Back to Journals » Psychology Research and Behavior Management » Volume 16
Trajectories of Learned Helplessness in Maintenance Haemodialysis Patients and Their Predictive Effects on Self-Management: A Latent Growth Mixture Modeling Approach
Received 13 December 2022
Accepted for publication 3 February 2023
Published 10 February 2023 Volume 2023:16 Pages 351—361
DOI https://doi.org/10.2147/PRBM.S401380
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mei-Chun Cheung
Chunyan Xie,1,2 Li Li,2,3 Yamin Li1
1Clinical Nursing Teaching and Research Section, the Second Xiangya Hospital, Central South University, Changsha, People’s Republic of China; 2XiangYa Nursing School, Central South University, Changsha, People’s Republic of China; 3The First Affiliated Hospital of Xinjiang Medical University, Urumqi, People’s Republic of China
Correspondence: Yamin Li, The Second Xiangya Hospital, Central South University, Changsha, Hunan, 410011, People’s Republic of China, Email [email protected]
Background: Learned helplessness (LH) is an essential psychological factor influencing maintenance haemodialysis (MHD) patients’ health behaviour and is closely related to prognosis of the disease. This study aimed to identify potential trajectories of LH in MHD patients and assess their predictive role in self-management.
Methods: This study was conducted in strict compliance with national laws, the Declaration of Istanbul, and the Declaration of Helsinki. A total of 347 MHD patients at a blood purification centre in Hunan Province, China, were selected as the study population. Four longitudinal surveys (baseline and second/fourth/sixth month after baseline) were conducted using the General Information Questionnaire for MHD patients, the Chinese version of the Learned Helplessness Scale for MHD patients, and the Self-Management Scale for Haemodialysis. Latent growth mixture model (LGMM) analysis was used to identify LH trajectories, and their predictors were analysed using multinomial logistic regression. The predictive role of LH trajectory on self-management was analysed using linear regression.
Results: This study identified three LH trajectories in MHD patients, named the “high-decreasing group” (57.9%), “low-increasing group” (21.3%), and “low-stability group” (20.7%). The results of the univariate analysis showed that sex (χ2=33.777, P < 0.001), age (χ2=10.605, P< 0.05), and subjective social status (SSS) (χ2=12.43, P< 0.01) were associated with LH trajectory classes. Multinomial logistic regression further demonstrated that gender, age, and SSS were predictors of different LH trajectories. The intercept and slope of the overall LH trajectory were negatively correlated with self-management (β=− 0.273, P< 0.001; β=− 0.234, P< 0.01).
Conclusion: MHD patients show three different LH trajectories. The initial level and developmental rate of LH can negatively predict future self-management. It is necessary to screen MHD patients’ LH and develop targeted interventions for them with different LH trajectories at specific stages.
Keywords: learned helplessness, maintenance haemodialysis, self-management, trajectories, longitudinal research
Introduction
Haemodialysis (HD) is the primary renal replacement therapy for end-stage renal disease (ESRD) patients.1 HD removes metabolic wastes and maintains electrolyte and acid-base balance by diverting the blood into the extracorporeal circulation and exchanging substances with dialysis fluid.2 Patients receiving HD for over three months are defined as maintenance haemodialysis (MHD) patients.3 More than 90% of ESRD patients in China are treated with MHD, with an annual growth rate of 20%. By 2021, there will be approximately 750,000 MHD patients in China.
MHD significantly improves patient survival but cannot completely replace renal function. Patients’ HD effects, prognosis, and quality of life are largely related to their self-management behaviours.4 Psychological factors are the most common risk factors for MHD patients’ self-management behaviours.5 Due to the severity and irreversibility of ESRD, the high medical charges, complications, and dietary and fluid restrictions, many patients suffer from learned helplessness (LH), such as hopelessness, depression, abandonment, and even self-destruction. LH refers to the psychological state of powerlessness or loss of confidence that occurs when an individual experiences long-term or repeated uncontrollable outcomes.6 The essence of LH is a learned negative motivation.7 It has been demonstrated that LH significantly impacts self-management and adherence in MHD patients.8,9 Patients with high LH are not confident in their ability to control disease and manage their lives and are prone to negative expectations. Thus, they tend to give up efforts or persist for a shorter time. In addition, patients who fall into helplessness may experience various negative consequences, such as mental distress, depression, and suicide, placing a heavy burden on society.10–13
Seligman proposes that LH is not a direct result of a traumatic event but rather is learned by the individual in response to a traumatic event.14 LH interacts with various variables. When individuals experience a stressful event (eg, dialysis), LH can be dynamic, which increases the complexity of their self-management interventions.14 Therefore, a longitudinal study of LH in MHD patients can inform the allocation of mental health resources and health-related behavioural interventions. Given that the current studies have been conducted based on variable-centred analysis, they are not conducive to clarifying the characteristics of individual LH growth. Using a person-centred approach, this study aimed to identify heterogeneous trajectories and examine the relationship between MHD patients’ self-management and heterogeneous trajectories. Specifically, we hypothesized that (a) different trajectories of LH in MHD patients would be found, (b) demographic variables and subjective social status (SSS) of MHD patients related to LH trajectories, and (c) the initial level and developmental rate of LH can be used to predict future self-management.
Materials and Methods
Participants
The MHD patients were selected using a convenience sampling method in May 2022 at the blood purification centre of a comprehensive hospital in Hunan Province, China. The inclusion criteria were as follows: (i) received HD treatment for ≥ three months and (ii) provided informed consent. Patients who did not complete baseline measurements were excluded.
Procedures
We clarified the purpose and significance of this study at the beginning to obtain informed consent from the participants. For the illiterate group, we explained the items’ content and helped them fill out questionnaires based on their real desires. The researchers confirmed the accuracy of the content with the participants to ensure that no omissions or mistakes were made. The investigation occurred one hour after the start of dialysis or 1 hour before the end when the patient’s blood circulation was stable Each participant took approximately 10–15 minutes to complete the questionnaire. The first measurement’s time was considered the baseline (T1). The follow-up occurred in the second (T2), fourth (T3), and sixth (T4) months after baseline. In the T1 stage, 400 questionnaires were distributed, and 369 valid questionnaires were returned, with a valid return rate of 92.25%. During the follow-up, 17 samples were lost due to moving, transplantation, and death, and another five incomplete questionnaires were also excluded. A final sample of 347 with no missing values was obtained to enter the analysis. The independent samples t test indicated no significant difference between the attrited sample and the final sample regarding the mean value of LH at baseline, indicating that the sample attrition was random.
Measures
General Information Questionnaire for MHD Patients
The research team designed a General Information Questionnaire for collecting MHD patients’ demographic information: gender, age, education, working status, monthly income and duration of the MHD/kidney transplant.
The Chinese Version of the Subjective Socioeconomic Status Scale (CSSS)
Subjective social status (SSS), a crucial psychological concept in social class psychology research, reflects how individuals perceive their position in the socioeconomic structure.15 The relationship between SSS and mental health has attracted much attention.
In this study, the CSSS scale was selected to validate the predictive role of SSS on LH trajectories. The CSSS was adapted from the MacArthur Scale of Subjective Social Status (SSS) developed by Adler et al.16 The scale consists of two items. Item 1 (social status) is linked to socioeconomic status (SES) and is used to assess an individual’s position in the social environment. Item 2 (community status) is related to the individual’s living environment, and the individual assesses his or her position in the community.17 Each item is scored from 1 to 10. The lower the score is, the lower the SSS of the individual. The scale is widely used in China, with a Cronbach’s α value of 0.82.18
The Learned Helplessness Scale for Maintenance Haemodialysis Patients in China (LHS-MHD-C)
There is no specific scale for MHD patients’ LH. Considering this limitation, we adapted a Chinese version of the learned helplessness scale for maintenance haemodialysis patients (LHS-MHD-C) based on Nicassio’s AHI scale.19 With his authorization, we conducted cross-cultural adaptation, psychological measurement, and evaluation. The LHS-MHD-C has 11 items classified into two dimensions (helplessness and internality) based on the results of exploratory factor analysis and confirmatory factor analysis. Responses were measured on a five-point Likert scale with options ranging from 1=strongly disagree to 5=strongly agree. Six items in the dimension of internality are reverse scored. The higher the total score was, the more severe the LH.20 In our previous study, the scale showed good internal consistency (Cronbach’s α value of 0.759), retest reliability (n=30, intragroup correlation=0.772, P<0.01), and split-half reliability (0.774).
Self-Management Scale for Haemodialysis (SMSH)
SMSH, developed by Song in 2009,21 was used to measure MHD patients’ self-management in this study. It has 20 items and is divided into four dimensions: problem solving, performing self-care, partnership, and emotional processing. Responses were measured on a 4-point Likert scale, with scores 1–4 representing the frequency of the behaviour: never, occasionally, often, and always, respectively. Total scores were 20–80. The higher the score was, the better the patient’s self-management behaviour.22 SMSH was adapted by Li,23 and its Cronbach’s α value was 0.813.
Data Analysis
Descriptive statistical analysis, univariate analysis, and multinomial logistic regression were performed using SPSS 25.0 software. Latent growth mixture modeling (LGMM) was performed using Mplus 7.0 software, which assumes that a class has similar but not identical trajectories, ie, variance variation is allowed for individuals within the same class.24 Therefore, LGMM helps examine LH’s dynamic pattern. The indicators of model fitness are the log-likelihood test, Akaike information criterion (AIC), Bayesian information criterion (BIC), and adjusted BIC (aBIC), and their smaller values indicate better model fit.25 The entropy index was used to assess the classification accuracy. The value of entropy ranged from 0 to 1, and when it was 0.8, it indicated that the classification accuracy was more than 90%.26 Lo-Mendell-Rubin (LMR) and Bootstrapped Likelihood Ratio Test (BLRT) were used to compare the difference in fit between the models. If both P values reached a significant level, the model with k classes was significantly better than that with k-1 classes.27 Models containing less than 5% of the samples in any class could be excluded.28
Ethical Considerations
The Ethics Committee of Xiangya Nursing School of Central South University approved this study on April 20, 2022 (No. E202255). Informed consent was obtained from all participants. This study was conducted strictly with national laws and the Declaration of Helsinki. All kidneys were donated voluntarily with written informed consent, and this process was conducted in accordance with the Declaration of Istanbul.
Results
General Characteristics
Of the 347 samples, 60.2% of the participants were male, 32.3% were 18–44 years old, and 43.5% had secondary education. Other characteristics of the participants are shown in Table 1.
 |
Table 1 Participant Characteristics (n=347) |
Descriptive Statistics of Key Variables
Descriptive statistical analysis of LH and self-management scores of MHD patients revealed that patients had the highest LH and self-management scores at time point T4, 36.12 ± 10.69 and 60.47 ± 12.85, respectively. Table 2 shows the means and standard deviations of key variables.
 |
Table 2 Means and Standard Deviations for Main Variables (n=347) |
Identification Trajectory Classes
In the initial GMM model, there was significant variance in the intercept and slope (P < 0.001), indicating significant variability in both the mean LH and the linear growth trajectory over six months. Based on the initial model, the number of classes in the model gradually increases until the best model fits the data. The results showed that the AIC, BIC, and aBIC indicators were higher in the 5-classes model than in the other models. The entropy of the 5-classes model was less than 0.8, and the probability of one of its classes was less than 5%, so it was not considered. The BIC of the 4-classes model was higher than that of the 3-classes model. The entropy value of the 4-classes model was smaller than that of the 3-classes model. Moreover, the LMR and BLRT of the 4-classes model were insignificant, indicating no difference between the 4-classes model and 3-classes models. Therefore, the 4-classes model was not considered. The AIC, BIC, and aBIC values were smaller in the 3-classes model than in the 2-classes model. Moreover, when three classes were retained, LMR and BLRT reached significant levels (P < 0.001), entropy values were more desirable (> 0.8), and the class probability was reasonable (all > 5%). Combining the above information with LH theory, the three-classes model was finally identified as the optimal model. The fitting index results are shown in Table 3.
 |
Table 3 Fit Indices of the Grow Mixture Models for Different Numbers of Latent Classes |
The latent classes were named according to their characteristics. In Class 1, the intercept of the LH trajectory model was low, and the slope was not significant (P>0.05). Therefore, Class 1 was named the low-stability group, accounting for 20.7% of the overall model. Class 2 had a high initial level of LH with a negative slope (P<0.01) and was named the high-decreasing group, accounting for 57.9% of the model. Class 3 had a low intercept of LH with a positive slope (P<0.01), indicating that MHD patients started with low LH but deteriorated significantly over time. Therefore, Class 3 was named the low-increasing group, accounting for 21.3% of the model. Three trajectories are shown in Figure 1.
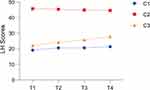 |
Figure 1 Three classes trajectory model for LH from baseline to six months (n=347). |
Predicting the Membership of Trajectory Classes
The univariate analysis explored the factors affecting LH trajectories. The results showed significant differences in the distribution of patients on gender, age, and SSS for the three trajectories (P<0.05). The results are detailed in Table 4.
 |
Table 4 Demographic, Disease, and SSS Characteristics by Trajectory Classes (n=347) |
Next, those variables were included in the multinomial logistic regression, with the three trajectories as dependent variables. The results showed that the predictors of MHD patients’ LH that were prone to develop into the high-decreasing group (Class 2) or low-increasing group (Class 3) compared to the low-stability group (Class 1) were male, 45–59 years old with low SSS. The results are detailed in Table 5.
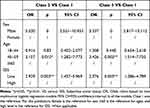 |
Table 5 Results of the Multinomial Logistic Regression (n=347) |
Predictive Effects of the Initial Level and Developmental Rate of LH on Self-Management
A linear regression model was constructed. The scores of self-management at the T4 stage were considered the dependent variable, and the intercept and slope of the LH trajectory were the independent variables. The results showed good model fit [χ2=26.54, degrees of freedom=7, P<0.001, χ2/df=3.79, comparative fit index (CFI)=0.992, Tucker‒Lewis index (TLI)=0.988, root mean square error of approximation (RMSEA) =0.09 (90% CI: 0.055 0.127), and standardized root mean square residual (SRMR)= 0.02]. The intercept and slope of LH were significant negative predictors of self-management scores (β=−0.273, P<0.001; β=−0.234, P<0.01). The prediction model is shown in Figure 2.
 |
Figure 2 Predictive effects of the initial level and slope of LH on self-management. Data in the figure are standardized path coefficients. The P values of all path coefficients were <0.05. |
Discussion
LH Trajectories in MHD Patients
In this study, we found that the LH trajectories of MHD patients had distinct characteristics and identified a three-classes trajectory model. The LH of all three subgroups in stage T1 was significantly different (P<0.001). The high-decreasing group had the highest percentage (57.9%), indicating that more than half of the participants were at a high level of LH. As the treatment progressed, the LH of this group showed a slowly decreasing trend. Notably, this group’s lowest LH level remained higher than the highest in the other two groups during the follow-up period. This suggests that despite MHD being a traumatic event, most patients could gradually adjust and show resilient changes in their helplessness, consistent with Bonanno’s trajectory theory of psychological change29 and Seligman’s LH theory.30 This may be because patients in this class are good at using psychological resources (eg, social support, family support, peer support) to cope with helplessness. The measures that should be taken for this class of patients are maintaining attention and using positive interventions to facilitate the accelerated remission of their helplessness symptoms to normal levels.
Meanwhile, the results of this study showed that the low-stability group accounted for 20.7% of the overall participants, indicating that a small proportion of patients maintained a stable low level during the six-month follow-up period. This may be because patients in this group have a more rational cognition of ESRD and MHD. They regard MHD as an opportunity to prolong their lives and can adapt more quickly to changes.31 These characteristics can help them maintain lower LH levels. In addition, the low-increasing group accounted for 21.3%. This group had a low initial level of LH, but during the six-month follow-up period, the LH scores increased significantly. This may be because this group of patients had no in-depth knowledge at the beginning of MHD treatment and did not feel great psychological stress. However, with the duration of treatment, patients gradually become aware of the disease’s uncontrollability and the MHD’s chronicity. They need more family attention, support, and care, making them feel guilty about their needs.9 In addition, resuscitation and death of ward mates, dialysis complications, lifestyle restrictions, medical costs, and low social status are easy triggers for their helplessness.32
It can be seen that MHD patients experience different LH trajectories. Although most patients showed a gradual declining trend in this study, they remained above normal during the follow-up period. In addition, some patients were at low LH levels but had a risk for growth. Health care staff should prioritize these two classes of patients, provide early identification and dynamic assessment of their LH and offer psychological support at the right time to prevent more serious consequences.
Predictors of the Different LH Trajectories
First, this study found a significant gender difference between the three trajectories. The proportion of males in the high-decreasing and low-increasing groups was significantly higher than that of females compared to the low-stability groups. It reveals that males are more likely to experience high levels of LH and persistently rising LH than females in MHD patients. This distribution is similar to the results reported in other fields.33 In China, the family model of “men outside the home, women inside” dictates that men have more important financial responsibilities. Men experience more life stress and cumulative negative events than women. The loss of income due to the inability to work has dealt a fatal blow to male family status and self-esteem, which may be why males are more likely to experience high LH or increasing LH. In addition, middle-aged patients (45–59 years old) were 3.157 and 3.426 times more likely to be in the high-decreasing and low-increasing groups, respectively, than in the low-stability group. A Chinese proverb describes the survival status of middle-aged people: “There are old and young at home.” Middle-aged patients bear the double responsibility of family and society. However, MHD greatly limits their careers, marriage, and family. Loss of job, postdialysis fatigue, high medical costs, dietary and water restrictions, and poor health status greatly increase the sense of loss of control and helplessness of middle-aged patients regarding disease prognosis and their future life.
SSS may be another factor in predicting LH trajectories in MHD patients. The results showed that patients with low SSS were more likely to be in the high-decreasing and low-increasing groups than in the low-stability group. This is similar to the results of another study.34 Many previous studies have reported the relationship between SSS and mental health problems, especially with regard to negative psychological aspects such as helplessness and depression. This can be explained by the fact that people with higher SSS have more access to health care resources, health literacy, and disease management skills to cope with helplessness.35 On the other hand, individuals with low SSS may excessively adopt emotional dysregulation strategies accompanied by strong negative emotions to deal with various stresses or challenges in life, which increases their susceptibility to LH.36 Therefore, SSS may play an essential role in the LH status of MHD patients and influence their trajectories.
Predictive Effects of the Initial Level and Developmental Rate of LH on Self-Management
This study showed that MHD patients with higher initial LH scores and a faster developmental rate of LH had a lower level of future self-management, which verified that LH is a hindering factor for self-management behaviour. According to Seligman’s LH theory, this may be because helpless individuals have had uncontrollable experiences contributing to their negative attributions and cognitive biases.37 They tend to believe that their self-management behaviours do not correlate with disease outcomes and that their efforts will not change disease progression and death.38 At this point, helpless patients lack self-confidence, passivity, and self-abandonment in health-related behaviours and develop low motivation and self-efficacy when faced with disease management.39 Helplessness can negatively affect the individual’s self-management and complicate their health interventions.38 MHD patients who fall into persistent helplessness may believe that no one or treatment can change the outcome of their kidney failure.40 Unless patients change this belief, high levels and growing LH will hinder their treatment adherence and self-management behaviour. Therefore, future interventions focusing on LH to improve patients’ self-management behaviours may have better outcomes.
Limitations and Strengths
First, the study population was from a single blood purification centre in a southern Chinese city. The convenience sampling method limits the generalizability of the findings to some extent. Second, this study used patients’ self-report questionnaires, which may be subject to recall bias. Third, the follow-up period of this study was short, and the dynamic changes after six months need to be further observed in our future studies.
Despite these limitations, the current study contributes to existing research and has important implications for future clinical practice. First, to our knowledge, this is the first study to investigate the heterogeneous trajectories of LH in MHD patients. Second, the present study is based on a person-centred philosophy and focuses on a group more likely to feel helpless in response to illness-related events and HD treatment. This provides valuable information for developing targeted intervention programs for vulnerable groups.
Conclusion
This study confirmed the existence of heterogeneous trajectories by longitudinally assessing LH levels in MHD patients. This study confirmed the theory of psychological trajectories in patients with chronic diseases.41 That is, most patients will have a gradual remission of LH. A small number of patients will have a continuous increase in LH, which needs to be noted. Age, sex, and SSS can predict LH trajectories in MHD patients. In addition, the initial level and developmental rate of the LH trajectory were negative predictors of patients’ self-management. In future clinical practice, medical professionals should pay attention to assessing and predicting patients’ LH, focusing on patients with high LH levels and potential growth and adapting targeted interventions to improve their adherence and health behaviours.
Acknowledgments
We express our heartfelt gratitude to all members who assisted in the data collection and processing and to every MHD patient who participated in this study.
Funding
This research received grants from the National Natural Science Foundation of China (No. 81873806), Major Scientific and Technological Projects in Hunan Province (No. 2020SK2085), 2022 Hunan Province Postgraduate Scientific Research Innovation Project (No. 12300-150110021), and 2022 Central South University Postgraduate Independent Exploration and Innovation Program (No. 1053320213471).
Disclosure
All authors declare that they have no conflicts of interest for this work.
References
1. O’Hare AM. Dialysis adequacy reconsidered: the person comes first. Semin Dial. 2020;33(6):486–489.
2. Ertuglu LA, Demiray A, Basile C, Afsar B, Covic A, Kanbay M. Sodium and ultrafiltration profiling in hemodialysis: a long‐forgotten issue revisited. Hemodialysis Int. 2021;25(4):433–446.
3. Szu LY, Tsao LI, Chen SC, Ho ML. Self-Participation Experiences among Well-Adapted Hemodialysis Patients. Healthcare. 2021;9(12):1742.
4. Victoria A, Maria T, Vasiliki M, Fotoula B, Sofia Z. Adherence to Therapeutic Regimen in Adults Patients Undergoing Hemodialysis: the Role of Demographic and Clinical Characteristics. Int Arch Nurs Health Care. 2018;44(3):096.
5. Kim ES. Development and effect of a rational‐emotive‐behaviour‐therapy‐based self‐management programme for early renal dialysis patients. J Clin Nurs. 2018;2018(27):4179–4191.
6. Camacho EM, Verstappen SM, Chipping J, Symmons DP. Learned helplessness predicts functional disability, pain and fatigue in patients with recent-onset inflammatory polyarthritis. Rheumatology. 2013;52(7):1233–1238.
7. He H. Students’ Learned Helplessness and Teachers’ Care in EFL Classrooms. Front Psychol. 2021;6010.
8. Ok E, Kutlu FY. Hopelessness, Anxiety, Depression and Treatment Adherence in Chronic Hemodialysis Patients. Int J Caring Sci. 2019;12(1):423–429.
9. Yu-Ying C, Li-Ya T. Applying Swanson’s Caring Theory to a Patient With End Renal Stage Disease Experiencing Hopelessness. J Nursing. 2021;68(2):99–106.
10. Simoni JM, Asarnow JR, Munford PR, Koprowski CM, Belin TR, Salusky IB. Psychological distress and treatment adherence among children on dialysis. Pediatr Nephrol. 1997;11(5):604–606.
11. Andrade SV, Sesso R, Diniz DH. Hopelessness, suicide ideation, and depression in chronic kidney disease patients on hemodialysis or transplant recipients. J Bras Nefrol. 2015;37(1):55–63.
12. Tommel J, Evers AWM, van Hamersvelt HW, et al. Predicting health-related quality of life in dialysis patients: factors related to negative outcome expectancies and social support. Patient Educ Couns. 2021;104(6):1474–1480.
13. Lee K, Song HC, Choi EJ, Pae CU, Kim YK. Posttraumatic Embitterment Disorder in Patients with Chronic Kidney Disease. Clin Psychopharmacol Neurosci. 2019;17(2):183–188.
14. Maier SF, Seligman ME. Learned helplessness: theory and evidence. J Exp Psychol Gen. 1976;105(1):3.
15. Lorant V, Deliège D, Eaton W, Robert A, Ansseau M. Socioeconomic Inequalities in Depression: a Meta-Analysis. Am J Epidemiol. 2003;157(2):98–112.
16. Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: preliminary data in healthy white women. Health Psychol. 2000;19(6):586–592.
17. Operario D, Adler NE, Williams DR. Subjective social status: reliability and predictive utility for global health. Psychology Health. 2004;19(2):237–246.
18. Giatti L. Reliability of the MacArthur scale of subjective social status-Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). BMC Public Health. 2012;12(1):1–7.
19. Nicassio PM, Wallston KA, Callahan LF, Herbert MA, Pincus T. The measurement of helplessness in rheumatoid arthritis. The development of the Arthritis Helplessness Index. J Rheumatol. 1985;12(3):462–467.
20. Thumboo J, Feng PH, Chan SP, Boey ML, Thio ST, Fong KY. A Chinese version of the Rheumatology Attitudes Index is a valid and reliable measure of learned helplessness in patients with SLE. Lupus. 2002;11(2):88–94.
21. Song YJ. The Formation and Test of Hemodialysis SelfManagement Instrument. Kaohsiung Medical University; 2009.
22. Song YY, Chen L, Wang WX, Yang DJ, Jiang XL. Social Support, Sense of Coherence, and Self-Management among Hemodialysis Patients. West J Nurs Res. 2022;44(4):367–374.
23. Li H, Cao YD, Jiang YF, Wang JJ. Introduction and reliability testing of a self-management scale for hemodialysis patients (in Chinese). Chin J Nurs. 2015;50(11):1392–1395.
24. Huang X, Luo W, Huang H, He J. Trajectories of posttraumatic growth in young and middle-aged stroke patients and their predictive effects on mental health. Ann Palliat Med. 2021;10(9):9435–9442.
25. Danhauer SC, Greg R, Douglas CL, et al. Trajectories of Posttraumatic Growth and Associated Characteristics in Women with Breast Cancer. Ann Behav Med. 2015;1(5):650–659.
26. Shafiq M, Malhotra R, Teo I, Ozdemir S, Malhotra C. Trajectories of physical symptom burden and psychological distress during the last year of life in patients with a solid metastatic cancer. Psycho-Oncology. 2021;31(1):139–147.
27. Baussard AL, Proust-Lima C. Determinants of distinct trajectories of fatigue in patients undergoing chemotherapy for a metastatic colorectal cancer: 6-month follow-up using Growth Mixture Modeling. J Pain Symptom Manage. 2021;63(1):140–150.
28. Min WJ. A longitudinal study of cognitive trajectories and its factors for Koreans aged 60 and over: a latent growth mixture model. Int J Geriatr Psychiatry. 2018;33(5):755–762.
29. Bonann OGA, Ho SM, Chan JC. Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: a latent class approach. Health Psychol. 2008;27(5):659–667.
30. Seligman M, Weiss J, Weinraub M, Schulman A. Coping behavior: learned helplessness, physiological change and learned inactivity. Behav Res Therapy. 1980;18(5):459–512.
31. Palmer SC, Hanson CS, Craig JC, et al. Dietary and fluid restrictions in CKD: a thematic synthesis of patient views from qualitative studies. Am J Kidney Dis. 2015;65(4):559–573.
32. Tagay S, Kribben A, Hohenstein A, Mewes R, Senf W. Posttraumatic stress disorder in hemodialysis patients. Am J Kidney Dis. 2007;50(4):594–601.
33. Bolland AC, Besnoy KD, Tomek S, Bolland JM. The Effects of Academic Giftedness and Gender on Developmental Trajectories of Hopelessness Among Students Living in Economically Disadvantaged Neighborhoods. Gifted Child Quarterly. 2019;63(4):225–242.
34. Lim S, Powell TW, Xue QL, et al. The Longitudinal Association between Perceived Powerlessness and Sexual Risk Behaviors among Urban Youth: mediating and Moderating Effects. J Youth Adolesc. 2019;48(8):1532–1543.
35. Camacho EM, Verstappen S, Symmons D. Association between socioeconomic status, learned helplessness, and disease outcome in patients with inflammatory polyarthritis. Arthritis Care Res. 2012;64(8):1225–1232.
36. Cancan C, Yanting Z, Qiuge Z, Lyu W, Yan A, Xiuzhen F. The multiple mediating effects of social connectedness and self-care confidence on the relationship between subjective social status and emotional well-being in patients with heart failure: a cross-sectional study. Eur J Cardiovascular Nursing. 2022;21(3):227–234.
37. Seligman ME. Learned helplessness as a model of depression. Comment and integration. J Abnorm Psychol. 1978;87(1):165–179.
38. Omachi TA, Katz PP, Yelin EH, et al. The COPD Helplessness Index: a New Tool to Measure Factors Affecting Patient Self-Management. Chest. 2010;137(4):823–830.
39. Xie CY, Li L, Li YM. Learned Helplessness in Renal Dialysis Patients: concept Analysis with an Evolutionary Approach. Patient Prefer Adherence. 2022;24(16):2301–2312.
40. Avdal EU, Ayvaz İ, Uran BNÖ, Yildirim JG, Sofulu F, Pamuk G. Opinions of hemodialysis and peritoneum patients regarding depression and psychological problems which they experience: a qualitative study. J Infection Public Health. 2020;13(12):1988–1992.
41. Bonanno GA, Wortman CB, Lehman DR. Resilience to loss and chronic grief: a prospective study from preloss to 18-months postloss. J Pers Soc Psychol. 2002;83(5):1150–1164.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
