Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 14
Trends and hospital outcomes of lung transplantation among patients with and without chronic obstructive pulmonary disease in Spain: a national population-based study (2001–2015)
Authors de Miguel-Díez J , López-de-Andres A, Hernández-Barrera V , de Miguel-Yanes JM, Méndez-Bailón M, Jiménez-García R
Received 27 September 2018
Accepted for publication 31 January 2019
Published 27 March 2019 Volume 2019:14 Pages 729—737
DOI https://doi.org/10.2147/COPD.S189010
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Javier de Miguel-Díez,1 Ana López-de-Andres,2 Valentín Hernández-Barrera,2 José M de Miguel-Yanes,3 Manuel Méndez-Bailón,4 Rodrigo Jiménez-García2
1Respiratory Department, Hospital General Universitario Gregorio Marañón, Facultad de Medicina, Universidad Complutense de Madrid (UCM), Instituto de Investigación Sanitaria Gregorio Marañón (IiSGM), Madrid, Spain; 2Preventive Medicine and Public Health Teaching and Research Unit, Health Sciences Faculty, Rey Juan Carlos University, Alcorcón, Madrid, Spain; 3Internal Medicine Department, Hospital General Universitario Gregorio Marañón, Facultad de Medicina, Universidad Complutense de Madrid (UCM), Madrid, Spain; 4Internal Medicine Department, Hospital Universitario Clínico San Carlos, Facultad de Medicina, Universidad Complutense de Madrid (UCM), Madrid, Spain
Purpose: To describe trends from 2001 to 2015 in incidence and in-hospital outcomes of patients suffering or not suffering from COPD who had undergone lung transplantation (LTx) in Spain.
Methods: We used the Spanish National Hospital Discharge Database to select all admissions for LTx. Incidence was estimated overall and according to the presence of COPD. Outcomes included infections, complications, length of hospital stay and in-hospital mortality (IHM).
Results: We identified 2,896 admissions for LTx. Admission rates rose in COPD sufferers and non-COPD sufferers over time, with higher rates among COPD patients. COPD and non-COPD patients were older, but mean age was higher in COPD patients. Although there was a male predominance among patients, the proportion of women significantly increased over time in the COPD population. COPD patients had lower Charlson Comorbidity Index values than non-COPD patients (score ≥1, 25.83% and 31.6%, P<0.05). We observed a significant increase in infections and complications of LTx or rejection for both groups over time. IHM decreased from 2001 to 2015 in both groups of patients. COPD was a predictor of lower IHM (OR 0.75, 95% CI 0.61–0.93) after LTx.
Conclusion: LTx-incidence rates were higher in COPD patients and increased over the study period in both groups. The proportion of women significantly increased over time among COPD sufferers. IHM decreased from 2001 to 2015 in both groups of patients. COPD was a predictor of lower mortality during admissions for LTx.
Keywords: lung transplantation, COPD, hospital admissions, incidence rates, in-hospital mortality, Spain
Background
Lung transplantation (LTx) is the therapeutic option of choice for patients who suffer an end-stage lung disease that would otherwise be fatal.1 Procedures include single and bilateral LTx. In addition, patients who also suffer severe right or left ventricular dysfunction are candidates for heart–lung transplantation.2
Since completion of the first successful LTx in the 1980s, thousands of procedures have been performed worldwide.3–5 This therapeutic modality has been recommended for several respiratory diseases, including patients suffering advanced COPD.6 Depending on the underlying disease and the time spent waiting for the transplant, LTx is effective in improving quality of life and increasing survival.7 Furthermore, advances in lung preservation, surgical techniques, posttransplant patient care, and immunosuppressant therapy during the last three decades have significantly improved outcomes over time.6
COPD is the most common indication worldwide for LTx for several reasons.8 COPD is a very common disease, significant pulmonary hypertension is infrequent, and these patients can survive a long time waiting for a transplant. Furthermore, some anatomical conditions, such as a large pleural cavity, usually free of adhesions, may facilitate LTx for COPD.7
In recent years, approximately a third of all LTxs have been performed for COPD. Bilateral LTx has been used with increasing frequency, and transplantation rates have increased considerably in patients aged ≥60 years, which reflects the increase in the number of LTxs in older patients with this disease.9 Compared with other pulmonary diseases, COPD patients show the best 1-year survival, although lower 10-year survival has been described, perhaps as a consequence of the greater age and prevalence of comorbidities in this group of patients.10 However, studies comparing outcomes during LTx admission in different groups of patients are still needed.
In Spain, since 2006 the Spanish Lung Transplant Registry (SLTR) has collected data on LTx and cooperated with international registries.11–13 Despite these documentation efforts, there is limited information regarding trends in LTxs in Spain in recent years.12 The number of LTx centers in Spain over the study period was eight. The highest annual volume was found in the Hospital Valle de Hebron, with 50–70 LTxs per year. Six centers had LTx figures ranging from 30 to 50, and the lowest number was reported by the Hospital 12 de Octubre: approximately 30 LTxs per year. More details can be found elsewhere.14
To conduct our investigation, we used data in the Spanish National Hospital Discharge Database (SNHDD). The objectives of our study were to assess temporal trends in the incidence of LTx in Spain from 2001 to 2015 among subjects suffering or not suffering from COPD, to describe the clinical characteristics of these two populations, such as comorbidities, complications of the transplanted lung or graft rejections, and posttransplant infections, and to analyze temporal trends in the length of hospital stay (LOHS) and in-hospital mortality (IHM) among COPD and non-COPD patients who had received an LTx.
Methods
For study purposes, we used data in the SNHDD corresponding to each year from 2001 to 2015. The variables and characteristics of the SNHDD have been described elsewhere.15 In the SNHDD, the diagnosis (1–14) and the diagnostic or therapeutic procedures (up to 20) are codified according to the ICD9-CM.
We selected admissions for patients whose medical procedures included LTx, coded as aspecific (33.5, 33.50), single (33.51), or bilateral (33.52) in any procedure field. We included all patients with a hospital admission in Spain from 2001 to 2015 with an ICD9 code for LTx. We grouped admissions by COPD status. We considered those patients with any of the codes 490, 491, 492, 496, 491.0, 491.1, 491.8, 491.9, 492.0, 492.8 and 491.2x, in any diagnostic position, as COPD sufferers and the rest of the patients as non-COPD sufferers.
To assess the presence of comorbidities, we used the Charlson Comorbidity Index (CCI), excluding COPD.16 Irrespective of the position on the diagnosis or procedure coding list, we retrieved data about in-hospital infection events, including pneumonia (997.39, 486), sepsis (995.91, 995.92), surgical-site infection (998.5, 998.51, 998.52, 998.53, 998.54, 998.55, 998.59, 998.50), and urinary tract infection (599.0). We additionally identified complications of transplanted lung or graft rejections (996.84). Therapeutic diagnostic procedures analyzed were noninvasive mechanical ventilation (93.90), invasive mechanical ventilation (96.7, 96.70, 96.71, 96.72), thoracentesis (34.91), pleural drainage–tube insertion (34.0, 34.01–34.09), bronchoscopy (33.21–33.24), red blood–cell transfusion (99.00, 99.01–99.08), hemodialysis (39.95), extracorporeal membrane oxygenation (39.65), and tracheostomy (31.1).
We searched the database for possible infections caused by specific microorganisms with the codes 112.5 for candidiasis, 078.5 for Cytomegalovirus disease, 481 for Streptococcus pneumoniae, 482.1 for Pseudomonas aeruginosa, 482.83 for other Gram-negative bacteria, 482.41 and 482.42 for Staphylococcus aureus, and 117.3 for Aspergillus. We also identified blood cultures (90.5x) and respiratory cultures (90.4x). LOHS was defined as days between hospital admission and discharge. The proportion of patients who died within the hospital after the LTx was the IHM.
Statistical analysis
For study purposes, we divided time into five consecutive periods: 2001–2003, 2004–2006, 2007–2009, 2010–2012, and 2013–2015. The methods used to estimate and analyze trends over time in the incidence rates of LTx for the populations of subjects suffering from COPD and for those patients without this disease have been described previously.17–19 To describe continuous variables, we used mean or median values with SD or IQR as appropriate. For categorical variables, we show proportions. To assess the association of study variables with time periods, we used χ2 for linear trends and the Kruskal–Wallis test.
Multivariate Poisson regression models were constructed to analyze the trends over time in the incidence of LTx among those patients with and without COPD. To identify predictors of IHM, we performed three multivariate logistic regression analyses (COPD population, non-COPD population, and entire population). Stata 10.1 (College Station, TX, USA) was used for statistical analyses, and P<0.05 (two-tailed) was considered significant. According to Spanish legislation, as the study was conducted using a public-access and anonymous database, approval of an ethics committee was not needed.
Results
From 2001 to 2015, we identified 2,896 admissions for LTx in Spain. Over the study period, 39.4% (n=1,142) of all admissions for LTx were performed in patients suffering from COPD.
Incidence and sociodemographic and clinical characteristics
Table 1 shows incidence rates and sociodemographic and clinical characteristics of hospitalized patients according to COPD status who underwent LTx in Spain from 2001 to 2015. The incidence rate of admissions for LTx among COPD patients increased from 3.25 (2001–2003) to 6.48 (2013–2015) cases per 100,000 COPD sufferers (P<0.05). In patients without COPD, the rates also increased: from 0.26 (2001–2003) to 0.43 (2013–2015) cases per 100,000 individuals without COPD. Incidence was significantly higher in COPD than non-COPD sufferers for all the periods analyzed.
Single LTx increased significantly over time in patients with and without COPD (27.78% and 29.77% in 2001–2003 vs 39.81% and 41.73% in 2013–2015, respectively; both P<0.05). However, bilateral LTx decreased significantly in both groups over time (Table 1). As shown in Figure 1, the number of single LTxs rose from 45 in 2001–2003 to 129 in 2013–2015 among patients with COPD and from 78 to 207 among subjects without COPD. This means that the number of single transplants multiplied by 2.87 and 2.65 times from 2001–2003 to 2013–2015, respectively. The number of bilateral transplants among non-COPD patients increased by 1.75 times (111–194) and 1.62 times (174–282) from 2001–2003 to 2013–2015, respectively.
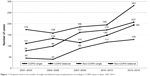  | Figure 1 Temporal trend in the number of single and bilateral lung transplantations according to COPD status in Spain, 2001–2015. |
Among patients who underwent LTx, there were more men than women (74.43% men for COPD and 56.84% men for no COPD). However, among those with COPD, the proportion of women increased from 15.43% in 2001–2003 to 31.17% in 2013–2005 (P<0.001). Over the entire study period, the mean age of COPD patients who underwent LTx was 10 years greater than patients without COPD (55.41±8.6 vs 45.43±16.11 years, P<0.001). COPD patients were significantly older in all the periods analyzed, and for both groups the mean age increased by approximately 4 years from 2001 to 2015. According to the CCI, patients without COPD had more comorbidities than COPD sufferers (P<0.05). Comorbidities increased over time, in addition to COPD status.
The global median LOHS was 34 days in COPD patients and 36 days in non-COPD patients. As shown in Table 1, none of the differences in LOHS between those with and without COPD was statistically significant. IHM was 17.16% for patients with COPD and 21.04% for non-COPD patients (P<0.05). Crude IHM decreased over time from 21.6% to 11.1% among COPD patients and 33.21% to 13.1% among non-COPD LTx patients (P<0.05). The proportion of infections showed a significant increase over time in both groups analyzed, reaching figures for 2013–2015 of 16.36% for COPD and 19.56% for non-COPD patients. Almost 50% of patients undergoing LTx, in addition to COPD status, suffered complications of LTx or graft rejections.
Procedures and pathogen isolations
Table 2 shows procedures used during admission for LTx according to COPD status. In COPD patients, bronchoscopy (56.04%), followed by mechanical ventilation (47.37%), and pleural drainage–tube insertion (22.68%) were the procedures most frequently used. The use of noninvasive mechanical ventilation, bronchoscopy, and extracorporeal membrane oxygenation rose over time in all groups analyzed. However, the use of mechanical ventilation and red blood–cell transfusion showed a significant decrease in the last 15 years when associated with COPD status. In non-COPD patients, the use of thoracentesis and pleural drainage–tube insertion increased significantly over time. Table 3 shows pathogen isolations during admission for LTx according to COPD status. The most commonly found pathogens among COPD sufferers were Aspergillus (5.52%), followed by candidiasis (3.42%), and Cytomegalovirus disease (2.28%). We detected a significant decrease in S. aureus and S. pneumoniae over time in both groups.
COPD versus non-COPD
After applying the Poisson regression model, we obtained an adjusted incidence-rate ratio of 10.64 (95% CI 9.84–12.40) for patients with COPD. This meant that the probability of undergoing an LTx in Spain from 2001 to 2015 was over ten times greater among persons suffering from COPD than among non-COPD subjects.
Predictors of in-hospital mortality
Table 4 shows the results of the multivariate analysis to identify the predictors of IHM after LTx in Spain in 2001–2015. Among all patients who underwent LTx, belonging to the 50- to 59-year-old group (vs <40 years old, OR, 1.35, 95% CI 1.03–1.78) and suffering more comorbidities (vs no comorbidities, OR 1.87, 95% CI 1.53–2.29) were positively associated with IHM. Suffering an in-hospital infection increased the risk of dying within the hospital threefold after an LTx. In either group, patients with and without COPD, IHM significantly decreased during 2001 to 2015. Finally, COPD was a predictor of lower IHM (OR 0.75, 95% CI 0.61–0.93) after LTx.
  | Table 4 Multivariate analysis of factors associated with mortality during hospital admission for lung transplantation in Spain, 2001–2015 |
Discussion
In our investigation, rates of hospitalization for LTx increased significantly from 2001 to 2015 in both COPD and non-COPD subjects. However, incidence was significantly higher in the first group for all the time periods analyzed. In fact, the probability of undergoing a LTx was over ten times greater among COPD subjects than in those without this disease. Coll et al also observed that in Spain from 2006 to 2010, indications for LTx due to COPD progressively increased, while the number of transplants for other indications remained stable.12 However, our results contrast with those found by Yusen et al in the US from 1998 to 2008. They observed that the percentage of patients with COPD undergoing LTx decreased and became stable in 2008, when COPD constituted 20% of the indications for LTx. This is half the proportion that COPD represented at the beginning of the decade.3 On the other hand, idiopathic pulmonary fibrosis as the indication for LTx has increased over time, becoming the most common disease in 2007 and onward. Yusen et al attributed these results to the implementation of the lung-allocation score (LAS) system in 2005. This system prioritized donor-lung allocation based on expected outcome and medical urgency.3 Iribarne et al found that 2 years after the LAS had been initiated, no significant changes in the distribution of indications for LTx were observed.20 However, they observed a decrease in the proportion of patients undergoing LTx for COPD and an increase in those undergoing LTx for idiopathic pulmonary fibrosis.
Our analysis showed that single LTx increased significantly over time, in addition to COPD status, while bilateral transplant decreased significantly in both groups over time. The time trend in the use of single and bilateral LTxs found in our investigation is in line with the results published by the SLTR in the 2016 report, showing that single LTx is becoming more frequently used over time in Spain.14
Single LTx has the advantage of making optimal use of available organs. However, the choice of single or bilateral LTx as the optimal procedure continues to be unclear.21 Although hospital survival seems to be similar for both procedures, bilateral recipients seem to have better long-term survival.7,22 In this regard, long-term outcomes for single LTxs could be inferior because of problems in the native lung (infection, cancer, hyperinflation, pneumothorax). However, in a more recent study, after a 5-year follow-up, no differences were found in survival among patients with COPD who had undergone a single or double LTx.23 In another retrospective analysis conducted in Spain, it was demonstrated that single or double LTx had no impact on patient survival or complications. Implementing single LTx widely may alleviate donor-organ shortages and contribute to decreases in the morbidity and mortality of those patients on the national waiting list.24 Like other authors, we observed a predominance of males in the patients who underwent LTx in Spain.3 However, the proportion of women significantly increased over time among the COPD patients in our study. As described in a recent meta-analysis, the rapid increase over the last few decades in the prevalence COPD among women, as well as the increase in mortality of this group, may justify these results.25 Unlike other authors, we did not find any relationship between female sex and mortality during admissions for LTx.26
LTx-recipient demographics have been changing over time, with patients becoming progressively older. In the same way, the proportion of recipients aged ≥65 years rose over the past decade in the US.3 However, recipients in this age-group have more posttransplant mortality in the first year than younger groups, as well as higher long-term mortality.3 The results of Coll et al agree with these findings, documenting higher 1-year mortality among older recipients.12 Our analysis also showed that IHM was significantly higher in patients aged 50–59 years than those <40 years old.
COPD patients who are considered eligible for LTx suffer fewer concomitant medical conditions than the general COPD population.27 It is possible that COPD patients undergoing LTx had lower CCI scores than those without COPD in our study. Comorbidity rose over the study period in both groups of patients. Furthermore, in addition to COPD status, multivariate analysis demonstrated that the presence of one or more comorbidities was an independent predictor of IHM.
Patients undergoing LTx have an increased risk of infection, due to worsening pulmonary defense mechanisms and the application of immunosuppressant therapies.9 In our investigation, the proportion of infections rose over time in patients with and without COPD, and in-hospital infections were a positive predictor of IHM. In fact, infections have been described as the most frequent cause of perioperative mortality and within the first year post-LTx.12,28 However, we must take into account that the increase in infections and complications over time may well be related to the increase in the number of single LTxs.
Patients who undergo LTx after ventilator or extracorporeal membrane–oxygenation (ECMO) support have decreased survival compared to other recipients.29 Nevertheless, we found an increase over time in the utilization of ECMO and noninvasive mechanical ventilation in patients with and without COPD. However, a recent temporal analysis has suggested that outcomes in these high-risk recipients have improved over time, particularly at high-volume centers.30 Other authors have also found that the increase in centers’ LTx rates is associated with a reduction in 1-year patient mortality.31
In line with the results of other studies, suffering COPD predicted lower mortality during admission for LTx.3,13 We observed a decrease in mortality over time, in addition to the presence or absence of COPD, despite the increase in age, comorbidity, and prevalence of infections over time. Possible reasons for the improvement in IHM over time include modifications in immunosuppressive treatments and better management of comorbidities.
The main strength of our investigation is that we collected information for an entire country over 15 years. Furthermore, the SNHDD was implemented in Spain in 1986, and since then the methodology has remained constant, so the external validity of the data is unquestionable.16–18 However, our study has some limitations. First, we cannot know whether the therapeutic procedures, such as mechanical ventilation, tracheostomy, and ECMO, were performed pre- or post-LTx. This limitation applies to registered infections and other complications. In addition, we were unable to analyze the impact of other variables that may play a role in post-LTx survival. The low rate found for the use of mechanical ventilation may be due to the methodology of the SNHDD. In this database, if a patient is extubated in the first 24 hours after surgery, mechanical ventilation is considered part of the surgical process and not recorded. This means that only patients receiving operation with >1 day on the ventilator have this procedure included in their discharge report.
Second, we also lacked information on transplant numbers for the individual centers in our database. This limitation occurred because of the confidentiality measures the SNHDD database enforces to ensure anonymity, which means that center information has been deleted. Furthermore, as all personal identifiers are also deleted, it is not possible to know the mean number of hospital admissions in survivors after 1, 3, 5, and 10 years, and thus the long-term survival of all groups following discharge is unknown. Finally, the information provided by the SLTR includes overall data, but this information is not stratified by presence of such concomitant conditions as COPD, so these data cannot be compared with our investigation.14 Despite these limitations, our study has addressed major issues related to LTx.
In conclusion, Spanish national data demonstrated that admissions for LTx were higher in patients with COPD than those without COPD, and LTx increased over time in both groups of patients. Although patients were older, the mean age was higher in COPD patients than those without this disease. We observed a male predominance among LTx patients, but the proportion of women significantly increased over time in the COPD population. IHM after LTx decreased over time in both groups analyzed. Remarkably, the presence of COPD was associated with lower mortality during admissions for LTx in our cohort.
Abbreviations list
CCI, Charlson Comorbidity Index; IHM, in-hospital mortality; IPF, idiopathic pulmonary fibrosis; IRR, incidence-rate ratio; LOHS, length of hospital stay; LTx, lung transplantation; SLTR, Spanish Lung Transplant Registry; SNHDD, Spanish National Hospital Discharge Database.
Acknowledgments
This paper was funded by the Fondo de Investigaciones Sanitarias (FIS) – Instituto de Salud Carlos III (ISCIII) and cofinanced by the European Union through the Fondo Europeo de Desarrollo Regional (FEDER, “Una manera de hacer Europa”): grant PI16/00564. The authors would like to thank NeumoMadrid (XVIII Awards Edition, 2018) for grant support.
Disclosure
The authors report no conflicts of interest in this work.
References
Whitson BA, Hayes D Jr. Indications and outcomes in adult lung transplantation. J Thorac Dis. 2014;6:1018–1023. doi:10.3978/j.issn.2072-1439.2014.07.04 | ||
Camargo PC, Teixeira RH, Carraro RM, et al. Lung transplantation: overall approach regarding its major aspects. J Bras Pneumol. 2015;41:547–553. doi:10.1590/S1806-37562015000000100 | ||
Yusen RD, Shearon TH, Qian Y, et al. Lung transplantation in the United States, 1999–2008. Am J Transplant. 2010;10:1047–1068. doi:10.1111/j.1600-6143.2010.03055.x | ||
Yusen RD, Edwards LB, Kucheryavaya AY, et al. The registry of the international society for heart and lung transplantation: thirty-second official adult lung and heart-lung transplantation report–2015; Focus theme: early graft failure. J Heart Lung Transplant. 2015;34:1264–1277. doi:10.1016/j.healun.2015.08.014 | ||
Paraskeva MA, Levin KC, Westall GP, Snell GI. Lung transplantation in Australia, 1986–2018: more than 30 years in the making. Med J Aust. 2018;208:445–450. | ||
Salamo O, Roghaee S, Schweitzer MD, et al. White donor, younger donor and double lung transplant are associated with better survival in sarcoidosis patients. Sci Rep. 2018;8:6968. doi:10.1038/s41598-018-25144-x | ||
Stewart KC, Patterson GA. Current trends in lung transplantation. Am J Transplant. 2001;1:204–210. | ||
Christie JD, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: 29th adult lung and heart-lung transplant report-2012. J Heart Lung Transplant. 2012;31:1073–1086. doi:10.1016/j.healun.2012.08.004 | ||
Todd JL, Palmer SM. Lung transplantation in advanced COPD: is it worth it? Semin Respir Crit Care Med. 2010;31:365–372. doi:10.1055/s-0030-1254076 | ||
Christie JD, Edwards LB, Aurora P, et al. Registry of the International Society for Heart and Lung Transplantation: twenty-fifth official adult lung and heart/lung transplantation report–2008. J Heart Lung Transplant. 2008;27:957–969. doi:10.1016/j.healun.2008.07.018 | ||
Vaquero Barrios JM, Santos Luna F, Salvatierra Velázquez Á. Lung re-transplantation. The opposite view point. Arch Bronconeumol. 2018;54:311–312. doi:10.1016/j.arbres.2018.04.001 | ||
Coll E, Santos F, Ussetti P, et al. The Spanish Lung Transplant Registry: first report of results (2006–2010). Arch Bronconeumol. 2013;49:70–78. doi:10.1016/j.arbres.2012.06.001 | ||
Christie JD, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: twenty-seventh official adult lung and heart-lung transplant report–2010. J Heart Lung Transplant. 2010;29:1104–1118. doi:10.1016/j.healun.2010.08.004 | ||
Organizacion Nacional de transplantes [National Transplants Organization]. Transplante pulmonar [lung transplant]. Available from: http://www.ont.es/infesp/Memorias/Memoria%20Pulm%C3%B3n.pdf. Accessed November 20, 2018. Spanish. | ||
Instituto Nacional de Gestión Sanitaria, Ministerio de Sanidad, Servicios Sociales e Igualdad. Conjunto Mínimo Básico de Datos, Hospitales del INSALUD. Available from: http://www.mscbs.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SolicitudCMBDdocs/Formulario_Peticion_Datos_CMBD.pdf. Accesed March 21, 2018. Spanish. | ||
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. | ||
de Miguel-Díez J, López-de-Andres A, Esteban-Vasallo MD, et al. Clostridium difficile infection in hospitalized patients with COPD in Spain (2001–2015). Eur J Intern Med. 2018;57:76–82. doi:10.1016/j.ejim.2018.06.022 | ||
de Miguel-Díez J, López-de-Andrés A, Hernández-Barrera V, et al. Influence of COPD on outcomes of patients hospitalized with heart failure: analysis of the Spanish National Hospital Discharge Database (2001–2015). Int J Cardiol. 2018;269:213–219. doi:10.1016/j.ijcard.2018.07.067 | ||
de Miguel-Díez J, López-de-Andrés A, Hernández-Barrera V, et al. Impact of COPD on outcomes in hospitalized patients with community-acquired pneumonia: analysis of the Spanish national hospital discharge database (2004–2013). Eur J Intern Med. 2017;43:69–76. doi:10.1016/j.ejim.2017.06.008 | ||
Iribarne A, Russo MJ, Davies RR, et al. Despite decreased wait-list times for lung transplantation, lung allocation scores continue to increase. Chest. 2009;135:923–928. doi:10.1378/chest.08-2052 | ||
Lane CR, Tonelli AR. Lung transplantation in chronic obstructive pulmonary disease: patient selection and special considerations. Int J Chron Obstruct Pulmon Dis. 2015;10:2137–2146. doi:10.2147/COPD.S78677 | ||
Sundaresan RS, Shiraishi Y, Trulock EP, et al. Single or bilateral lung transplantation for emphysema? J Thorac Cardiovasc Surg. 1996;112:1485–1494. | ||
Schaffer JM, Singh SK, Reitz BA, Zamanian RT, Mallidi HR. Single- vs double-lung transplantation in patients with chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis since the implementation of lung allocation based on medical need. JAMA. 2015;313:936–948. doi:10.1001/jama.2015.1175 | ||
Borro JM, Delgado M, Coll E, Pita S. Single-lung transplantation in emphysema: retrospective study analyzing survival and waiting list mortality. World J Transplant. 2016;6:347–355. doi:10.5500/wjt.v6.i2.347 | ||
Ntritsos G, Franek J, Belbasis L, et al. Gender-specific estimates of COPD prevalence: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2018;13:1507–1514. doi:10.2147/COPD.S146390 | ||
Marshall MB, Kohman LJ. Gender and lung transplantation: size matters, does sex? J Thorac Cardiovasc Surg. 2004;128:352–353. doi:10.1016/j.jtcvs.2004.05.014 | ||
Reed RM, Cabral HJ, Dransfield MT, et al. Survival of lung transplant candidates with COPD: BODE score reconsidered. Chest. 2018;153:697–701. doi:10.1016/j.chest.2017.10.008 | ||
Cerón Navarro J, de Aguiar Quevedo K, Mancheño Franch N, Peñalver Cuesta JC, Vera Sempere FJ, Padilla Alarcón J. Complications after lung transplantation in chronic obstructive pulmonary disease. Med Clin (Barc). 2013;140:385–389. doi:10.1016/j.medcli.2012.07.028 | ||
Mason DP, Thuita L, Nowicki ER, Murthy SC, Pettersson GB, Blackstone EH. Should lung transplantation be performed for patients on mechanical respiratory support? The US experience. J Thorac Cardiovasc Surg. 2010;139:765–773.e1. doi:10.1016/j.jtcvs.2009.09.031 | ||
George TJ, Beaty CA, Kilic A, Shah PD, Merlo CA, Shah AS. Outcomes and temporal trends among high-risk patients after lung transplantation in the United States. J Heart Lung Transplant. 2012;31:1182–1191. doi:10.1016/j.healun.2012.07.001 | ||
Scarborough JE, Bennett KM, Davis RD, et al. Temporal trends in lung transplant center volume and outcomes in the United States. Transplantation. 2010;89:639–643. doi:10.1097/TP.0b013e3181ceecf7 |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



