Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 11
Treatment, Resource Use and Costs Among Pediatric Patients with Neurofibromatosis Type 1 and Plexiform Neurofibromas
Authors Yang X, Desai K, Agrawal N , Mirchandani K , Chatterjee S , Sarpong E, Sen S
Received 16 June 2020
Accepted for publication 5 August 2020
Published 7 October 2020 Volume 2020:11 Pages 421—428
DOI https://doi.org/10.2147/PHMT.S265690
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Xiaoqin Yang,1 Kaushal Desai,1 Neha Agrawal,2 Kirti Mirchandani,2 Sagnik Chatterjee,2 Eric Sarpong,1 Shuvayu Sen1
1Merck & Co., Inc. Center for Observational and Real-World Evidence, Kenilworth, NJ, USA; 2Complete HEOR Solutions, North Wales, PA, USA
Correspondence: Xiaoqin Yang
Merck & Co., Inc., Center for Observational and Real-World Evidence (CORE), 126 East Lincoln Avenue, Rahway, NJ 07065-0900, USA
Tel +1 732 594-7587
Email [email protected]
Background: Neurofibromatosis type 1 (NF1) is an autosomal dominant genetic condition which predisposes individuals to tumors of the nervous system, skin, bones, and eyes. Plexiform neurofibromas (PNs) occur in 20– 50% of NF1 cases, causing multiple morbidities and conferring a risk of malignancy. NF1 with PN is poorly characterized in the literature with regard to treatment patterns, healthcare resource utilization, and costs in the real world.
Methods: This was a retrospective analysis of data from a commercial claims database in the US between October 2014 and March 2018. Persons with at least 1 diagnostic code for both NF1 and PN, aged ≤ 18 years on the index date, and continuously enrolled for ≥ 12 months before the index date were included. The index date was defined as the date of the first diagnosis of NF1 or PN during the study period, whichever occurred later. Healthcare resource utilization during follow-up included outpatient, inpatient, emergency room (ER), and pharmacy encounters; corresponding costs were calculated as the mean per patient per year (PPPY) in 2018 US dollars. Treatments were classified as PN surgery, pain medication, chemotherapy, radiotherapy, and targeted therapies. All analyses were descriptive.
Results: A total of 301 patients were included. In the follow-up period, nearly all patients (99.7%) had outpatient visits, while 81.1% had pharmacy visits, 25.2% had ER visits, and 13.0% had inpatient visits. Mean ± SD [median] total healthcare costs PPPY were $38,292 ± $80,556 [$16,037]. During follow-up, 44.2% of patients used pain medications, 23.9% received chemotherapy, 5.0% underwent surgery for PN, 1.3% received radiotherapy, and 1.0% received targeted therapies.
Conclusion: Commercially insured pediatric patients diagnosed with NF1 and PN were treated primarily with supportive care, highlighting a substantial unmet need in the United States.
Keywords: neurofibromatosis type 1, plexiform neurofibromas, treatment patterns, healthcare resource use, treatment costs
Plain Language Summary
What is Already Known About This Subject?
- Neurofibromatosis type 1 (NF1) is an autosomal dominant genetic condition which predisposes individuals to tumors of the nervous system, skin, bones, and eyes.
- Plexiform neurofibromas (PNs) occur in 20–50% of NF1 cases.
- Disease progression, pain, and behavioral symptoms in patients with NF1 with PN have been reported in the literature, but less is known about treatment patterns or interactions with the health care system.
What This Study Adds?
- Our findings demonstrate the considerable healthcare resource utilization and costs in children and adolescents with NF1 and PN.
- These patients were treated primarily with supportive care.
- New therapeutic options are needed to help improve patient health outcomes.
Introduction
Neurofibromatosis type 1 (NF1) is a genetic disorder characterized by diverse, progressive cutaneous, neurological, skeletal, and neoplastic manifestations.1 These manifestations range from minor freckling of the skin to mobility-limiting disfigurement and serious neurological deficits.2 NF1 is progressive throughout the lifetime of an individual and significantly decreases lifespan.3–5
The global prevalence of NF1 is 1 in 3000 to 1 in 6000 people.6,7 The diagnostic criteria are well established and include café au lait macules on the skin, Lisch nodules in the eye, dysplasia in the bones, and externally visible or internal neurofibromas.8 The major clinical manifestations of NF1 become apparent during childhood and adolescence, with most patients diagnosed by the age of 8.9 Clinical management of patients with NF1 initially consists of surveillance of disease progression and palliative care for symptoms, including, when possible, surgical excision of tumors.8
Approximately 20–50% of NF1 patients exhibit a type of tumor known as plexiform neurofibroma (PN).2,10-12 Distinct from other NF1-related tumors, PNs grow in the nerve sheaths of multiple large nerve bundles and are anatomically invasive.13,14 They are typically benign, but can give rise to malignant peripheral nerve sheath tumors, particularly in young adults.15,16 PNs grow most rapidly during childhood and adolescence, and because of their invasive nature, complete removal of PNs is generally impossible.6,8,13 Ongoing trials are examining the efficacy of targeted therapies, namely drugs targeted to the specific cellular signaling pathways that are disrupted by the genetic mutation that gives rise to NF1,17,18 with the goal of slowing or stopping the growth of PNs. One such therapy, selumetinib, has recently been approved by the FDA for the treatment of pediatric NF1 patients with symptomatic, inoperable PNs.19,20
Several aspects of the burden of PN in children and adolescents with NF1 have been studied in the National Cancer Institute’s NF1 natural history cohort (NCT00924196). One retrospective study of 7 years of clinical data described the increase in PN tumor volume and the progression of PN-associated pain and motor dysfunction over time.21 Surveys of caregivers and adolescents with NF1 and PN found that pain interfered with the child’s daily functioning despite using pain medication.22 Behavioral assessments of children in the cohort found that behavior scores were linked to both disease- and environment-related variables.23 However, NF1 with PN is poorly characterized in the literature with regards to treatment patterns, healthcare resource utilization, and costs in the real world. The objective of this study was to describe the real-world demographics and clinical characteristics, treatment patterns, healthcare resource utilization, and costs among pediatric patients diagnosed with NF1 and PN in the United States.
Materials and Methods
Study Design
This was a retrospective analysis of medical and pharmacy claims data. The study period was from October 1, 2014, to March 31, 2018 (Supplemental Figure 1). The index date was the date of first diagnosis of NF1 or PN, whichever occurred later, on or after October 1, 2015. The baseline period was defined as the 12-month period before the index date. The follow-up period varied in length, spanning from the index date to the end of the study period or the end of continuous enrollment in the health plan, whichever occurred first.
Data Source
Claims data were from the MarketScan® Commercial Claims and Encounters (CCAE) database. This database, compiled and maintained by IBM® Watson Health, belongs to a family of administrative claims databases that contain data on over 250 million unique patients in the United States.24 The databases are large, nationally representative, and contain patient-level data on clinical utilization, expenditures, and enrollment across inpatient, outpatient, and prescription drug services. The CCAE database contains de-identified, individual-specific details for people covered by employer-sponsored private health insurance, as well as their spouses and dependents. Institutional Review Board (IRB) approval was not required because this study was an analysis of de-identified secondary data.
Study Population
Patients diagnosed with both NF1 and PN, aged ≤18 on the index date, and continuously enrolled for ≥12 months before the index date were included in the study population. Continuous enrollment was defined as no lapse in insurance coverage longer than 45 days. NF1 and PN were identified using International Classification of Diseases, 10th revision, Clinical Modification (ICD-10-CM) codes of Q85.01 for NF1; and D36.1x, D31.6x, and D33.3 for PN.
Study Outcomes
The study outcomes were demographic and clinical characteristics in the baseline period (or on the index date); and all-cause healthcare resource utilization, all-cause costs, imaging services, and treatments in the follow-up period. Patient demographics included age, sex, type of health insurance, and region of residence. Clinical characteristics included the baseline Charlson comorbidity index (CCI) score based on 12 months of claims prior to the index date. The CCI score was calculated using Deyo’s modified method incorporating the following conditions: acute myocardial infarction, congestive heart failure, peripheral vascular disease, cerebral vascular accident, dementia, chronic pulmonary disease, connective tissue disorder, peptic ulcer, mild/moderate/severe liver disease, diabetes with/without complications, hemiplegia or paraplegia, renal disease, cancer, metastatic solid tumor, and AIDS/HIV.25–27 Information about the index diagnosis was also collected, including the place of service codes and provider type category on the diagnosis claim. The specialist provider type included provider codes 100–799 (excluding codes 204 and 240), which in practice meant primarily neurologists, ophthalmologists, pediatricians, radiologists, pediatric hematologists/oncologists, and geneticists.
All-cause healthcare resource utilization included inpatient, outpatient, emergency room (ER), pharmacy, and other encounters. Costs associated with inpatient, outpatient, ER, and other encounters were classified as medical costs, separate from the costs associated with pharmacy claims. Claims for imaging services (computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET)) were identified by the Healthcare Common Procedure Coding System (HCPCS) and ICD PROC codes (list available upon request). Treatments were broadly classified as surgery for PN, pain medication, chemotherapy, radiotherapy, and targeted therapies. Surgery for PN was identified by Current Procedural Terminology codes 64790 and 64792.28 Pain medications were identified by National Drug Codes using previously published methods.21,22,29 Chemotherapy included all medications and procedures coded as “chemotherapy” in the Cancer Research Network’s 2017 chemotherapy look-up tables.30 Radiotherapy was identified by codes listed in the Cancer Research Network’s radiation therapy look-up tables.30 Targeted therapies included MAPK/ERK kinase (MEK) inhibitors (binimetinib, cobimetinib, and trametinib dimethyl sulfoxide), tyrosine kinase inhibitors (bosutinib, dasatinib, imatinib, nilotinib, ponatinib, and sunitinib), and pegylated interferon alpha-2b.
Statistical Methods
All statistical analyses were descriptive and were carried out using SAS version 9.4. Patient characteristics from the baseline period or index date were presented as numbers and percentages for categorical variables and as means and standard deviations (SDs) for continuous variables. Follow-up healthcare resource utilization was tabulated both as the number and proportion of patients with each type of resource use. The mean (SD) and median (range) number of claims per patient with each type of healthcare resource utilization were determined, as well as the mean (SD) per patient per year (PPPY), which was calculated as the total number of claims for each type of resource use divided by the total length of follow-up in years for the group of patients with each type of healthcare resource utilization. Costs during follow-up were presented as means (SD) or medians ([interquartile range [IQR]). Healthcare costs PPPY were calculated as the total cost divided by the total number of days of enrollment in years, where costs were weighted by each patient’s length of follow-up to avoid overestimation and annualized for patients observed for less than 1 year. All costs were adjusted to 2018 US dollars based on the medical care component of the Consumer Price Index.31 Imaging services and treatments during the follow-up period were presented as the number and proportion of patients with each service or treatment type.
Results
Demographic and Clinical Characteristics of Patients Diagnosed with NF1 and PN
A total of 301 patients were included in the analysis (Figure 1), 153 (50.8%) of whom were female (Table 1). The mean±SD age on the index date was 11.7±4.6 years, and the mean±SD baseline CCI score was 0.93±1.41. Most index diagnoses occurred in a doctor’s office (57.8%) or outpatient hospital (46.5%) and were provided by a specialist (77.1%). The mean±SD and median (range) duration of follow-up were 496±275 and 481 (0–912) days, respectively, for a total of 149,297 follow-up days (data not shown).
 |
Table 1 Baseline Demographic and Clinical Characteristics Among Pediatric Patients Diagnosed with NF1 and PNa |
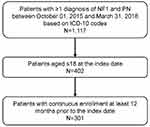 |
Figure 1 Patient selection flow chart. The index date was defined as the date of the first diagnosis of NF1 or PN during the study period, whichever occurred later. |
Healthcare Resource Use and Costs of Patients Diagnosed with NF1 and PN
In analyses of healthcare resource utilization during the follow-up period, nearly all patients (99.7%) had outpatient visits, while 81.1% had pharmacy visits, 25.2% had ER visits, and 13.0% had inpatient visits (Table 2). The mean±SD numbers of outpatient encounters and pharmacy visits PPPY were 18.2±15.4 and 9.8±10.6, respectively.
 |
Table 2 All-Cause HCRU During the Follow-Up Period Among Pediatric Patients Diagnosed with NF1 and PN |
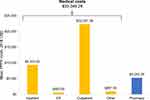
Mean±SD and median (IQR) costs PPPY during follow-up were $38,292±$80,556 and $16,037 ($6,933-$40,138), respectively (Supplemental Table 1). The cost breakdown showed that medical costs constituted 86.3% of the total and were driven by outpatient costs (67.5% of medical costs; Figure 2).
Imaging Services and Treatment Patterns of Patients Diagnosed with NF1 and PN
Of the 213 patients (70.8%) who underwent imaging in the follow-up period, most received MRI (n=208; Table 3). In analyses of treatment patterns, 15 patients (5.0%) had surgery for PN. Just under half (44.2%) of the patients used pain medications, mostly corticosteroids, opioids, and analgesics; while 23.9% received chemotherapy, 1.3% received radiotherapy, and 1.0% received targeted therapies. The most common chemotherapy was dexamethasone (n=50; 16.6%). Targeted therapies in use during follow-up were the MEK inhibitor trametinib dimethyl sulfoxide (n=2; 0.7%) and the tyrosine kinase inhibitor imatinib mesylate (n=1; 0.3%).
 |
Table 3 Imaging Services and Treatment Patterns During the Follow-Up Period Among Pediatric Patients Diagnosed with NF1 and PN |
Discussion
This study showed that the healthcare resource utilization and costs of commercially insured pediatric patients with NF1 and PN were considerable. Treatment consisted primarily of pain relievers.
Our findings on the use of pain relievers (44% usage rate) are consistent with previous studies. In a population drawn from the National Cancer Institute’s Natural History Study of Patients with NF1 (N=41; median age 8 years), 43% were using pain relievers at the study baseline; however, this value rose to 63% at the time point of maximum PN volume (a median time span of 6.5 years).21 In a cross-sectional survey of NF1 patients attending the Cincinnati Children’s Hospital Medical Center (n=28; median age 12 years), 43% were taking pain medication.32 The use of pain medication has been correlated with lower quality of life (both self-rated and caregiver-rated) in children and adolescents with NF1 and PNs.22 Among 60 children and adolescents in the National Cancer Institute’s natural history cohort, 33% were taking pain medication, but the caregivers of 73% of these patients reported that pain still interfered with daily functioning,22 indicating that pain medications are an ineffective therapy for PN-related pain in NF1.
Other treatments used less frequently in our study population were chemotherapy (24%) and surgery (5%). In contrast, among 59 children (median age 8 years) enrolled in NF1/PN trials at the National Institutes of Health in 1996–2007,33 very few had had prior chemotherapy (5%), while 47% had had debulking surgery for their PN. These differences may be attributed to differences in age and duration of disease between the study populations, differences in the definitions of chemotherapy, and/or potential selection bias toward including patients with more severe symptoms in the clinical trial population.
Our study characterized a real-world, commercially insured population, and presents novel information about healthcare resource utilization and costs incurred by pediatric NF1 patients with PNs. The substantial resource use and cost burden described here, along with the findings of others regarding the burden of disease, highlights the need for new and more effective pharmacotherapies. Agents that target the cellular signaling pathways disrupted by the genetic mutation that gives rise to NF1 are being developed. Particularly promising results were obtained from a Phase I trial of selumetinib, where tumor volume reductions of ≥20% were seen in 17 of 24 children (71%),34 and from a Phase II trial of imatinib mesylate, where 26% of patients who took the drug for at least 6 months (n=23; ages 3–33) experienced tumor volume reductions of ≥20%.35 Phase II trial results on selumetinib showed that, over a median of 3 years of monthly treatment cycles, 70% of patients (N=50; ages 4–17) had a confirmed tumor volume reduction ≥20%, and this reduction was maintained for a year or more in 56% of patients.36 In addition, 38% of evaluable children reported clinically meaningful improvements in the interference of pain in their daily functioning. Selumetinib was recently approved by the FDA for the treatment of pediatric NF1 patients with symptomatic, inoperable PNs,19,20 providing additional treatment options for patients being managed with supportive care alone.
Limitations
Several limitations inherent to the use of administrative claims data apply to our study. First, the use of diagnosis codes and procedure codes to identify patients and procedures is imperfect because of variations in coding; specifically, there is no single ICD code identifying PN. The ICD diagnosis codes for PN may not be specific to PN; however, the diagnosis codes used in this study were reviewed for accuracy by a clinician specializing in NF1. Second, since the CCAE database contains information on individuals with employer-sponsored health coverage, the results may not be generalizable to other populations, e.g., the uninsured or those with Medicaid coverage. Third, drugs administered during an inpatient stay do not appear in the database, so we were not able to capture individual drugs administered in hospital. A corollary is that any treatments which were not covered by the insurance would not be included. Fourth, although dexamethasone and tretinoin are included as chemotherapy in the Cancer Research Network’s 2017 chemotherapy look-up tables,30 they may be used as non-chemotherapies in conditions other than cancer. Finally, NF1-related PN is a chronic condition, and the relatively short length of the follow-up period in our study (mean follow-up of 496 days) did not allow us to capture healthcare resource utilization and cost beyond the follow-up period.
Conclusions
This study characterized the treatment patterns, healthcare resource utilization, and costs of commercially insured pediatric patients with NF1 and PN in the United States. Our findings demonstrate the considerable healthcare resource utilization and costs in this patient population and show that pediatric patients with NF1 and PN are treated primarily with supportive care. It is clear that new therapeutic options, such as the emerging class of targeted therapies, are sorely needed to help improve pediatric NF1 and PN patient health outcomes.
Abbreviations
CCAE, Commercial Claims and Encounters; CCI, Charlson Comorbidity Index; CT, computed tomography; HCPCS, Healthcare Common Procedure Coding System; ICD-10-CM, International Classification of Diseases, 10th revision, Clinical Modification; IQR, interquartile range; IRB, Institutional Review Board; MRI, magnetic resonance imaging; NF1, neurofibromatosis type 1; PET, positron emission tomography; PN, plexiform neurofibroma; PPPY, per patient per year; SD, standard deviation.
Data Sharing Statement
Claims data were from the CCAE database.
Ethics Approval and Informed Consent
The CCAE database contains de-identified information, and, therefore IRB approval and informed consent were not necessary.
Acknowledgments
The authors thank Melissa Stauffer, PhD, and Anna Kaufman, MPH, in association with ScribCo, for medical writing assistance.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Funding was provided by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA. The analysis was conducted by Complete HEOR Solutions LLC and funded by Merck Co. & Inc.
Disclosure
Xiaoqin Yang, Kaushal Desai, Eric Sarpong, and Shuvayu Sen are employees of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA and may be stockholders of Merck & Co., Inc., Kenilworth, NJ, USA. Kaushal Desai is a stockholder of AstraZeneca. Neha Agrawal, Kirti Mirchandani, and Sagnik Chatterjee, are employees of Complete HEOR Solutions, North Wales, PA, USA which has received financial compensation for conducting the study analysis. The authors report no other conflicts of interest in this work.
References
1. Neurofibromatosis. Conference statement. National Institutes of health consensus development conference. Arch Neurol. 1988;45(5):575–578.
2. Korf BR. Plexiform neurofibromas. Am J Med Genet. 1999;89(1):31–37. doi:10.1002/(SICI)1096-8628(19990326)89:1<31::AID-AJMG7>3.0.CO;2-W
3. Evans DG, O’Hara C, Wilding A, et al. Mortality in neurofibromatosis 1: in North West England: an assessment of actuarial survival in a region of the UK since 1989. Eur J Hum Genet. 2011;19(11):1187–1191. doi:10.1038/ejhg.2011.113
4. Masocco M, Kodra Y, Vichi M, et al. Mortality associated with neurofibromatosis type 1: a study based on Italian death certificates (1995–2006). Orphanet J Rare Dis. 2011;6(1):11. doi:10.1186/1750-1172-6-11
5. Rasmussen SA, Yang Q, Friedman JM. Mortality in neurofibromatosis 1: an analysis using U.S. death certificates. Am J Hum Genet. 2001;68(5):1110–1118. doi:10.1086/320121
6. Gutmann DH, Ferner RE, Listernick RH, Korf BR, Wolters PL, Johnson KJ. Neurofibromatosis type 1. Nat Rev Dis Primers. 2017;3(1):17004. doi:10.1038/nrdp.2017.4
7. Uusitalo E, Leppavirta J, Koffert A, et al. Incidence and mortality of neurofibromatosis: a total population study in Finland. J Invest Dermatol. 2015;135(3):904–906. doi:10.1038/jid.2014.465
8. Ferner RE, Huson SM, Thomas N, et al. Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. J Med Genet. 2007;44(2):81–88. doi:10.1136/jmg.2006.045906
9. DeBella K, Szudek J, Friedman JM. Use of the national institutes of health criteria for diagnosis of neurofibromatosis 1 in children. Pediatrics. 2000;105(3 Pt 1):608–614. doi:10.1542/peds.105.3.608
10. Mautner VF, Asuagbor FA, Dombi E, et al. Assessment of benign tumor burden by whole-body MRI in patients with neurofibromatosis 1. Neuro Oncol. 2008;10(4):593–598. doi:10.1215/15228517-2008-011
11. Karaconji T, Whist E, Jamieson RV, Flaherty MP, Grigg JRB. Neurofibromatosis type 1: review and update on emerging therapies. Asia Pac J Ophthalmol (Phila). 2019;8(1):62–72. doi:10.22608/APO.2018182
12. Nguyen R, Kluwe L, Fuensterer C, Kentsch M, Friedrich RE, Mautner VF. Plexiform neurofibromas in children with neurofibromatosis type 1: frequency and associated clinical deficits. J Pediatr. 2011;159(4):652–655 e652. doi:10.1016/j.jpeds.2011.04.008
13. Lai JS, Jensen SE, Charrow J, Listernick R. Patient reported outcomes measurement information system and quality of life in neurological disorders measurement system to evaluate quality of life for children and adolescents with neurofibromatosis type 1 associated plexiform neurofibroma. J Pediatr. 2019;206:190–196. doi:10.1016/j.jpeds.2018.10.019
14. Korf BR. Malignancy in neurofibromatosis type 1. Oncologist. 2000;5(6):477–485. doi:10.1634/theoncologist.5-6-477
15. Evans DG, Baser ME, McGaughran J, Sharif S, Howard E, Moran A. Malignant peripheral nerve sheath tumours in neurofibromatosis 1. J Med Genet. 2002;39(5):311–314. doi:10.1136/jmg.39.5.311
16. Ducatman BS, Scheithauer BW, Piepgras DG, Reiman HM, Ilstrup DM. Malignant peripheral nerve sheath tumors. A clinicopathologic study of 120 cases. Cancer. 1986;57(10):2006–2021. doi:10.1002/1097-0142(19860515)57:10<2006::AID-CNCR2820571022>3.0.CO;2-6
17. Karajannis MA, Ferner RE. Neurofibromatosis-related tumors: emerging biology and therapies. Curr Opin Pediatr. 2015;27(1):26–33. doi:10.1097/MOP.0000000000000169
18. Gutmann DH, Blakeley JO, Korf BR, Packer RJ. Optimizing biologically targeted clinical trials for neurofibromatosis. Expert Opin Investig Drugs. 2013;22(4):443–462. doi:10.1517/13543784.2013.772979
19. U.S. Food and Drug Administration. FDA Approves First Therapy for Children with Debilitating and Disfiguring Rare Disease; 2020.
20. U.S. Food and Drug Administration. KOSELUGO (selumetinib) capsules [Prescribing information]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/213756s000lbl.pdf. Accessed May 4, 2020.
21. Gross AM, Singh G, Akshintala S, et al. Association of plexiform neurofibroma volume changes and development of clinical morbidities in neurofibromatosis 1. Neuro Oncol. 2018;20(12):1643–1651. doi:10.1093/neuonc/noy067
22. Wolters PL, Burns KM, Martin S, et al. Pain interference in youth with neurofibromatosis type 1 and plexiform neurofibromas and relation to disease severity, social-emotional functioning, and quality of life. Am J Med Genet A. 2015;167A(9):2103–2113. doi:10.1002/ajmg.a.37123
23. Martin S, Wolters P, Baldwin A, et al. Social-emotional functioning of children and adolescents with neurofibromatosis type 1 and plexiform neurofibromas: relationships with cognitive, disease, and environmental variables. J Pediatr Psychol. 2012;37(7):713–724. doi:10.1093/jpepsy/jsr124
24. IBM. Data brochure: research databases for life sciences researchers. Available from: https://www.ibm.com/downloads/cas/OWZWJ0QO.
25. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57(12):1288–1294. doi:10.1016/j.jclinepi.2004.03.012
26. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi:10.1016/0895-4356(92)90133-8
27. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi:10.1097/01.mlr.0000182534.19832.83
28. Neurofibroma Midwest. Insurance coverage for neurofibroma removal. Available from: https://www.nfmidwest.org/wp-content/uploads/2016/03/Insurance-Coverage-of-Fibroma-Removal.pdf.
29. Rasu RS, Sohraby R, Cunningham L, Knell ME. Assessing chronic pain treatment practices and evaluating adherence to chronic pain clinical guidelines in outpatient practices in the United States. J Pain. 2013;14(6):568–578. doi:10.1016/j.jpain.2013.01.425
30. Cancer Research Network. Cancer therapy look-up tables. Available from: http://www.hcsrn.org/crn/en/RESEARCH/LookupTables/. Accessed January 29, 2020.
31. US Bureau of Labor Statistics. Consumer Price Index. Available from: https://www.bls.gov/cpi/home.htm.
32. Kongkriangkai AM, King C, Martin LJ, et al. Substantial pain burden in frequency, intensity, interference and chronicity among children and adults with neurofibromatosis type 1. Am J Med Genet A. 2019;179(4):602–607. doi:10.1002/ajmg.a.61069
33. Kim A, Gillespie A, Dombi E, et al. Characteristics of children enrolled in treatment trials for NF1-related plexiform neurofibromas. Neurology. 2009;73(16):1273–1279. doi:10.1212/WNL.0b013e3181bd1326
34. Dombi E, Baldwin A, Marcus LJ, et al. Activity of selumetinib in neurofibromatosis type 1-related plexiform neurofibromas. N Engl J Med. 2016;375(26):2550–2560. doi:10.1056/NEJMoa1605943
35. Robertson KA, Nalepa G, Yang FC, et al. Imatinib mesylate for plexiform neurofibromas in patients with neurofibromatosis type 1: a Phase 2 trial. Lancet Oncol. 2012;13(12):1218–1224. doi:10.1016/S1470-2045(12)70414-X
36. Gross AM, Wolters PL, Dombi E, et al. Selumetinib in children with inoperable plexiform neurofibromas. N Engl J Med. 2020;382(15):1430–1442. doi:10.1056/NEJMoa1912735
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.