Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Understanding the Health System Conditions Affecting the Use of Long-Acting Injectable Antipsychotics in the Treatment of Schizophrenia in Clinical Practice: A US Healthcare Provider Survey
Authors Zhdanava M, Starr HL , Lefebvre P, Totev TI , Shah A, Sheng K, Pilon D
Received 13 April 2022
Accepted for publication 30 June 2022
Published 22 July 2022 Volume 2022:18 Pages 1479—1493
DOI https://doi.org/10.2147/NDT.S369494
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Maryia Zhdanava,1 H Lynn Starr,2 Patrick Lefebvre,1 Todor I Totev,3 Aditi Shah,1 Kristy Sheng,4 Dominic Pilon1
1Analysis Group, Inc, Montréal, Quebec, Canada; 2Janssen Scientific Affairs, LLC, Titusville, NJ, USA; 3Analysis Group, Inc, Boston, MA, USA; 4Analysis Group, Inc, Menlo Park, CA, USA
Correspondence: Maryia Zhdanava, Analysis Group, Inc, 1190 avenue des Canadiens-de-Montréal, Suite 1500, Montréal, Quebec, H3B 0G7, Canada, Tel +1 514-394-4469, Email [email protected]
Purpose: To describe factors that enable the routine use of long-acting injectable antipsychotics (LAIs) for appropriate patients in the current clinical practice, including changes in LAI prescribing due to the COVID-19 pandemic and expectations for prescribing in 2021 in the United States (US).
Methods: Frequent LAI prescribers recruited from a nationwide panel in 2020 completed an online survey regarding practice characteristics, perspectives on healthcare system conditions enabling routine use of LAIs, and prescribing patterns and changes in patterns during the COVID-19 pandemic.
Results: Of 408 prescribers who completed the survey, 77.7% were physicians and 59.1% had ≥ 10 years of psychiatry practice. More than half of frequent prescribers (57.1%) reported treating > 20% of their patients with schizophrenia with LAIs. The American Psychiatric Association (APA) guideline was followed by 64.0% of prescribers. Most prescribers identified poor adherence to antipsychotics as a circumstance when LAIs are recommended (94.9%) and patient/caregiver involvement in treatment decisions as a key factor impacting the decision to prescribe LAIs (97.3%). Most prescribers reported that LAI prescribing rates were unchanged in 2020 (59.8%). Similar proportions of prescribers expected no change (44.1%) or an increase (42.9%) in LAI prescribing rates in 2021. The number of patients followed, cost of treatment, and availability of staff to administer LAIs were the main driving factors identified by prescribers expecting an increase in LAI prescribing rates.
Conclusion: LAIs were commonly recommended to patients with poor adherence, and patient/caregiver involvement was an important factor affecting prescribers’ treatment decisions. LAI prescribing rates remained unchanged during the COVID-19 pandemic in 2020.
Keywords: COVID-19, healthcare providers, long-acting injectable antipsychotics, prescribing patterns, schizophrenia
Introduction
Schizophrenia is a debilitating, chronic psychiatric disorder characterized by symptoms of delusions and hallucinations.1,2 The annual prevalence of schizophrenia is estimated to range between 0.25% and 0.64% in the United States (US).3–5
Oral antipsychotics (OAPs) are commonly used in routine care for schizophrenia.2,6 However, adherence to medication that requires daily oral administration may be difficult to maintain. Thus, long-acting injectable antipsychotics (LAIs), which are administered biweekly, monthly, or once every few months, have the potential to improve adherence and symptom control and reduce the rate of hospitalizations in patients with schizophrenia compared to OAPs.7–9 Indeed, the 2021 American Psychiatric Association (APA) schizophrenia practice guideline recommends the use of LAIs in patients with a history of nonadherence and by patient choice,2 while the Florida Medicaid guidelines recommend LAIs as the initial treatment after a trial of an OAP monotherapy or among patients who are nonadherent or refractory to initial treatment.10
Despite guideline recommendations and evidence demonstrating improved antipsychotic adherence and symptom control with LAIs vs OAPs,2,10–13 LAIs are infrequently prescribed. Reports indicate that fewer than 20% of patients with schizophrenia are prescribed LAIs in Western countries.14,15 Multiple factors may influence the decision to treat with LAIs vs OAPs, including patient characteristics, preferences, and costs.15,16 For instance, LAI prescription was found to be associated with female sex and younger age in two separate studies of real-world treatment patterns.16,17 Physician and patient perspectives on LAIs may also create barriers to their use.15,18 In a survey-based study of physicians and their patients with schizophrenia in a US community mental health center conducted in 2011–2012, physicians discussed the option of LAIs with only 50% of their patients, notably because they were concerned about potentially damaging the relationship established with their patients.18 Furthermore, patient attitudes toward the option of using LAIs were largely neutral or unfavorable. Additional factors that may influence the utilization of LAIs vs OAPs in clinical practice include costs related to storage, time and effort related to their administration, and the availability of trained healthcare professionals to administer doses.15 Given the high risk of relapse and hospitalization when patients with schizophrenia are nonadherent or inadequately treated,19 removing these barriers to the use of LAIs may reduce the clinical and public health burden associated with the condition.
More recently, the COVID-19 pandemic has challenged care provision for patients with schizophrenia and put certain in-person encounters needed to ensure patients’ stability, such as the administration of LAIs, at risk.20,21 Disruption of continuity of care in schizophrenia and subsequent decompensation may place, in the context of a global pandemic, an additional strain on healthcare systems worldwide, further increasing emergency department visits and hospitalizations and contributing to COVID-19 outbreaks.21 However, the effect of COVID-19 on LAI use may as well have been minimal based on the relatively infrequent administration of LAIs.
Given the evolving guidelines related to LAI use, the role of LAIs in reducing hospitalizations, and the challenges associated with provision of in-person care during the COVID-19 pandemic, there is a need to better evaluate characteristics of healthcare providers and clinical practices enabling the routine use of LAIs for appropriate patients, as well as changes in LAI prescribing due to the COVID-19 pandemic and expectations for prescribing in 2021.
Methods
Data Source
For this descriptive, hypothesis-generating study, de-identified, individual-level data were collected nationwide between November 17, 2020, and December 12, 2020, through an anonymous cross-sectional double-blinded online survey of US-based frequent LAI prescribers (ie, those who treat ≥1 patient with LAIs monthly) via an online panel, which comprised US-based healthcare professionals with a psychiatry specialty. Study participants received a link to the online questionnaire containing 41 questions and a description of the study and were required to provide their informed consent prior to responding to the survey questions.
The survey collected information about the characteristics of participating prescribers, the prescribers’ perspectives on healthcare system conditions enabling routine use of LAIs, and the prescribers’ perspectives on the evolution of LAI prescribing patterns and the conditions that influenced them both during the COVID-19 pandemic and in 2021.
All study materials, including the study protocol and the questionnaire, were approved by the New England Independent Review Board (now WIRB-Copernicus Group Independent Review Board) and the study was granted an institutional review board exemption (#17-1364883-1).
Study Participants
Study participants recruited from a nationwide online panel were screened for the following criteria: (1) had a primary specialty in psychiatry, (2) were prescribed LAIs for the treatment of schizophrenia in the past 12 months, and (3) had ≥1 patient with schizophrenia treated with LAIs in their caseload in an average month (ie, were considered a frequent LAI prescriber). The threshold for identification as a frequent LAI prescriber was determined based on the 50th percentile or higher in the distribution of annual patient days on LAIs per prescriber obtained across all US LAI prescribers in 2019 (data on file).
Statistical Analysis
The responses from the survey were summarized using means, medians, and standard deviations (SDs) for continuous variables and frequencies and proportions for categorical variables. Completed surveys did not contain missing data because answers to all questions were required. All analyses were conducted using SAS Enterprise Guide 7.1 (SAS Institute, Cary, NC).
Subgroup Analysis
Of all the frequent prescribers included in the study, two subgroups were identified. Specifically, the frequent prescribers were stratified based on the proportion of patients with schizophrenia in a monthly caseload who were treated with LAIs: (1) moderately frequent LAI prescribers (ie, those who treated ≤20% of patients with schizophrenia with LAIs) and (2) very frequent LAI prescribers (ie, those who treated >20% of patients with schizophrenia with LAIs). Prescribers who answered “don’t know or unsure” when queried for the percentage of their patients with schizophrenia who were treated with LAIs were excluded from either subgroup.
Results
Characteristics of Frequent LAI Prescribers and Their Clinical Practices
Between November 17, 2020, and December 12, 2020, a total of 408 prescribers (of 648 who viewed the survey) completed the online survey (Table 1). Most of the frequent LAI prescribers were physicians (77.7%), 17.2% were nurse practitioners, and 5.1% were physician assistants. Most frequent LAI prescribers had >10 years of practice in psychiatry (59.1%). Almost all practiced in urbanized areas or urban clusters (92.7%), with the most common clinical settings being community health centers (27.9%), private practices (22.8%), and inpatient units of psychiatric hospitals (15.2%).
 |
Table 1 Characteristics of Frequent LAI Prescribers |
The availability of LAI administration services on site was reported by 71.6% of frequent LAI prescribers; other commonly reported on-site services included counseling (82.1%) and social work/referral services (71.8%). The average time spent with a patient during an encounter (excluding the first encounters) was in the range of 11–30 minutes for 87.8% of frequent LAI prescribers. The prescribers surveyed identified medical staff involved in the care of patients with schizophrenia as including psychiatrists (81.6%), registered nurses (64.0%), social workers (61.8%), psychologists/therapists (55.4%), and nurse practitioners (49.3%).
Psychiatric Caseload of Frequent LAI Prescribers
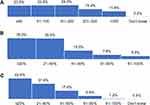
More than two-thirds of frequent LAI prescribers had total monthly psychiatric caseloads of ≤200 patients (71.6%) (Figure 1A) and a subset of patients with schizophrenia in their psychiatric caseload ≤40% (71.5%) (Figure 1B). More than half (57.1%) of frequent LAI prescribers reported treating over 20% of their patients with schizophrenia with LAIs (Figure 1C). In absolute terms, just over half (53.2%) of frequent LAI prescribers treated >10 patients with schizophrenia with LAIs in a given month (Figure 2).
 |
Figure 2 Number of patients with schizophrenia on LAIs in monthly caseload of frequent LAI prescribers per respondents (N = 408). Abbreviation: LAI, long-acting injectable. |
Education on LAI Use
When reporting receiving routine training and/or education on LAI use, 75.7% of prescribers (including physicians, nurse practitioners, and physician assistants) and 60.3% of registered nurses reported receiving frequent training and/or education, while the number of pharmacists, patients or caregivers, social workers, and psychologists or therapists who reported receiving routine LAI training and/or education was lower (Table 2). The prescribers noted their main resources for education on LAI use as online continuing medical education (CME; 79.9%), professional literature (78.9%), and participation in conferences or congresses (58.6%) (Table 2). Frequent LAI prescribers reported using 2.9 resources (SD = 1.3; median = 3.0) on average for ongoing education on LAI use. Of note, 7.4% of prescribers reported that no LAI education was provided at their clinical practice.
 |
Table 2 Training and Education on LAI Use, According to Prescribers |
Specialists identified by prescribers as providing education on LAI use to patients and caregivers were psychiatrists (81.9%), registered nurses (61.3%), and nurse practitioners (45.3%) (Table 2). The main resources and approaches to patient and caregiver education were in-person conversations (78.2%), paper information sheets (59.8%), and website referrals (eg, to advocacy groups; 43.9%) (Table 2).
Schizophrenia Treatment Guidelines Followed by Frequent LAI Prescribers and Their Clinical Practices
Most frequent LAI prescribers reported following the APA practice guideline for the treatment of patients with schizophrenia (64.0%); 53.9% reported that their clinical practice followed this guideline (Figure 3). More than half (52.9%) of prescribers reported that both they and their clinical practice follow the APA schizophrenia practice guideline. About one-quarter of responding prescribers (24.5%) and clinical practices (24.0%) did not follow any formal clinical guidelines when treating patients with schizophrenia (Figure 3).
 |
Figure 3 Schizophrenia treatment guidelines followed by respondents (N = 408). Abbreviations: APA, American Psychiatric Association; NCBH, National Council for Behavioral Health. |
Circumstances in Which Frequent LAI Prescribers Recommended LAIs and Factors Impacting Prescribing of LAI in Eligible Patients
Most frequent LAI prescribers reported poor adherence to antipsychotics as a circumstance when LAIs are recommended in patients with schizophrenia (94.9%) (Table 3). Of note, 87.0% of frequent LAI prescribers reported that adherence to antipsychotics at their clinical practice was measured based on self-reported information from patients and/or caregivers. Other frequently reported circumstances for LAI prescribing included multiple relapses (86.8%), failure of treatment with oral medications (78.2%), and chronic schizophrenia (72.8%). Over one-third of frequent LAI prescribers (36.0%) reported that they recommend use of LAIs in the early stage of schizophrenia (Table 3).
 |
Table 3 LAI Prescribing Patterns and Clinical Practice Characteristics of Frequent LAI Prescribers |
Among patients clinically eligible for LAIs, the key factors impacting the decision to prescribe LAIs were patient and caregiver involvement in treatment decisions (97.3%), prescriber experience with managing adverse events (AEs) related to LAI use (95.8%), and cost of treatment for patients (90.2%) (Figure 4). Of note, 89.2% of the responding prescribers reported inviting patients and caregivers to participate in decisions regarding the best treatment plan.
Collaboration of Frequent LAI Prescribers with Nonprescribing Members of Clinical Teams
More than three-quarters (80.6%) of LAI prescribers reported collaborating with nonprescribing members of the treatment team on schizophrenia treatment plans, including LAI selection (Table 3). Responding prescribers most frequently collaborated with registered nurses (51.7%), social workers (51.2%), psychologists/therapists (46.6%), and pharmacists (34.3%).
Factors Affecting LAI Prescribing During the COVID-19 Pandemic
Most frequent LAI prescribers reported that LAI prescribing rates remained unchanged during the COVID-19 pandemic (59.8%), while 17.6% reported a decrease and 13.7% reported an increase in prescribing rates (Figure 5). Among those who reported that prescribing remained unchanged (n = 244), most identified patient concerns with COVID-19 exposure (56.6%) as a factor impacting the dynamics of LAI prescribing; patient concerns with transportation (45.5%) and staff concerns with COVID-19 exposure (42.2%) were also common responses (Figure 6A). Among those reporting that prescribing decreased (n = 72), most named patient and staff concerns with COVID-19 exposure (55.6% and 45.8%, respectively) as key factors impacting the dynamics of prescribing; facility closure or restricted visits (43.1%) and patient concerns with transportation (43.1%) were also common responses (Figure 6B). Among those reporting that prescribing increased (n = 56), common factors contributing to LAI prescribing dynamics were increased confidence in adherence with LAIs (44.6%) and patient concerns with transportation (44.6%) (Figure 6C).
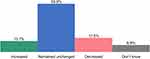 |
Figure 5 Changes in LAI prescribing during the COVID-19 pandemic per respondents (N = 408). Abbreviation: LAI, long-acting injectable. |
Factors Affecting Expected LAI Prescribing in 2021
Similar proportions of frequent LAI prescribers expected no change (44.1%) or an increase (42.9%) in LAI prescribing rates in 2021, while only 3.4% expected a decrease (Figure 7). Among those who expected that prescribing would remain unchanged (n = 180), the cost of treatment for patients (45.0%), followed by clinical staff availability to administer LAIs on site (38.9%), and the number of patients with schizophrenia followed at their clinical practice (37.8%) were cited as common factors impacting the expected dynamics of prescribing (Figure 8A). Among those who reported that prescribing would increase (n = 175), the number of patients with schizophrenia followed at their clinical practice (36.0%), the cost of treatment for patients (36.0%), and clinical staff availability to administer LAIs on site (33.7%) were common factors identified as impacting the expected dynamics of prescribing (Figure 8B). Among the responding prescribers who reported that prescribing would decrease (n = 14), most identified clinical staff availability to administer LAIs on site (57.1%) as a factor impacting the expected dynamics of prescribing (Figure 8C).
 |
Figure 7 Expected changes in LAI prescribing during the next year (2021) per respondents (N = 408). Abbreviation: LAI, long-acting injectable. |
Subgroup Analysis
The subgroups of moderately frequent LAI prescribers included 173 respondents, and the subgroup of very frequent prescribers included 233 respondents. A higher proportion of very frequent (80.7%) relative to moderately frequent (42.2%) LAI prescribers had >20% of patients with schizophrenia in their monthly psychiatric caseload. Higher proportions of very frequent relative to moderately frequent LAI prescribers appeared to work in a community health center (31.3% vs 23.1%) or inpatient unit of a psychiatric hospital (18.5% vs 11.0%) and have LAI administration services (82.8% vs 56.1%) and staff available to inject LAIs (94.8% vs 81.5%) at their clinical practice. Higher proportions of very frequent relative to moderately frequent LAI prescribers appeared to collaborate on schizophrenia treatment plans with registered nurses (60.5% vs 40.5%) and social workers (56.2% vs 45.1%), as well as when prescribing LAIs at a patient’s request (73.8% vs 63.0%) or for early-stage schizophrenia (49.4% vs 17.9%).
In addition, the two subgroups differed both with respect to the perception of change in LAI prescribing during the COVID-19 pandemic and the expected change in 2021. A higher proportion of the very frequent relative to moderately frequent LAI prescribers reported increased LAI prescribing during the COVID-19 pandemic (19.3% vs 6.4%). Very frequent LAI prescribers were also more likely to expect LAI prescribing to increase in 2021 than moderately frequent LAI prescribers (51.1% vs 31.8%).
In terms of education on LAI use, higher proportions of very frequent relative to moderately frequent LAI prescribers reported that registered nurses (69.1% vs 48.0%) and patients or caregivers (24.5% vs 11.6%) received routine training on LAI use at their clinical practices and that registered nurses were involved in educating patients and caregivers on LAI use (69.5% vs 49.7%). Higher proportions of very frequent relative to moderately frequent LAI prescribers reported availability of various resources to educate patients and caregivers on LAIs, specifically, in-person conversations (84.1% vs 69.9%), paper information sheets (68.2% vs 48.6%), website referrals (48.9% vs 37.0%), phone calls (29.6% vs 20.8%), videos (22.3% vs 12.1%), and apps (9.4% vs 3.5%).
Discussion
The existing literature on LAI prescribing in the US has focused on the clinical benefits (eg, lower discontinuation rates and higher number of prescription fills) or reduced healthcare resource utilization (eg, IP admissions, hospital days, and ER visits) associated with LAIs vs OAPs.7,22–24 This study provides additional and timely insights into the characteristics of frequent LAI prescribers and the factors impacting their decision to prescribe LAIs, as well as historic and anticipated changes in LAI prescribing over time due to the impacts of the COVID-19 pandemic. Using the data collected in late 2020 across all US regions, this study reflects a recent treatment landscape for schizophrenia in the US, which evolves as therapeutic guidelines are updated.
In this study, frequent LAI prescribers were predominantly physicians with at least a decade of experience in psychiatry who were routinely trained on LAI use and had LAI administration services available on site at their clinical practice. Over half of these prescribers were treating more than 20% of their patients with schizophrenia with LAIs. To put this finding in context, only 10%–20% of antipsychotic treatment in the US involves LAIs (based on anecdotal reports).14,15
Poor adherence to antipsychotics was reported as a key circumstance for recommending LAIs. This finding is consistent with the current recommendations in the APA guideline,2 which was the most followed guideline among the responding prescribers and their clinical practices. Interestingly, over one-third of frequent LAI prescribers and close to half of very frequent LAI prescribers reported that they also recommend the use of LAIs in the early stage of schizophrenia. While LAIs are typically used in patients with multiple relapses, literature and guidelines are increasingly shifting toward consideration of LAI use earlier in the course of illness to prevent future nonadherence and relapse.2,10
Most frequent prescribers reported recommending LAIs at the patients’ request (69.4%; 73.8% in the very frequent prescriber subgroup). Patient/caregiver involvement in treatment decisions was consistently identified as a top consideration when initiating LAI prescribing in eligible patients, and almost 90% of frequent LAI prescribers reported inviting patients and caregivers to participate in treatment plan decisions in their clinical practice. These findings all suggest that joint decision-making with patients/caregivers has been adopted by the surveyed frequent LAI prescribers. This is in contrast to a prior study by Potkin et al that showed patient/caregiver involvement in 25% of psychiatrist-patient conversations about LAI prescription based on a smaller sample (N = 60) that predominately consisted of prescribers at community mental health centers in 2011–2012.18 Thus, frequent LAI prescribers may place a higher value on patient/caregiver involvement compared to other prescribers, and the importance of this factor in prescribing decisions may have also increased over the past decade. Indeed, because LAI-naïve patients typically express indifferent or negative attitudes towards LAIs,18 patients may become more cooperative and accepting of LAIs when the treatment option is discussed in the context of shared decision-making.2 Eventually, as demonstrated by Pietrini et al, switching adults with stabilized schizophrenia from OAPs to the equivalent LAIs could be associated with significant improvement in patient-reported attitude toward treatment, subjective experience of treatment, and health-related quality of life.25 Taken together, patient education and shared decision-making are of utmost importance for the improvement of patient acceptance of LAIs and, subsequently, clinical outcomes during treatment.
With reduced access to healthcare due to the COVID-19 pandemic starting in 2020, there was concern that patients with schizophrenia would not receive in-person LAI treatment in a timely manner, which could lead to decompensation and relapse.20,21 The majority of the frequent LAI prescribers surveyed reported that their LAI prescribing remained unchanged during the COVID-19 pandemic. This is consistent with a report by Gannon et al, who found that LAI prescribing largely remained stable before and after the implementation of social distancing and COVID-19 restrictions in March 2020 at a Pittsburgh ambulatory clinic.20 Gannon et al cited established rapport between staff and patients and emphasis on the importance of ongoing adherence as key reasons for this lack of workflow and treatment disturbance, further emphasizing the significance of communication between healthcare professionals and patients for LAI prescribing.20 With the limited literature examining the potential impact of global pandemic and shelter-in-place orders on LAI prescribing behaviors, the current findings are encouraging and highlight the perceived value of continuing LAI treatment for patient stability, even during such emergency scenarios. Due to the complexity and unpredictable nature of the ongoing COVID-19 pandemic, further research is warranted to evaluate the changes it introduced to the treatment of patients with schizophrenia, as well as to understand its potential effect on health-related outcomes of patients with schizophrenia.
Limitations
The findings of this study should be interpreted in light of some limitations. First, the analysis of prescriber characteristics, treatment patterns, and historical and anticipated future trends in this study was based on self-reporting by the participating prescribers, which may be subject to recall bias. Second, although attempts were made to minimize selection bias (eg, enrolling a relatively large number of participants from a nationwide panel), there remained a potential for bias given that a healthcare provider’s decision to be on a panel and to contribute time to the survey was not random. Although frequent LAI prescribers from all US geographic regions were included, regions may not have been proportionally captured, so no statements regarding the national representativity of the study findings, or their generalizability to countries outside of the US, can be made. Lastly, due to the timeframe of this study, the results related to the COVID-19 pandemic only covered part of the first year of the pandemic.
Conclusions
Over half of respondents who were frequent LAI prescribers in the US were treating ≥20% of their patients with schizophrenia with LAIs. Poor adherence to antipsychotics was a key circumstance for recommending LAIs, while patient/caregiver involvement in treatment decisions was a top consideration for prescribing LAIs in eligible patients. The majority of the frequent LAI prescribers surveyed reported that their LAI prescribing remained unchanged during the COVID-19 pandemic and expected LAI prescribing to remain unchanged or to increase in 2021. The insights from this study may influence strategies for ensuring routine use of LAIs in eligible patients.
Data Sharing Statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data are not available. Therefore, restrictions apply to the availability of these data, which are not publicly available.
Ethics Approval and Informed Consent
Study participants provided their informed consent prior to responding to the survey questions. All study materials were approved by the New England Independent Review Board (now WIRB-Copernicus Group Independent Review Board).
Acknowledgments
The authors thank the prescribers who participated in this survey. Medical writing assistance was provided by Christine Tam, an employee of Analysis Group, Inc., which provided consulting services to Janssen Scientific Affairs, LLC for the conduct of this study. Sophia Monaghan and Camilo Obando contributed to the study design, data collection, and results interpretation. Pamela Baker contributed to the study design and data collection. Sophia Monaghan was an employee of Janssen Scientific Affairs, LLC. Camilo Obando and Pamela Baker are employees of Janssen Scientific Affairs, LLC and hold stock in Johnson & Johnson. Some data in this manuscript were presented virtually at the Psych Congress 2021, October 29 – November 1, 2021, in San Antonio, Texas, USA.
Funding
This work was supported by Janssen Scientific Affairs, LLC.
Disclosure
Maryia Zhdanava, Patrick Lefebvre, Todor I. Totev, Aditi Shah, Kristy Sheng, and Dominic Pilon are employees of Analysis Group, Inc., a company that provided consulting services to Janssen Scientific Affairs, LLC for the conduct of this study. H. Lynn Starr is an employee of Janssen Scientific Affairs, LLC and holds stock in Johnson & Johnson, Inc. The authors report no other conflicts of interest in this work.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. American Psychiatric Publishing; 2013.
2. American Psychiatric Association (APA). Practice Guideline for the Treatment of Patients with Schizophrenia. American Psychiatric Association (APA); 2021.
3. Desai PR, Lawson KA, Barner JC, Rascati KL. Estimating the direct and indirect costs for community-dwelling patients with schizophrenia. J Pharm Health Services Res. 2013;4(4):187–194. doi:10.1111/jphs.12027
4. Kessler RC, Birnbaum H, Demler O, et al. The prevalence and correlates of nonaffective psychosis in the National Comorbidity Survey Replication (NCS-R). Biol Psychiatry. 2005;58(8):668–676. doi:10.1016/j.biopsych.2005.04.034
5. Wu EQ, Shi L, Birnbaum H, Hudson T, Kessler R. Annual prevalence of diagnosed schizophrenia in the USA: a claims data analysis approach. Psychol Med. 2006;36(11):1535–1540. doi:10.1017/S0033291706008191
6. Kahn RS, Sommer IE, Murray RM, et al. Schizophrenia. Nat Rev Dis Primers. 2015;1:15067. doi:10.1038/nrdp.2015.67
7. Pilon D, Tandon N, Lafeuille M-H, et al. Treatment patterns, health care resource utilization, and spending in Medicaid beneficiaries initiating second-generation long-acting injectable agents versus oral atypical antipsychotics. Clin Ther. 2017;39(10):1972–1985. doi:10.1016/j.clinthera.2017.08.008
8. Pilon D, Muser E, Lefebvre P, Kamstra R, Emond B, Kruti J. Adherence, healthcare resource utilization and Medicaid spending associated with once monthly paliperidone palmitate versus oral atypical antipsychotic treatment among adults recently diagnosed with schizophrenia. BMC Psychiatry. 2017;17(1):207. doi:10.1186/s12888-017-1358-3
9. Alphs L, Benson C, Cheshire-Kinney K, et al. Real-world outcomes of paliperidone palmitate compared to daily oral antipsychotic therapy in schizophrenia: a randomized, open-label, review board-blinded 15-month study. J Clin Psychiatry. 2015;76(5):554–561. doi:10.4088/JCP.14m09584
10. University of South Florida, Florida Medicaid Drug Therapy Management Program sponsored by the Florida Agency for Health Care Administration. 2019-2020 Florida Best Practice Psychotherapeutic Medication Guidelines for Adults. 2020; 1–78. Available from: https://floridabhcenter.org/wp-content/uploads/2021/04/2019-Psychotherapeutic-Medication-Guidelines-for-Adults-with-References_06-04-20.pdf.
11. El Khoury A, Patel C, Huang A, Wang L, Bashyal R. Transitioning from oral risperidone or paliperidone to once-monthly paliperidone palmitate: a real-world analysis among Veterans Health Administration patients with schizophrenia who have had at least one prior hospitalization. Curr Med Res Opin. 2019;35(12):2159–2168. doi:10.1080/03007995.2019.1651129
12. Joshi K, Lafeuille MH, Kamstra R, et al. Real-world adherence and economic outcomes associated with paliperidone palmitate versus oral atypical antipsychotics in schizophrenia patients with substance-related disorders using Medicaid benefits. J Comp Eff Res. 2018;7(2):121–133. doi:10.2217/cer-2017-0043
13. Mental Health Clinical Advisory Group, Oregon Health Authority. Mental Health Care Guide for Licensed Practitioners and Mental Health Professionals. Mental Health Clinical Advisory Group, Oregon Health Authority; 2019.
14. Nasrallah HA. The case for long-acting antipsychotic agents in the post-CATIE era. Acta Psychiatr Scand. 2007;115(4):260–267. doi:10.1111/j.1600-0447.2006.00982.x
15. Parellada E, Bioque M. Barriers to the use of long-acting injectable antipsychotics in the management of schizophrenia. CNS Drugs. 2016;30(8):689–701. doi:10.1007/s40263-016-0350-7
16. Olayinka O, Oyelakin A, Cherukupally K, et al. Use of long-acting injectable antipsychotic in an inpatient unit of a community teaching hospital. Psychiatry J. 2019;2019:8629030. doi:10.1155/2019/8629030
17. Robinson DG, Schooler NR, John M, et al. Prescription practices in the treatment of first-episode schizophrenia spectrum disorders: data from the national RAISE-ETP study. Am J Psychiatry. 2015;172(3):237–248. doi:10.1176/appi.ajp.2014.13101355
18. Potkin S, Bera R, Zubek D, Lau G. Patient and prescriber perspectives on long-acting injectable (LAI) antipsychotics and analysis of in-office discussion regarding LAI treatment for schizophrenia. BMC Psychiatry. 2013;13:261. doi:10.1186/1471-244X-13-261
19. Li G, Keenan A, Daskiran M, et al. Relapse and treatment adherence in patients with schizophrenia switching from paliperidone palmitate once-monthly to three-monthly formulation: a retrospective health claims database analysis. Patient Prefer Adherence. 2021;15:2239–2248. doi:10.2147/PPA.S322880
20. Gannon J, Conlogue J, Sherwood R, et al. Long acting injectable antipsychotic medications: ensuring care continuity during the COVID-19 pandemic restrictions. Schizophr Res. 2020;222:532–533. doi:10.1016/j.schres.2020.05.001
21. Kozloff N, Mulsant BH, Stergiopoulos V, Voineskos AN. The COVID-19 global pandemic: implications for people with schizophrenia and related disorders. Schizophr Bull. 2020;46(4):752–757. doi:10.1093/schbul/sbaa051
22. Lin J, Wong B, Offord S, Mirski D. Healthcare cost reductions associated with the use of LAI formulations of antipsychotic medications versus oral among patients with schizophrenia. J Behav Health Serv Res. 2013;40(3):355–366. doi:10.1007/s11414-013-9329-z
23. Schreiner A, Svensson A, Wapenaar R, et al. Long-acting injectable risperidone and oral antipsychotics in patients with schizophrenia: results from a prospective, 1-year, non-interventional study (InORS). World J Biol Psychiatry. 2014;15(7):534–545. doi:10.3109/15622975.2014.902990
24. Shah A, Xie L, Kariburyo F, Zhang Q, Gore M. Treatment patterns, healthcare resource utilization and costs among schizophrenia patients treated with long-acting injectable versus oral antipsychotics. Adv Ther. 2018;35(11):1994–2014. doi:10.1007/s12325-018-0786-x
25. Pietrini F, D’Anna G, Tatini L, et al. Changes in attitude towards LAI antipsychotic maintenance treatment: a two-year follow-up study. Eur Psychiatry. 2018;53:58–65. doi:10.1016/j.eurpsy.2018.06.002
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.