Back to Journals » Orthopedic Research and Reviews » Volume 14
Ultrasound-Guided Motor-Sparing Knee Blocks for Postoperative Analgesia Following Total Knee Arthroplasty: A Cost Analysis
Authors Sogbein OA , Marsh JD, Somerville LE, Howard JL, Lanting BA
Received 9 February 2022
Accepted for publication 29 June 2022
Published 19 July 2022 Volume 2022:14 Pages 247—253
DOI https://doi.org/10.2147/ORR.S361556
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Olawale A Sogbein,1,2 Jacquelyn D Marsh,1 Lyndsay E Somerville,1 James L Howard,1 Brent A Lanting1
1Division of Orthopaedic Surgery, Department of Surgery, London Health Sciences Centre – University Hospital, London, Ontario, Canada; 2Schulich School of Medicine & Dentistry, Western University, London, Ontario, Canada
Correspondence: Olawale A Sogbein, Tel +1 519-476-1151, Email [email protected]
Background: We recently performed a clinical trial comparing motor sparing blocks (MSB) to periarticular infiltration (PAI) following total knee arthroplasty (TKA). We found that MSBs provided longer analgesia (8.8 hours) than PAI with retention of quadriceps strength, and with similar function, satisfaction, and length hospital stay. However, its potential increased cost could serve as a barrier to its adoption. Therefore, our aim was to compare the costs of MSBs to PAI following TKA.
Methods: We conducted a retrospective review of data from our previous RCT. There were 82 patients included in the RCT (n = 41 MSB group, n = 41 PAI group). We compared the mean total costs associated with each group until hospital discharge including intervention costs, health-care professional service fees, intraoperative medications, length of stay, and postoperative opioid use.
Results: Seventy patients were included (n = 35 MSB group, n = 35 PAI group). The mean total costs for the MSB group were significantly higher ($1959.46 ± 755.4) compared to the PAI group ($1616.25 ± 488.33), with a mean difference of $343.21 (95% CI = $73.28 to $664.11, p = 0.03). The total perioperative intervention costs for performing the MSB was also significantly higher; however, postoperative inpatient costs including length of stay and total opioid use did not differ significantly.
Conclusion: Motor sparing blocks had significantly higher mean total and perioperative costs compared to PAI with no significant difference in postoperative inpatient costs. However, its quadricep sparing nature and previously demonstrated prolonged postoperative analgesia can be used to facilitate an outpatient TKA pathway thereby offsetting its increased costs.
Keywords: costs, total knee arthroplasty, outpatient arthroplasty, adductor canal blocks, periarticular infiltration, motor sparing blocks
Introduction
Total knee arthroplasty remains one of the most successful surgical procedures with the ability to restore a patient’s knee function and alleviate pain once nonoperative modalities have been exhausted. Total knee arthroplasties are associated with a significant amount of postoperative pain which can be problematic resulting in interference with patient’s sleep, mobility, and overall rehabilitation.1 If not adequately controlled, this undoubtedly lengthens a patient’s hospital stay and increases the financial burden on the health-care system.2 As the demand for primary TKAs is projected to grow sixfold by 2030, peripheral nerve blocks have increasingly become an attractive option as they have been shown to reduce postoperative analgesia, result in shorter length of stay, reduce health-care utilization costs, and have been incorporated into outpatient TKA pathways.3–6
Specifically, abductor canal blocks (ACBs) have gained popularity as an attractive option to provide postoperative analgesia, while preserving quadriceps function compared to more traditional techniques.5,7,8 As a result, the patient’s immediate postoperative rehabilitative process is improved. Furthermore, ACBs have been combined with interspace between the popliteal artery and posterior capsule of the knee (IPACK) to provide posterior analgesic coverage.9
We recently performed a randomized clinical trial comparing a single injection adductor canal block combined with IPACK and a lateral femoral cutaneous nerve block (motor sparing block) to PAI, our current standard following TKA. We found that in patients undergoing TKA, the motor sparing block provided longer analgesia (8.8 hours) than PAI with retention of quadriceps muscle strength, and similar function, satisfaction, and length hospital stay.10 However, the increased cost of this intervention could serve as a barrier to its adoption; therefore, evaluation of the additional costs relative to the improvement in outcome is warranted. Our hypothesis was that although motor sparing blocks would be more expensive, the additional cost may be offset by a decreased length of stay and reduced postoperative resource use in an outpatient TKA pathway.
Therefore, the objective of this study was to compare the costs of MSBs to patients who received PAI following TKA.
Materials and Methods
We conducted a retrospective review of patient data from a randomized clinical trial performed from July 2014 to June 2015 at our institution.10 There were 82 patients included in the prospective RCT (n = 41 MSB group, n = 41 PAI group). This study was approved by the Health Sciences Research Ethics Board for Research Involving Human Subjects at Western University, Ontario, Canada. Our study complies with the Declaration of Helsinki.
Inclusion Criteria
Patients aged 18 to 85 years old with American Society of Anesthesiologists (ASA) I, II, or III physical status scheduled to undergo elective primary TKA were included. Patients were recruited from the practices of four fellowship trained orthopaedic surgeons.
Exclusion Criteria
Patients with cognitive impairment, narcotic dependency, extraneous sources of chronic pain, allergies to study drugs, or any contraindications to nerve blocks or multimodal analgesia were excluded. Patients ambulating in a wheelchair, had a language barrier, or were unwilling to provide informed consent were also excluded.
Interventions
Complete details regarding the technical performance of the MSB in the experimental group and PAI in the control group are outlined in our previously published clinical trial.10
Outcome Assessments
The primary outcome was the total costs associated with each group until discharge from hospital. The total cost included the cost of the intervention, in-hospital costs including performing the procedure, health-care professional service fees, intraoperative medications, length of stay, and total postoperative opioid use.
For the MSB group, we collected costs attributed to the materials required to perform the MSB such as the ultrasound, medications, equipment, as well as provider costs including anaesthetist and nursing monitoring. Unit costs were obtained from the case costing department at our institution and health-care professional reimbursement fees were obtained from the Ontario Schedule of Benefits.11 A SonoSite Edge II (Sonosite Inc., Bothell, WA) ultrasound was used during the clinical trial.12 For our institution, its approximate cost is $55,000 with a lifespan of eight years. We calculated the cost of ultrasound per person using an annual estimated caseload of 2000 (primary TKAs, revision TKAs, spinals, other peripheral blocks). The material costs to perform the PAI intraoperatively were also recorded. The costs of knee arthroplasty implants and surgeon fees were excluded from our calculations as they were identical between the groups. We recorded total postoperative hydromorphone and oxycodone consumption and obtained the unit prices for medications using the Ontario Drug Benefit Formulary.13 The unit costs pertaining to study patient’s length of inpatient hospital stay were obtained from our institution. All costs are reported in 2020 Canadian dollars.
We further analyzed and compared the mean total costs until discharge by dividing it into perioperative intervention performance costs and postoperative outcome costs. These were compared between the patient groups. The perioperative intervention performance costs for the MSB included: ultrasound, medications, equipment, and provider costs. These costs for PAI included: medications and equipment. Finally, the postoperative outcome costs included the inpatient length of stay, and total postoperative inpatient opioid medication consumption. These total postoperative outcome costs were also separately compared between patient groups.
Statistical Analysis
Baseline characteristics were summarized with descriptive statistics (mean ± SD for continuous variables, and proportions for nominal variables). Independent t-tests were used to compare the costs between the two groups. Non-normally distributed variables were identified via Shapiro–Wilks test, then compared using the Mann–Whitney U-test. Statistical significance was determined using an a priori alpha level of 0.05. Data analysis was performed using IBM SPSS for Mac OS X, Version 23 (IBM Corp., Armonk, NY, USA).
Results
From July 2014 to March 2015, eighty-two patients were randomized to the MSB or PAI group. Twelve patients were withdrawn after randomization (Figure 1). Therefore, a total of 70 patients were reviewed for the present investigation. Patient demographics and comorbidities were similar between groups (Table 1).
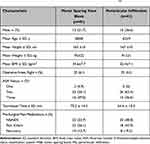 |
Table 1 Baseline Demographics for Patients Undergoing Total Knee Arthroplasty with Either the Motor Sparing Block or Periarticular Infiltration Techniques10 |
 |
Figure 1 Participant flow through the study. Some patients were ineligible for >1 reason. †Patients could be ineligible for multiple reasons. |
The mean total in-hospital cost for the patients who received the motor-sparing block group was significantly higher ($1959.46 ± 755.4) compared with those who received periarticular infiltration group ($1616.25 ± 488.33), with a mean difference of $343.21 (95% CI = $73.28 to $664.11, p = 0.03; Table 2).
 |
Table 2 Calculated Costs for interventions and Postoperative Outcomes for Patients Undergoing Total Knee Arthroplasty with Either the Motor Sparing Block or Periarticular Infiltration Techniques |
The total perioperative intervention cost for performing the motor-sparing block was significantly higher ($227.84± 0.0) than the periarticular infiltration ($17.75± 0.0), with a cost difference of $210.09 (95% CI = 210.09 to 210.09, p = 0.001; Table 2). Finally, there was no significant difference in postoperative costs between MSB ($1731.62± 755.4) and PAI patients ($1598.5± 488.3), with a mean cost difference of $133.12 (95% CI = 143.01 to 460.9, p = 0.39; Table 2).
Discussion
This study compared perioperative and inpatient postoperative costs of patients who underwent TKA with either MSB or PAI. Overall, the mean total inpatient cost for patients who received the MSB was significantly higher than the PAI group with a mean cost difference of approximately $343.21 CAD per patient. Specifically, perioperative performance of the MSB was significantly more expensive than our institution’s standard of PAI with a mean cost difference of $210.09 CAD. However, inpatient postoperative costs did not differ significantly between groups.
There has been a steady trend of reduced hospital length of stay following nearly all surgical procedures over the last two decades. This has undoubtedly stemmed from increasing pressures on hospitals to reduce costs in addition to the development of enhanced recovery protocols, improved surgical technology, and more effective analgesia.3 With increasing health-care expenditures, the emphasis and implementation of outpatient (same day discharge) TKA through fast-track pathways has increased.14 However, two common barriers to early discharge are inadequate pain control and limited mobility, both heavily influenced by the analgesic plan.3
When we previously investigated our MSB protocol, an increased duration of analgesia of approximately nine hours was found postoperatively compared to our control group.10 Furthermore, quadriceps function was retained with no differences in time to or distance walked on first mobilization between the MSB and control groups. Jenstrup et al performed the first randomized clinical trial demonstrating that patients who received adductor canal blocks had faster mobilization tests and decreased pain with knee flexion up to 24 hours.5 Similarly, in Eccles et al trial, patients who received a combination of ACB and IPACK had shorter length of stay, ambulated further on postoperative day zero, and required less narcotic consumption compared to patients who received femoral and sciatic nerve blocks following TKA.9 Kim et al reported significantly lower NRS pain scores on postoperative day zero ambulation and less opioid consumption in patients receiving a combination of ACB, IPACK, and modified PAI compared to their control group following TKA.7 The literature has supported our findings and demonstrated the advantages of adductor canal blocks with improved pain control and function in the immediate postoperative following TKA.15,16 As such, we believe our intervention can potentially be used as an analgesic modality in outpatient pathways.
In Canada between 2018 and 2019, 75,345 knee arthroplasties were performed which represented a volume increase of 22.5% compared to five years earlier.17 The current median length of stay for hip and knee arthroplasty in Canada is three days with the vast majority of patients requiring at least one overnight hospital stay.17,18 Since these procedures instill a significant economic burden on the health-care system especially with an aging population, outpatient joint arthroplasty is an evolving avenue to reduce costs globally. A systematic review of outpatient arthroplasty found similar complication rates between inpatient and outpatient groups with lower costs in the latter. However, a moderate to high amount of bias in most studies included in this review was reported.14
Our analysis showed that performing the MSB was associated with significantly increased costs, however given its advantageous and potential use in outpatient pathways these costs may be offset. Costs associated with outpatient TKA pathways have been previously described. Lovald et al investigated and compared outpatient to standard-stay TKA showing a sizeable reduction in costs of approximately $8527 USD at two years follow-up.19 In Canada, Huang et al compared costs between same day discharge and inpatient TKA. They demonstrated savings of 30% of the inpatient costs which was approximately $3100 CAD per patient with majority of savings coming from inpatient pharmacy costs, physiotherapy, meals, and surgical floor care.20 Similarly, Marsh et al performed a retrospective study evaluating in-hospital costs in their patients following TKA. They demonstrated significant inpatient cost savings with a mean total cost for their early discharge group (26.5 hours postoperatively) of $649.62 ± $281.71 versus $1279.71 ± $515.98 for their standard care group (48.9 hours postoperatively) with no differences in patient reported outcomes.21 Although in hip arthroplasty, Bertin reported a mean cost of $19,021.24 USD for outpatient THA versus $23,087.38 USD for inpatient THA and Aynardi et al found a mean cost of $24,529 USD in outpatient THA versus $31,327 USD in inpatient.2,11 As such, we believe the increased expenditures to implement the MSB (approximately $343 CAD) would be significantly outweighed by the financial benefits associated with its facilitation of outpatient TKA.
The increased costs associated with MSB were largely due to the ultrasound. For our analysis, we estimated this cost based on the value and lifespan of the machine relative to the annual caseload of patients for which it would be used. Therefore, the cost per patient for performing the MSBs would be greater in institutions with smaller caseloads. However, given the substantial cost savings that may be achieved with an outpatient model (approximately $2500 CAD when comparing the mean inpatient and outpatient TKA costs reported by the Canadian Joint Replacement Registry and Huang et al) it is still likely that the additional ultrasound cost per patient would be offset by the cost savings realized in an outpatient model.17,20 However, a smaller institution would have to take their case loads into account.
This study has limitations which stem from its retrospective design. The accuracy of our cost estimates is intimately linked to the quality of our available institutional data reported in our case costing department. Furthermore, the institutional cost of the ultrasound is difficult to estimate and generalize given the various models available, multiple uses by practitioners, and differing hospital contracts. However, we believe our cost estimation is accurate in a high-volume arthroplasty center with an established peripheral block program. We solely focused on perioperative and inpatient costs associated with MSBs. However, it is important to note that important post discharge expenses such as time away from employment, prescription medications, and home-based physiotherapy were not captured in our investigation. This study focused on inpatient costs calculated from outcomes collected and reported in our previous clinical trial. Therefore, limitations outlined in our previous publication would apply to this current investigation as well.10 Finally, future clinical trials are warranted to evaluate the overall cost-effectiveness of MSBs as part of an outpatient TKA pathway in comparison to the current standard of care.
Conclusion
This study revealed that the mean total inpatient and perioperative costs for patients who received the MSB was significantly higher than the PAI group following TKA. However, inpatient postoperative costs did not differ significantly between groups specifically. Given the quadricep sparing nature and extended analgesia provided postoperatively by the MSB, this intervention is potentially conducive to an outpatient TKA pathway leading to overall cost savings.
Data Sharing Statement
No further data will be shared.
Acknowledgment
We would like to acknowledge the primary author’s thesis work. https://ir.lib.uwo.ca/etd/3193/
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
Dr James L Howard reports grants, personal fees from DePuy, and personal fees from Stryker, Smith and Nephew, personal fees from Intellijoint, personal fees from Sanofi, outside the submitted work. Dr Brent A Lanting reports PI, consultant and institutional support from DePuy, Smith and Nephew and Stryker. The authors report no other conflicts of interest in this work.
References
1. Chaumeron A, Audy D, Drolet P, Lavigne M, Vendittoli PA. Periarticular injection in knee arthroplasty improves quadriceps function knee. Clin Orthop Relat Res. 2013;471:2284–2295. doi:10.1007/s11999-013-2928-4
2. Bertin KC. Minimally invasive outpatient total Hip arthroplasty: a financial analysis. Clin Orthop Relat Res. 2005:154–163. doi:10.1097/01.blo.0000157173.22995.cf
3. Cullom C, Weed JT. Anesthetic and analgesic management for outpatient knee arthroplasty. Curr Pain Headache Rep. 2017;21:1–6. doi:10.1007/s11916-017-0623-y
4. Ilfeld BM, Mariano ER, Girard PJ, et al. A multicenter, randomized, triple-masked, placebo-controlled trial of the effect of ambulatory continuous femoral nerve blocks on discharge-readiness following total knee arthroplasty in patients on general orthopaedics wards. Bone. 2011;23:1–7. doi:10.1016/j.pain.2010.05.028.A
5. Jenstrup MT, Jæger P, Lund J, et al. Effects of Adductor-Canal-Blockade on pain and ambulation after total knee arthroplasty: a randomized study. Acta Anaesthesiol Scand. 2012;56:357–364. doi:10.1111/j.1399-6576.2011.02621.x
6. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision Hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg - Ser A. 2007;89:780–785. doi:10.2106/JBJS.F.00222
7. Kim DH, Beathe JC, Lin Y, et al. Addition of infiltration between the popliteal artery and the capsule of the posterior knee and adductor canal block to periarticular injection enhances postoperative pain control in total knee arthroplasty: a randomized controlled trial. Anesth Analg. 2019;129:526–535. doi:10.1213/ANE.0000000000003794
8. Shah NA, Jain NP. Is continuous adductor canal block better than continuous femoral nerve block after total knee arthroplasty? Effect on ambulation ability, early functional recovery and pain control: a randomized controlled trial. J Arthroplasty. 2014;29:2224–2229. doi:10.1016/j.arth.2014.06.010
9. Eccles CJ, Swiergosz AM, Smith AF, Bhimani SJ, Smith LS, Malkani AL. Decreased opioid consumption and length of stay using an IPACK and adductor canal nerve block following total knee arthroplasty. J Knee Surg. 2019;1. doi:10.1055/s-0039-1700840
10. Sogbein OA, Sondekoppam RV, Bryant D, et al. Ultrasound-guided motor-sparing knee blocks for postoperative analgesia following total knee arthroplasty. J Bone Jt Surg - Am. 2017;99:1274–1281. doi:10.2106/JBJS.16.01266
11. Aynardi M, Post Z, Ong A, Orozco F, Sukin DC. Outpatient surgery as a means of cost reduction in total hip arthroplasty: a case-control study. HSS J. 2014;10(3):252–255. doi:10.1007/s11420-014-9401-0
12. SonoSite. Sonosite Edge II – FujiFilm; n.d..
13. Ontario drug benefit formulary/comparative drug index; n.d. Available from: https://www.formulary.health.gov.on.ca/formulary/.
14. Pollock M, Somerville L, Firth A, Lanting B. Outpatient total Hip arthroplasty, total knee arthroplasty, and unicompartmental knee arthroplasty: a systematic review of the literature. JBJS Rev. 2016;4:1–15. doi:10.2106/JBJS.RVW.16.00002
15. Kuang M-J, Xu L-Y, Ma J-X. Adductor canal block versus continuous femoral nerve block in primary total knee arthroplasty: a meta-analysis. Int J Surg. 2016;31:17–24. doi:10.1016/j.ijsu.2016.05.036
16. Perlas A, Kirkham KR, Billing R, et al. The impact of analgesic modality on early ambulation following total knee arthroplasty. Reg Anesth Pain Med. 2013;38:334–339. doi:10.1097/AAP.0b013e318296b6a0
17. Canadian Institute for Health Information. Hip and Knee Replacements in Canada, 2018–2019. Canada: Canadian Joint Replacement Registry; 2018.
18. Zomar BO, Sibbald SL, Bickford D, et al. Implementation of outpatient total joint arthroplasty in Canada: where we are and where we need to go. Orthop Res Rev. 2020;12:1–8. doi:10.2147/ORR.S239386
19. Lovald ST, Ong KL, Malkani AL, et al. Complications, mortality, and costs for outpatient and short-stay total knee arthroplasty patients in comparison to standard-stay patients. J Arthroplasty. 2014;29:510–515. doi:10.1016/j.arth.2013.07.020
20. Huang A, Ryu JJ, Dervin G. Cost savings of outpatient versus standard inpatient total knee arthroplasty. Can J Surg. 2017;60:57–62. doi:10.1503/cjs.002516
21. Marsh J, Somerville L, Howard JL, Lanting BA. Significant cost savings and similar patient outcomes associated with early discharge following total knee arthroplasty. Can J Surg. 2019;62:20–24. doi:10.1503/cjs.002118
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
