Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Triglyceride-Glucose Index is Related to Carotid Artery Plaque in Railway Workers: A Cross-Sectional Study
Authors Pan J, Yang B, Wang Z, Tang L, Jia P, Yang S, Zeng H
Received 23 April 2023
Accepted for publication 16 August 2023
Published 24 August 2023 Volume 2023:16 Pages 2561—2571
DOI https://doi.org/10.2147/DMSO.S418358
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Jia Pan,1,* Bo Yang,1,* Zihang Wang,2 Lei Tang,1 Peng Jia,3,4 Shujuan Yang,1,2,4 Honglian Zeng1
1Department of Clinical Medical College & Affiliated Hospital of Chengdu University, Chengdu University, Chengdu, Sichuan, People’s Republic of China; 2Department of West China School of Public Health and West China Fourth Hospital, Sichuan University, Chengdu, Sichuan, People’s Republic of China; 3Department of School of Resources and Environmental Sciences, Wuhan University, Wuhan, People’s Republic of China; 4Department of International Institute of Spatial Health Epidemiology (ISLE), Wuhan University, Wuhan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Shujuan Yang; Honglian Zeng, Email [email protected]; [email protected]
Aim: China has the highest rail transportation density in the world. Compared to other occupational populations, railway workers in China face increased risk of chronic non-communicable diseases. This study aims to investigate the relationship between the triglyceride-glucose (TyG) index and carotid artery plaque (CAP) in a population of railway workers in southwest China.
Methods: The cross-sectional study was conducted among 3169 railway workers who were categorized into four groups based on TyG index quartiles. The presence of CAP was assessed using carotid Doppler ultrasound. Logistic regression and restricted cubic spline analyses were used to estimate the association between TyG index and CAP, and subgroup analyses were performed based on age, blood pressure, metabolic dysfunction-associated fatty liver disease (MAFLD), smoking, drinking, and physical activity.
Results: Participants with higher TyG index quartiles had a higher prevalence of CAP, with 11.63%, 14.11%, 20.20%, and 18.56% from the first to fourth quartile, respectively. The multi-adjusted logistic regression models showed a positive association between TyG index and the risk of CAP (odds ratio [OR]: 1.22, 95% confidence interval [CI]: 1.06– 1.41) when treated as a continuous variable. When analyzed as a categorical variable with increasing TyG index tertiles, the risk of CAP substantially increased with ORs (95% CIs) of 1.22 (0.90– 1.65) for the second quartile, 1.70 (1.27– 2.28) for the third quartile, and 1.46 (1.08– 1.98) for the fourth quartile compared to the lowest quartile. Restricted cubic spline revealed that the association gradually strengthened with the increase of the TyG index below 9.56.
Conclusion: TyG index was significantly associated with CAP, notably in populations with elevated quartiles of TyG index among railway workers. Monitoring the TyG index could be a useful risk management strategy for CAP in occupation population.
Keywords: TyG index, insulin resistance, carotid artery plaque, MAFLD, occupational population
Introduction
China has the highest rail transportation density in the world,1 leading to a heavy workload for railway workers. Compared to other occupational populations, railway workers in China face increased mental stress, longer working hours, poorer sleep quality, less physical activity, and circadian rhythm disorders. These factors can increase the risk of chronic non-communicable diseases such as dysglycemia, dyslipidemia, and carotid artery plaque (CAP).2
CAP, measured through ultrasound, is a non-invasive and simple method for assessing the risk of early atherosclerosis and cardiovascular disease (CVD).3 Recent evidence suggests that the presence of CAP may be linked to insulin resistance (IR), thereby increasing the risk of atherosclerotic cardiovascular disease (ASCVD).4–6 The triglyceride glucose (TyG) index, a cost-effective and innovative surrogate for IR, is derived from fasting triglyceride (TG) and fasting blood glucose (FBG) measurements.7,8 Several studies have linked the TyG index to chronic noncommunicable diseases, such as type 2 diabetes and metabolic syndrome, as well as early markers of ASCVD, such as intima-media thickness and arterial stiffness.9–11 However, there is limited evidence on the association between CAP and the TyG index, with inconsistent results.12,13 Additionally, few studies have examined this relationship among railway workers, who often have unhealthy lifestyles and irregular work schedules.
In this cross-sectional study based on a large sample of railway workers in southwest China, we aim to investigate the association between the TyG index and CAP and assess how specific lifestyle factors may have modified this relationship. The findings of our study may help in understanding the impact of the TyG index on the risk of CAP in occupational populations and promoting strategies for preventing ASCVD.
Materials and Methods
Study Design and Population
This cross-sectional study was conducted among 3169 railway workers in southwest China from January to December 2021.
The inclusion criteria were all on-job railway drivers. Participants with insufficient clinical information (eg, fasting blood glucose and blood lipid) and severe systemic disease (such as cardiac, renal or liver failure, and malignant) were excluded. A flowchart of the participants’ recruitment is shown in Figure 1.
 |
Figure 1 Flowchart of the participants’ recruitment. |
Data Collection
Body mass index (BMI) (kg/m2) was calculated based on the participants’ height and weight. The participants were then categorized into two groups based on their BMI: BMI < 23 kg/m2, indicating underweight or normal weight, and BMI ≥ 23 kg/m2, indicating overweight or obese. Blood pressure was measured using sphygmomanometers in the seated position, and the average of two readings was recorded for systolic blood pressure (SBP) and diastolic blood pressure (DBP). Hypertension was defined as high blood pressure (SBP ≥140 mmHg or DBP ≥90 mmHg), a previous diagnosis, or the use of antihypertensive medications.
Fasting blood samples were taken after an overnight fast of 8 to 12 hr, and laboratory analysis was conducted on total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), fasting blood glucose (FBG), and high-sensitivity C-reactive protein (hs-CRP) by a laboratory physician at Clinical Medical College & Affiliated Hospital of Chengdu University. FBG levels ≥7.0 mmol/L, a previous diagnosis, or the use of hypoglycemic medications were used to determine diabetes. Dyslipidemia was defined as a self-reported history or use of lipid-lowering medications or TC levels ≥5.17 mmol/L or TG levels ≥1.69 mmol/L or LDL-C levels ≥3.62 mmol/L or HDL-C level ≤1.04 mmol/L.
The TyG index was calculated using the following formula: Ln[(fasting TG (mg/dl) × FBG (mg/dl)/2].8
Digital ultrasonic diagnostics were utilized to evaluate the presence or absence of CAP (EPIQ CX, Philips Ultrasound Inc., USA). The common carotid artery, the carotid artery bulb, and the near and far wall portions of the internal carotid artery were bilaterally imaged. Two physicians with over 5 years of expertise in vascular ultrasound imaging blindly examined the images. The CAP was described by the Mannheim criteria14 as a focal zone invading the arterial lumen by at least 0.5 mm, >50% of the surrounding intima-media thickness values, or a thickness of 1.5 mm above the distance between the lumen-intima and the media–adventitia interface.
Covariates
The TyG index and CAP confounders selected by previous studies were potential factors in our analysis.13,15,16 Our skilled physicians collected sociodemographic and personal medical history (diabetes, hypertension, hyperlipidemia, medication history) and lifestyle factors (smoking status, drinking status, dietary pattern, physical activity, etc.) using a standard questionnaire. Smoking status was defined as smoking at least one cigarette per day, and drinking status was defined as consuming at least 50g of alcohol once every week for at least 6 months. Physical activity was evaluated based on the total metabolic equivalent (MET) score and categorized into two groups (≥3000 MET min/w, <3000 MET min/w).17 According to the standard questionnaire, dietary patterns were assessed according to the consumption of vegetables, fruits, red meat (such as pork, beef, lamb), white meat (such as poultry, fish), and preserved foods.18 The frequency categories for these five items were recorded as follows: “never” = 0, “less than once per week” = 0.5, “2–3 times per week” = 2.5, “4–6 times per week” = 5, and “once or more daily” = 7. The participants’ median scores for each item were calculated, and the individual score ≥median of the vegetable, fruit, and white meat options were assigned 1 score, and the individual score ≤median of the red meat and preserved food options were assigned 1 score. The total diet score ranged from 0 to 5, with one point assigned for each nutritional component that was deemed beneficial. Poor diet (score of 0 or 1), intermediate diet (score of 2 or 3), and ideal diet (score of 4 or 5) were categorized into three groups. The individuals’ self-reported daily salt intake was categorized into three groups: low, moderate, and high intakes.
Metabolic dysfunction-associated fatty liver disease (MAFLD) was also considered a subgroup in our study. The proposed criteria for a diagnostic diagnosis of MAFLD were hepatic steatosis detected by ultrasound picture and one of the following three criteria: overweight/obesity, the presence of type 2 diabetes mellitus, or evidence of metabolic dysregulation.19
Statistical Analysis
According to the previous study, the prevalence of CAP in the general Chinese population was about 20.15%.19 Assuming 80% power, a 2-sided α error of 0.05, and the allowable error was 3%; finally, we obtained a sample size of 687. Considering a dropout rate of 20%, we decided on a minimal sample size of 825. The sample size of this study has reached this standard.
The tertiles of the TyG index were used to divide participants into four categories. Continuous variables were described as the mean (SD) and analyzed by ANOVA test. Multiple regression models were employed to estimate the associations between TyG and CAP risk after adjusting age, SBP, DBP, BMI, physical activity, smoking, drinking, salt intake, and dietary pattern. ROC curves were plotted for different models in predicting CAP. When the TyG index was considered as a continuous variable, a restricted cubic spline with three knots at the 10th, 50th, and 95th percentiles of the TyG index is used to analyze the detailed association between the TyG index and CAP. The subgroup analyses were stratified by age, MAFLD, smoking and drinking, physical activity, dietary pattern, sodium intake, and elevated blood pressure. In addition, sensitivity analyses were conducted to assess the robustness of our findings by excluding patients with hypertension, diabetes, and dyslipidemia.
All statistical analyses were conducted in R Studio (Version 4.0.5). A two-sided P < 0.05 was considered statistically significant.
Results
Baseline Characteristics
A total of 3169 subjects were enrolled in the study, with an average age of 49.25 years. Compared with participants in the lowest quartile of the TyG index, those with high quartiles were more likely to have a higher prevalence of diabetes, hypertension, hyperlipidemia, and higher levels of BMI, SBP, DBP, FBG, TC, TG, LDL-C, AST, ALT, SUA, hs-CRP, and a lower level of HDL-C. Among railway workers, the prevalence of hepatic steatosis, MAFLD, and CAP were 51.78%, 50.87%, and 511 16.12%, respectively. The detailed characteristics of the participants stratified by TyG index quartiles are presented in Table 1.
 |
Table 1 General Characteristics of the Study Participants According to the TyG Index |
The rate of hepatic steatosis detected by hepatic steatosis index (HSI) is shown in Supplementary Table 1.
Association Between the TyG Index and CAP
When the TyG index was treated as a continuous variable, the multivariate adjusted logistic regression models showed that TyG index was associated with the increased risk of CAP (OR: 1.22, 95% CI: 1.06, 1.41) after adjustment for age, SBP, DBP, BMI, physical activity, smoking, drinking, salt intake, and dietary pattern (Table 2). When using the quartiles of the TyG index, the risk of CAP increased with higher ORs in quartile 2 (OR: 1.22, 95% CI: 0.90, 1.65), quartile 3 (OR: 1.70, 95% CI: 1.27, 2.28), and quartile 4 (OR: 1.46, 95% CI: 1.08, 1.98).
 |
Table 2 Association Between the TyG Index and CAP |
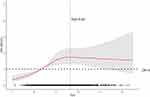
In addition, restricted cubic spline was also used to examine the association between the TyG index and CAP (Figure 2), which revealed that the association was gradually strengthened with the increase of the TyG index below 9.56.
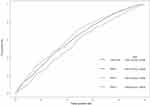
For our study population, we constructed a ROC curve for different models to predict CAP (Figure 3). Model 1 was adjusted age, SBP, DBP, model 2 added BMI based on model 1, and model 3 added physical activity, smoking, drinking, salt intake, dietary pattern based on model 2. Compared with other models, model 3 with added lifestyle increased AUC in CAP detection (AUC = 0.642, 95%Cl 0.617, 0.667).
Subgroup Analysis
The subgroup analysis was stratified by age, SBP, DBP, BMI, smoking, drinking, and physical activity. We found a significant positive association between the TyG index and CAP in different subgroups after adjustment for age, SBP, DBP, BMI, physical activity, smoking, drinking, salt intake, and dietary pattern. Since blood pressure and BMI were included in the assessment of MAFLD, we only made adjustments for age and lifestyle for the MAFLD subgroup in order to prevent collinearity in the statistical analysis. The results showed that TyG index was still correlated with carotid plaque. However, we did not find a modification effect by age, MAFLD, blood pressure, smoking, drinking, and physical activity (P for interaction >0.05). When considering the TyG index in quartiles, we observed that TyG at quartile 3 was strongest associated with risk of CAP, compared with other quartiles among different subgroups (Table 3).
 |
Table 3 Subgroup Analysis for Association Between the TyG Index and CAP |
The results of MAFLD subgroups as determined by HSI are shown in Supplementary Table 2.
Sensitivity Analysis
Sensitivity analyses were performed to assess the association between the TyG index and CAP by excluding participants with hypertension, diabetes, and dyslipidemia. After adjusting for age, SBP, DBP, BMI, physical activity, smoking, drinking, salt intake, and dietary pattern, the sensitivity analysis results were still robust (Table 4).
 |
Table 4 Sensitivity Analysis for Association Between the TyG Index and CAP After Excluding Participants with Hypertension, Diabetes, Dyslipidemia |
Discussion
This study contributes novel findings on the association of the TyG index with CAP among railway workers in southwest China. The primary finding of the present study is that TyG index was significantly associated with CAP, a notable feature in populations with elevated quartiles of TyG index. Furthermore, this relationship was confirmed in various subgroups based on age, smoking, drinking, physical activity, blood pressure, and MAFLD.
The finding that the TyG index is a predictor of atherosclerosis is significant because it suggests that the TyG index could be a useful tool for identifying individuals at higher risk for developing CVD. A case–control study from Taipei revealed that the TyG index could predict the intima-media thicknesses of common carotid arteries.20 This association between the TyG index and atherosclerosis has been demonstrated in multiple populations, including those with hypertension and diabetes.12,13,21 To the best of our knowledge, this is the first study to demonstrate this relationship between the TyG index and CAP in occupational population. Atherosclerosis can be evaluated in many ways, and previous studies have been performed using ankle-brachial pulse wave velocity, carotid-femoral pulse wave velocity, ankle-brachial index, and arterial stiffness.22,23 Although CAP is regarded as an early lesion of atherosclerosis, few studies have examined the relationship between the TyG index and CAP, and the results have been contradictory.12,13,16,24 A study indicated that the TyG index was associated with a high risk of arterial stiffness in elderly adults, but not CAP.24 Our results are in line with some other studies.13,16 There are many factors affecting the relationship between TyG and CAP. However, the prior study’s regression models did not take into account the risk factors like dietary pattern and physical activity. Moreover, scientific evidence demonstrates that lifestyle factors, such as good physical activity and dietary pattern, can successfully improve CVD.25,26 In this study, after adjusting for a number of potential confounders and performing additional sensitivity analysis excluding patients with diabetes, hypertension, and dyslipidemia, the results of this study remained stable.
In addition, our optimal cutoff point for the TyG index in the case of CAP was 9.56, which was higher than the cutoff point determined by other studies (7.9).13 This may be due to differences in the study populations. As one of the most prevalent metabolic diseases, MAFLD, a novel concept presented by an international consensus in 2020, was mostly associated with IR and as a risk factor for CVD; additionally, the TyG index was a potential risk factor for MAFLD.27–31 Subgroup analysis of MAFLD was not performed in prior studies. Results from this study showed that the TyG index was associated with an increased risk of CAP in individuals with MAFLD, suggesting that MAFLD may amplify the influence of the TyG index on the risk of CAP. A recent study revealed that people with MAFLD had an elevated risk of ASCVD relative to those without MAFLD.30 Thus, our findings might provide clinical implications for subjects with MAFLD. Two considerations may explain the likely mechanism of association between the TyG index and CAP. Firstly, IR as measured by the TyG index is related to a reduction in atherosclerosis-promoting shear stress in the carotid artery.32 Secondly, IR can promote inflammation, oxidative stress, lipohyaline deposition, and metabolic alterations, resulting in inflammation-related damage to the endothelium.33,34
There were some limitations in the study. Firstly, this study was a cross-sectional study. Therefore, caution should be taken in making causal interpretations between the TyG index and CAP. Additional prospective research was required to determine the association in the occupational population. Secondly, due to the occupational features of railway workers, the vast majority of male participants limited the applicability of our findings to females. Thirdly, even though the results have been adjusted for a number of significant confounding variables, there are still a number of other uncollected variables, such as more clinical parameters (eg, waist circumference, apolipoprotein B, etc.) and detailed information about the disease (eg, different hypoglycemic medications, the progression of hypertension, diabetes, hyperlipidemia, etc.). Therefore, additional research on this population is absolutely necessary to gather these confounding factors.
Conclusion
TyG index was significantly associated with CAP, notably in populations with elevated quartiles of TyG index among railway workers. Monitoring the TyG index could be a useful risk management strategy for CAP in occupation population.
Abbreviations
ASCVD, Atherosclerotic cardiovascular disease; BMI, Body mass index; CAP, Carotid artery plaque; CVD, Cardiovascular disease; DBP, Diastolic blood pressure; FBG, Fasting blood glucose; HDL-C, High-density-lipoprotein cholesterol; hs-CRP, High-sensitivity C-reactive protein; IR, Insulin resistance; LDL-C, Low-density-lipoprotein cholesterol; MAFLD, Metabolic dysfunction-associated fatty liver disease; MET, Metabolic equivalent; SBP, Systolic blood pressure; TC, Total cholesterol; TG, Triglyceride; TyG, Triglyceride-glucose.
Data Sharing Statement
The datasets used and/or analyzed in this study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
All individuals participated in the survey voluntarily and their informed consent was obtained. This study was in accordance with the principles of the Declaration of Helsinki and approved by the Ethics Committee of Clinical Medical College & Affiliated Hospital of Chengdu University (Grant number: No. PJ 2019-015-02).
Acknowledgments
Jia Pan and Bo Yang are co-first authors of this study. We are particularly grateful to the participants. We also thank all staff involved in this study for their painstaking efforts in conducting the data collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Regional Innovation Cooperation Program of Science and Technology Commission Foundation of Sichuan Province (2021YFQ0031), the Chengdu Technological Innovation Research and Development Project (2021-YF05-00886-SN), and the Sichuan University-Dazhou Cooperation Project (2020CDDZ-26).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Jiang Y, Wu C, Hu T, et al. Association for combined exposure to job strain, shift work on mental health among Chinese railway workers: a cross-sectional study. BMJ Open. 2020;10(10):e037544. doi:10.1136/bmjopen-2020-037544
2. Dong C, Zeng H, Yang B, Zhang Y, Li Z. The association between long-term night shift work and metabolic syndrome: a cross-sectional study of male railway workers in southwest China. BMC Cardiovasc Disord. 2022;22(1):263. doi:10.1186/s12872-022-02705-7
3. Nguyen-Thanh HT, Benzaquen BS. Screening for subclinical coronary artery disease measuring carotid intima media thickness. Am J Cardiol. 2009;104(10):1383–1388. doi:10.1016/j.amjcard.2009.07.005
4. Kozakova M, Natali A, Dekker J, et al. Insulin sensitivity and carotid intima-media thickness: relationship between insulin sensitivity and cardiovascular risk study. Arterioscler Thromb Vasc Biol. 2013;33(6):1409–1417. doi:10.1161/ATVBAHA.112.300948
5. Pané A, Conget I, Boswell L, et al. Insulin resistance is associated with preclinical carotid atherosclerosis in patients with type 1 diabetes. Diabetes Metab Res Rev;2020. e3323. doi:10.1002/dmrr.3323
6. Di Pino A, DeFronzo RA. Insulin resistance and atherosclerosis: implications for insulin-sensitizing agents. Endocr Rev. 2019;40(6):1447–1467. doi:10.1210/er.2018-00141
7. Hong S, Han K, Park CY. The insulin resistance by triglyceride glucose index and risk for dementia: population-based study. Alzheimers Res Ther. 2021;13(1):9. doi:10.1186/s13195-020-00758-4
8. Park K, Ahn CW, Lee SB, et al. Elevated TyG index predicts progression of coronary artery calcification. Diabetes Care. 2019;42(8):1569–1573. doi:10.2337/dc18-1920
9. Khan SH, Sobia F, Niazi NK, Manzoor SM, Fazal N, Ahmad F. Metabolic clustering of risk factors: evaluation of Triglyceride-glucose index (TyG index) for evaluation of insulin resistance. Diabetol Metab Syndr. 2018;10:74. doi:10.1186/s13098-018-0376-8
10. Miao M, Zhou G, Bao A, et al. Triglyceride-glucose index and common carotid artery intima-media thickness in patients with ischemic stroke. Cardiovasc Diabetol. 2022;21(1):43. doi:10.1186/s12933-022-01472-1
11. Won KB, Park GM, Lee SE, et al. Relationship of insulin resistance estimated by triglyceride glucose index to arterial stiffness. Lipids Health Dis. 2018;17(1):268. doi:10.1186/s12944-018-0914-2
12. Wang A, Tian X, Zuo Y, Zhang X, Wu S, Zhao X. Association between the triglyceride-glucose index and carotid plaque stability in nondiabetic adults. Nutr Metab Cardiovasc Dis. 2021;31(10):2921–2928. doi:10.1016/j.numecd.2021.06.019
13. Wang A, Li Y, Zhou L, et al. Triglyceride-glucose index is related to carotid plaque and its stability in nondiabetic adults: a cross-sectional study. Front Neurol. 2022;13:823611. doi:10.3389/fneur.2022.823611
14. Touboul PJ, Hennerici MG, Meairs S, et al. Mannheim carotid intima-media thickness and plaque consensus (2004–2006–2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc Dis. 2012;34(4):290–296. doi:10.1159/000343145
15. Wu Z, Wang J, Li Z, et al. Triglyceride glucose index and carotid atherosclerosis incidence in the Chinese population: a prospective cohort study. Nutr Metab Cardiovasc Dis. 2021;31(7):2042–2050. doi:10.1016/j.numecd.2021.03.027
16. Li Z, He Y, Wang S, et al. Association between triglyceride glucose index and carotid artery plaque in different glucose metabolic states in patients with coronary heart disease: a RCSCD-TCM study in China. Cardiovasc Diabetol. 2022;21(1):38. doi:10.1186/s12933-022-01470-3
17. Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi:10.1249/01.MSS.0000078924.61453.FB
18. Wang M, Zhou T, Song Q, et al. Ambient air pollution, healthy diet and vegetable intakes, and mortality: a prospective UK Biobank study. Int J Epidemiol. 2022;51:1243–1253. doi:10.1093/ije/dyac022
19. Song P, Xia W, Zhu Y, et al. Prevalence of carotid atherosclerosis and carotid plaque in Chinese adults: a systematic review and meta-regression analysis. Atherosclerosis. 2018;276:67–73. doi:10.1016/j.atherosclerosis.2018.07.020
20. Alizargar J, Bai CH. Comparison of carotid ultrasound indices and the triglyceride glucose index in hypertensive and normotensive community-dwelling individuals: a case control study for evaluating atherosclerosis. Medicina. 2018;54(5). doi:10.3390/medicina54050071
21. Park HM, Lee HS, Lee YJ, Lee JH. The triglyceride-glucose index is a more powerful surrogate marker for predicting the prevalence and incidence of type 2 diabetes mellitus than the homeostatic model assessment of insulin resistance. Diabetes Res Clin Pract. 2021;180:109042. doi:10.1016/j.diabres.2021.109042
22. Wu Z, Zhou D, Liu Y, et al. Association of TyG index and TG/HDL-C ratio with arterial stiffness progression in a non-normotensive population. Cardiovasc Diabetol. 2021;20(1):134. doi:10.1186/s12933-021-01330-6
23. Lambrinoudaki I, Kazani MV, Armeni E, et al. The TyG index as a marker of subclinical atherosclerosis and arterial stiffness in lean and overweight postmenopausal women. Heart Lung Circ. 2018;27(6):716–724. doi:10.1016/j.hlc.2017.05.142
24. Zhao S, Yu S, Chi C, et al. Association between macro- and microvascular damage and the triglyceride glucose index in community-dwelling elderly individuals: the Northern Shanghai Study. Cardiovasc Diabetol. 2019;18(1):95. doi:10.1186/s12933-019-0898-x
25. Farinha C, Santos H, Serrano J, et al. The impact of aquatic exercise programs on the intima-media thickness of the carotid arteries, hemodynamic parameters, lipid profile and chemokines of community-dwelling older persons: a randomized controlled trial. Int J Environ Res Public Health. 2022;19(6):3377. doi:10.3390/ijerph19063377
26. Starmans-Kool MJ, Stanton AV, Xu YY, McG Thom SA, Parker KH, Hughes AD. High dietary salt intake increases carotid blood pressure and wave reflection in normotensive healthy young men. J Appl Physiol. 2011;110(2):468–471. doi:10.1152/japplphysiol.00917.2010
27. Liu Z, He H, Dai Y, et al. Comparison of the diagnostic value between triglyceride-glucose index and triglyceride to high-density lipoprotein cholesterol ratio in metabolic-associated fatty liver disease patients: a retrospective cross-sectional study. Lipids Health Dis. 2022;21(1):55. doi:10.1186/s12944-022-01661-7
28. Song K, Park G, Lee HS, et al. Comparison of the triglyceride glucose index and modified triglyceride glucose indices to predict nonalcoholic fatty liver disease in youths. J Pediatr. 2022;242:79–85.e71. doi:10.1016/j.jpeds.2021.11.042
29. Beran A, Ayesh H, Mhanna M, et al. Triglyceride-glucose index for early prediction of nonalcoholic fatty liver disease: a meta-analysis of 121,975 Individuals. J Clin Med. 2022;11(9):2666. doi:10.3390/jcm11092666
30. Han E, Lee YH, Lee JS, et al. Fibrotic burden determines cardiovascular risk among subjects with metabolic dysfunction-associated fatty liver disease. Gut Liver. 2022;16:786–797. doi:10.5009/gnl210290
31. Eslam M, Sanyal AJ, George J. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020;158(7):1999–2014.e1991. doi:10.1053/j.gastro.2019.11.312
32. Tripolino C, Irace C, Scavelli FB, et al. Triglyceride glucose index and common carotid wall shear stress. J Investig Med. 2014;62(2):340–344. doi:10.2310/JIM.0000000000000043
33. Li W, Liu T, Qian L, et al. Insulin resistance and inflammation mediate the association of abdominal obesity with colorectal cancer risk. Front Endocrinol. 2022;60(13):983160. doi:10.3389/fendo.2022.983160
34. Dong R, Chen J, Zheng J, et al. The role of oxidative stress in cardiometabolic risk related to phthalate exposure in elderly diabetic patients from Shanghai. Environ Int. 2018;121(Pt 1):340–348. doi:10.1016/j.envint.2018.09.028
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.