Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Trends of Over-the-Counter and Prescribed Medication Use During Pregnancy: A Cross-Sectional Study
Authors Alyami AA, Alem MM, Dorgham SR, Alshamandy SA
Received 12 May 2023
Accepted for publication 16 October 2023
Published 5 December 2023 Volume 2023:16 Pages 3847—3856
DOI https://doi.org/10.2147/JMDH.S421087
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Amal A Alyami,1 Manal M Alem,2 Shereen R Dorgham,3 Sahar A Alshamandy4
1Obstetrics & Gynecology Hospital, King Saud Medical City, Riyadh, Saudi Arabia; 2Department of Pharmacology, College of Clinical Pharmacy, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia; 3Department of Nursing Education, College of Nursing, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia; 4Obstetrics and Women’s Health Nursing Department, College of Nursing, Minia University, Minya, Egypt
Correspondence: Manal M Alem, Department of Pharmacology, College of Clinical Pharmacy, Imam Abdulrahman Bin Faisal University, PO Box 1982, Dammam, 31441, Saudi Arabia, Email [email protected]
Background: Globally, unjustified medication use during pregnancy, a critical phase in human life, is a threat that compromises the safety of both, the mother and the child. We aim to investigate the prevalence of over-the-counter (OTC) or non-prescription and prescription medication use during pregnancy in women from the city of Riyadh, Saudi Arabia, the level of prior knowledge, and the sources of their information about medication hazard/safety.
Methods: A cross-sectional study was performed using a self-administered questionnaire for 287 pregnant women visiting King Saud Medical City (KSMC) – outpatient departments for routine antenatal care during 3 months (1st Mar– 31st May 2021). The questionnaire was developed by Navaro et al with 4 sections: socio-demographic data, medication use during pregnancy, level of knowledge, and relevant sources of information.
Results: The participants had a mean age of 32.21 years ± 6.41 (SD), and gestational age of 23.67 weeks ± 8.47. About 76.66% of them reported using medication during their current pregnancy: predominantly prescribed (86.36%). Women who used medication during pregnancy were slightly older; the mean difference was 1.97 years (95% CI 0.23– 3.71) (P=0.027). Women living in an urban environment as compared with rural had a higher prevalence of medication use (79.01% vs 52%) (P=0.002). Overall, 58.19% reported using non-prescribed medications during pregnancy, with analgesics as the most frequently used class (70.30%). The mild nature of the illnesses and availability of an old prescription and information from pharmacists were the main reasons for self-medication. About 40.77% denied receiving any information about medication use during pregnancy.
Conclusion: The prevalence of the medication use during pregnancy in our population is alarmingly high. Analgesics were the most frequently used. Lack of adequate information from treating physicians appears to be contributory to self-medication during this critical time.
Keywords: nursing, antenatal care, pregnancy care, prescription medication, non-prescription medications, over-the-counter, fetal health and development, self-medication
Introduction
Drug dispensing is subject to different regulations in different countries, creating differences in legal status and product control. A medical prescription with instructions from the treating physician is needed for dispensing prescription medications, while over-the-counter (OTC) medications or non-prescription medications can be dispensed by the pharmacist to treat common conditions such as fever, pain, cough and cold, allergies, heartburn, and diarrhea or constipation.1 Women might need to take medications from “both categories” during pregnancy for pre-existing medical conditions and/or newly developing illnesses. Scattered studies have shown that a large percentage of pregnant women receive prescription medications other than vitamins or minerals.2 The use of OTC (non-prescription) medications during pregnancy is an important and additional health concern, but little research has been done and the patterns of use are unknown.
Before the thalidomide and diethylstilbestrol tragedies, the discovery that cortisone was teratogenic in the offspring of pregnant mice in 1951 raised awareness about possible teratogenicity in humans.3 Accordingly, any drug that has the capacity to pass through the placenta to the developing fetus imposes a significant threat.4 Despite public attention and the FDA (and other authorities) publishing the latest labeling for prescription drugs and biological products in humans,5 gaps remain about the safety of OTC and prescription medications in pregnancy. Accordingly, precautionary measures and restrictions need to be imposed by local authorities to limit the unjustified and potentially harmful use of medications during pregnancy.
In Saudi Arabia, very few studies have assessed the use of medications during pregnancy; the first study showed that a 40% of women used prescription and non-prescription medications during pregnancy and that, despite frequent physician input, the information obtained about medication use in pregnancy was inadequate.6 A second study reported a slightly smaller figure of 32% use of OTC (non-prescription) medication use during pregnancy but with pharmacists as the main source of information.7 A third study reported that 29% of women would avoid prescribed medications in pregnancy: this obviously raises concerns about non-compliance for serious underlying health conditions.8 In this study, we surveyed the use of OTC (non-prescription) and prescription medications during pregnancy, assessed the knowledge, and explored sources of information.
Methods
Design and Setting
A cross-sectional study that was conducted at the obstetrics and gynecology outpatient departments in King Saud Medical City (KSMC), a public hospital and one of the largest tertiary care centers in Riyadh, the capital of Saudi Arabia. A convenient sample of 287 women was enrolled during the study period (1st Mar–31st May, 2021).
Inclusion criteria were pregnant women visiting KSMC-outpatient departments for routine antenatal care at any gestational age. Pregnant women who were hospitalized were excluded. The reporting system of this study was in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.9
Tool
Data were collected via a self-administered structured questionnaire as developed by Navaro et al.10 The questionnaire consisted of 4 sections to record the followings:
- Socio-demographic data, gestational age, medical as well as obstetric history (11 questions).
- Medication use during pregnancy: OTC (non-prescribed) and prescribed (5 questions). Patients were allowed to choose multiple answers from the medication groups listed, as well as from reasons for their use.
- Level of knowledge regarding the potential consequences of medication use during pregnancy (4 questions). Multiple answers were allowed in this section.
- Sources of information regarding medication use during pregnancy and willingness to learn more (4 questions). Multiple answers were allowed in this section.
Validity & Reliability
The self-administered structured questionnaire used was developed by Navaro et al.10 Following the translation of the questionnaire to Arabic (Supplement 1), the tool has been assessed for the face and content validity by 3 experts: an obstetrics and gynecology nursing specialist, a pharmacology specialist, and an Arabic language specialist. A pilot study was conducted on 10% of the participants (excluded from the study sample), to assess the clarity and applicability and to allow the necessary modifications to be made. Furthermore, the tool was tested twice for its reliability (test–retest reliability) in two different weeks. The obtained value of Cronbach’s alpha test coefficient was 0.87.
Ethical Approval
The study protocol was reviewed and approved by Imam Abdulrahman bin Faisal University Institutional Review Board (IRB) (PGS-2021-04-092), as well as King Saud Medical City, IRB (H1RI-14-Mar 21–01). The study was conducted in accordance with the ethical principles in the Declaration of Helsinki (2013), the ICH Harmonized Tripartite Good Clinical Practice Guidelines, and the laws of Saudi Arabia. An informed written consent was obtained from all participants, and the questionnaire was given after explaining to each woman by the researchers the purpose of the study, data protection, and privacy.
Statistical Analysis
Summary statistics were presented with mean ± SD for continuous data, and numbers and percentages for categorical data. Associations between trend of medication use, knowledge, and sources of information with demographic and other characteristics of the participants were tested by Chi-square test of association. Binary logistic regression model was used to determine predictors of medication use during pregnancy and reported as odds ratios (OR) and 95% confidence intervals (CIs). Predictors included were as follows: age, educational level, living residence and co-morbid conditions. Primary/secondary education, rural residence, and lack of co-morbidities were used as reference groups. All statistical analyses were performed using Minitab 18 (Minitab Inc., State College, PA, USA). A value of p˂0.05 was considered statistically significant.
Sample Size Calculation
The prevalence of use of prescription and non-prescription medications during pregnancy, which was reported in a previous study from another region of Saudi Arabia was 40%,6 while the expected number of pregnant women visiting the outpatient departments in KSMC during the study period was 1000 women. Therefore, this study required a sample size of 270 participants in order to detect the prevalence with a 95% confidence level and 5% margin of error.
Results
Demographic and Obstetric Information
A total of 287 pregnant women participated in the study with a mean age of 32.21 years ± 6.41 (SD). The participants were predominantly Saudi nationals (269, 93.73%), married (267, 93.03%), and living in urban areas (262, 91.29%). Educational status was high with a university degree or equivalent in 166 participants (57.84%), but only 95 were in employment (33.10%). Their obstetric history showed that 35 women (12.20%) were in their first trimester, 135 (47.04%) in the second, and 117 (40.77%) in the third (Table 1). Number of previous pregnancies were in order of frequency; 1–2 (136 women; 47.39%), 3–4 (107; 37.28%), 5–6 (32; 11.15%), ≥7 (11; 3.83%), and none (1; 0.35%).
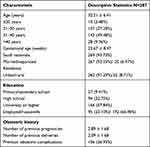 |
Table 1 Demographic and Obstetric Data of Study Population |
No history of obstetric complications was reported by 181 women (63.07%), while 106 women reported the following; miscarriages (68, 23.69%), intrauterine fetal death (5, 1.74%), stillbirth (5, 1.74%), premature deliveries (5, 1.74%), multiple complications (23, 8.01%) (Table 1). Comorbid conditions were reported by 56 women (19.51%) and most frequently attributed to diabetes mellitus (18 patients, 6.27%), hypertension (8, 2.79%), bronchial asthma and other allergies (7, 2.44%), and rheumatoid arthritis (2, 0.70%).
Medication Use During Pregnancy
A total of 220 women (76.66%) reported that they had used medications during the current pregnancy: predominantly those prescribed by a treating physician (190 women, 86.36%) but OTC (non-prescribed) in 30 women (13.64%), dispensed with the help of a pharmacist (Figure 1A). Significant relationships between medication use during the current pregnancy and the demographic and obstetric characteristics of the participants showed women who had used medications during pregnancy were slightly older (32.67 years ± 6.39 vs 30.70 ± 6.27) (P=0.027). The prevalence of medication use among the studied women during the current pregnancy was higher in those with co-morbid conditions (52 participants, 92.86%) as compared to those without (168 participants, 72.73%) (P=0.001) and higher in those coming from urban areas (207 participants, 79.01%) as compared to those coming from rural areas (13 participants, 52%) (P=0.002).
In general, 167 women (58.19%) reported using non-prescribed medications during pregnancy (Table 2), along with the reported reasons behind this trend. In summary, analgesics in 116 women (70.30%), cough and cold remedies in 47 (28.48%), antiemetic drugs in 41 (24.85%), and laxatives in 33 (20%), respectively. The most frequent justifications for using non-prescribed medications were the mild nature of the illness, the availability of an old prescription, and advice from a pharmacist (Table 2 and Figure 1B).
 |
Table 2 Non-Prescribed Medications Used in Study Population and the Reported Reasons |
Binary logistic regression model showed that significant predictors of medication use (prescribed and non-prescribed) during the current pregnancy were living in urban residence and presence of co-morbid conditions (OR 4.435, 95% CI 1.736, 11.327) and (OR 5.978, 95% CI 1.951, 18.321), respectively, while the significant predictor of non-prescribed medication use during pregnancy in general was the presence of co-morbid conditions (OR 4.079, 95% CI 1.945, 8.553) (Table 3).
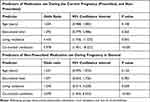 |
Table 3 Binary Logistic Regression Presenting Predictors of Medication Use During Pregnancy |
Knowledge About Medication Use During Pregnancy
A total of 168 women (58.54%) were aware that medication use during pregnancy is potentially harmful and 155 (54.01%) reported that advice from a physician is necessary. Eighty-one women (28.22%) identified that the first trimester of pregnancy is more vulnerable to harm/damage and potential harm was identified at any stage of pregnancy by another 101 (35.19%). The most frequent potential adverse effects on the unborn baby were thought to be visible malformation in subsequent ages (163 women, 56.79%), fetal growth retardation, and intrauterine death (139, 48.43%, and 138, 48.08%), respectively. Corresponding potential effects on the mother were abortion (200 women, 69.69%), followed by uterine contraction and bleeding (152, 52.96% and 136, 47.39%), respectively (Table 4).
 |
Table 4 Knowledge Towards Medication Use During Pregnancy |
Sources of Information
Table 5 lists the responses regarding the sources of information about medication use in pregnancy. While 117 women (40.77%) reported that they received none, the remaining 170 women (59.23%) reported multiple sources, in ranking order: pharmacists, midwives, physicians, and internet-based sources. The medication leaflet was read by 124 women (43.21%) but the majority (256, 89.20%) answered that they needed more information about medication use in pregnancy.
 |
Table 5 Sources of Information |
Discussion
The following are the main findings of this study.
First, although only 20% of the participants had co-morbid conditions, 77% of women used medications during current pregnancy (mostly prescribed).
Second, non-prescribed medications were used by 58% of pregnant women in general, with 70% of those using analgesics.
Third, the justification for taking non-prescribed medications was the mild nature of the illness (61%), followed by the availability of an old prescription and advice from pharmacists (26% and 22%), respectively.
Fourth, Most participants had reasonable knowledge about medication use during pregnancy and their potential harm.
Fifth, 41% of the participants did not receive any information about medication use in pregnancy; those who did receive information had it mainly from pharmacists (39%).
Sixth, 43% of the participants used the medication leaflet as a source of information.
Prevalence Comparisons Nationally and Internationally
The prevalence (77%) of medication use in the current pregnancy in this study was higher than the 40% reported in a previous national study of prescribed and non-prescribed medication in a sample with similar age, education, and employment status, albeit from predominantly rural areas.6 Our prevalence was also higher than that reported in another study from Gulf countries (48%) although in a slightly younger population and with lower educational status.11 However, in USA, the corresponding prevalence of using prescribed and non-prescribed medications during pregnancy was 89%,12 with a pattern rising with maternal age and education. In Europe, the corresponding prevalence of using prescribed and non-prescribed medications during pregnancy was 81%, with a pattern rising with maternal age but with an opposite pattern in relation to education, ie more medication use with less education.13 While we noticed this rising pattern with age in our cohort, the association between educational attainment and medication usage in pregnancy seems complex.10 Other studies have reported prevalences of 60% in Italy,10 82% in Norway,14 and 39% in Ireland.15 The reported prevalence (58%) of using non-prescribed medications during pregnancy in general in our cohort exceeded those of most other populations; 32% in another national study,7 40% in the United Arab Emirates,16 44% in Italy,10 20% in Ireland,15 6% in Serbia,17 but less than 62.8% reported in USA.18
Among the socio-demographic and other factors related to the participants, co-morbid medical conditions at baseline appeared to be the strongest predictor of using medications (prescribed and non-prescribed) during pregnancy. Similarly, this factor was found to be a significant predictor of medication use during pregnancy by Navaro et al10 but not by Cleary et al15 or Odalovic et al.17 Further comparisons with the afore-mentioned studies were not feasible because patients with co-morbidities were excluded from some studies;19 lack of reporting of any co-morbidities in the participants;6 while some reported various co-morbidities (6.4%)16, (37.9%),7 (46.2%)14 but did not explore if they were predictors for medication use during pregnancy. It seems that women with preconception medical problems might be more familiar with taking medications in general and probably have a lower threshold for their use.
Medication Safety
Analgesics were the most frequently used class in our study, and this is in agreement with other studies.6,7,10,11,13,15,16,20,21 Although some analgesics are labeled safe during pregnancy,22 analgesics consumption is a global concern with consumption rates that are rising sharply and associated with developmental defects in the offspring.23,24 Cough and cold remedies come next and include many potential agents with the following risk classification: pseudoephedrine (C), chlorpheniramine (C), guaifenesin (C), and dextromethorphan (C).25 However, risk classification must be cautiously interpreted, as the dose–response curve for the embryo toxic effects of drugs may have a steep slope, moving from minimal to maximum adverse effects only by doubling the dose.26
Self-Medication and Source of Information
In our cohort, the tendency for self-medication was due to the patient’s assessment that the medical problem was mild (and not due to the non-availability of advice from the treating physician). Alternatively, advice was obtained from pharmacists: this is consistent with the limited information in the published literature.7,10 However, other studies have indicated that gynecologists/physicians are the primary sources of information.6,8,10 There is a paucity of data about the pharmacist’s initiative to ask about pregnancy status and the accuracy of the information provided. One local study showed that only 55% of pharmacists asked about the pregnancy status.27 Obstetrics and gynecologists in another study were found to provide different treatment practices between pregnant and non-pregnant patients, with 41% of them prescribing medications during pregnancy without sufficient information about their potential effects on the fetus.28 Another important source of information is the medication leaflet, but only 43% of women read the leaflet in our study; this is lower than other reports: 58%,8 70%,16 86%.6 Overall, the obvious conclusion is that multi-disciplinary collaboration (obstetricians, physicians, pharmacists, and midwives) is required to ensure medication safety in antenatal care.
Study Limitations
Our study has a number of limitations, particularly the small sample size that came from a local community; therefore, generalization of the findings described requires other samples from our population. Ideally, other sub-groups of medications could have been explored; for example, the use of vitamins and minerals as a separate group or the use of herbal medicines since our general population has one of the highest rates of herbal medicine usage.29 The study depends on self-administered questionnaire and that is subject to recall bias by the participants. It was not feasible to study specific medications used from a certain class, the dose used, and at which stage of pregnancy by such tool. Confounding factors such as medication use before pregnancy were not studied that could have predicted medication use during pregnancy.17 Finally, excluding hospitalized women with high-risk pregnancy might have missed another category where rates of medication use would be expected to be very high.
Conclusion
This survey has identified one of the highest prevalence rates for consuming OTC and prescription medication during pregnancy, particularly analgesic drugs. Pregnant patients do not receive adequate information from physicians/obstetricians. Although pharmacists do provide essential information, a significant percentage of women rely on reading medication leaflets as a source of information. In the light of these findings, there is an urgent and obvious need in Saudi Arabia that legislation be put in place to increase awareness in our community and prevent the consumption of unjustified medication during pregnancy.
Relevance to Clinical Practice
This study has demonstrated alarming rates of medication use in the current pregnancy (77%), as well as in pregnancy in general (58%). These rates are higher than those reported in two other local studies in Saudi: 40%6 and 32%.7 They are also higher than several international studies. The finding of this study flags an urgent need for the Saudi local authority to impose more regulations on medication use and design educational programs that target pregnant women.
Ethical Approval
The study protocol was reviewed and approved by Imam Abdulrahman bin Faisal University Institutional Review Board (IRB) (PGS-2021-04-092), as well as King Saud Medical City, IRB (H1RI-14-Mar 21-01). The study was conducted in accordance with the ethical principles in the Declaration of Helsinki (2013), the ICH Harmonized Tripartite Good Clinical Practice Guidelines, and the laws of Saudi Arabia. An informed written consent was obtained from all participants, and the questionnaire was given after explaining to each woman by the researchers the purpose of the study, data protection, and privacy.
Consent for Publication
The authors grant Journal of Multidisciplinary Healthcare the consent to publish the manuscript.
Acknowledgment
We are very grateful to all the patients that kindly participated in our study.
Funding
This research has not been funded by any source.
Disclosure
The authors declare no conflict of interest.
References
1. Taking over-the-counter medicines during pregnancy; 2021. Available from: https://www-uptodate-com.library.iau.edu.sa/contents/taking-over-The-counter-medicines-during-pregnancy-The-basics?search=over-The-counter%20medications%20in%20pregnancy&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1.
2. Andrade SE, Gurwitz JH, Davis RL, et al. Prescription drug use in pregnancy. Am J Obstet Gynecol. 2004;191(2):398–407. doi:10.1016/j.ajog.2004.04.025
3. Fraser FC, Fainstat TD. Production of congenital defects in the off-spring of pregnant mice treated with cortisone; progress report. Pediatrics. 1951;8(4):527–533. doi:10.1542/peds.8.4.527
4. Wilson RD, Sogc Genetics C; Sogc Infectious Disease C. Principles of human teratology: drug, chemical, and infectious exposure. J Obstet Gynaecol Can. 2007;29(11):911–917. doi:10.1016/S1701-2163(16)32668-8
5. Pernia S, DeMaagd G. The new pregnancy and lactation labeling rule. P T. 2016;41(11):713–715.
6. Zaki NM, Albarraq AA. Use, attitudes and knowledge of medications among pregnant women: a Saudi study. Saudi Pharm J. 2014;22(5):419–428. doi:10.1016/j.jsps.2013.09.001
7. Raheel H, Alsakran S, Alghamdi A, Ajarem M, Alsulami S, Mahmood A. Antibiotics and over the counter medication use and its correlates among Arab pregnant women visiting a tertiary care hospital in Riyadh, Saudi Arabia. Pak J Med Sci. 2017;33(2):452–456. doi:10.12669/pjms.332.12376
8. Aljoher AM, Alsaeed MA, AlKhlfan MA, et al. Pregnant women risk perception of medications and natural products use during pregnancy in Alahsa, Saudi Arabia. Egypt J Hospital Med. 2018;70(1):13–20. doi:10.12816/0042956
9. Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4(10):e297. doi:10.1371/journal.pmed.0040297
10. Navaro M, Vezzosi L, Santagati G, Angelillo IF, Collaborative Working G. Knowledge, attitudes, and practice regarding medication use in pregnant women in Southern Italy. PLoS One. 2018;13(6):e0198618. doi:10.1371/journal.pone.0198618
11. Al-Riyami IM, Al-Busaidy IQ, Al-Zakwani IS. Medication use during pregnancy in Omani women. Int J Clin Pharm. 2011;33(4):634–641. doi:10.1007/s11096-011-9517-y
12. Mitchell AA, Gilboa SM, Werler MM, et al. Medication use during pregnancy, with particular focus on prescription drugs: 1976–2008. Am J Obstet Gynecol. 2011;205(1):51 e1–8. doi:10.1016/j.ajog.2011.02.029
13. Lupattelli A, Spigset O, Twigg MJ, et al. Medication use in pregnancy: a cross-sectional, multinational web-based study. BMJ Open. 2014;4(2):e004365. doi:10.1136/bmjopen-2013-004365
14. Smedberg J, Brathen M, Waka MS, Jacobsen AF, Gjerdalen G, Nordeng H. Medication use and drug-related problems among women at maternity wards-A cross-sectional study from two Norwegian hospitals. Eur J Clin Pharmacol. 2016;72(7):849–857. doi:10.1007/s00228-016-2042-0
15. Cleary BJ, Butt H, Strawbridge JD, Gallagher PJ, Fahey T, Murphy DJ. Medication use in early pregnancy-prevalence and determinants of use in a prospective cohort of women. Pharmacoepidemiol Drug Saf. 2010;19(4):408–417. doi:10.1002/pds.1906
16. Abduelkarem AR, Mustafa H. Use of over-the-counter medication among pregnant women in Sharjah, United Arab Emirates. J Pregnancy. 2017;2017:4503793. doi:10.1155/2017/4503793
17. Odalovic M, Vezmar Kovacevic S, Nordeng H, Ilic K, Sabo A, Tasic L. Predictors of the use of medications before and during pregnancy. Int J Clin Pharm. 2013;35(3):408–416. doi:10.1007/s11096-013-9750-7
18. Refuerzo JS, Blackwell SC, Sokol RJ, et al. Use of over-The-counter medications and herbal remedies in pregnancy. Am J Perinatol. 2005;22(6):321–324. doi:10.1055/s-2005-873235
19. Alosaimi AAM, Zamzam SM, Berdida DJE, Villagracia HN. Perceived risks of over-The-counter medication use among pregnant Saudi mothers: a cross-sectional study. J Taibah Univer Med Sci. 2022;17(5):755–764. doi:10.1016/j.jtumed.2022.03.001
20. Werler MM, Mitchell AA, Hernandez-Diaz S, Honein MA. The national birth defects prevention S. Use of over-The-counter medications during pregnancy. Am J Obstet Gynecol. 2005;193(3):771–777. doi:10.1016/j.ajog.2005.02.100
21. Tuha A, Faris AG, Mohammed SA, Gobezie MY. Self-medication and associated factors among pregnant women attending antenatal care at kemisie general hospital, North East Ethiopia. Patient Prefer Adherence. 2020;14:1969–1978. doi:10.2147/ppa.S277098
22. Black RA, Hill DA. Over-The-counter medications in pregnancy. Am Fam Physician. 2003;67(12):2517–2524.
23. Zafeiri A, Mitchell RT, Hay DC, Fowler PA. Over-The-counter analgesics during pregnancy: a comprehensive review of global prevalence and offspring safety. Hum Reprod Update. 2020;27(1):67–95. doi:10.1093/humupd/dmaa042
24. Toda K. Is Acetaminophen safe in pregnancy? Scand J Pain. 2017;17:445–446. doi:10.1016/j.sjpain.2017.09.007
25. Servey J, Chang J. Over-the-counter medications in pregnancy. Am Fam Physician. 2014;90(8):548–555.
26. Fraser FC. Handbook of Teratology.
27. Alrabiah Z, Al-Arifi MN, Alghadeer SM, et al. Knowledge of community pharmacists about the risks of medication use during pregnancy in central region of Saudi Arabia. Saudi Pharmac J. 2017;25(7):1093–1096. doi:10.1016/j.jsps.2017.05.005
28. Morgan MA, Cragan JD, Goldenberg RL, Rasmussen SA, Schulkin J. Management of prescription and nonprescription drug use during pregnancy. J Matern Fetal Neonatal Med. 2010;23(8):813–819. doi:10.3109/14767050903387045
29. Al Akeel MM, Al Ghamdi WM, Al Habib S, Koshm M, Al Otaibi F. Herbal medicines: Saudi population knowledge, attitude, and practice at a glance. J Family Med Prim Care. 2018;7(5):865–875. doi:10.4103/jfmpc.jfmpc_315_17
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

