Back to Journals » OncoTargets and Therapy » Volume 11
Transcatheter hepatic arterial infusion chemotherapy vs sorafenib in the treatment of patients with hepatocellular carcinoma of Barcelona Clinic Liver Cancer stage C: a meta-analysis of Asian population
Authors Ni JY, Liu SS, Sun HL, Wang WD, Zhong ZL, Hou SN, Chen YT, Xu LF
Received 12 November 2017
Accepted for publication 6 July 2018
Published 6 November 2018 Volume 2018:11 Pages 7883—7894
DOI https://doi.org/10.2147/OTT.S156844
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Samir Farghaly
Jia-Yan Ni,1,* Shan-Shan Liu,2,* Hong-Liang Sun,1 Wei-Dong Wang,1 Ze-Long Zhong,1 Si-Nan Hou,1 Yao-Ting Chen,1 Lin-Feng Xu1
1Guangdong Provincial Key Laboratory of Malignant Tumor Epigenetics and Gene Regulation, Department of Interventional Radiology, Sun Yat-Sen Memorial Hospital, Sun Yat-Sen University, Guangzhou 510120, Guangdong Province, People’s Republic of China; 2Department of Public Health, Sushe Community Health Service Center, Guangzhou 510220, Guangdong Province, People’s Republic of China
*These authors contributed equally to this work
Objective: To compare the clinical efficacy and safety of transcatheter hepatic arterial infusion chemotherapy (HAIC) with those of sorafenib in the treatment of patients with hepatocellular carcinoma (HCC) of Barcelona Clinic Liver Cancer (BCLC) stage C.
Methods: Potentially relevant studies comparing the clinical efficacy and safety of HAIC with those of sorafenib were searched using Medline, PubMed, Embase, Cochrane Library, and Chinese databases (Wanfang Data and China National Knowledge Infrastructure). Overall survival rate (OSR), tumor response rate, disease control rate (DCR), and serious adverse events (SAEs) were compared and analyzed. Pooled ORs with 95% CIs were calculated using either the fixed-effects model or the random-effects model. All statistical analyses were conducted using Review Manager (version 5.3) from the Cochrane Collaboration.
Results: A total of 1,264 patients were included in this meta-analysis. The results of this study showed that HAIC was associated with significantly higher 1-, 2-, and 3-year OSRs than sorafenib (OR 1.88, 95% CI1-year: [1.27–2.78], P1-year=0.002; OR 2.15, 95% CI2-year: [1.06–4.37], P2-year=0.03; OR 7.90, 95% CI3-year: [2.12–29.42], P3-year=0.002). Compared to sorafenib, HAIC was associated with superior complete response (CR), partial response (PR), and objective response rate (ORR) (OR 3.90, 95% CICR: [1.89–8.03], PCR =0.0002; OR 3.47, 95% CIPR: [2.31–5.24], PPR <0.00001; OR 3.02, 95% CIOR: [2.05–4.45], POR <0.0001). There was no statistically significant difference between HAIC and sorafenib in stable disease (SD), progressive disease (PD), DCR, and SAEs (OR 0.86, 95% CISD: [0.51–1.45], PSD =0.56; OR 0.62, 95% CIPD: [0.35–1.11], PPD =0.11; OR 0.53, 95% CISAE: [0.14–1.92], PSAE =0.33).
Conclusion: This study showed that HAIC was associated with better efficacy than sorafenib in terms of OSR and tumor response. Therefore, HAIC can be considered as an alternative treatment option for patients with HCCs of BCLC stage C.
Keywords: HCC, HAIC, targeted therapy, BCLC, prognosis, meta-analysis
Introduction
Hepatocellular carcinoma (HCC) is a serious health problem, which accounts for more than 700,000 new cases worldwide annually.1,2 HCC is the second leading cause of cancer-related death in many countries and regions.3 The Barcelona Clinic Liver Cancer (BCLC) staging system has been widely accepted as a treatment guideline that comprehensively considers tumor burden, hepatic function, and performance status of patients with HCC.4,5 Sorafenib is a multikinase inhibitor that targets raf kinase, which participates in the proliferation of tumor cells, and vascular endothelial growth factor (VEGF) receptor-2, VEGF receptor-3, and platelet-derived growth factor receptor, which contribute to angiogenesis of tumor cells. In clinical practice, according to the current guidelines, including the BCLC staging classification, sorafenib is the standard treatment modality for patients with advanced HCC in many countries. In previous studies, sorafenib was proved to prolong overall survival by 2.3–2.8 months and improve the response rate by 2.0%–3.3%, compared to placebo.6,7 However, because of the comprehensive consideration of limited efficacy, adverse events, and high cost, the clinical benefits of sorafenib were still unsatisfying.
In the last decade, epirubicin-, cisplatin-, interferon-, or 5-fluorouracil-based transcatheter hepatic arterial infusion chemotherapy (HAIC) was widely used for patients with BCLC stage C HCCs in Asian countries. HAIC was suggested as a promising treatment as it can inhibit tumor growth through antiangiogenic mechanisms with less toxicity and fewer systemic side effects than the maximum tolerated dose therapy. Several studies have reported the clinical effectiveness of HAIC for BCLC stage C HCCs, with response rates ranging from 20.8% to 52%, and the median survival time in complete and partial responders is approximately 40 and 17 months, respectively.8–10 Some previous studies comparing the clinical efficacy of HAIC with that of sorafenib suggested that HAIC was superior to sorafenib for patients with BCLC stage C HCCs.8,12–14 However, some other studies reported conflicting results.10,11,15
To the best of our knowledge, no meta-analysis studies have been performed to compare the clinical benefits and safety of HAIC with those of sorafenib in the treatment of patients with BCLC stage C HCCs. In this study, we designed a meta-analysis to compare comprehensively the efficacy and safety of HAIC with those of sorafenib for BCLC stage C HCCs. We hope that the comparison of these treatments could help stratify the benefits of treatment choices for patients with HCC.
Methods
Search strategy
In this meta-analysis, Medline, PubMed, Embase, Cochrane Library, and Chinese databases (Wanfang Data and China National Knowledge Infrastructure) were searched for studies comparing the clinical efficacy and safety of HAIC with those of sorafenib in the treatment of patients with BCLC stage C HCCs from January 2007 to June 2017. The study search used the following MeSH search headings: “hepatocellular carcinoma” or “primary liver cancer”, “BCLC stage C”, “transcatheter”, “hepatic arterial infusion chemotherapy”, and “sorafenib”. A limit was set on clinical studies that were designed to compare the clinical effectiveness and adverse events of HAIC with those of sorafenib in BCLC stage C HCCs. There was no language restriction in this search.
Inclusion criteria of published trials
To be considered as eligible in this meta-analysis, the enrolled studies were required to have comparative data on clinical efficacy (overall survival rate [OSR], tumor response rate, disease control rate [DCR]) and adverse events of HAIC and sorafenib in patients with BCLC stage C HCCs. The inclusion criteria were as follows: 1) trial design: the trials must be designed as clinical studies with comparative data on clinical effectiveness and adverse events of HAIC and sorafenib for BCLC stage C HCCs; 2) clear document indications for use of HAIC and sorafenib; 3) treatment design: HAIC vs sorafenib; 4) characteristics of patients: the studies were required to have relatively integrated basic characteristics of enrolled patients, such as average age, percentage of male, Child–Pugh class, tumor size, portal vein tumor thrombosis (PVTT), and virus infection; 5) time of publication: from January 2007 to June 2017; and 6) study results: at least one item of results on OSR, tumor response rate, DCR, or adverse event was applicable.
Reviews without abstracts, original data, editorials, expert opinions, letters, case reports, and studies lacking control groups were excluded from the analysis.
Evaluation strategy
Data extraction was independently conducted by two reviewers using the standardized methods, with any disagreements being settled by discussion of the respective study data and adjudicated by an experienced reviewer. From each study, the following data were abstracted: data for publication details (name of the first author and year of publication) and study characteristics (study design, age, gender of patients, study design, tumor size, tumor number, Child–Pugh class, OSR, tumor response rate, incidence of adverse events, etc.).
Statistical analysis
Statistical analyses were performed on dichotomous outcomes, and standard meta-analytical techniques were used in this study. Pooled ORs with 95% CIs were calculated using either the fixed-effects model or the random-effects model. For each meta-analysis, the χ2 and I2 statistics were first calculated to assess the heterogeneity of the included studies. P<0.1 and I2>50% were considered significant. For P<0.1 and I2>50%, the random-effects model was used; otherwise, data were assessed using the fixed-effects model. The risk of publication bias in this study was assessed by visual inspection of the symmetry of the funnel plot. All statistical analyses were performed using Review Manager (version 5.3) from the Cochrane Collaboration. The significance of the pooled ORs was assessed by the Z-test. P<0.05 was considered significant.
Results
Search results
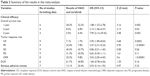
This study found a total of 86 potentially relevant studies. On the basis of the inclusion and exclusion criteria of this study, 10 retrospective cohort studies comparing the clinical efficacy and adverse events of HAIC with those of sorafenib for the treatment of BCLC stage C HCCs were finally included.8–17 The flowchart of the search strategy for included studies is shown in Figure 1. A total of 1,264 patients were included in the study, of whom 505 patients underwent sorafenib treatment and 759 patients underwent HAIC treatment. The basic characteristics, OSR, tumor response rate, and DCR of patients in enrolled trials are summarized in Tables 1 and 2. The quality of the included studies was assessed using the Cochrane Collaboration’s tool.
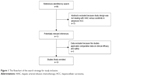  | Figure 1 The flowchart of the search strategy for study inclusion. |
Meta-analysis results
OSR
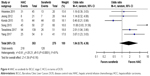
Six, four, and four studies reported the comparative data for OSR at 1, 2, and 3 years, respectively. From the results of tests for heterogeneity between trials (χ21-year =7.16, P1-year =0.21, I21-year =30%; χ22-year =1.15, P2-year =0.77, I22-year =0%; χ23-year =1.70, P3-year =0.64, I23-year =0%), the fixed-effects model was used to pool the results in the analysis of the effects of OSR. Compared to sorafenib, the data and forest plots of our study showed that HAIC was associated with significantly higher 1-, 2-, and 3-year OSR in the treatment of patients with BCLC stage C HCC (OR 1.88, 95% CI1-year: [1.27–2.78], P1-year=0.002; OR 2.15, 95% CI2-year: [1.06–4.37], P2-year=0.03; OR 7.90, 95% CI3-year: [2.12–29.42], P3-year=0.002) (Figure 2 and Table 3).
Tumor response to therapy
Nine, nine, nine, nine, and ten studies reported the comparative data for tumor response rate in terms of complete response (CR), partial response (PR), stable disease (SD), progressive disease (PD), and objective response rate (ORR), respectively. From the results of tests for heterogeneity between trials (χ2CR =7.76, PCR =0.26, I2CR =23%; χ2PR =14.95, PPR =0.06, I2PR =46%; χ2SD =29.72, PSD =0.0002, I2SD =73%; χ2PD =34.62, PPD ≤0.0001, I2PD =38%; χ2OR =12.73, POR =0.08, I2OR =45%), either the random-effects model or the fixed-effects model was used to pool the results in the analysis of the effects of CR, PR, SD, PD, and OR. The data and forest plots of our study revealed that HAIC was associated with obviously better CR, PR, and OR than sorafenib (OR 3.90, 95% CICR: [1.89–8.03], PCR =0.0002; OR 3.47, 95% CIPR: [2.31–5.24], PPR <0.00001; OR 3.02, 95% CIOR: [2.05–4.45], POR <0.0001). There was no statistically significant difference between HAIC and sorafenib in stable SD and PD (OR 0.86, 95% CISD: [0.51–1.45], PSD =0.56; OR 0.62, 95% CIPD: [0.35–1.11], PPD =0.11) (Figure 3 and Table 3).
DCR
Six studies reported the comparative data on DCR of HAIC and sorafenib for patients with BCLC stage C HCC. From the results of tests for heterogeneity between trials (χ2DCR =26.21, PDCR ≤0.0001, I2DCR =83%), the random-effects model was used to pool the results in the analysis of the effects of DCR. The data and forest plot of our study showed no statistically significant difference in DCR between HAIC and sorafenib (OR 1.84, 95% CIDCR: [0.78–4.36], PDCR =0.16) (Figure 4 and Table 3).
Serious adverse events
In this meta-analysis, the incidence of serious adverse events (SAEs) of HAIC and sorafenib in the treatment of patients with BCLC stage C HCC was analyzed and compared. Here, the SAEs were defined as Common Terminology Criteria for Adverse Events grade 3/4 adverse events or adverse events that lead to discontinuation of treatment with HAIC or sorafenib. Seven studies reported the comparative data on SAEs of HAIC and sorafenib for patients with BCLC stage C HCC. From the results of tests for heterogeneity between trials (χ2SAE =30.89, PSAE ≤0.0001, I2SAE =81%), the random-effects model was used to pool the results in the analysis of the effects of SAEs. The data and forest plot of our study showed no statistically significant difference in SAEs between HAIC and sorafenib (OR 0.53, 95% CISAE: [0.14–1.92], PSAE =0.33) (Figure 5 and Table 3).
Assessment of publication bias
In this study, the risk of publication bias was assessed by visual inspection of the symmetry level of funnel plot. The fixed-effects model was used to pool the results in the analysis of the effects of CR, PR, OR, and 1-, 2-, and 3-year OSRs. The results of our meta-analysis revealed that the symmetry level of the funnel plots was high. This suggested that there was no serious publication bias in the trials included in this study (Figure 6).
Discussion
The BCLC staging classification is one of the most widely used guidelines for the clinical treatment of HCC in many countries. According to the BCLC staging classification, BCLC stage C HCC is suggested as the advanced-stage HCC, and sorafenib is considered as the primary treatment option for HCCs of that stage. However, because of the adverse effects, moderate efficacy, and high cost of sorafenib, its application is limited. Thus, the clinical benefits of sorafenib are still not satisfactory. To improve the prognosis of patients with advanced HCC, alternative treatment strategies are being investigated. In the recent years, HAIC was proved as an effective and safe therapy for advanced HCC. Previous studies had reported that HAIC was associated with better efficacy than sorafenib for patients with advanced HCCs.8,12–14 However, some other studies had reported conflicting results.10,11,15 Meta-analysis is a method that combines data from all eligible studies, and has the advantages of reducing random error, obtaining more precise estimates, and defining the effect of clinical interventions more precisely.18,19 Hence, meta-analysis is an eligible method to resolve such conflicts. In this study, the OSR, tumor response rate, and the incidence of SAEs were analyzed and compared. The results of this study showed that HAIC was associated with significantly better OSR and tumor response rate in comparison with sorafenib. This indicated that HAIC was superior to sorafenib in the treatment of patients with advanced HCCs.
In this meta-analysis, epirubicin-, cisplatin-, or 5-fluorouracil-based HAIC was performed by the transcatheter method, and the chemotherapeutic agent was delivered through the hepatic arterial infusion chemoport. From previous studies and our clinical practice, we found that the mechanisms by which HAIC affects HCCs might include the inhibition of angiogenesis, stimulation of immunity, and direct inhibition of tumor cell proliferation.8,14,20–22 Inhibition of angiogenesis is the most important mechanism. During HAIC treatment, the angiogenesis of tumor cells can be inhibited by direct destruction and inhibition of proliferation of endothelial cells. Further, the expression levels of endogenous antiangiogenic factors and endogenous angiogenic factors were reported to be upregulated and downregulated, respectively.23,24 Recently, the reduction in endothelial progenitor cell mobilization and stimulation of immunity were also investigated as mechanisms of HAIC for HCC.23,24
PVTT is an important cause of tumor spread, portal hypertension, and deterioration of liver function, leading to variceal rupture, intractable ascites, and hepatic encephalopathy. Patients with advanced HCC and PVTT were associated with poor prognosis, with a median survival time ranging from 2.7 to 4 months. As the first-line treatment option suggested by the BCLC staging system, sorafenib can prolong the survival of patients with PVTT from 6.5 to 8 months.25,26 However, the survival benefits and treatment responses of sorafenib in patients with advanced HCCs with PVTT were modest. Thus, the availability of sorafenib is limited. In recent years, surgical resection or transarterial chemoembolization in selected patients, HAIC, external radiation, I125 seed implantation, radioembolization, and combination therapies have been performed as alternative treatment options for patients with advanced HCCs with PVTT.25–27 Compared to sorafenib, HAIC was proved to be associated with more favorable clinical efficacy in terms of overall survival and tumor response in the treatment of patients with PVTT. In previous studies in which HAIC was performed for HCC with PVTT, the ORR and DCR ranged from 33% to 52.6% and 47.1% to 77%, respectively.27–30 Two randomized controlled trials (RCTs) showed that ORR was 2%–3%, and the DCR was 57.3%–73%.6,7 Hence, from the data of previous studies and our study, we found that the ORR of HAIC was significantly higher than that of sorafenib, whereas the DCR of the two treatments appeared to be identical. In this study, the meta-analysis data showed that HAIC was associated with significantly better 1-, 2-, and 3-year OS rates and CR, PR, and ORR in comparison with sorafenib. This indicated that the results of our meta-analysis study were reliable.
This study is the first meta-analysis designed to comprehensively compare the clinical efficacy and safety of HAIC with those of sorafenib in the treatment of patients with HCCs of BCLC stage C. In this study, the OSR, tumor response rate, DCR, and the incidence of SAEs were compared and analyzed. The risk of publication bias in the included studies was assessed by the visual inspection of the symmetry level of the funnel plot.31,32 The results of our study showed that the level of symmetry of the funnel plot was high. This suggested that there was no serious publication bias in the trials included in this meta-analysis. Thus, we can see that the studies included in the meta-analysis are strong evidence to support our results.
Finally, the potential limitations of this study must be mentioned. First, there were limited available and applicable RCTs comparing the effectiveness and adverse event of HAIC and sorafenib for the treatment of advanced HCCs in the last several years. However, although a meta-analysis has traditionally been applied and is best confined to RCTs, meta-analytical techniques using non-RCTs might be a valid method in clinical settings in which either the number or the sample size of the RCTs is insufficient.33 In the future, more RCTs should be conducted to provide further evidence. Second, because all included studies in this meta-analysis were from Asian countries, data bias caused by the source of patients might be present. More high-quality RCTs from other continents and countries are needed to provide more data for future research.
Conclusion
Our meta-analysis showed that HAIC was associated with better clinical efficacy and reliable safety in comparison with sorafenib for patients with BCLC stage C HCCs. Therefore, HAIC can be considered as an alternative treatment option for advanced HCCs.
Acknowledgments
This work was supported by grant [2013]163 from the Key Laboratory of Malignant Tumor Molecular Mechanism and Translational Medicine of Guangzhou Bureau of Science and Information Technology and grant KLB09001 from the Key Laboratory of Malignant Tumor Gene Regulation and Target Therapy of Guangdong Higher Education Institutes.
Disclosure
The authors report no conflicts of interest in this work.
References
Ghouri YA, Mian I, Rowe JH. Review of hepatocellular carcinoma: Epidemiology, etiology, and carcinogenesis. J Carcinog. 2017;16(1):1. | ||
Allaire M, Nault JC. Advances in management of hepatocellular carcinoma. Curr Opin Oncol. 2017;29(4):288–295. | ||
Sia D, Villanueva A, Friedman SL, Llovet JM. Liver Cancer Cell of Origin, Molecular Class, and Effects on Patient Prognosis. Gastroenterology. 2017;152(4):745–761. | ||
Bruix J, Sherman M, American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020–1022. | ||
Kinoshita A, Onoda H, Fushiya N, et al. Staging systems for hepatocellular carcinoma: Current status and future perspectives. World J Hepatol. 2015;7(3):406–424. | ||
Cheng AL, Kang YK, Chen Z, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10(1):25–34. | ||
Llovet JM, Ricci S, Mazzaferro V, et al for the SHARP Investigators Study Group. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–390. | ||
Yang H, Woo HY, Lee SK, et al. A comparative study of sorafenib and metronomic chemotherapy for Barcelona Clinic Liver Cancer-stage C hepatocellular carcinoma with poor liver function. Clin Mol Hepatol. 2017;23(2):128–137. | ||
Terashima T, Yamashita T, Arai K, et al. Beneficial Effect of Maintaining Hepatic Reserve during Chemotherapy on the Outcomes of Patients with Hepatocellular Carcinoma. Liver Cancer. 2017;6(3):236–249. | ||
Hatooka M, Kawaoka T, Aikata H, et al. Comparison of Outcome of Hepatic Arterial Infusion Chemotherapy and Sorafenib in Patients with Hepatocellular Carcinoma Refractory to Transcatheter Arterial Chemoembolization. Anticancer Res. 2016;36(7):3523–3529. | ||
Fukubayashi K, Tanaka M, Izumi K, et al. Evaluation of sorafenib treatment and hepatic arterial infusion chemotherapy for advanced hepatocellular carcinoma: a comparative study using the propensity score matching method. Cancer Med. 2015;4(8):1214–1223. | ||
Kawaoka T, Aikata H, Hyogo H, et al. Comparison of hepatic arterial infusion chemotherapy versus sorafenib monotherapy in patients with advanced hepatocellular carcinoma. J Dig Dis. 2015;16(9):505–512. | ||
Kondo M, Morimoto M, Ishii T, et al. Hepatic arterial infusion chemotherapy with cisplatin and sorafenib in hepatocellular carcinoma patients unresponsive to transarterial chemoembolization: a propensity score-based weighting. J Dig Dis. 2015;16(3):143–151. | ||
Song DS, Song MJ, Bae SH, et al. A comparative study between sorafenib and hepatic arterial infusion chemotherapy for advanced hepatocellular carcinoma with portal vein tumor thrombosis. J Gastroenterol. 2015;50(4):445–454. | ||
Hiramine Y, Uto H, Imamura Y, et al. Sorafenib and hepatic arterial infusion chemotherapy for unresectable advanced hepatocellular carcinoma: A comparative study. Exp Ther Med. 2011;2(3):433–441. | ||
Jeong SW, Jang JY, Lee JE, et al. The efficacy of hepatic arterial infusion chemotherapy as an alternative to sorafenib in advanced hepatocellular carcinoma. Asia Pac J Clin Oncol. 2012;8(2):164–171. | ||
Shiozawa K, Watanabe M, Ikehara T, et al. Comparison of Sorafenib and Hepatic Arterial Infusion Chemotherapy for Advanced Hepatocellular Carcinoma: A Propensity Score Matching Study. Hepatogastroenterology. 2014;61(132):885–891. | ||
Kivimäki M, Kuosma E, Ferrie JE, et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health. 2017;2(6):e277–e285. | ||
Ulug P, Sweeting MJ, von Allmen RS, Thompson SG, Powell JT. SWAN collaborators. Morphological suitability for endovascular repair, non-intervention rates, and operative mortality in women and men assessed for intact abdominal aortic aneurysm repair: systematic reviews with meta-analysis. Lancet. 2017;389(10088):2482–2491. | ||
Ogawa K, Kamimura K, Watanabe Y, et al. Effect of double platinum agents, combination of miriplatin-transarterial oily chemoembolization and cisplatin-hepatic arterial infusion chemotherapy, in patients with hepatocellular carcinoma: Report of two cases. World J Clin Cases. 2017;5(6):238–246. | ||
Imamine R, Shibata T, Shinozuka K, Togashi K. Complications in hepatic arterial infusion chemotherapy: retrospective comparison of catheter tip placement in the right/left hepatic artery vs. the gastroduodenal artery. Surg Today. 2017;47(7):851–858. | ||
Ikeda M, Shimizu S, Sato T, et al. Sorafenib plus hepatic arterial infusion chemotherapy with cisplatin versus sorafenib for advanced hepatocellular carcinoma: randomized phase II trial. Ann Oncol. 2016;27(11):2090–2096. | ||
Tsunematsu S, Suda G, Yamasaki K, et al. Combination of neutrophil-to-lymphocyte ratio and early des-γ-carboxyprothrombin change ratio as a useful predictor of treatment response for hepatic arterial infusion chemotherapy against advanced hepatocellular carcinoma. Hepatol Res. 2017;47(6):533–541. | ||
Wen X, Reynolds L, Mulik RS, et al. Hepatic Arterial Infusion of Low-Density Lipoprotein Docosahexaenoic Acid Nanoparticles Selectively Disrupts Redox Balance in Hepatoma Cells and Reduces Growth of Orthotopic Liver Tumors in Rats. Gastroenterology. 2016;150(2):488–498. | ||
Moriguchi M, Furuta M, Itoh Y. A Review of Non-operative Treatments for Hepatocellular Carcinoma with Advanced Portal Vein Tumor Thrombus. J Clin Transl Hepatol. 2017;5(2):1–7. | ||
Han K, Kim JH, Ko GY, Gwon DI, Sung KB, Gy K. Treatment of hepatocellular carcinoma with portal venous tumor thrombosis: A comprehensive review. World J Gastroenterol. 2016;22(1):407–416. | ||
Lin CC, Hung CF, Chen WT, Lin SM. Hepatic Arterial Infusion Chemotherapy for Advanced Hepatocellular Carcinoma with Portal Vein Thrombosis: Impact of Early Response to 4 Weeks of Treatment. Liver Cancer. 2015;4(4):228–240. | ||
Nagai H, Mukozu T, Ogino YU, et al. Sorafenib and hepatic arterial infusion chemotherapy for advanced hepatocellular carcinoma with portal vein tumor thrombus. Anticancer Res. 2015;35(4):2269–2277. | ||
Wu J, Huang WJ, Wang HY, et al. Arterial infusion of 5-fluorouracil combined with subcutaneous injection of pegylated interferon alpha-2b in treating unresectable hepatocellular carcinoma with portal vein tumor thrombus. Med Oncol. 2015;32(3):65. | ||
Ikeda M, Okusaka T, Furuse J, et al. A multi-institutional phase II trial of hepatic arterial infusion chemotherapy with cisplatin for advanced hepatocellular carcinoma with portal vein tumor thrombosis. Cancer Chemother Pharmacol. 2013;72(2):463–470. | ||
Higgins JP, Altman DG, Gøtzsche PC, et al; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. | ||
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. | ||
Mathurin P, Raynard B, Dharancy S, et al. Meta-analysis: evaluation of adjuvant therapy after curative liver resection for hepatocellular carcinoma. Aliment Pharmacol Ther. 2003;17(10):1247–1261. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.