Back to Journals » Patient Preference and Adherence » Volume 16
Translation, Cultural Adaptation and Validation of the Hill Bone Compliance to High Blood Pressure Therapy Scale to Nepalese Language
Authors Shakya R , Shrestha R , Shrestha S , Sapkota P, Gautam R, Rai L, Khatiwada AP , Ranabhat K , KC B , Sapkota B , Khanal S , Paudyal V
Received 4 December 2021
Accepted for publication 14 February 2022
Published 8 April 2022 Volume 2022:16 Pages 957—970
DOI https://doi.org/10.2147/PPA.S349760
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Naifeng Liu
Rajina Shakya,1,* Rajeev Shrestha,2,* Sunil Shrestha,3,* Priti Sapkota,1 Roshani Gautam,4 Lalita Rai,4 Asmita Priyadarshini Khatiwada,5 Kamal Ranabhat,6,7 Bhuvan KC,3 Binaya Sapkota,8 Saval Khanal,9 Vibhu Paudyal10
1Department of Nursing, Nobel College, Kathmandu, Province Bagmati, Nepal; 2Department of Pharmacy, District Hospital Lamjung, Lamjung, Province Gandaki, Nepal; 3School of Pharmacy, Monash University Malaysia, Subang Jaya, Selangor, Malaysia; 4Department of Nursing, Tribhuvan University, Maharajgunj Nursing Campus, Kathmandu, Nepal; 5Department of Pharmaceutical and Health Service Research, Nepal Health Research and Innovation Foundation, Lalitpur, Province Bagmati, Nepal; 6Center Department of Public Health, Institute of Medicine, Tribhuvan University, Maharajgunj, Kathmandu, Nepal; 7Ministry of Health and Population, Kathmandu, Nepal; 8Department of Pharmaceutical Sciences, Nobel College, Affiliated to Pokhara University, Kathmandu, Province Bagmati, Nepal; 9Division of Health Sciences, Warwick Medical School, University of Warwick, Coventry, UK; 10School of Pharmacy, Institute of Clinical Sciences, College of Medical and Dental Sciences, University of Birmingham, Birmingham, UK
*These authors contributed equally to this work
Correspondence: Rajeev Shrestha, Department of Pharmacy, District Hospital Lamjung, Besisahar, Province Gandaki, Nepal, Tel +977 9845445205, Email [email protected] Sunil Shrestha, School of Pharmacy, Monash University Malaysia, Jalan Lagoon Selatan, Subang Jaya, Selangor, Malaysia, Tel +60 102874113, Email [email protected]
Background: Control of high blood pressure and prevention of cardiovascular complications among hypertensive patients depends on patients’ adherence to therapy. The Hill–Bone Compliance to High Blood Pressure Therapy Scale (HBCTS) is one of the most popular scale to assess hypertensive patients’ adherence behaviour. Unfortunately, no questionnaire in the Nepalese language is available to date to assess adherence to anti-hypertensive therapy.
Aim: To translate, culturally adapt and validate the English original version of the HBCTS into Nepalese language to measure treatment adherence of Nepalese hypertensive patients.
Methods: The cross-sectional study was conducted to translate, culturally adapt and validate the HBCTS into Nepalese version. The standard translation process was followed and was evaluated among 282 hypertensive patients visiting selected primary healthcare centers (PHCCs) of Kathmandu district, Nepal. Cronbach’s alpha was measured to assess the reliability of the tool. Exploratory factor analysis using principal component analysis with varimax rotation was used to evaluate structural validity.
Results: The mean±SD age of 282 participants was 58.49± 12.44 years. Majority of participants were literate (75.2%), and consumed at least one anti-hypertensive medication per day (85.5%). Nearly half (42.2%) of the participants had a family history of hypertension, and almost half (48%) of them had comorbid conditions. Mean ±SD score for overall adherence was 17.85± 3.87 while those of medication taking, reduced salt taking, and appointment keeping subscales were 10.63± 2.55, 4.16± 1.12 and 3.06± 1.07, respectively. Kaiser Meyer Olkin (KMO) was found to be 0.877. Exploratory factor analysis revealed a three-component structure; however, the loading of components into medication adherence, reduced salt intake and appointment keeping constructs were not identical to the original tool. Cronbach’s alpha score for the entire HBCTS scale was 0.846.
Conclusion: The translated Nepali version of the HBCTS demonstrated acceptable reliability and validity to measure adherence to antihypertensive therapy among hypertensive patients in clinical and community settings in Nepal.
Keywords: cultural adaptation, Hill–Bone scale, hypertension, Nepal, treatment adherence, translation
Introduction
Cardiovascular diseases (CVDs) contribute to approximately 17.9 million global deaths annually.1 More than half of these deaths are due to complications of hypertension (HTN).2 Each year, HTN is estimated to cause 10 million preventable deaths worldwide and is expected to lead to 23 million by 2030 AD.3,4 Ibrahim et al, reported that the distribution of the population with HTN increases in developing countries than in developed countries.5 HTN is a crucial preventable risk factor for major cardiovascular disease-associated complications and death.6
Anti-hypertensive medication is one of the key measures to manage HTN to an optimal level and mitigate adverse outcomes related to CVDs.5,7 Despite improvements in its detection and treatment since the 1970s, studies showed that 60–75% of treated hypertensive patients do not reach the recommended target blood pressure.8 In recent years, the incidence and prevalence of HTN have increased while rates of HTN control have declined. To assess HTN control among patients under treatment, American Heart Association has updated blood pressure targets as reduction in blood pressure by at least 20/10 mmHg or ideally to <130/80 mmHg.9,10 One of the major factors for ineffective control of blood pressure is non-adherence. According to World Health Organization (WHO), at least 50% of patients diagnosed with HTN do not take their anti-hypertensive medication as prescribed.8 Moreover, various studies have concluded that medication adherence behaviour in hypertensive patients is not satisfactory11–14 and vary greatly in different countries such as 30.2% in European country,11 34.9% in China,15 38.6% in India,16 24.9% in Ethiopia,17 27.9% in Saudi Arabia,12 85% in Lebanon14 and 43.5– 72% in Nepal.13,18
Treatment adherence is essential for effective control of HTN19 and several methods are available to assess the patient’s adherence behavior. The most effective biological methods (measuring drug level in plasma) are relatively costly and impractical for use in large populations and clinical settings.20,21 Therefore, physicians’ estimates and patients’ self-reports are more practical to assess their adherence level.22 Different medication adherence self-report scales have been developed and used in different therapeutic settings.20,21,23,24 One of the frequently used scales for hypertensive patients is the Hill Bone Compliance to high blood pressure Therapy Scale (HBCTS) developed by Kim et al.22
The Hill Bone scale (HBCTS) based on patient’s self-report was designed in the form of a rating scale for use by health care professionals to assess patients’ adherence to anti-hypertensive therapy in three main domains: i) medication-taking ii) salt intake restriction, and iii) appointment keeping.22,25 Control of hypertension depends on adherence to salt restriction, regular medication and follow-up; thus, assessing adherence to all these behaviors is essential among hypertensive patients. The psychometric properties of HBCTS have been evaluated in several countries, including Poland,26 Namibia,27 Korea,28 Turkey,25 Portugal29 and Saudi Arabia12 and found that scale was suitable for use in primary care settings.22,25,27,29 Though, the German and Persian versions of HBCTS were unreliable and not valid enough to use among the general population,21,30 some studies found sufficient internal consistency and validity of medication-taking subscale only.31,32
May Measurement Month 2019, a screening campaign conducted in 30 districts of Nepal, reported that 27.5% of the total participating population had hypertensive blood pressure in Nepal. Among them, only 37.5% regularly took anti-hypertensive medication and blood pressure was under control only in 54.3% of those taking anti-hypertensive medication.33 STEPwise Approach to NCD Risk Factor Surveillance (STEPS) survey Nepal reported that almost 90% of the diagnosed hypertension were not treated.34
In Nepal, few studies have been conducted to assess adherence to anti-hypertensive therapy using various tools, however, those tools were not reported to translate into Nepalese language, checked cultural acceptability and carried validity testing.13,18,35 Although the general medication adherence measurement scale has been recently validated among Nepalese patients,36 there is a lack of a specialized valid, reliable, and concise scale to measure medication adherence among Nepalese patients with hypertension. Variation in knowledge level, cultural diversity, lifestyle and socioeconomic statuses among the Nepalese population may affect the adherence level. A valid, reliable and efficient measurement tool is needed to assess the level of adherence to HTN treatment among the Nepalese population. Thus, we aimed to undertake the translation, cultural adaptation, and validation of the English version of HBCTS into Nepalese language among hypertensive patients.
Methods
Study Design and Settings
The cross-sectional study was conducted to translate, culturally adapt, and validate the English version of the HBCTS (see Appendix 1a), developed by Kim et al, into Nepali language.22
The study was conducted among patients visiting four randomly selected primary Healthcare centres (PHCCs) of Kathmandu district, namely Sangla PHCC, Bishnudevi PHCC, Gokarneswor PHCC and Ramghat PHCC. Kathmandu is the capital and the largest metropolitan city of Nepal with social, ethnic and cultural diversities that cover the largest urban agglomeration in the Kathmandu valley.37 Kathmandu district has eight PHCCs38 at the local level to provide essential health care services, public awareness, health education and promotion for lifestyle modification, health screening, and monitoring programs to prevent NCDs. Also, anti-hypertensive medications, and regular BP monitoring services are targeted to the patients with HTN. On average, 30–40 patients visited each PHCC per day for various reasons during the study period. In addition, approximately 5–6 patients came for BP monitoring or follow up for anti-hypertensive therapy.
Study Population, Inclusion and Exclusion Criteria
Native Nepalese patients (18 years and above) diagnosed with HTN (confirmed by the clinical information and diagnosis made in the OPD ticket of visited patients) and who were under anti-hypertensive therapy for at least six months and who visited selected PHCCs in Kathmandu district between March to May 2021 were enrolled in the study using a convenience sampling technique. Participants who were not interested and not taking hypertensive medication even if he/she was diagnosed with hypertension by healthcare personnel were excluded from the study. Healthcare personnel of PHCCs measured BP of the patients using aneroid sphygmomanometer, and based on their BP reports, they were diagnosed in their respective OPD card as hypertensive or not. Patient’s OPD card was taken to confirm hypertensive patients, and those confirmed were selected for the study.
For exploratory factor analysis, most studies performed a subject-to-item ratio of (5–20):1 as the rule of thumb.26,30,39 This ratio gives 70% correct factor structure. Thus, the sample size for this study was calculated based on the 20:1 ratio.40 As there are total 14 items in the HBCTS, sample size was calculated as 280 (14*20).
Ethical Consideration
The ethical approval for the study was taken from the Institutional Review Committee of Nobel College, Kathmandu, Province Bagmati, Nepal (approval ID: Ref. IRC330/2020). Official administrative permission was obtained from the respective PHCCs and the municipalities. The study was conducted in accordance with the Declaration of Helsinki. Total 282 participants were informed about the aims of the study, and both written and verbal informed consents were taken from them before they were enrolled in the study. Participants were also assured about their voluntary participation, anonymity, and confidentiality of information. Consent from the participating experts was also taken to form an expert review committee in written form.
Research Instrument
The instrument used for this study included questionnaire with socio-demographic (age, sex, religion, marital status, education, occupation),health-related data (current BP status, duration of diagnosis and medication use) and Hill-Bone Compliance to High Blood Pressure Therapy Scale (HBCTS).
The HBCTS was developed by Kim et al in 2000, which consists of 14 items, divided into 3 subscales: medicine taking (9 items), reduced salt intake (3 items) and appointment-keeping (2 items). Every item of the tool is scored on four-point Likert scale (1= none of the time, 2= some of the time, 3= most of the time and 4 = all of the time). The total score ranges from the lowest 14 to the highest 56. A score of 14 represents perfect adherence, and a score greater than 14 represents non-perfect adherence.22 Item 6 ie, “How often do you make the next appointment before you leave the doctor’s office?” needed reverse scoring.
Translation and Cultural Adaptation
After receiving permission from the original developer of the English version of the HBCTS, the tool was translated into Nepalese-language. The standard translation process, ie, WHO process of translation and adaptation of instruments based on four steps, was adopted.41
Forward translation: Two native Nepali-English bilingual translators, having previous translation experiences, independently translated the English version of the scale to its corresponding Nepalese version. Third bilingual translator, along with the translation coordinator, reconciled both translations and resolved any discrepancies.
Backward translation: The reconciled version was then translated into English by two bilingual translators with medical background and who were blinded to the original questionnaire.
Expert panel discussion: Expert panel was formed by the study team for cultural adaptation. An expert committee comprised of Nursing professors, lecturers, and pharmacy academicians. The back-translated versions were discussed, reviewed, and compared with the original version among the expert panel. Based on discussion and experts’ opinions, improvements were made to develop a culturally acceptable version of the tool. The panel approved the Nepalese version of the tool for pre-testing after reaching a consensus.
Pre-testing: In the last step, pre-testing and cognitive interviewing of the translated tool were done. After pre-testing, the data collectors’ comments and suggestions were reviewed, discussed with the experts’ team, and the wording, grammatical and typographic errors were corrected. Then, the final revised pre-tested version of the translated tool was subjected to psychometric analysis (see Appendix 1b).
Nepalese version of the HBCTS tool was generated through the processes of translation and cultural adaptation, with no significant difficulties during the process. However, some minor changes were made to maintain the integrity of the questions. Pre-testing also showed no difficulties among participants to understand all questions of the translated tool. Finally, the expert panel reviewed the translated tools for cultural adaptation.
Validity and Reliability Analysis of the Tool
Face Validity
The face validity of the Nepali Version of the HBCTS tool was based on pre-testing feedback. Pretesting was conducted among 32 patients visiting the outpatient department of a community Hospital (Council of community health services) in Kathmandu to verify the clarity and understandability of the translated Nepalese version of the tool. Participants were asked if they had any difficulty or confusion in understanding the questionnaire, and were also approached for any suggestions to improve the quality of the questionnaire. None of the participants reported any disagreement and difficulties in understanding the questionnaire, while some suggested minor changes in words to enhance the clarity of the questionnaires. All of their suggestions were taken into consideration and addressed while revising the questionnaires.
Content Validity
The original HBCTS tool was evaluated for content validity and used to measure treatment adherence in many studies.26,27,32 However, to maintain the content validity of the translated tool in the Nepalese context, it was subjected to subject experts in Nepal, who were medical and nursing professors. The opinion and views of the experts were analysed, and the tool was revised accordingly with minor language corrections.
Construct Validity
The construct validity of the Nepalese version of the HBCTS was evaluated with exploratory factor analysis (EFA) using principal component extraction with varimax rotation on 14 items of the scale. Eigen values associated with each factor was analysed before extraction. Factors having more than 1 eigen value were extracted. A scree plot was further used to confirm the number of factors.
Known Group Validity
It was hypothesized from previous findings that medication non-adherence among hypertensive patients was significantly associated with the patient having more than one medication per day and the patient taking medication for more than 10 years in Nepal.13,18 As there was no cut off value in the HBCTS, the patient adherence level was divided into perfect adherence (score 14) and non-perfect adherence (score >14). Chi-square test was used to evaluate the association between perfect medication adherence (both overall treatment adherence and medicine taking adherence subscale) and more than one medication user and patients taking hypertensive medication for more than 10 years. A p-value less than 0.05 was considered statistically significant.
Data Collection and Statistical Analysis
Eligible patients visiting PHCCs were approached for data collection. First, participants were explained about the study objectives and written informed consent was obtained from them. Then, the trained enumerators collected data. Literate participants were allowed to complete the questionnaire themselves, while the enumerator facilitated participants who asked for support to complete the questionnaire. Personal and health-related data were collected in the convenient area, and BP was reported from their hospital OPD card.
Statistical analysis, including EFA, was performed using the Statistical Package for Social Science (SPSS) version 25. Socio-demographic and health-related data were analysed using descriptive statistics such as mean ± standard deviation, frequency, and percentage. Cronbach’s alpha coefficient was used to measure the internal consistency and reliability of the items in the scale. A coefficient value greater than 0.70 indicated a high level of internal consistency.42
The sampling adequacy and appropriateness of data for factor analysis were assessed by estimating Kaiser-Meyer-Olkin (KMO) statistics and Bartlett’s test of sphericity; KMO has to be more than 0.5 to be considered acceptable.43
Results
Socio-Demographic Characteristics of Respondents
Out of 282 respondents under anti-hypertensive therapy, 52.5% were male. Mean age±SD was 58.49±12.44 years. Majority of respondents were residing at urban residence (62.8%) and were married (89.4%) and living with a spouse (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Respondents (n =282) |
Health-Related Characteristics of Respondents
Of the respondents, 42.2% had a family history of HTN, 47.9% had comorbidities, among which diabetes was the common (52.6%). Majority of respondents (85.5%) took one medicine per day, and amlodipine was the frequently used (70.9%) anti-hypertensive medication. Mean duration of diagnosis and medication were 7.34±6.54 and 6.37±5.92 years, respectively. Also mean systolic and diastolic blood pressure of respondents were 126.76±13.66 mm of Hg and 82.16±8.33 mm of Hg, respectively (Table 2).
 |
Table 2 Health-Related Characteristics of Respondents (n =282) |
Participants’ Response to the HBCTS
In the adherence assessment (n=282), the mean score of overall adherence was 17.85±3.87 (14–56) points. Mean scores of medicine taking adherence, reduced salt intake, and appointment keeping were 10.63±2.55, 4.16±1.12 and 3.06±1.07, respectively. The question “How often do you take someone else’s HBP pills?” had the majority of respondents (96%) who answered never (See Appendix 2). Only 10.6% respondents were perfectly adherent to all subscales of HBCTS scale, while 62.1% were perfectly adherent to appointment keeping only and 45% perfectly adherent to medication taking only (Table 3).
 |
Table 3 Summary of Participants’ Response to HBTCS (n =282) |
Sampling Adequacy and Sphericity
Since the KMO statistic was 0.877 (ie, >0.6), it indicated that the sample size was adequate for factor analysis. The p-value of the Bartlett test of homogeneity of variances (sphericity) was 0.000 (< 0.001), which reflected that the variance was different for various components from 1 to 14 items of questionnaires. Also, the significant Bartlett test result indicated that correlations between items were sufficiently large for PCA (Table 4).
 |
Table 4 KMO and Bartlett’s Test |
Construct Validity of the Tool
The correlation matrices determinant was 0.007, greater than 0.00001, so none of the variables created any problem. Therefore, all questions or items were understood as correlated, and no questions were removed at this stage (see Appendix 3). Principal component analysis showed a total of three factors having eigen value (sums of squared loadings) more than one (see Appendix 4). Similarly, the scree plot test also showed three components with more than 1 eigen value (Figure 1). Therefore, three factors were extracted as per the Kaiser’s criterion. These three factors, in combination, explained 55% of the variance. Hence, PCA was conducted on three factors with orthogonal rotation (varimax) (see Appendix 4). All items retaining in each factor have loading more than 0.4 (Table 5).
 |
Table 5 Exploratory Factor Analysis by Varimax Rotation with Kaiser’s Normalizationa |
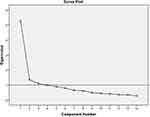 |
Figure 1 Scree test. |
Hill-Bone questionnaire originally contains three subscales. The distributions of questionnaires among three factors are presented in Table 5. Among nine items of medicine taking domain of the HBCTS tool, eight items were retained in factor 1. Similarly, factor 2 retains two items of reducing sodium or salt intake and two items of appointment keeping, and factor 3 retains one item of reducing sodium intake and one item of the medicine-taking domain of the original tool (Table 6).
 |
Table 6 Chi-Square Test of Adherence Level with Duration of Medication and Medication Number |
Known Group Validity
The overall perfect adherence and medicine taking adherence subscale were significantly associated with the duration of medication administration (more than 10 years). However, a significant association was not reported with the number of medication taking variable (more than one pill per day) (Table 6).
Reliability and Internal Consistency
The composite alpha value was 0.846 (ie, 84.6%). Only one item showed a slightly higher alpha value ie 0.855 than the composite value (0.846). That means that items could be deleted to enhance reliability. However, a coefficient value greater than 0.70 indicated a high level of internal consistency. Alpha values ≥0.7 were considered satisfactory. Item-to-total correlation ranged from 0.397 to 0.713 (Table 7).
 |
Table 7 Reliability Analysis of Nepali Version of Hill Bone Questionnaires (n =282) |
Discussion
Since control of HTN depends on patient’s adherence to therapy, assessing adherence to the same is a major step in controlling high BP and preventing complications among hypertensive patients. In Nepal, the increasing prevalence of HTN urges the identification of determinants of poor adherence towards anti-hypertensive therapy.44 For that, initially there is a need of valid and reliable tool for the measurement of treatment adherence. Unfortunately, there is a lack of a standard, specific validated tool in the Nepalese version to assess adherence of Nepalese patients to anti-hypertensive therapy. Therefore, the most widely followed and utilized medication adherence tool for hypertensive patients ie, HBCTS was taken to translate into Nepalese language, culturally adapt and validate in Nepalese context to assess the medication adherence of Nepalese hypertensive patients.
Initially the tool was translated and pre-tested to check its cultural applicability and acceptability by Nepalese hypertensive patients. None of the participants objected the applicability and acceptability of the tool, however, gave minor comments and suggestions to enhance the comprehensibility of the questionnaire in Nepalese cultural context. Furthermore, to enhance acceptance of the questionnaires, along with patients’ comments, critical comments and suggestions from experts’ team comprising nursing and pharmaceutical academicians were sought to confirm the content validity and cultural acceptability; and the tool was revised based on their comments. Additionally, the discussion with expert team inferred the need for statistical analysis. For that, EFA was performed using principal component analysis (PCA), and the analysis reported and confirmed three constructs in the tool with the eigen value greater than one and this was also supported by the scree plot. It was similar to the original tool22 confirmed in many other validation studies, such as the Polish version of the Hill-Bone tool.26,39
However, the components in each factor retained were not identical to the original tool. Some components were not differentiated into three factors as of the original study. Appointment keeping and reduced salt intake components were mixed in the same factor, and item number 13, which initially belonged to the medicine taking domain, was also shown to retain with reducing salt intake component in factor 3. Similar to our results, many other translations and validation studies also showed variations in the component loading in each factor.26,39,45 Chinese version showed four factors with two components for medicine taking, one for salt intake and one for appointment keeping.45 Similarly, Polish, and Malay versions also showed improper loading of components in three factors.26,39 The difference in theoretical concept and practical elucidation of the components in each factor could be due to less relevance of those particular questionnaires to the Nepalese context. This study considered patients residing in the community and visiting primary healthcare centres, where the government provides basic health services including few antihypertensive medicines. They usually do not have a practice or culture of using or sharing others’ medication, eating fast food, and regular appointment taking for their treatment. In developing countries like Nepal, healthcare providers usually advise patients to come for regular hospital visits on a fixed date of follow ups. Therefore, further in-depth study is still essential to justify this finding. Additionally, the KMO and Bartlett’s test conducted before the EFA showed sufficiency of sample size (KMO = 0.877, p-value =0.000). Therefore, the inadequacy of sample size for the impaired distribution of components in each factor during EFA cannot be ruled out.
Similarly, in order to strengthen the validity of tool, we performed a correlation test between the known predicting factors of medication non-adherence among hypertensive patients in Nepal such as duration of treatment and number of medications as reported in previous studies with perfect non-adherence and perfect adherence determined by the use of translated Nepalese HBTCS;13,18 however, the duration of treatment only showed a significant relationship with medication adherence in chi-square test. This probably was due to 100% perfection criteria of the original tool for perfect adherence and non-adherence.22 HBCTS tool gives either perfect or non-perfect adherence behavior of patients but does not provide a cut-off point for optimal and poor adherence as in other adherence scales like the Morisky scale,24 thus, limiting the clinical outcome correlation with adherence.45 Therefore, the appropriate cut-off point is to be used to categorize the adherence score, which was also noted in a study by Pan et al.45 Similarly, the salt reduction and appointment taking-related items require further study whether to include or exclude while determining medication adherence level in the Nepalese context. Furthermore, as Pan et al suggested, along with salt reduction by food intake consideration, the physical activities, cigarette smoking and alcohol consumption-related factors can also be considered in further development of the tool in future.45 As the purpose of the study was only to translate, culturally adapt and statistically validate the translated tool among Nepalese hypertensive patients, no modification was made in the original tool, but some recommendations have been discussed for future study.
All 14 items were retained, and no component was removed as the reliability assessment resulted in reliable internal consistency for Nepalese version of the HBCTS.42 The calculated Cronbach alpha for all 14 items of HBCTS was 0.846, and removal of any item did not show any significant increase in the alpha value. Previous validation studies of this tool in various languages also revealed reliable overall alpha values such as Turkish version 0.72,25 Polish 0.851,26 Chinese version 0.857,45 and did not remove any items. However, the components were not loaded appropriately into each factor as in the Turkish, Polish, and Chinese versions of the original tool.25,26,45 Similarly, Uchmanowicz et al had not reported the alpha value of the subscale because of the deficient number of items in the subscale.26 However, we calculated the alpha score of subscales in this study. Although the items for subscale was low, all three subscales extracted had not shown much low Cronbach alpha score [“medication taking” subscale (9 items) was 0.853, “reduce salt intake” subscale (3 items) 0.496 and “appointment keeping” subscale (2 items) was 0.645]. Krousel-wood et al argued that reduced salt intake subscale may not be acceptable because of the lower alpha value.36 However, it can be accepted and applied as the subscale retained only three items. Furthermore, national-level large-scale studies among a wide range of Nepalese hypertensive patients are recommended to explore an improved alpha value of reducing salt intake subscale.
Strengths and Limitations
This is the first study to translate, culturally adapt and validate English version of HBCTS into Nepalese language. It provides a validated tool to study the medication adherence of hypertensive patients in Nepalese language. In addition, it forms the preliminary foundation to carry out the further studies on developing appropriate Nepalese tool for measuring the medication adherence and factors associated with medication non-adherence among hypertensive patients of Nepal including Nepalese speaking community.
Similarly, the study retains some limitations. First of all this was a cross-sectional study conducted using a non-probability sampling and the tool used for assessing treatment adherence was a self-reporting tool. Thus, there is a risk of reporting and social desirability bias. Secondly, the study collected the response of hypertensive patients visiting PHCCs of certain region of Kathmandu, Province Bagmati only, but could not able to cover the wide range of hypertensive patients living in different administrative sectors, geography variation and diverse cultural background of hypertensive people living in the country, and those visiting various levels of healthcare institutions. Thus, in future studies, inclusion of a larger sample size with diverse cultural community of Nepal offers better opportunities to test the instrument.
Conclusion
The Hill-Bone compliance to high blood pressure therapy scale was successfully translated, culturally adapted, and checked for the reliability and validity of translated tool. The reliability and validity studies confirmed that the tool can measure treatment adherence amongst patients with hypertension in Nepal as well as Nepalese speaking community outside Nepal. However, further validation studies are recommended to carry out among large population representing wide range of diverse Nepalese community to strengthen its validity and relevance among Nepalese patients with hypertension.
Data Sharing Statement
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
Ethical Approval and Consent to Participate
The study was conducted in accordance with the guidelines of declaration of Helsinki. The ethical approval was obtained from the Institutional Review Committee of Nobel College, Kathmandu, Nepal. Written and verbal informed consents of the participants were taken before collecting their responses.
Acknowledgments
The authors are thankful to all the participants and primary healthcare centres who helped to collect responses during the study period.
Author Contributions
All authors contributed to data analysis, drafting, or revising the article, have agreed on the journal to which the article was submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
Authors received no financial support for conducting this research work. The authors want to acknowledge the support from the University of Birmingham to cover the open access fees for the article.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. World Health Organization. Noncommunicable diseases; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases.
2. Centers for Disease Control and Prevention. Facts about hypertension; 2021. Available from: https://www.cdc.gov/bloodpressure/facts.htm.
3. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–2260. doi:10.1016/S0140-6736(12)61766-8
4. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi:10.1371/journal.pmed.0030442
5. Ibrahim MM, Damasceno A. Hypertension in developing countries. Lancet. 2012;380(9841):611–619. doi:10.1016/S0140-6736(12)60861-7
6. Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020;75(2):285–292. doi:10.1161/HYPERTENSIONAHA.119.14240
7. Ramli A, Ahmad NS, Paraidathathu T. Medication adherence among hypertensive patients of primary health clinics in Malaysia. Patient Prefer Adherence. 2012;6:613–622. doi:10.2147/PPA.S34704
8. World Health Organization. Adherence to long-term therapies. Evidence for action; 2003. Available from: http://apps.who.int/iris/bitstream/handle/10665/42682/9241545992.pdf?sequence=1.
9. Chopra HK, Ram CVS. Recent guidelines for hypertension. Circ Res. 2019;124(7):984–986. doi:10.1161/CIRCRESAHA.119.314789
10. Unger T, Borghi C, Charchar F, et al. 2020 International society of hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334–1357. doi:10.1161/HYPERTENSIONAHA.120.15026
11. Tilea I, Petra D, Voidazan S, Ardeleanu E, Varga A. Treatment adherence among adult hypertensive patients: a cross-sectional retrospective study in primary care in Romania. Patient Prefer Adherence. 2018;12:625–635. doi:10.2147/PPA.S162965
12. Alsolami F, Hou X-Y, Correa-Velez I. [PS 03-23] Factors affecting antihypertensive medications adherence among hypertensive patients in Saudi Arabia. J Hypertens. 2016;34(Supplement 1):e132. doi:10.1097/01.hjh.0000500233.12767.52
13. Bhandari B, Bhattarai M, Bhandari M, Ghimire A, Pokharel PK, Morisky DE. Adherence to antihypertensive medications: population based follow up in Eastern Nepal. J Nepal Health Res Counc. 2015;13(29):38–42.
14. Abbas H, Kurdi M, Watfa M, Karam R. Adherence to treatment and evaluation of disease and therapy knowledge in Lebanese hypertensive patients. Patient Prefer Adherence. 2017;11:1949. doi:10.2147/PPA.S142453
15. Lee GK, Wang HH, Liu KQ, Cheung Y, Morisky DE, Wong MC. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale. PLoS One. 2013;8(4):e62775. doi:10.1371/journal.pone.0062775
16. Sheilini M, Hande HM, Prabhu M, et al. Antihypertensive prescription pattern, self-reported reasons for non adherence to antihypertensives and adherence to lifestyle practices among the elderly. J Clin Diagn Res. 2018;12(1):OC01–OC04.
17. Teshome DF, Bekele KB, Habitu YA, Gelagay AA. Medication adherence and its associated factors among hypertensive patients attending the Debre Tabor General Hospital, northwest Ethiopia. Integr Blood Press Control. 2017;10:1. doi:10.2147/IBPC.S128914
18. Roka T, Ghimire M. Medication adherence among hypertensive patients attending a Tertiary Care Hospital in Nepal. J Nepal Health Res Counc. 2019;17(4):521–527. doi:10.33314/jnhrc.v17i4.2337
19. Kim J, Bushnell CD, Lee HS, Han SW. Effect of adherence to antihypertensive medication on the long-term outcome after hemorrhagic stroke in Korea. Hypertension. 2018;72(2):391–398. doi:10.1161/HYPERTENSIONAHA.118.11139
20. Lavsa SM, Holzworth A, Ansani NT. Selection of a validated scale for measuring medication adherence. J Am Pharm Assoc. 2011;51(1):90–94. doi:10.1331/JAPhA.2011.09154
21. Koschack J, Marx G, Schnakenberg J, Kochen MM, Himmel W. Comparison of two self-rating instruments for medication adherence assessment in hypertension revealed insufficient psychometric properties. J Clin Epidemiol. 2010;63(3):299–306. doi:10.1016/j.jclinepi.2009.06.011
22. Kim MT, Hill MN, Bone LR, Levine DM. Development and testing of the Hill-bone compliance to high blood pressure therapy scale. Prog Cardiovasc Nurs. 2000;15(3):90–96. doi:10.1111/j.1751-7117.2000.tb00211.x
23. Garfield S, Clifford S, Eliasson L, Barber N, Willson A. Suitability of measures of self-reported medication adherence for routine clinical use: a systematic review. BMC Med Res. Methodol. 2011;11(1):149. doi:10.1186/1471-2288-11-149
24. Ben AJ, Neumann CR, Mengue SS. The brief medication questionnaire and Morisky-Green test to evaluate medication adherence. Rev Saude Publica. 2012;46(2):279–289. doi:10.1590/S0034-89102012005000013
25. Karademir M, Koseoglu IH, Vatansever K, Van Den Akker M. Validity and reliability of the Turkish version of the Hill–bone compliance to high blood pressure therapy scale for use in primary health care settings. Eur J Gen Pract. 2009;15(4):207–211. doi:10.3109/13814780903452150
26. Uchmanowicz I, Jankowska-Polańska B, Chudiak A, Szymańska-Chabowska A, Mazur G. Psychometric evaluation of the Polish adaptation of the Hill-bone compliance to high blood pressure therapy scale. BMC Cardiovasc Disord. 2016;16(1):87. doi:10.1186/s12872-016-0270-y
27. Nashilongo M, Singu B, Kalemeera F, et al. Assessing adherence to antihypertensive therapy in primary health care in Namibia: findings and implications. Cardiovasc Drugs Ther. 2017;31(5):565–578. doi:10.1007/s10557-017-6756-8
28. Song Y, Han HR, Song HJ, Nam S, Nguyen T, Kim MT. Psychometric evaluation of hill-bone medication adherence subscale. Asian Nurs Res. 2011;5(3):183–188. doi:10.1016/j.anr.2011.09.007
29. Nogueira-Silva L, Sá-Sousa A, Lima MJ, Monteiro A, Dennison-Himmelfarb C, Fonseca JA. Translation and cultural adaptation of the hill-bone compliance to high blood pressure therapy scale to Portuguese. Rev Port Cardiol. 2016;35(2):93–97. doi:10.1016/j.repc.2015.07.013
30. Dehghan M, Dehghan-Nayeri N, Iranmanesh S. Translation and validation of the Persian version of the treatment adherence questionnaire for patients with hypertension. ARYA Atheroscler. 2016;12(2):76–86.
31. Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19(4):357–362. doi:10.1097/01.hco.0000126978.03828.9e
32. Lambert EV, Steyn K, Stender S, Everage N, Fourie JM. Cross-cultural validation of the hill-bone compliance to high blood pressure therapy scale in a South African, primary healthcare setting. Ethn Dis. 2006;16(1):286.
33. Bhattarai H, McLachlan CS, Khanal P, et al. May measurement month 2019: an analysis of blood pressure screening results from Nepal. Eur Heart J Suppl. 2021;23(Supplement_B):B110–B113. doi:10.1093/eurheartj/suab042
34. Aryal KK, Mehata S, Neupane S, et al. The burden and determinants of non communicable diseases risk factors in Nepal: findings from a nationwide STEPS survey. PLoS One. 2015;10(8):e0134834. doi:10.1371/journal.pone.0134834
35. Shakya R, Shrestha S, Gautam R, et al. Perceived illness and treatment adherence to hypertension among patients attending a tertiary hospital in Kathmandu, Nepal. Patient Prefer Adherence. 2020;14:2287–2300. doi:10.2147/PPA.S270786
36. Shrestha R, Sapkota B, Khatiwada AP, et al. Translation, cultural adaptation and validation of General Medication Adherence Scale (GMAS) into the Nepalese Language. Patient Prefer Adherence. 2021;15:1873. doi:10.2147/PPA.S320866
37. World Population Review. Kathmandu Population 2021; 2021. Available from: https://worldpopulationreview.com/world-cities/kathmandu-population.
38. Number of health facilities in Province 3, Department of Health Services (2074/75), Nepal; 2020. Available from: https://publichealthupdate.com/number-of-health-facilities-in-province-3-nepal/.
39. Cheong AT, Tong SF, Sazlina SG. Validity and reliability of the Malay version of the Hill-bone compliance to high blood pressure therapy scale for use in primary healthcare settings in Malaysia: a cross-sectional study. Malays Fam Physician. 2015;10(2):36–44.
40. Costello AB, Osborne J. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval. 2005;10(1):7.
41. World Health Organization. Process of translation and adaptation of instruments. Geneva: World Health Organization; 2016: 2018.
42. Taber KS. The use of Cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Educ. 2018;48(6):1273–1296. doi:10.1007/s11165-016-9602-2
43. Kaiser-Meyer-Olkin (KMO) test for sampling adequacy. Available from: https://www.statisticshowto.com/kaiser-meyer-olkin/.
44. Dhungana RR, Pandey AR, Shrestha N. Trends in the prevalence, awareness, treatment, and control of hypertension in Nepal between 2000 and 2025: a systematic review and meta-analysis. Int J Hypertens. 2021;2021:6610649. doi:10.1155/2021/6610649
45. Pan J, Hu B, Wu L, Wang H, Lei T, Liu Z. The translation, reliability and validity of the Chinese version of the Hill–bone compliance to high blood pressure therapy scale in adults with hypertension. Patient Prefer Adherence. 2020;14:1853. doi:10.2147/PPA.S268031
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
