Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Transverse Tibial Bone Transfer in the Treatment of Diabetes Foot Ulcer: A Pilot Study
Authors Wen R, Cheng X, Cao H, Zhang L, Luo F, Shang W
Received 23 March 2023
Accepted for publication 26 May 2023
Published 3 July 2023 Volume 2023:16 Pages 2005—2012
DOI https://doi.org/10.2147/DMSO.S413884
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Gian Paolo Fadini
Rongzhi Wen,* Xinhua Cheng,* Hong Cao, Lei Zhang, Fangcheng Luo, Wei Shang
Department of Orthopaedics, Renmin Hospital, Hubei University of Medicine, Shiyan, Hubei, 442000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Fangcheng Luo; Wei Shang, Email [email protected]; [email protected]
Background: The treatment of diabetes-related foot complications is a clinical challenge. The underlying complicating factors of peripheral vascular disease render most diabetic foot ulcers asymptomatic until the ulcer fails to heal and becomes clinically distinct, constituting a significant cause of disability and even death in diabetic patients.
Objective: To evaluate the clinical efficacy of tibial transverse transport (TTT) in the treatment of patients with diabetic foot ulcers.
Methods: A total of 35 patients who met the inclusion criteria were selected as the study group from patients with diabetic foot ulcers diagnosed and treated at our hospital between August 2019 and March 2021 and were treated with TTT, and 35 patients who also met the inclusion criteria were included in the routine group and were given conventional wound debridement. The primary endpoint of this study was clinical efficacy, including pain condition, trauma condition, ankle-brachial index, and peripheral nerve recovery.
Results: Patients receiving TTT showed significantly reduced visual analogue scale (VAS) scores than those with conventional treatment (P< 0.05). TTT resulted in a significant reduction of trabecular area and better trabecular healing versus conventional treatment (P< 0.05). TTT was associated with significantly higher ankle-brachial index (ABI) and lower Michigan neuropathy screening instrument (MNSI) scores in patients versus conventional debridement (P< 0.05).
Conclusion: TTT effectively alleviates the pain of diabetic foot ulcer patients, promotes wound healing, and improves ankle-brachial index and peripheral nerve recovery. In the context of the high amputation rate of diabetic foot ulcers treated by internal medicine, TTT contributes positively to the enhancement of patient prognosis and merits clinical promotion.
Keywords: tibial transverse transport, diabetic foot ulcer, clinical efficacy
Introduction
Diabetes is associated with a range of microvascular and macrovascular changes and their associated widespread complications.1 There are over 400 million patients with diabetes, with a prevalence of diabetic foot ulcers (DFU) being 12–15% among all diabetic cases. Common risk factors for the development of foot ulcers include poor glycemic control, peripheral neuropathy, peripheral vascular disease, and immunosuppression.2,3 Boulton reported that up to 85% of diabetic foot ulcers were attributable to altered foot pressure due to underlying peripheral neuropathy. According to relevant epidemiological statistics, approximately 50%-70% of lower extremity amputations are induced by diabetes mellitus. Diabetic foot ulcers are complex chronic traumas that significantly influence the morbidity, mortality, and quality of life of patients.
In recent years, the incidence of diabetic foot in China has been increasing year by year. With a prevalence rate of 8.1%, amputation rate of 22% and mortality rate of 11% among people over 50 years old, diabetic foot has constituted a serious public issue in China. The outcome of traditional bypass surgery and interventional treatment is undesirable, as evidenced by the high incidence of postoperative restenosis or occlusion. Peripheral vascular and neurological lesions in patients with diabetic foot ulcers severely delay wound healing and even cause amputation due to difficult repair. Therefore, effective reconstruction of the local blood supply and reduction of amputation rate are the keys to the management of diabetic foot ulcers.
At present, the major treatment for diabetic foot includes blood glucose control,4 surgical treatment mainly includes debridement, vascular intervention and arterial bypass graft,5 etc. Various topical products such as PDGF preparation, stem cell preparation,6 LeucoPatch patch,7 sucrose octasulphate dressing8 and related adjuvant treatments (eg nitric oxide generation device,9 hyperbaric oxygen,10 etc.) have yielded favorable outcomes, they however did not fundamentally change the pathological state of diabetic foot with ischemia and hypoxia, and a large number of patients with refractory diabetic foot have their limbs amputated eventually. Tibial transverse transport was proposed by Ilizarov, which was initially used to correct limb deformities and achieved promising results.11,12 It has been extensively used in the treatment of chronic osteomyelitis with the benefits of minimal invasiveness, improved microcirculation, and one-stage repair of bone and soft tissue defects. According to the tension-stress law of distraction osteogenesis, the bone and soft tissues of the lower limbs can be restored to active regeneration by appropriate stress stimulation using external fixators that slowly and regularly stretch the bone tissue.13 It has been reported that the Ilizarov technique can promote the healing of diabetic foot ulcers by increasing vascular endothelial growth factor and reconstructing microcirculation.12 In the area of osteotomy distraction, active microvascular network regeneration preceded osteogenesis, and angiography also confirmed the regeneration and reconstruction of “neovascularisation and microcirculation” in the osteotomy distraction area. Further studies have shown that the microvascular network is most actively regenerated at 7–21 d after bone removal, and that the slow and continuous pulling force stimulates cell proliferation and biosynthesis, based on which local blood vessels, bones, muscles and nerves are regenerated, thus promoting regeneration and healing of damaged tissues.14 Accordingly, the current study was performed to evaluate the clinical efficacy of tibial transverse transport (TTT) in the treatment of patients with diabetic foot ulcers.
Materials and Methods
Participants
The study was approved by the ethics committee of our hospital (No. 201903234) and was conducted following the principles of the Declaration of Helsinki. A total of 35 patients who met the inclusion criteria were selected as the study group from patients with diabetic foot ulcers diagnosed and treated at our hospital between August 2019 and March 2021 and were treated with TTT, and 35 patients who also met the inclusion criteria were included in the routine group and were given conventional wound debridement. All eligible patients were aged 18–80 years old. Undersigned written informed consent was obtained from all eligible patients.
Inclusion and Exclusion Criteria
Inclusion Criteria
1) Patients were clinically diagnosed with diabetes mellitus; 2) patients who met the characteristics related to diabetic foot and were diagnosed with Wagner grade 2 or above; 3) the trauma of the affected limb did not involve the ankle; 4) patients with a good nutritional status and can tolerate surgery’ 5) CTA was performed on both lower extremities and showed varying degrees of stenosis and poor blood flow in the affected extremities, with weak pulsation of the dorsalis pedis artery, which in severe cases could not even be palpated; 6) ankle brachial index <0.9 and transcutaneous oxygen pressure <60mmHg.
Exclusion Criteria
1) Patients with major diseases such as stroke and myocardial infarction; 2) hematological system diseases or autoimmune dysfunction; 3) other uncontrollable diabetic complications; 4) cognitive dysfunction or psychiatric abnormalities.
Dropout Criteria
1) Patients spontaneously dropped out and lost access; 2) who revoked their consent; 3) serious adverse reactions occurred, which prevented the continuation of the trial.
Treatment Method
Upon admission, basic information about all patients was collected, and biochemical tests and relevant clinical examinations were performed.
Tibial Transverse Transport
Patients were informed of the risks associated with the procedure and signed informed consent for the project and procedure prior to surgery. Patients were fasted and abstained from water 6 hours before surgery and prophylactic antibiotics were administered 30 minutes before surgery, followed by routine anesthesia after vital sign examination and blood glucose stabilization. At 10 and 30 cm below the tibial plateau of the affected limb, the external fixator pins were passed through the bilateral cortical fixators, and two 3–5 cm incisions were designed between the two external fixator pins, with an interval of 2 cm, so as to completely peel the periosteum. A 3 * 2 cm bone cortex was cut under each incision with a 0.8 m bone drill, and the external fixator pin was fixed in the middle of the bone, and the periosteum and subcutaneous tissue were sutured in situ. The foot diabetic foot wound was cleaned and repaired, and VSD negative pressure suction was performed if necessary. After surgery, the external fixator and wound were ligated, the dressing was changed regularly, and the patient was strictly bedridden to avoid increasing the weight bearing of the affected limb. On the 5th postoperative day, the external stent was moved outward and regular dressing changes were administered to the skin incisions and foot wounds. If necessary, debridement surgery was performed on the wound surface and regular anti-infective antibiotic therapy was administered to maintain stable blood glucose.
Routine Wound Debridement
Wound debridement was performed according to the condition of the patient’s foot, and drugs were applied directly to the wound surface and fixed with sterile gauze. Management of trauma was performed with regular dressing changes, antibiotics and other anti-infective treatments.
Outcome Measures
Postoperative Pain
The visual analogue scale (VAS) was used to assess the pain of all patients at different time points (before treatment, one month after treatment, three months after treatment, and six months after treatment). The scores ranged from 0–10, with higher scores indicating more severe pain.
Trauma Assessment
Trauma area reduction and trauma healing were evaluated in all patients. The healing status was classified as complete healing (healing with no limb loss), incomplete healing (incomplete healing with no limb loss), and amputation (limb loss), and was compared between the two groups.
Ankle-Brachial Index
The ankle-brachial index (ABI) was recorded for all patients before and after treatment. ABI is the ratio of maximum ankle systolic pressure to maximum brachial artery systolic pressure, with 0.9–1.3 for normal, 0.71–0.89 for mild ischemia, 0.5–0.7 for moderate ischemia, and <0.5 for severe ischemia.
Peripheral Nerve Recovery
The Michigan Neuropathy Screening Instrument (MNSI) was used to assess and record peripheral nerve recovery in all patients after treatment, with a score out of 5. A score higher than 2.5 indicated the presence of peripheral neuropathy. The scale was divided into five main items, namely foot appearance, foot ulcer, ankle reflex, foot thumb vibratory sensation, and monofilament tactile sensation.
Statistical Analysis
The data of this study were organized and analyzed using SPSS 22.0, and GraphPad Prism 8 was employed as the graphing software. Measurement data were expressed as mean ± standard deviation (x ̅ ± s) and examined using the t-test. Count data were expressed as the number of cases (rate) and tested using chi-square (x²) test. Statistically significant differences were indicated at P < 0.05.
Results
Baseline Clinical Profiles
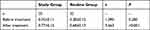
In the study group, there were 18 males and 17 females, aged 35–78 (55.21±6.37) years, with a duration of diabetes of 5–23 (13.94±7.56) years and a duration of diabetic foot ulcer of 15–60 (30.54±10.88) d. There were 15 patients with lesions on the left side and 20 on the right side, 12 patients with Wagner grade 2, 15 patients with grade 3 and 8 patients with grade 4. In the routine group, there were 19 males and 16 females, aged 33–79 (55.84±6.09) years, with a duration of diabetes of 5–22 (13.46±7.79) years and a duration of diabetic foot ulcer of 15–58 (30.79±10.17) d. There were 14 patients with lesions on the left side and 21 on the right side, 11 patients with Wagner grade 2, 14 patients with grade 3 and 10 patients with grade 4. The baseline clinical profiles of the two groups of patients were comparable (P>0.05) (Table 1).
 |
Pain
The VAS scores of patients in the study group were (6.68±2.41) before treatment, (2.08±1.01) one month after treatment, (1.56±0.87) three months after treatment, and (1.03±0.54) six months after treatment. The VAS scores of routine group patients were (6.71±2.16) before treatment, (3.94±1.95) one month after treatment, (3.15±1.37) three months after treatment and (2.48±1.08) six months after treatment. Patients receiving TTT showed significantly reduced VAS scores than those with conventional treatment (P<0.05) (Figure 1).
 |
Figure 1 VAS scores. Note: *Indicates P<0.05. |
Trauma Condition
The reduction rate of trauma area in the study group was (89.64±5.23), with 22 cases of complete healing, 13 cases of incomplete healing, and 0 cases of amputation. The reduction rate of trauma area in routine group patients was (70.11±8.79), with 9 cases of complete healing, 23 cases of incomplete healing, and 3 cases of amputation. TTT resulted in a significant reduction of trabecular area and better trabecular healing versus conventional treatment (P<0.05) (Table 2).
 |
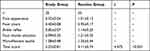
ABI
The ABI in the study group was (0.35±0.11) before treatment and (0.77±0.15) after treatment. The ABI in the routine group was (0.38±0.12) before treatment and (0.68±0.13) after treatment. TTT was associated with a significantly higher ABI in patients versus conventional debridement (P<0.05) (Table 3).
 |
Peripheral Nerve Recovery
In the study group, the foot appearance score was (0.53±0.04), the foot ulcer score was (0.40±0.08), the ankle reflex score was (0.82±0.07), the foot thumb vibration score was (0.99±0.25), the monofilament tactile score was (1.08±0.48), and the total score was (3.23±0.81). The routine group patients had a foot appearance score of (1.01±0.12), foot ulcer score of (0.95±0.17), ankle reflex score of (1.14±0.25), thumb vibration score of (1.21±0.35), monofilament tactile score of (1.35±0.44), and total score of (4.11±0.74). TTT resulted in significantly lower MNSI scores in patients versus conventional debridement (P<0.05) (Table 4).
 |
Discussion
The underlying pathophysiology of diabetic foot ulcers is a complex interaction between the body’s persistent hyperglycemic state and neuropathic, vascular, and immune system components.14 The presence of pathogenic factors such as hyperglycemia, hyperlipidemia, and hyperglycoprotein in diabetic patients leads to decreased blood fibrinolytic activity, increased platelet adhesion, ischemic necrosis of the distal lower extremity, and peripheral neuropathy. The occurrence of mechanical foot injuries wounds is refractory to healing and prone to infection, leading to diabetic foot.15 Clinical prevention strategies in the form of patient education and regular foot assessment for peripheral vascular disease and neuropathy, as well as risk stratification, are commonly used for diabetic foot disease management.16,17 Patients with diabetic foot ulcers usually exhibit significant clinical complexity, and chronic trauma is a major clinical concern. Wound healing in diabetic foot ulcers is impaired and delayed, and disease progression even leads to amputation.18,19 The restoration of adequate blood supply to the foot and the reconstruction of limb microcirculation are the keys to limb preservation treatment.
Multidisciplinary comprehensive treatment is clinically encouraged for the management of diabetic foot ulcers, such as glycemic control, improvement of circulation, local debridement and drug exchange, anti-infection, and neurotrophy. Multiple therapies have been designed, such as endovascular stenting, percutaneous endovascular angioplasty, and lower extremity vascular bypass grafting, which, however, only improve the blood supply to the affected area and provide poor clinical results. Ilizarov reported that continuous slow traction stimulation could promote local tissue regeneration.20,21 Currently, TTT has been extensively employed in the treatment of infectious osteomyelitis, but its use in the treatment of diabetic foot ulcers has scarcely been reported.
The results of the present study showed that TTT resulted in significantly reduced VAS scores, a more marked reduction of trabecular area, and better trabecular healing versus conventional treatment, and TTT was associated with significantly higher ABI and lower MNSI scores in patients versus conventional debridement, suggesting the high feasibility of TTT in the management of diabetic foot ulcers. The action of repeated mechanical stretching of the transverse tibial bone transport stimulated blood vessel regeneration and improved blood circulation in the leg and foot to promote the healing of the diabetic foot wounds. A related review suggests that the biochemical basis of ulcers is the result of a combination of components that lead to tissue breakdown. Persistent hyperglycemia causes a complex formation of advanced glycosylation end products and cytokines that cause oxidative stress in nerve cells and lead to motor, autonomic and sensory neuropathy called pudendal ulcers. In addition, alterations in autonomic nerves and skin insensitivity impair sweat gland function, leading to further formation of healing tissue, which compromises gait mechanisms. Traditional treatments only target the infected wounds of diabetic foot, including the use of antibiotics, cleaning the wounds, removal of necrotic tissues, and adequate flushing of the infected wounds, so as to potentiate the treatment effect. Nonetheless, traditional interventions fail to provide sufficient infection control, resulting in inadequate treatment efficiency. It has been suggested that repeated pressure on the diabetic foot is associated with healing tissue formation, and in the present study, the patients in the routine group received routine debridement. Removal of necrotic and hyperkeratotic tissue by means of superficial ulcer debridement or selective acral debridement can thus promote wound healing. However, it has also been argued that deeper wounds, especially those involving bone and soft tissue, require more aggressive debridement, such as surgical interventions.
The results of Liu et al showed that TTT improves blood flow and promotes vascular regeneration and wound healing in the treatment of stage 3 and 4 diabetic foot, which is consistent with the results of the current study. Compared to conventional treatments, TTT offers more benefits in the treatment of microcirculatory wall stenosis, occlusion and microcirculation because of the slow, horizontal and continuous traction tension applied at the tibial axial window to promote nerve and vascular regeneration in the motor area and its distal part, increase the number of distal microvessels or small vessels and improve blood supply to the distal tissues. It thus lays the foundation for the resolution of diabetic neuropathy and tissue ischemic necrosis.22,23 Furthermore, it is characterized by unique biochemical effects that remarkably improve microcirculation, including microcirculatory reconstruction and microcirculatory collateral circulation.24 Studies have shown that TTT induces differentiation of bone marrow stem cells into three major growth factors including vascular growth factor, epidermal growth factor and nerve cell growth factor mainly through complex biochemical reactions. It is the use of vascular growth factors to promote the repair and reconstruction of microcirculation and microcirculation, establish collateral circulation, improve local blood flow, fundamentally cure blood flow recalcitrant diabetic foot tissue necrosis and refractory infection, and hence achieve chronic wound control and healing.25 Moreover, continuous stretching of the bone window with an external fixator after surgery mobilizes the full natural repair potential of the tissue, promotes cell proliferation and biosynthesis, accelerates tissue metabolism, and facilitates the growth of fascia, muscles, nerves, and capillaries attached to the bone.26
This study has the following limitations, including a small sample size, short follow-up time, and lack of multiple surgical procedures, which may lead to the risk of bias. Further trials with larger sample size and long-term follow-ups are required to provide more reliable data.
Conclusion
TTT effectively alleviates the pain of diabetic foot ulcer patients, promotes wound healing, and improves ankle-brachial index and peripheral nerve recovery. In the context of high amputation rate of diabetic foot ulcers treated by internal medicine, TTT contributes positively to the enhancement of patient prognosis and merits clinical promotion.
Data Sharing Statement
All data generated or analysed during this study are included in this published article.
Ethics Approval and Consent to Participate
This study has been approved by ethics committee of Renmin Hospital, Hubei University of Medicine. Patients and their families were informed of the research content and voluntarily signed the informed consent. All the methods were carried out in accordance with the Declaration of Helsinki.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This study was supported by: The general health research project of Hubei Provincial Health Commission from 2021-2022: Experimental study on BMP-2 combined with autologous BMSCs to promote tendon bone healing after anterior cruciate ligament reconstruction (No: WJ2021M052); Key open project of Hubei Provincial Key Laboratory of Wudang Characteristic Chinese Medicine Research (Hubei Medical College): Research on the mechanism of trillium saponin inhibiting the proliferation of MG63 human osteosarcoma cells (No: WDCM2020003); Guiding project of Shiyan Science and Technology Bureau (22Y51): application of platelet rich gel combined with membrane induction technology in bone defects; Hubei Provincial Health Commission's 2021-2022 Health Research General Project (No: WJ2021M052): Experimental Study on BMP-2 Combined with Autologous BMSCs to Promote Tendon Bone Healing after Anterior Cruciate Ligament Reconstruction Surgery.
Disclosure
The authors declare that they have no competing interests.
References
1. Ghotaslou R, Memar MY, Alizadeh N. Classification, microbiology and treatment of diabetic foot infections. J Wound Care. 2018;27(7):434–441.
2. Eraydin Ş, Avşar G. The effect of foot exercises on wound healing in type 2 diabetic patients with a foot ulcer: a randomized control study. J Wound Ostomy Continence Nurs. 2018;45(2):123–130.
3. Izadi M, Kheirjou R, Mohammadpour R, et al. Efficacy of comprehensive ozone therapy in diabetic foot ulcer healing. Diabetes Metab Syndr. 2019;13(1):822–825.
4. Cianci PE. The treatment of diabetic foot ulcers: a historical perspective. Undersea Hyperb Med. 2018;45(2):225–229. doi:10.22462/03.04.2018.10
5. Uçkay I, Gariani K, Pataky Z, et al. Diabetic foot infections: state-of-The-art. Diabetes Obes Metab. 2014;16(4):305–316. doi: 10.1111/dom.12190
6. Cruciani M, Lipsky BA, Mengoli C, et al. Granulocyte-colony stimulating factors as adjunctive therapy for diabetic foot infections. Cochrane Database Syst Rev. 2009;3:CD006810.
7. Game F, Jeffcoate W, Tarnow L, et al. LeucoPatch system for the management of hard-to-heal diabetic foot ulcers in the UK, Denmark, and Sweden: an observer-masked, randomised controlled trial. Lancet Diabetes Endocrinol. 2018;6(11):870–878. doi:10.1016/S2213-8587(18)30240-7
8. Edmonds M, Lázaro-Martínez JL, Alfayate-García JM, et al. Sucrose octasulfate dressing versus control dressing in patients with neuroischaemic diabetic foot ulcers (Explorer): an international, multicentre, double-blind, randomised, controlled trial. Lancet Diabetes Endocrinol. 2018;6(3):186–196. doi:10.1016/S2213-8587(17)30438-2
9. Edmonds ME, Bodansky HJ, Boulton AJM, et al. Multicenter, randomized controlled, observer-blinded study of a nitric oxide generating treatment in foot ulcers of patients with diabetes-ProNOx1 study. Wound Repair Regen. 2018;26(2):228–237. doi:10.1111/wrr.12630
10. Dong S, Huang D, Zhu L, et al. 负压封闭引流联合胫骨横截骨移植治疗糖尿病足 [Treatment of diabetic foot with vacuum sealing drainage combined with transverse tibial bone transport]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2020;34(7):869–873.
11. Zhao X, Liu L, Yuan Q, et al. 糖尿病足胫骨横向运输研究进展 [Research progress of tibial transverse transport for diabetic foot]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2020;34(8):969–973. Chinese.
12. Zhen P, Chen Y, Gao W, et al. 应用Ilizarov技术治疗糖尿病足的疗效观察并发全身炎症反应综合征 [The effectiveness of Ilizarov technique-based transverse tibial bone transport on treatment of severe diabetic foots complicated with systemic inflammation response syndrome]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2018;32(10):1261–1266. Chinese.
13. Guo B, Zhao W, Wu H, et al. 伊利扎罗夫跖骨延长术治疗糖尿病足溃疡合并慢性骨髓炎跖骨头 [Ilizarov metatarsal bone lengthening in treatment of diabetic foot ulcer complicated with chronic osteomyelitis of metatarsal head]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2020;34(8):1000–1004. Chinese.
14. Reardon R, Harding KG. The diabetic foot ulcer. Aust J Gen Pract. 2020;49(5):250–255.
15. Monteiro-Soares M, Boyko EJ, Jeffcoate W, et al. Diabetic foot ulcer classifications: a critical review. Diabetes Metab Res Rev. 2020;36(Suppl 1):e3272.
16. Bandyk DF. The diabetic foot: pathophysiology, evaluation, and treatment. Semin Vasc Surg. 2018;31(2–4):43–48.
17. Lavery LA, Davis KE, Berriman SJ, et al. WHS guidelines update: diabetic foot ulcer treatment guidelines. Wound Repair Regen. 2016;24(1):112–126.
18. Lim JZ, Ng NS, Thomas C. Prevention and treatment of diabetic foot ulcers. J R Soc Med. 2017;110(3):104–109.
19. Wang Y, Shao T, Wang J, et al. An update on potential biomarkers for diagnosing diabetic foot ulcer at early stage. Biomed Pharmacother. 2021;133:110991.
20. Chinese Orthopaedic Physicians Association. Chinese Bone Moving Diabetic Foot Association, [Expert consensus on the treatment of diabetic foot ulcers using tibial transverse transport (2020)]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2020;34(8):945–950.
21. Zhang X, Dong T, Yao S, et al. Application of transverse tibial bone transport and microcirculation reconstruction in the treatment of diabetic foot ulcer: a case report. Ann Palliat Med. 2021;10(7):8358–8364.
22. Sun Y, Xiao YG, Wang H. 胫骨横向移位治疗糖尿病足溃疡 [Transverse tibial bone movement for the treatment of diabetic foot ulcers]. Zhongguo Gu Shang. 2018;31(10):949–952. Chinese.
23. Akkurt MO, Demirkale I, Öznur A. Partial calcanectomy and Ilizarov external fixation may reduce amputation need in severe diabetic calcaneal ulcers. Diabet Foot Ankle. 2017;8(1):1264699.
24. Liu Z, Xu C, Yu YK, et al. Twenty Years Development of Tibial Cortex Transverse Transport Surgery in PR China. Orthop Surg. 2022;14(6):1034–1048.
25. Jia ZW, Yu JP, Su YX, et al. 胫骨横截骨内固定联合负压引流治疗慢性疲劳综合征的临床疗效分析 [Clinical efficacy analysis of transverse tibial bone transport combined with vacuum drainage for the treatment of diabetic foot ulcer]. Zhongguo Gu Shang. 2018;31(3):232–236. Chinese.
26. Li H, You J, Liu C, et al. 胫骨横截骨移植治疗糖尿病足溃疡的疗效 [Effectiveness of transverse tibial bone transport in treatment of diabetic foot ulcer]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33(1):23–27. Chinese.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




