Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Trend Analysis of Palliative Care Utilization in Patients with Chronic Obstructive Pulmonary Disease During Hospitalization from 2007 to 2018 in Taiwan
Authors Kao LT, Ko SC, Chen PJ , Wu YC, Liao KM , Liang YS, Ho CH , Liang FW
Received 13 September 2023
Accepted for publication 10 December 2023
Published 20 December 2023 Volume 2023:18 Pages 3015—3026
DOI https://doi.org/10.2147/COPD.S435954
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Min Zhang
Li-Ting Kao,1 Shian-Chin Ko,2 Ping-Jen Chen,3,4 Yu-Cih Wu,5 Kuang-Ming Liao,6 Yi-Shan Liang,1 Chung-Han Ho,5,7,8 Fu-Wen Liang9– 11
1Department of Respiratory Therapy, Chi Mei Medical Center, Tainan, Taiwan; 2Center for Palliative Care, Chi Mei Medical Center, Tainan, Taiwan; 3Department of Family Medicine and Division of Geriatrics and Gerontology, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan; 4School of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan; 5Department of Medical Research, Chi Mei Medical Center, Tainan City, Taiwan; 6Department of Internal Medicine, Chi Mei Medical Center, Chiali, Tainan, Taiwan; 7Department of Information Management, Southern Taiwan University of Science and Technology, Tainan City, Taiwan; 8Cancer Center, Taipei Municipal Wanfang Hospital, Taipei Medical University, Taipei, Taiwan; 9Department of Public Health, College of Health Sciences, Kaohsiung Medical University, Kaohsiung, Taiwan; 10Department of Medical Research, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan; 11Center for Big Data Research, Kaohsiung Medical University, Kaohsiung, Taiwan
Correspondence: Chung-Han Ho, Department of Medical Research, Chi Mei Medical Center, No. 901, Zhonghua Road Yongkang District, Tainan City, 71004, Taiwan, Tel +886-6-281-2811, Email [email protected] Fu-Wen Liang, Department of Public Health, College of Health Sciences, Kaohsiung Medical University, No. 100, Shih-Chuan 1st Road, Sanmin District, Kaohsiung, 807, Taiwan, Tel +886-7-312-1101 Ext 2786, Fax +886-7-311-0811, Email [email protected]
Purpose: Palliative care utilization among hospitalized patients with advanced chronic obstructive pulmonary disease (COPD) in Taiwan remains low despite its costs making it eligible for reimbursement since 2009. Few studies have examined the trends of palliative care utilization. We analyzed the annual rate, associated factors, and timing of the inpatient palliative care utilization by hospitalized patients with COPD.
Patients and Methods: We conducted a cross-sectional observational study between 1 January 2007 and 31 December 2018. Population-based claims data were extracted from Taiwan’s National Health Insurance Research Database to identify patients aged ≧40 years with COPD five years before the first instance of inpatient palliative care utilization.
Results: There were 24,502 patients with COPD receiving inpatient palliative care. Our results indicated that older age, concomitant chronic conditions—especially cancer—and severity of comorbidities were associated with a higher rate of palliative care utilization by hospitalized patients with chronic obstructive pulmonary disease. In our study, the proportion of hospitalized patients with COPD receiving inpatient palliative care and having a Charlson comorbidity index score of 1– 2 was lower than that of patients with cancer and a Charlson comorbidity index score ≧3 during the 12-year study-observation period. In addition, approximately 50% of hospitalized patients with COPD received palliative care within 18 months after their initial admission for COPD during the study period. However, individuals with a CCI score of 1– 2 exhibited a slower entry into palliative care, with nearly 50% initiating it within the first two years.
Conclusion: Inpatient palliative care utilization by hospitalized patients with advanced COPD remains low due to various causes. Our findings highlight that palliative care may be considered by professional care providers as routine care and as a way to manage problematic symptoms during hospitalization.
Keywords: cancer comorbidity, inpatient care, joinpoint regression, Taiwan’s health insurance database
Introduction
Chronic obstructive pulmonary disease (COPD), a progressive respiratory disorder, accounts for 2.6% of disability-adjusted life years and has caused approximately 3.2 million deaths worldwide in 2019.1,2 The functional disability of patients with COPD is associated with high-grade dyspnoea.3 Patients with advanced COPD experience unpredictable fluctuations between stable episodes of COPD and acute exacerbations.4 In Taiwan, progressive respiratory disorders is prevalent in approximately 6.1% of the general population5 and is the ninth leading cause of death.6 As it has the potential to overwhelm healthcare systems, a comprehensive care program for patients with progressive respiratory disorders experiencing exacerbations or concomitant conditions requiring hospitalization is necessary to build a patient-care network based on both disease management and palliative treatments.7,8
Palliative care may benefit patients who have respiratory diseases with concomitant serious illnesses and multifaceted needs, and has been recommended internationally by healthcare professionals.9 Population-based studies were conducted to explore palliative care utilization by patients with COPD in North America and Belgium; their findings indicated that prevalence of COPD gradually increased and was influenced by comorbidities at a life-limiting stage.10–12 Globally, 38.5% of cardiovascular diseases, 34% of cancers, 10.3% of chronic respiratory diseases, and other chronic diseases may benefit from palliative care; however, its utilization in such cases remains limited.13 To respect patients’ dignity and their end-of-life preferences, the Taiwanese National Health Insurance has taken progressive steps by reimbursing both inpatient and outpatient palliative care services, including patients with advanced lung disease.14
The Taiwanese National Health Insurance has been reimbursing palliative care costs to patients with COPD since 2009. A study found that the proportion of patients with COPD receiving inpatient and home-based palliative care significantly increased from 1997 to 2013 in Taiwan.14 Although its benefits include decreased intensive care unit (ICU) mortality and aggressive medical interventions, palliative care should be promoted among these patients owing to underutilization.15 The above studies primarily examined the inpatient utilization status, but they did not assess the timing of inpatient utilization among patients with COPD. Our study aimed to identify the factors associated with different timings and observed the trend in utilization by hospitalized patients with COPD during 2007–2018. We hypothesized that older age and severity of comorbidities, especially of cancer, may influence the timing of palliative care utilization.
Materials and Methods
Study Design, Setting, and Data Sources
This was a population-based cross-sectional study conducted using datasets from Taiwan’s National Health Insurance Research Database, obtained from Taiwan’s National Health Insurance program, which comprehensively covers 99.9% of Taiwan’s residents.16 The database records beneficiaries’ sex, date of birth, primary and secondary diagnoses, detailed information about outpatient and inpatient treatments and healthcare services received, and death registries. These administrative datasets underwent electronic processing, and the monthly beneficiary information obtained from the healthcare facilities was subjected to de-identification and anonymization procedures.
This cross-sectional observational study was approved by the Institutional Review Board of Chi Mei Medical Centre (IRB: 11,012-E01) and conducted in compliance with the ethical standards and guidelines of the 2013 revision of the Declaration of Helsinki. Informed consent was also waived by the Institutional Review Board of Chi Mei Medical Centre due to the use of secondary data and the absence of personal information in the study.
Study Participants
Patients had diagnosed with COPD (ICD-9-CM: 490–492, 496; ICD-10-CM: J41–44), aged >40 years, and who first utilized inpatient palliative care services between 1 January 2007 and 31 December 2018 (n=24,502) were enrolled as study participants. To focus on COPD-related palliative care, patients without COPD history within the five years preceding their first utilization of palliative care services were excluded. Additionally, claims with incomplete information or patients who utilized inpatient palliative care prior to 1 January 2007 were excluded. Figure 1 presents the flowchart of study participants’ inclusion.
 |
Figure 1 Flowchart of study participant inclusion. |
In Taiwan, palliative care is not legally mandated but is progressively integrated into the healthcare system. The decision to initiate palliative care consults is a collaborative process, involving attending physicians, healthcare teams, patients, and families. Taiwan’s National Health Insurance program has covered inpatient palliative care units for cancer or amyotrophic lateral sclerosis since 2000. In 2009, the coverage expanded to add eight advanced chronic diseases, including COPD. The enactment of the “Palliative Care and Hospice Care Act” in 2013 allowed end-of-life patients, diagnosed by a physician with family consent, to choose or decline cardiopulmonary resuscitation or life-sustaining treatment. Patients with palliative care could still access any medical service within Taiwan’s National Health Insurance program.17–19
Measurements
Demographic characteristics and major-disease-related factors for receiving palliative care were measured. Sex was dichotomously classified as either male or female and the following age groups were identified: 40–64, 65–74, and >75 years. In Taiwan, cancer has been the leading cause of death since 1982, and patients with cancer comprise a majority of those receiving palliative care. Therefore, the absence or presence of cancer among hospitalized patients with COPD was taken into consideration. The Charlson Comorbidity Index (CCI) score was used to measure the severity of comorbidities and the value thresholds considered were 1–2 and ≧3. To summarize, we assessed the palliative care utilization by factors such as age, sex, severity of comorbidities, and presence of cancer.
Statistical Analysis
Statistical Analysis System version 9.4 (SAS institute, Inc., Cary, NC, USA) was used for computing descriptive statistics, including patient characteristics, risk factors, and palliative care utilization. Categorical variables were presented as frequencies with percentages and continuous variables as mean ± standard deviation or median [interquartile range]. Joinpoint regression analysis was used to examine the trend and critical point of palliative care utilization over time; thus, the statistically significant points of trend changes were estimated.20 All significance levels, annual percentage change, and semi-annual percentage change values were set at p<0.05.
Results
A total of 24,502 hospitalized patients with COPD received inpatient palliative care. Table 1 presents the patient characteristics.
 |
Table 1 Characteristics of Hospitalized Patients with Chronic Obstructive Pulmonary Disease Receiving Palliative Care Utilization |
Annual Trend of COPD Palliative Care Utilization
An approximative seven-fold increase occurred in the number of hospitalized patients with COPD who utilized inpatient palliative care from 2007 (595) to 2018 (3,818). (Figure 2a) presents the overall trend of hospitalized patients with COPD who utilized palliative care; this demonstrates a significant increase over time (p<0.0001). Compared with the annual percentage change in inpatient palliative care utilization among hospitalized patients with COPD in 2007–2009, the annual percentage change was 44.04 (p=0.0353) in 2009–2012 and 25.67 (p=0.0282) in 2012–2016, reflecting a significant increase; it gradually declined during 2016–2018. The trend of hospitalized patients with COPD utilizing palliative care significantly increased over the years (p<0.0001) among both female and male patients and demonstrated a significant sex-based difference (p<0.0001). The trend of palliative care utilization in hospitalized patients with COPD who had cancer or CCI scores ≧ 3 gradually declined over time (Figure 2b). From 2009 to 2018, significant annual percentage changes of −6.28 (p<0.0001) and −5.32 (p<0.0001) among hospitalized patients with COPD and cancer, respectively, and those with CCI score ≧3 were observed. Conversely, the trend of palliative care utilization in hospitalized patients with COPD with a CCI score 1–2 significantly increased over time (p<0.0001), with an annual percentage change of 26.54 from 2009 to 2013 (p=0.0067) and 7.10 from 2013 to 2018 (p=0.0283). The proportion of hospitalized patients with COPD who concomitantly had cancer, with CCI scores 1–2 and ≧3, approached 50% in 2018.
 |
Figure 2 Trend of the palliative care utilization by hospitalized patients with COPD from 2007 to 2018 in Taiwan. (A) Overall and different sex; (B) Different disease severity. |
Annual Trend of COPD Palliative Care Timing
Approximately 50% of hospitalized patients with COPD (n=11,566, 47.20%) received palliative care within one and a half years after their initial admission for COPD during the study period. Overall, the trend of palliative care timing declined during the period of five years prior to patients’ first utilization of inpatient palliative care; semi-annual percentage changes of 42.19 and 10.74 (p<0.0001) were observed during 1–18 months and 18–60 months, respectively (Figure 3). Male and female patients showed similar trends in the timing of their palliative care utilization (p=0.3426).
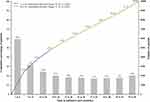 |
Figure 3 Trend of palliative care timing during the period of five years prior to patients’ first utilization of palliative care. |
Influence of Age, Sex, and Comorbidities
Approximately 50% of both men and women utilized inpatient palliative care within 18 months of admission to the hospital for COPD (Figure 4a). There was no difference in how the timing of the palliative care utilization changed among the three age groups; more than half of the hospitalized patients with COPD aged <65 years utilized inpatient palliative care within 13–18 months, whereas those aged >65 years utilized inpatient palliative care within 19–24 months (Figure 4b). Regarding the severity of comorbidities, the change in timing among hospitalized patients with a CCI score of 1–2 significantly differed from that among those with a score of ≧3 (p<0.0001). The timing of palliative care utilization among hospitalized patients with CCI scores of 1–2 demonstrated semi-annual percentage changes of 45.64 (p=0.0001) and 14.85 (p<0.0001) for 1–24 months and 24–60 months of diagnosis, respectively. Patients with CCI scores ≧ 3 demonstrated a semi-annual percentage change of 37.62 and 8.14 (p<0.0001) in 1–18 months and 18–60 months (Figure 4c). A significant difference (p=0.0221) was observed in timing between hospitalized patients with COPD with and without cancer (Figure 4d). The timing of the palliative care utilization by hospitalized patients with COPD and cancer revealed semi-annual percentage changes of 41.43 and 9.52 (p<0.0001) for 1–18 months and 18–60 months of diagnosis, respectively, compared with semi-annual percentage changes of 44.55 (p=0.0001) and 13.60 (p<0.0001) for 1–18 months and 18–60 months, respectively, for patients without cancer. Overall, 50.83% of patients with cancer and 56.04% of patients without cancer with COPD received inpatient palliative care within 13–18 and 25–30 months, respectively.
Figure 4 Continued.
Discussion
In this population-based cross-sectional study, we observed a significant increase in the utilization of inpatient palliative care among hospitalized patients with COPD from 2007 to 2018, consistent with the impact of palliative care policy modifications implemented in 2009 and 2012–2013. Furthermore, our findings indicated that among hospitalized COPD patients receiving inpatient palliative care, those with CCI scores of 1–2 had a lower proportion than patients with cancer and a CCI score ≧3 around the 12-year observation period. This highlights the influence of specific patient characteristics on the utilization of palliative care services. Consistent with previous studies, older age and the severity of comorbidities, especially cancer, have been identified as factors associated with the utilization of palliative care among patients with advanced COPD during hospitalization.11,21,22
In older patients with COPD with multiple comorbidities, hospitalization for palliative care is more likely. However, physicians in Taiwan may misunderstand or stereo typify palliative care as an end-of-life program only for patients with terminal cancer. Cultural differences in physicians’ attitudes towards patient autonomy and a goal of “good death” are prevalent in clinical practice in East Asian countries.23 As some hospitalized patients with COPD may be critically ill, autonomous decision-making for availing palliative care may not be possible in such cases. Our previous study, focus on the COPD patients in ICU, indicated that a significant difference in the utilization of palliative care and healthcare intervention burdens between those with and without cancer. It also indicated that patients without cancer, particularly those receiving mechanical ventilation, showed a slightly higher rate of palliative care utilization compared to patients with cancer in the ICU. Specifically, it suggested that the COPD patients without cancer had lower rates of palliative care utilization and experienced more burden of healthcare interventions.24 Proactive efforts should be undertaken to identify COPD early and integrate geriatric and pulmonary medicine disciplines and palliative care in a timely manner into routine care for these patients.25,26 Timely introduction of an interdisciplinary inpatient palliative care team, consisting of specialists from various fields such as physicians, nurses, respiratory therapists, physical therapists and more, could help patients manage their physical, emotional, and psychological burdens, while respecting their needs and preferences.25–28
In addition, this study analyzed the effect of government health strategies on palliative care for patients with COPD. We found that two key points in 2009 and 2013 may have influenced the use of palliative care from 2007 to 2018. By 2018, Hospitalized patients with COPD have shown an increasing overlap with palliative care. These health strategies could establish a high-quality care system for older, high-need, and high-cost patients with COPD, balancing pay-for-performance and value-based care.29,30 Government health strategies had a significant impact on palliative care utilization in Taiwan. In 2009, the introduction of the Hospice Palliative Care Act and the expansion of National Health Insurance coverage to include non-cancer diseases, such as COPD, marked a key step. Following the initiatives, the Inpatient Shared-Hospice care project in 2011, an amendment to the Hospice Palliative Care Act in 2013, and the Patient Right to Autonomy Act in 2016, continued to focus on patients with severe illnesses and protect their medical decision-making rights.31 Furthermore, the emphasis on hospice palliative care within hospital accreditation procedures contributed to make it growth. In 2017, the COPD clinical management guideline and the Pay for Performance (P4P) program served as motivating factors to promote the delivery of high-quality care with clinical guidelines.32 Furthermore, financial incentives for training programs and monitoring/evaluating clinical outcomes of palliative care, in addition to the accountability of palliative care provision and surveillance of performance, were used to improve access to such services for patients and reduce unnecessary medical costs.33
Our study found that there were differences in the timing of palliative care utilization by hospitalized patients with COPD, indicating difficulty in decision-making from clinicians when recommending palliative care in clinical practice. Previous studies examined palliative care services for patients without cancer in reverse order from the time of the patient’s death.34–37 Palliative care utilization assessed from the time of COPD diagnosis or retrospective from patient death indicates that patients with COPD may require a longer time of inpatient palliative care. The accuracy of prognostic or survival predictions for COPD patients, made two days prior to their death, was approximately 50%.38 Several studies aimed to identify potential disease-specific predictors for patients with COPD at the end-of-life stage.39,40 Timely palliative care support for severely ill patients without cancer entirely relies on changing the misperception of palliative care as end-of-life care, resolving the shortage of trained palliative care providers, improving physician–patient discussions about these services, and supplementing the inadequate reimbursement coverage for palliative care.25,41,42 Therefore, integrating respiratory, geriatric, and palliative treatment for older patients with COPD and improving their quality of life by managing multiple symptoms is required. A collaborative care program with interdisciplinary professionals may offer optimal medical treatment for breathlessness and ageing-related problems, as well as support, including palliative care and preferences, according to patient needs and their living wills.43–45
Limitations
Our study had several limitations. First, patients’ socioeconomic characteristics such as residence in urban or rural areas, educational level, marital and income statuses and the availability of informal caregivers were not measured. These characteristics have been considered as palliative care access-related determinants in published studies. Additionally, our participant data did not include clinical laboratory tests (such as arterial blood gas values), COPD assessment scales for pulmonary function tests, nor quality-of-life questionnaires. In real-world clinical practice, these data may be essential indicators for identifying COPD severity and helping healthcare providers assess the need for palliative care in hospitalized patients. Second, we only described the trend of inpatient palliative care utilization for hospitalized patients with COPD without evaluating its components comprehensively. These components may be considered that palliative care had been utilized by hospitalized patients with COPD, especially incomprehensively tracing the prevalence of long-term inpatient palliative care utilization. This is particularly true regarding the appropriate timing of such care for patients with COPD during hospitalization, ICU admissions, and aggressive medical interventions because of their multi-dimensional needs and heterogeneous life trajectories. Moreover, we acknowledged a limitation related to the severity classification of COPD in our study. Although we attempted to use hospitalized patients with primary COPD diagnosis codes as the level of severity, the results were consistent with our current findings (Supplementary Figures 1 and 2), indicating potential limitations in the precision of this approach. Finally, our study focused on inpatient palliative care utilization, but community-based palliative care was also crucial in managing COPD patients effectively. Future studies could investigate the impact of these alternative care settings on hospital admissions, patient outcomes, and healthcare costs, providing more views of palliative care for COPD patients.
Conclusion
Our findings indicated a seven-fold increase in inpatient palliative care utilization among hospitalized patients with COPD during the study period. This increase represents a substantial shift in practice, confirming the historical underutilization of palliative care in this population. Our study presented the developing situation and revealed complexities in the timing and frequency of palliative care initiation for COPD patients. Specifically, our results demonstrated that approximately 50% of hospitalized COPD patients receiving palliative care within 18 months of their initial admission. However, for patients with a CCI score of 1–2, their entry into palliative care tends to occur more slowly, with nearly 50% initiating within the first two years. This suggested a significant improvement but also indicated room for further optimization.
In conclusion, our study show a significant increase in inpatient palliative care utilization for COPD patients. However, optimizing the timing and delivery of palliative care in this population remains an ongoing challenge, requiring advanced data analysis. The complexities involved need further investigation. In the future research, exploring the association between palliative care utilization and life-sustaining interventions, especially mechanical ventilation, may reveal a critical area for investigation.
Data Management and Sharing
The data have been sourced from the Taiwan Nation Health Insurance Database and Taiwan Cancer Registry. The data are available with permission from the Taiwan Health and Welfare Data Science Centre: https://dep.mohw.gov.tw/DOS/np-2497-113.html (accessed 5 January 2023). Restrictions apply to the availability of these data, which were used under license for this study.
Ethics Approval and Consent to Participate
This study was conducted in compliance with the ethical standards and guidelines of the 2013 revision of the Declaration of Helsinki and approved by the Institutional Review Board of Chi Mei Medical Centre (IRB: 11012-E01). Informed consent was also waived by the Institutional Review Board of Chi Mei Medical Centre owing to the use of secondary data and the absence of personal information in the study.
Acknowledgments
The authors are grateful to the Health Data Science Centre of the National Cheng Kung University Hospital for providing administrative and technical support.
Funding
This study was supported by grants from the Chi Mei Medical Center (grant reference: CMFHR11128 and 111CM-KMU-09). The funding agency was not involved in any aspect of the study design, including data collection, data interpretation, or manuscript preparation.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Soriano JB, Abajobir AA, Abate KH.; GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;5(9):691–706. doi:10.1016/S2213-2600(17)30293-X
2. World Health Organization. Chronic obstructive pulmonary disease (COPD); 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd).
3. Weingaertner V, Scheve C, Gerdes V, et al. Breathlessness, functional status, distress, and palliative care needs over time in patients with advanced COPD or lung cancer: a cohort study. J Pain Symptom Manage. 2014;48(4):569–581. doi:10.1016/j.jpainsymman.2013.11.011
4. Murray SA, Kendall M, Boyd K, Sheikh A. Illness trajectories and palliative care. BMJ. 2005;330(7498):1007–1011. doi:10.1136/bmj.330.7498.1007
5. Cheng SL, Chan MC, Wang CC, et al. COPD in Taiwan: a national epidemiology survey. Int J Chron Obstruct Pulmon Dis. 2015;10:2459–2467. doi:10.2147/COPD.S89672
6. Ministry of Health and Welfare. Taiwan’s leading causes of death in 2022. Available from: https://www.mohw.gov.tw/cp-16-74869-1.html.
7. Lanken PN, Terry PB, DeLisser HM, et al. An official American Thoracic Society clinical policy statement: palliative care for patients with respiratory diseases and critical illnesses. Am J Respir Crit Care Med. 2008;177(8):912–927. doi:10.1164/rccm.200605-587ST
8. Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med. 2017;195(5):557–582. doi:10.1164/rccm.201701-0218PP
9. Kelley AS, Morrison RS. Palliative care for the seriously ill. New Eng J Med. 2015;373(8):747–755. doi:10.1056/NEJMra1404684
10. Gershon AS, Maclagan LC, Luo J, et al. End-of-life strategies among patients with advanced COPD. Am J Respir Crit Care Med. 2018;198(11):1389–1396. doi:10.1164/rccm.201803-0592OC
11. Rush B, Hertz P, Bond A, McDermid RC, Celi LA. Use of palliative care in patients with end-stage COPD and receiving home oxygen: national trends and barriers to care in the United States. Chest. 2017;151(1):41–46. doi:10.1016/j.chest.2016.06.023
12. Faes K, Cohen J, Annemans L. Resource use during the last six months of life among COPD patients: a population-level study. J Pain Symptom Manage. 2018;56(3):318–326.e7. doi:10.1016/j.jpainsymman.2018.06.002
13. World Health Organization. Palliative care; 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/palliative-care.
14. Kuo LC, Chen JH, Lee CH, Tsai CW, Lin CC. End-of-life health care utilization between COPD and lung cancer patients. J Pain Symptom Manage. 2019;57(5):933–943. doi:10.1016/j.jpainsymman.2019.01.011
15. Chou WC, Lai YT, Hung YS. Comparing end-of-life care in hospitalized patients with COPD with and without palliative care in Taiwan. J Res Med Sci. 2013;18(7):594–600.
16. Hsieh CY, Su CC, Shao SC, et al. Taiwan’s national health insurance research database: past and future. Clin Epidemiol. 2019;11:349–358. doi:10.2147/CLEP.S196293
17. Chen RC. Providing patients with dementia and neurological diseases a dignified peaceful demise. BAOJ Pall Medicine. 2016;2:15.
18. Lai CF, Tsai HB, Hsu SH, et al. Withdrawal from long-term hemodialysis in patients with end-stage renal disease in Taiwan. J Formos Med Assoc. 2013;112:589–599. doi:10.1016/j.jfma.2013.04.009
19. Chen PJ, Liang FW, Ho CH, et al. Association between palliative care and life-sustaining treatments for patients with dementia: a nationwide 5-year cohort study. Palliat Med. 2018;32(3):622–630. doi:10.1177/0269216317751334
20. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. doi:10.1002/(SICI)1097-0258(20000215)19:3<335::AID-SIM336>3.0.CO;2-Z
21. Meffert C, Hatami I, Xander C, Becker G. Palliative care needs in COPD patients with or without cancer: an epidemiological study. Eur Respir J. 2015;46(3):663–670. doi:10.1183/09031936.00208614
22. Bloom CI, Slaich B, Morales DR, Smeeth L, Stone P, Quint JK. Low uptake of palliative care for COPD patients within primary care in the UK. Eur Respir J. 2018;51(2):1701879. doi:10.1183/13993003.01879-2017
23. Morita T, Oyama Y, Cheng SY, et al. Palliative care physicians’ attitudes toward patient autonomy and a good death in East Asian countries. J Pain Symptom Manage. 2015;50(2):190–191. doi:10.1016/j.jpainsymman.2015.02.020
24. Kao LT, Cheng KC, Chen CM, et al. Burden of healthcare utilization among chronic obstructive pulmonary disease patients with and without cancer receiving palliative care: a population-based study in Taiwan. Int J Environ Res Public Health. 2020;17(14):4980. doi:10.3390/ijerph17144980
25. Brown CE, Jecker NS, Curtis JR. Inadequate palliative care in chronic lung disease. An issue of health care inequality. Ann Am Thorac Soc. 2016;13(3):311–316. doi:10.1513/AnnalsATS.201510-666PS
26. Patel K, Janssen DJ, Curtis JR. Advance care planning in COPD. Respirol. 2012;17(1):72–78. doi:10.1111/j.1440-1843.2011.02087.x
27. Smith TJ, Temin S, Alesi ER, et al. American society of clinical oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol. 2012;30(8):880–887. doi:10.1200/JCO.2011.38.5161
28. Ferrell BR, Temel JS, Temin S, et al. Integration of palliative care into standard oncology care: American society of clinical oncology clinical practice guideline update. J Clin Oncol. 2017;35(1):96–112. doi:10.1200/JCO.2016.70.1474
29. Heffner JE, Mularski RA, Calverley PM. COPD performance measures: missing opportunities for improving care. Chest. 2010;137(5):1181–1189. doi:10.1378/chest.09-2306
30. Shah T, Press VG, Huisingh-Scheetz M, et al. COPD readmissions: addressing COPD in the era of value-based health care. Chest. 2016;150(4):916–926. doi:10.1016/j.chest.2016.05.002
31. Cheng SY, Chen CY, Chiu TY. Advances of hospice palliative care in Taiwan. Korean J Hospice Palliat Care. 2016;19(4):292–295. doi:10.14475/kjhpc.2016.19.4.292
32. Cheng SL, Li YR, Huang N, et al. Effectiveness of Nationwide COPD pay-for-performance program on COPD exacerbations in Taiwan. Int J Chron Obstruct Pulmon Dis. 2021;16:2869–2881. doi:10.2147/COPD.S329454
33. Meier DE, Back AL, Berman A, et al. A national strategy for palliative care. Health Aff. 2017;36(7):1265–1273. doi:10.1377/hlthaff.2017.0164
34. Beernaert K, Cohen J, Deliens L, et al. Referral to palliative care in COPD and other chronic diseases: a population-based study. Respir Med. 2013;107(11):1731–1739. doi:10.1016/j.rmed.2013.06.003
35. Scheerens C, Beernaert K, Pype P, et al. Comparing the use and timing of palliative care services in COPD and lung cancer: a population-based survey. Eur Respir J. 2018;51(5):1702405. doi:10.1183/13993003.02405-2017
36. Jordan RI, Allsop MJ, ElMokhallalati Y, et al. Duration of palliative care before death in international routine practice: a systematic review and meta-analysis. BMC Med. 2020;18(1):1–25. doi:10.1186/s12916-020-01829-x
37. Quinn KL, Wegier P, Stukel TA, et al. Comparison of palliative care delivery in the last year of life between adults with terminal noncancer illness or cancer. JAMA Netw Open. 2021;4(3):e210677. doi:10.1001/jamanetworkopen.2021.0677
38. Claessens MT, Lynn J, Zhong Z, et al. Dying with lung cancer or COPD: insights from SUPPORT. J Am Geriatr Soc. 2000;48(S1):S146–153. doi:10.1111/j.1532-5415.2000.tb03124.x
39. Coventry PA, Grande GE, Richards DA, et al. Prediction of appropriate timing of palliative care for older adults with non-malignant life-threatening disease: a systematic review. Age Ageing. 2005;34(3):218–227. doi:10.1093/ageing/afi054
40. Smith LJE, Moore E, Ali I, et al. Prognostic variables and scores identifying the end of life in COPD: a systematic review. Int J Chron Obstruct Pulmon Dis. 2017;12:2239. doi:10.2147/COPD.S137868
41. Aldridge MD, Hasselaar J, Garralda E, et al. Education, implementation, and policy barriers to greater integration of palliative care: a literature review. Palliat Med. 2016;30(3):224–239. doi:10.1177/0269216315606645
42. Tang ST, Liu TW, Liu LN, et al. Physician-patient end-of-life care discussions: correlates and associations with end-of-life care preferences of cancer patients-a cross-sectional survey study. Palliat Med. 2014;28(10):1222–1230. doi:10.1177/0269216314540974
43. Higginson IJ, Bausewein C, Reilly CC, et al. An integrated palliative and respiratory care service for patients with advanced disease and refractory breathlessness: a randomised controlled trial. Lancet Respir Med. 2014;2(12):979–987. doi:10.1016/S2213-2600(14)70226-7
44. Iyer AS, Curtis JR, Meier DE. Proactive integration of geriatrics and palliative care principles into practice for COPD. JAMA Intern Med. 2020;180(6):815–816. doi:10.1001/jamainternmed.2020.1088
45. Voumard R, Rubli TE, Benaroyo L, et al. Geriatric palliative care: a view of its concept, challenges and strategies. BMC Geriatr. 2018;18(1):1–6. doi:10.1186/s12877-018-0914-0
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

