Back to Journals » Vascular Health and Risk Management » Volume 12
Treatment adherence and quality of life in patients on antihypertensive medications in a Middle Eastern population: adherence
Authors Alhaddad IA , Hamoui O , Hammoudeh A , Mallat S
Received 5 February 2016
Accepted for publication 20 May 2016
Published 27 October 2016 Volume 2016:12 Pages 407—413
DOI https://doi.org/10.2147/VHRM.S105921
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Daniel Duprez
Imad A Alhaddad,1 Omar Hamoui,2 Ayman Hammoudeh,3 Samir Mallat4
1Cardiovascular Department, Jordan Hospital, Amman, Jordan; 2Cardiology Department, Clemenceau Medical Center, Beirut, Lebanon; 3Cardiology Department, Istishari Hospital, Amman, Jordan; 4Department of Internal Medicine, Nephrology Division, American University of Beirut Medical Center, Beirut, Lebanon
Background: Poor adherence to antihypertensive treatment remains a clinical challenge worldwide. The objectives of this study were to assess the adherence level to antihypertensive treatment and to identify its associated factors in a sample of hypertensive patients in Lebanon and Jordan.
Methods: We conducted an observational study between May 2011 and September 2012. A total of 1,470 eligible hypertensive patients were enrolled in our study and followed up for a period of 6 months. Data were collected regarding sociodemographic, health behavior, and hypertension-related characteristics. The adherence to treatment and the quality of life were self-reported using the Morisky, Green & Levine Scale and the Hypertension Quality of Life Questionnaire.
Results: Our results revealed that 55.9 % of the patients were adherent to their antihypertensive medication. Older age was associated with better adherence, whereas being divorced or widowed, having a poorer quality of life, and being classified as having stage 1 or 2 hypertension at the end of the study were all associated with poorer adherence.
Conclusion: Efforts should be exerted on all levels in order to increase the adherence to antihypertensive treatment through the implementation of educational campaigns.
Keywords: adherence, NC 7 guidelines, Morisky, Green & Levine Scale, Hypertension Quality of Life Questionnaire, Lebanon, Jordan
Introduction
Hypertension remains a global health challenge as its prevalence continues to grow rapidly in both developed and developing countries.1 This chronic condition requires long-term treatment, and is deemed responsible for 12.8% of deaths worldwide.2 Strong evidence from randomized controlled trials has revealed that treatment of high blood pressure significantly decreases cardiovascular disease (CVD)-associated morbidity and mortality.3,4 A recent clinical trial associated the reductions of 3.8 mmHg and 1.5 mmHg in systolic and diastolic pressure, respectively, to a 37% decrease in the development of left ventricular hypertrophy as well as a 50% decrease in CVD events.5 To achieve such positive outcomes, long-term adherence to antihypertensive treatment is essential.6 Over the last few years, new antihypertensive drugs with lower incidence of adverse events have been developed.7 Despite the significant improvement in medical therapies, the lack of adherence to these treatments remains a clinical challenge considering the serious health risks associated with high blood pressure and its heavy burden on the public health. Adherence is defined by the World Health Organization as “the extent to which a person’s behavior – taking medication, following a diet, and/or executing lifestyle changes – corresponds with agreed recommendations from a health care provider”.8 In fact, poor adherence has been widely recognized among patients on antihypertensive therapy. Consequently, despite appropriate diagnosis and drug prescription, considerable number of patients fail to benefit from the treatment; this results in poor health outcomes and lower quality of life.6–13 It is important to highlight the role of adherence in improving the outcome of antihypertensive treatments.14 Little is known in Lebanon and Jordan regarding treatment adherence and quality of life in hypertensive patients. We designed an observational study, with the primary objective of assessing antihypertensive treatment adherence in a cohort of hypertensive Jordanian and Lebanese patients newly diagnosed with hypertension, or patients diagnosed with uncontrolled essential hypertension according to the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure Guidelines criteria,7 and treated with antihypertensive medication for more than 6 months. The study also aimed at identifying potential factors that may alter adherence to antihypertensive treatment, including different therapeutic modalities.
This study provides unique multinational data and a valuable update on the current adherence to antihypertensive therapy in a hypertensive population from Jordan and Lebanon.
Methods
Study design and patients
We conducted an observational study in a cohort of hypertensive patients attending hospitals and private clinics in Lebanon and Jordan between May 2011 and September 2012. Hospitals and clinics were chosen to represent the private and public sectors as well as to cover rural and urban areas. The target survey population included subjects of either sex, aged above 21 years, newly diagnosed with hypertension, or uncontrolled on medication after being treated for 6 months or more. Subjects were approached by their treating physicians and asked about their willingness to participate in the study. Participants had to provide written informed consent and comply with the survey schedule. Exclusion criteria were secondary hypertension, acute illnesses, psychiatric diseases, pregnant women, nursing mothers, and subjects who were unable to provide informed consent. Ethics committee approval was obtained from the American University of Beirut Institutional Review Board and from the Jordan Hospital Institutional Review Board. Since there was no available literature on the prevalence of adherence among Lebanese and Jordanian hypertensive patients at the time of the study design, a 50% expected adherence rate was used. Considering a precision of 4% and a 95% confidence level, the minimum required sample size in each country was 601, and considering a 20% attrition rate the final calculated sample size was 720 subjects per country.
Participants
A total of 1,506 patients gave written informed consent to participate in the study, 750 from Jordan and 756 from Lebanon. Five participants from Jordan and 31 from Lebanon were excluded because they did not fulfill the inclusion criteria. The remaining 1,470 hypertensive patients, 745 from Jordan and 725 from Lebanon, were enrolled in the study.
Procedure
Patients were instructed on how to take their newly prescribed medication, but no interventions targeting adherence took place during the study. Data collection took place during three mandatory visits over 6 months. Patients were seen at study inclusion (V0), at an intermediate visit, 1–3 months after inclusion (VI), and at study end (VE). During the three visits, investigators completed a case report form including the patient’s personal information, the physical examination assessment, and the antihypertensive treatment and modality (drug class and monotherapy vs combined therapy). Information regarding the patient’s adherence to the antihypertensive treatment was collected during the final visit (VE), while data on quality of life were collected during the first and final visits. Data on sociodemographic characteristics (age, sex, nationality, marital status, education level, work experience, and health care system), family history of CVD, and clinical characteristics including medical history and comorbidities (ischemic heart disease, respiratory disease, and others) were also collected. Blood pressure measurements were classified into normal, prehypertension, stage 1 hypertension, and stage 2 hypertension based on the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure guidelines.7 The CVD risk was stratified into five categories: very low, medium low, medium high, high, and very high according to the National Cholesterol Education Program Adult Treatment Panel III guidelines.15 Patients’ identity was kept anonymous and was only accessible to the principal investigator.
Outcome measures
Morisky, Green & Levine Scale
Adherence was assessed using the Morisky, Green & Levine Scale.16 The scale consists of the following four close-ended questions, which could be answered by YES or NO: 1) Have you ever forgotten to take your medication? 2) Are you, at times, careless regarding the time to take your medication? 3) When you have felt good, have you ever stopped taking your medication? 4) Have you ever failed to take the medicine when you felt ill? A negative answer was graded 1, whereas a positive answer was graded 0. Subjects were considered adherent to treatment if they scored 4 on the Morisky, Green & Levine Scale, and non adherent to their treatment if they scored three or lower.
Health-related quality of life assessment
The Hypertension Quality of Life Questionnaire (MINICHAL)17 was used. MINICHAL consists of 17 items of which ten are pertinent to the domain of mental status, six to the domain of somatic manifestations, and a last one to the patient’s overall perception of his/her quality of life. Items are answered on a 4-point Likert scale ranging from 0 to 3: 0 (No, Never), 1 (Yes, At least once in the past week), 2 (Yes, At least once per day), and 3 (Yes, Several times per day). MINICHAL was created by adding all the scale item scores, and it ranged from 0 to 48 with a lower score indicating the best level of health.18
Statistical analysis
Statistical analyses were performed using the statistical software SPSS Inc. (version 17.0; Chicago, IL, USA). Mean values and standard deviations were used to describe continuous variables, whereas percentages were used to describe categorical variables. Student’s t-test was used for comparison of means, and Pearson chi-square test (c2) was used for comparison of proportions between groups. A P-value <0.05 was considered statistically significant. A multivariate analysis using logistic regression was carried out taking into account potential confounding variables that had a P-value< 0.1. The dependent variable was adherence to treatment and was binary (YES or NO). Adjusted odds ratios and their 95% confidence intervals were reported. Hosmer and Lemeshow test was used to assess the goodness-of-fit of the regression model. The dependent variable was adherence to treatment and was binary (YES or NO). Adjusted odds ratios (ORs) and their 95% confidence intervals (CIs) were reported.
Results
The study population consisted of 842 (57.3%) males and 628 (42.7%) females. Mean age was 54.7±13.1 years. Of the total, 622 were newly diagnosed with hypertension, and 848 patients had uncontrolled hypertension. The majority of the subjects (80%) were married, and almost half of them (47.7%) had secondary education. Of the total, 754 patients (55.9%) were adherent to treatment, while the remaining 596 (44.1%) were not (Table 1). After 6 months of follow-up, the percentage of patients with stage 2 hypertension decreased from 68% to 4.8%. In addition, the percentage of those fitting the high CVD risk category decreased from 7.2% to 2.8% (Table 2).
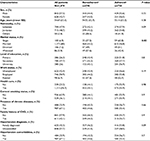  | Table 1 Baseline characteristics of hypertensive patients by adherence status Note: aSubjects were considered adherent to treatment if they scored 4 on Morisky, Green & Levine Scale and nonadherent to their treatment if they scored 3 or lower.16 P-values were generated from a chi square test in the case of qualitative variables and from a Student’s t-test in the case of quantitative variables. A P-value<0.05 was considered statistically significant. Statistically significant P-values are highlighted in bold. Abbreviations: SD, standard deviation; CVD, cardiovascular disease. |
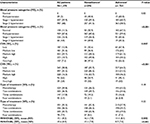  | Table 2 Blood pressure categories, cardiovascular risk stratification, antihypertensive treatment, and quality of life of patients by adherence status Notes: aSubjects were considered adherent to treatment if they scored 4 on Morisky, Green & Levine Scale and nonadherent to their treatment if they scored 3 or lower.16 Blood pressure measurements were classified based on the JNC7 guidelines.7 SBP/DBP (mmHg) <120/80: normal, 120–139/80–89: prehypertension, 140–159/90–99: stage 1 hypertension, 160–179/100–109: stage 2 hypertension. Cardiovascular risk was stratified into five categories according to the NCEP ATP III guidelines.15 P-values were generated from a chi square test in the case of qualitative variables and from a Student’s t-test in the case of quantitative variables. A P-value<0.05 was considered statistically significant. Statistically significant P-values are highlighted in bold. Abbreviations: VO, first visit; VE, final visit; CVS, Cardiovascular Score; MINICHAL, Hypertension Quality of Life Questionnaire; SD, standard deviation; JNC7, Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; SBP, systolic blood pressure; DBP, diastolic blood pressure; NCEP ATP III, National Cholesterol Education Program Adult Treatment Panel III. |
Mean score of the health-related quality of life (MINICHAL) was higher at the first visit (15.1±8.2) than at the final visit (8.7±7.6), suggesting a better quality of life after 6 months of antihypertensive treatment use (Table 2).
The bivariate analysis showed that marital status, blood pressure classifications, CVD risk stratification, and health-related quality of life were significantly associated with patient adherence. The percentage of adherent patients was the highest among single patients (62.8%) and the lowest among widowed patients (42.4%) (P=0.02) (Table 1). Adherence differed significantly by blood pressure categories as assessed at the end of the study (P<0.001). The percentage was the lowest (30.2%) among patients with stage 2 hypertension and the highest among normotensive (67.1%) and pre-hypertensive patients (59.4%). Patients who had a low CVD risk at V0 and VE were more likely to be adherent (67.4% and 64.3%, respectively). Moreover, mean MINICHAL scores at V0 (14.4±8.4) and VE (8.7±7.6) were lower among adherent patients suggesting a better quality of life (Table 2). On another note, results showed that adherence was not statistically associated with the modality of antihypertensive treatment (P>0.05).
After controlling for independent variables with P-value <0.1, only age, marital status, blood pressure categories at the end of the study, and health-related quality of life (MINICHAL) remained associated with adherence at the multivariate level. Older patients were more likely to be adherent to antihypertensive treatment (OR 1.01, 95% CI 1.00–1.02). Divorced (OR 0.30, 95% CI 0.15–0.62), and widowed (OR 0.33, 95% CI 0.15–0.70) patients were less likely to be adherent to treatment as compared to single patients. Patients categorized at the end of the study as having stage 1 (OR 0.35, 95% CI 0.19–0.64) or stage 2 (OR 0.47, 95% CI 0.23–0.94) hypertension were also less likely to be adherent as compared to those with normal blood pressure. An increase in the MINICHAL score was associated with lower odds of adherence (Table 3).
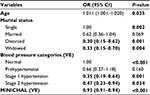  | Table 3 OR and 95% CI for factors associated with adherence in hypertensive patients Notes: Blood pressure measurements were classified based on the JNC7 guidelines.7 SBP/DBP (mmHg) <120/80: normal, 120–129/80–84: prehypertension, 140–159/90–99: stage 1 hypertension, 160–179/100–109: stage 2 hypertension. P-values were generated from the logistic regression of the adherence variables on the corresponding covariates. A P-value<0.05 was considered statistically significant. Statistically significant P-values are highlighted in bold. Abbreviations: OD, odds ratio; CI, confidence interval; VE, final visit; MINICHAL, Hypertension Quality of Life Questionnaire; JNC7, Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; SBP, systolic blood pressure; DBP, diastolic blood pressure. |
Discussion
This is the first report that evaluates adherence to treatment and its associated factors among hypertensive patients in Jordan and Lebanon. This study revealed a high percentage of low adherence to antihypertensive drug therapy in Jordan and Lebanon reaching 44%. Older age was associated with better adherence, whereas divorced and widowed status, as well as stage 1 and stage 2 hypertension, and poorer quality of life were associated with poorer adherence.
The adherence rate found in this study was lower than that reported in developed countries such as the US (91%)19 and Scotland (91%).20 Though the latter studies used different adherence assessment measurements, Morisky, Green & Levine Scale in the US and an objective assessment of adherence based on drug supply in Scotland, the observed difference with our study results might be due to the free access to medical care in these countries. However, adherence rate was higher than that in other developing countries such as Palestine (45.7%)21 and Saudi Arabia (27.9%),22 but lower to that in Pakistan (77%).23 The variation in antihypertensive adherence rate reported in developing countries could be explained by the lack of a standardized measurement of adherence, along with the variation in the sampling methodology. Though all the three studies used a subjective assessment of adherence; however, the Hill–Bone medication adherence scale, which was used in the study conducted in Saudi Arabia, not only assesses adherence to medication but also to other behaviors such as reduced sodium intake and appointment keeping. This could have been responsible for the very low adherence rate reported in Saudi Arabia. We found that adherence was significantly associated with age. Our finding is consistent with other papers published by Al-Sowielem and Elzubier, Hashmi et al, and Yiannakopoulou et al.24–26 This could be explained by the social dynamics of the Arab populations, which are mostly portrayed in close family ties, social support, and respect for the elders. In contrast to senior subjects, younger patients refute the need to be treated for hypertension once diagnosed and deny the necessity for regular drug use. This could be one of the many reasons that lead to drug adherence issues among this age group.27,28
Marital status was also found to affect adherence. Married participants were as adherent as single patients, while divorced and widowed subjects were less likely to be adherent. This is discordant with the results of a study conducted by Karaeren et al, which reported that married patients were more adherent to treatment (85%) compared to those who were not married (70%), suggesting that spousal help and support improved adherence.29 Adherence was associated with improved quality of life. The decrease in blood pressure to less than 120/80 mmHg was significantly more observed in adherent participants compared to nonadherent patients. Indeed, many publications supported the association between adherence to treatment and a controlled blood pressure26,30–32 as well as better health outcomes.33
Despite the abundance of literature reports describing the low rate of adherence among hypertensive patients, no immediate solution has been forwarded to answer this unmet need. However, appropriate follow-up and awareness should be offered to the patients for achieving better health outcomes. Health education by a multidisciplinary team should be provided to such patients.
Consistency of our findings with other literature, the relatively large sample size, the use of a validated tool (Morisky, Green & Levine Scale) to evaluate treatment adherence, and the adjustment for wide determinants of adherence including sociodemographic, clinical, and disease-related characteristics as well as health-related quality of life are all distinctive assets of our study. However, several limitations are worth mentioning, such as the possibility of selection bias secondary to the recruitment of participants from tertiary care hospitals and not from the general population, which limits the generalizability of our findings. Moreover, the reliance on self-reported adherence using Morisky questionnaire rather than on objective measures of adherence, such as drug counts or electronic monitoring, might introduce response bias. Another limitation is the absence of the direct assessment of drug tolerability, which can mask an important aspect that has been extensively shown to be related to adherence.34,35 Though drug tolerability was indirectly measured in the MINICHAL questionnaire, it would have been more informative to explicitly assess this concept in such studies exploring adherence to treatment.
Conclusion
Almost half of the study population was nonadherent to antihypertensive medication. Age, marital status, high blood pressure categories (stages 1 and 2), and health-related quality of life were found to be the main factors affecting adherence. Moreover, our study revealed that 6 months of adherence to antihypertensive treatment could improve quality of life as well as blood pressure level among hypertensive Middle Eastern patients.
Future studies should further investigate other sociocultural factors that may affect adherence. Based on the findings of this study, there is a need for planning and implementation of health education campaigns involving health care providers, patients, and the public, with the aim of increasing awareness, improving treatment of high blood pressure, and enhancing adherence to therapy.
Acknowledgments
We thank Professor Donald Morisky for his helpful review and editorial assistance. This study was supported by funding from AstraZeneca.
Disclosure
The authors report no conflicts of interest in this work.
References
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. | ||
Mathers C, Stevens G, Mascarenhas M. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. 2009. Available from: http://www.who.int/healthinfo/global_burden_disease/global_health_risks/en/index.html. Accessed August 15, 2014. | ||
Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet. 1997;350(9080):757–764. | ||
Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA. 1991;265(24):3255–3264. | ||
Verdecchia P, Staessen JA, Angeli F, et al. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): an open-label randomised trial. Lancet. 2009;374(9689):525–533. | ||
Burnier M. Long-term compliance with antihypertensive therapy: another facet of chronotherapeutics in hypertension. Blood Press Monit. 2000;5(1):S31–S34. | ||
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–1252. | ||
World Health Organization. Chapter XIII – Hypertension in Adherence to Long-Term Therapies-Evidence for Action. 2003:129–136. Available from: http://www.emro.who.int/ncd/Publications/adherence_report.pdf. Accessed March 5 2015. | ||
Eraker SA, Kirscht JP, Becker MH. Understanding and improving patient compliance. Ann Intern Med. 1984;100(2):258–268. | ||
Monane M, Bohn RL, Gurwitz JH, Glynn RJ, Levin R, Avorn J. Compliance with antihypertensive therapy among elderly Medicaid enrollees: the roles of age, gender, and race. Am J Public Health. 1996;86(12):1805–1808. | ||
Ren XS, Kazis LE, Lee A, Zhang H, Miller DR. Identifying patient and physician characteristics that affect compliance with antihypertensive medications. J Clin Pharm Ther. 2002;27(1):47–56. | ||
Lüscher TF, Vetter H, Siegenthaler W, Vetter W. Compliance in hypertension: facts and concepts. J Hypertens Suppl. 1985;3(1):S3–S9. | ||
Gusmão JL, Mion D Jr, Pierin AM. Health-related quality of life and blood pressure control in hypertensive patients with and without complications. Clinics. 2009;64(7):619–628. | ||
Cramer JA. Consequences of intermittent treatment for hypertension: the case for medication compliance and persistence. Am J Manag Care. 1998;4(11):1563–1568. | ||
Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486–2497. | ||
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. | ||
Roca-Cusachs A, Badia X, Dalfó A, et al. Relationship between clinical and therapeutic variables and health-related quality of life in patients with hypertension. MINICHAL Study. Med Clin (Barc). 2003;121(1):12–17. | ||
Badia X, Roca-Cusachs A, Dalfó A, et al. Validation of the short form of the Spanish Hypertension Quality of Life Questionnaire (MINICHAL). Clin Ther. 2002;24(12):2137–2154. | ||
Krousel-Wood M, Islam T, Webber LS, Re RN, Morisky DE, Muntner P. New medication adherence scale versus pharmacy fill rates in seniors with hypertension. Am J Manag Care. 2009;15(1):59–66. | ||
Inkster ME, Donnan PT, MacDonald TM, Sullivan FM, Fahey T. Adherence to antihypertensive medication and association with patient and practice factors. J Hum Hypertens. 2006;20(4):295–297. | ||
Al-Ramahi R. Adherence to medications and associated factors: a cross-sectional study among Palestinian hypertensive patients. J Epidemiol Glob Health. 2015;5(2):125–132. | ||
Alsolami F, Correa-Velez I, Hou X-Y. Factors affecting antihypertensive medications adherence among hypertensive patients in Saudi Arabia. Am J Med Sci. 2015;5(4):181–189. | ||
Hashmi SK, Afridi MB, Abbas K, et al. Factors associated with adherence to anti-hypertensive treatment in Pakistan. PLoS One. 2007;2(3):e280. | ||
Al-Sowielem L, Elzubier A. Compliance and knowledge of hypertensive patients attending PHC centers in Al-Khobar, Saudi Arabia. East Mediterr Health J. 1998;4(2):301–307. | ||
Hashmi SK, Afridi MB, Abbas K, et al. Factors associated with adherence to anti-hypertensive treatment in Pakistan. PloS One. 2007;2(3):e280. | ||
Yiannakopoulou ECh, Papadopulos JS, Cokkinos DV, Mountokalakis D. Adherence to antihypertensive treatment: a critical factor for blood pressure control. Eur J Cardiovasc Prev Rehabil. 2005;12(3):243–249. | ||
Cingil D, Delen S, Aksuoğlu A. Evaluation of compliance and level of knowledge of patients with hypertension living in Karaman city center, Turkey. Turk Kardiyol Dern Ars. 2009;37(8):551–556. | ||
Daniel AC, Veiga EV. Factors that interfere the medication compliance in hypertensive patients. Einstein (Sao Paulo). 2013;11(3):331–337. | ||
Karaeren H, Yokuşoğlu M, Uzun S, et al. The effect of the content of the knowledge on adherence to medication in hypertensive patients. Anadolu Kardiyol Derg. 2009;9(3):183–188. | ||
Elzubier AG, Husain AA, Suleiman IA, Hamid ZA. Drug compliance among hypertensive patients in Kassala, eastern Sudan. East Mediterr Health J. 2000;6(1):100–105. | ||
Lim TO, Ngah BA, Rahman RA, et al. The Mentakab hypertension study project. Part V--Drug compliance in hypertensive patients. Singapore Med J. 1992;33(1):63–66. | ||
Hershey JC, Morton BG, Davis JB, Reichgott MJ. Patient compliance with antihypertensive medication. Am J Public Health. 1980;70(10):1081–1089. | ||
Murphy J, Coster G. Issues in patient compliance. Drugs. 1997;54(6):797–800. | ||
Munger MA, Van Tassell BW, LaFleur J. Medication non-adherence: an unrecognized cardiovascular risk factor. MedGenMed. 2007;9(3):58. | ||
Elliott WJ, Plauschinat CA, Skrepnek GH, Gause D. Persistence, adherence, and risk of discontinuation associated with commonly prescribed antihypertensive drug monotherapies. J Am Board Fam Med. 2007;20(1):72–80. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
