/S0140-6736(08)60306-2
56. Osakede KO, Ijimakinwa SA. The effect of public sector health care workers strike: Nigeria experience. Rev Public Adm Manag. 2014;3(6):154–161.
57. Ogbonayya LU, Ogbonnaya CE, Adeoye-Sunday IM. The perception of health professions on causes of inter-professional conflict in a tertiary health institution in Abakaliki, southeast Nigeria. Niger J Med. 2007;16(2):161–168. doi:10.4314/njm.v16i2.37300
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
