Back to Journals » Clinical Epidemiology » Volume 14
Trajectories in Outpatient Care for People with Multimorbidity: A Population-Based Register Study in Denmark
Authors Bell C , Prior A , Frølich A, Appel CW , Vedsted P
Received 23 February 2022
Accepted for publication 18 May 2022
Published 3 June 2022 Volume 2022:14 Pages 749—762
DOI https://doi.org/10.2147/CLEP.S363654
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Henrik Sørensen
Cathrine Bell,1 Anders Prior,2 Anne Frølich,3,4 Charlotte Weiling Appel,1 Peter Vedsted1,2
1Diagnostic Centre - University Research Clinic for Innovative Patient Pathways, Silkeborg Regional Hospital, Department of Clinical Medicine, Aarhus University, Silkeborg, Denmark; 2Research Unit for General Practice, Aarhus, Denmark; 3Innovation and Research Centre for Multimorbidity, Slagelse Hospital, Region Zealand, Denmark; 4Centre for General Practice, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark
Correspondence: Cathrine Bell, Diagnostic Centre - University Research Clinic for Innovative Patient Pathways, Silkeborg Regional Hospital, Department of Clinical Medicine, Aarhus University, Denmark, Tel +45 7841 7884, Email [email protected]
Background: Multimorbidity is a global health challenge. Individuals with multimorbidity are frequent users of healthcare services, and many experience fragmented healthcare. We assessed the number of outpatient trajectories and contacts with hospital outpatient clinics for individuals with multimorbidity and explored different time intervals for the occurrence of concurrent outpatient trajectories.
Methods: A population-based cohort of 1.3 million residents, ≥ 18 years, with multimorbidity was identified through Danish national health registries. Multimorbidity was defined as having two or more of 39 specific chronic conditions. Nine disease system categories were used to categorize outpatient contacts in 2018 into outpatient trajectories and trajectory-related contacts. We defined an “outpatient trajectory” as two contacts within 12 consecutive months for the same medical condition. All outpatient contacts and trajectories with related contacts were counted for 2018. The impact of different time intervals on the number of concurrent trajectories was analyzed.
Results: On 1 January 2019, 29% of the adult Danish population was classified as multimorbid. During 2018, 68% of them had ≥ 1 outpatient contact (median: 2 (IQI: 0– 4)). Twenty-six percent had ≥ 1 outpatient trajectory. The median number of trajectory contacts was 3 (IQI: 2– 5). The 4% of individuals with ≥ 2 outpatient trajectories accounted for 28% of trajectory contacts. During the 6-week period from the latest outpatient contact, 33% of all patients with ≥ 2 trajectories in 2018 experienced concurrent trajectories with outpatient contact.
Conclusion: Two-thirds of adult Danes with multimorbidity attended an outpatient clinic in 2018, and one-fourth had at least one outpatient trajectory. Individuals with two or more trajectories represented 4% and comprised 28% of the trajectory contacts; 33% had concurrent trajectories within a 6-week period. It appears that a small proportion place demands on outpatient clinics because of frequent attendance. A more uniform way of organizing outpatient trajectories for these patients merits consideration.
Keywords: outpatient, hospital, multimorbidity, prevalence, healthcare utilization, trajectory
Plain Language Summary
What is new
- This study provides a novel approach for identifying hospital outpatient trajectories for people with multimorbidity.
- The extent of concurrent outpatient trajectories has not previously been investigated, and this study investigates different time intervals for estimating their prevalence.
- The results inform future research on integration through alignment of outpatient trajectories.
Introduction
Multimorbidity is defined by the World Health Organization (WHO) as the coexistence of two or more chronic conditions in an individual.1–3 The prevalence of multimorbidity varies widely, depending on study populations, the definition of multimorbidity, and the diseases included,4–10 where a prevalence of 20–30% has often been documented in general populations of adults.4,7,9 Multimorbidity is a major concern in public healthcare due to increasing life expectancy and development of multiple chronic conditions.11–15 Multimorbidity often requires outpatient hospital attendance, and the number of contacts has been shown to rise in parallel with an increasing number of chronic conditions.9,16–19 Disease patterns and treatment regimens may be manifold, represent high severity, and make healthcare management complex.20–24 Hospital care has gradually shifted towards more specialized services, but clinical guidelines and disease management programs remain focused on managing individual conditions.25,26 Thus, the management of care is challenged when healthcare providers are faced with multimorbid patients with interacting diseases because these patients may have several providers managing their care.24,27–33 Research exploring outpatient attendance in hospitals among patients with multimorbidity is limited9,13,17–21,33–35 and does not categorize data into outcomes of outpatient trajectories. A Danish study showed that the proportion of patients treated in multiple hospital outpatient clinics nearly doubled during a 10-year period.13 Measuring multimorbidity and defining patients in an outpatient trajectory is complex, challenging the research in this area.1,36 This necessitates methodological approaches to identify long-term outpatient trajectories that, go beyond determining the number of visits to outpatient clinics. Another factor to consider is the time interval studied, which will determine the number of concurrent outpatient trajectories. If different outpatient trajectories take place simultaneously within a compatible time interval, integration through alignment of outpatient contacts may be considered.33 Thus, exploring how different time intervals modulate the number of concurring outpatient trajectories and the number of contacts to hospital outpatient clinics may inform the design of future interventions for patients with multimorbidity with the aim of integrating parallel outpatient trajectories.
The aim of this study was to assess the number of outpatient trajectories and the number of contacts to hospital outpatient clinics for people with multimorbidity, and to explore different time intervals for finding concurrent outpatient trajectories.
Methods
Setting
The study was conducted in Denmark, which has a population of 5.8 million residents.37 Denmark is a high-income country, and the demographic development is similar to that in other Western European countries.38 The Danish healthcare system is publicly funded through taxation, providing free access to general practitioners and hospital care. Reimbursement for prescribed medicine is available for some patient groups and for certain diseases.38,39 Denmark has a long tradition of routinely recording administrative, health, and clinical data. Data are registered for each resident using the unique 10-digit personal identification number assigned to all Danish residents at birth or immigration. This enables accurate linkage of data across registries. The personal number is stored in the Danish Civil Registration System (CRS), which contains continuously updated information on place of residence, vital status, and emigration/immigration.40
Study Design
This study was designed as a population-based register study, including all individuals with multimorbidity, aged ≥18 years, and residing in Denmark for at least 1 year before the index date (1 January 2019). We identified outpatient hospital contacts in 2018 for all eligible individuals, and these contacts were categorized into trajectories.
Study Population
Data from the CRS were used to establish our study population, which included all adult individuals living in Denmark (N=4.6 million) on the index date. WHO’s definition (two or more chronic conditions)1–3 and the Danish Multimorbidity Index by Prior et al formed the basis for establishing multimorbidity.41 The Danish Multimorbidity Index includes information on 39 chronic conditions (Appendix 1). Information on chronic conditions in the cohort was obtained from the Danish National Patient Register (NPR) from 1993 onwards, and from the Danish Psychiatric Central Register (DPCR), from 1995 onwards. The NPR holds information on all treatment at public and private somatic hospitals in Denmark, including inpatient hospital care and outpatient specialist care,42 whereas the DPCR holds records on psychiatric treatment.43 Since 1993, all contacts have been coded as a specific condition based on WHO’s International Classification of Diseases, 10th revision (ICD-10).
Conditions were further identified by use of condition-specific medication through the Danish National Drug Prescription Register (NDPR). The NDPR contains data on medication prescriptions redeemed at Danish pharmacies and coded according to the Anatomical Therapeutic Chemical (ATC) classification system. ATC codes 2 years prior to the index date were included.44 To ensure condition chronicity, medical conditions and medical prescriptions were limited to those occurring for the first time at least 6 months prior to the index date.
Outcomes
Four outcomes were investigated: hospital outpatient contacts, hospital outpatient trajectories, trajectory contacts, and concurrent outpatient trajectories.
Hospital Outpatient Contacts
Our data included all hospital outpatient contacts from 1 January to 31 December 2018. Information on outpatient activity came from the NPR. We excluded duplicate contacts and outpatient contacts to emergency rooms. This outcome provided an overview of all with outpatient attendance in 2018. The following outcomes were based on a selection of chronic conditions for assessment of outpatient trajectories.
Hospital Outpatient Trajectories
We categorized the outpatient contacts of the study population according to their medical conditions by using the “disease system categories” from the Danish Multimorbidity Index by Prior et al.41 This entailed sorting the outpatient contacts related to 31 chronic conditions. These categories (circulatory, endocrine, pulmonary, gastrointestinal, urogenital, musculoskeletal, hematologic, neurologic, and cancer) were applied as proxies for determining the medical specialties responsible for the outpatient trajectories. This categorization was for the most part in accordance with the classification of diagnoses based on the organization of somatic care in Danish hospitals.45 Mental health conditions were excluded as an outpatient trajectory category because these conditions do not entail somatic outpatient trajectories. Thus, nine disease system categories for outpatient trajectories were defined (Appendix 1).
To ensure inclusion of active trajectories, at least one of the outpatient contacts for each medical condition had to be in 2018. We defined a trajectory for the same medical condition as at least two outpatient contacts within 12 months from the latest outpatient contact (Figure 1). The number of outpatient trajectories in 2018 was tabulated for each individual, regardless of concurrency.
Trajectory Contacts
The number of trajectory contacts was calculated by adding up all outpatient contacts in the nine outpatient trajectories. We did not include contacts that were not part of a trajectory. This supplemented our “hospital outpatient trajectories” outcome by extending information on the number of outpatient contacts related to these trajectories.
Concurrent Outpatient Trajectories
To assess concurrency, we identified outpatient trajectories with overlapping time periods. The latest trajectory contact date in 2018 was used as a starting point. By moving backwards in time intervals of 2-, 6-, 10-, 14-, 18-, 22-, and 26-weeks from the starting point, concurrent trajectories were identified and summed up per individual across the nine categories of outpatient trajectories. Outpatient trajectories with the latest contact date at the beginning of 2018 were followed up into 2017 to ensure a study period of up to 26 weeks (Figure 1).
Covariates
The following sociodemographic variables were obtained from Statistics Denmark on the index date and used to describe the study population: gender, age, educational level, country of origin, civil status, population density, occupation, and household income. Age was grouped into five categories: <50, 50–59, 60–69, 70–79, and ≥80 years. Data on educational level were grouped according to the International Standard Classification of Education 2011.46 Country of origin followed the categorization made by Statistics Denmark into Western and non-Western countries.47 Population density was grouped into >5000, 5000–99,999, and <100,000 inhabitants per town according to the registered place of residence of each patient. Civil status was dichotomized into living with a partner or living alone. Occupational status was categorized into employed, unemployed, or student,47 and household income in 2018 was categorized into EUR <25,000, 25,000–49,999, 50,000–74,999, and >75,000.
Statistical Analysis
This study used descriptive statistics reported as proportions and medians with interquartile intervals (IQI). A Lorenz diagram was used to display the accumulated number of people with multimorbidity according to their accumulated number of trajectory contacts. Bar plots were used to show the outpatient attendance of patients with concurrent trajectories according to different time intervals. All statistical analyses were conducted in Stata version 16.0 via data access through a remote server at Statistics Denmark.
Ethical Considerations
Approval of the study was obtained from the Danish Data Protection Agency (file no. 2016–051-000001). According to Danish legislation, no further ethical approval was required for register-based studies and informed consent was not obtained from the participants. The study complies with the Declaration of Helsinki. The STROBE guidelines were used to ensure adequate reporting and transparency.
Results
Population
On the index date, 1,339,840 adult individuals (29%) were identified as having lived with multimorbidity for at least 6 months; this cohort comprised the study population. Circulatory conditions were present in 77.5% of the study population, with hypertension being the most frequent condition (Table 1). Females accounted for 54.3%, and individuals aged ≥70 years constituted 69.4% (median: 68 years (IQI: 57–76)) of the study population. The distribution of the other characteristics is displayed in Table 2.
 |
Table 1 Chronic Conditionsa in Individuals with Multimorbidity in Denmark, 1 January 2019 |
 |
Table 2 Characteristics of All Individuals with Multimorbidity (≥2 Conditions) Living in Denmark on 1 January 2019 |
Hospital Outpatient Contacts
In total, 913,502 (68.2%) of the study population had at least one hospital outpatient contact in 2018 (5,033,144 contacts), median two contacts (IQI: 0–4).
Hospital Outpatient Trajectories
In 2018, 25.9% (N = 346,979) of the study population had at least one outpatient trajectory: 22.3% had one outpatient trajectory and 3.6% had two or more outpatient trajectories (Table 3). Thus, 74.1% had no outpatient trajectory.
 |
Table 3 Hospital Outpatient Trajectories and Related Trajectory Contacts from Individuals with Multimorbidity in 2018 |
Trajectory Contacts
For individuals in at least one outpatient trajectory, the median number of trajectory contacts was three (IQI: 2–5) for 2018. For those with four or more outpatient trajectories in 2018, the median number of trajectory contacts was 15 (IQI: 11–24). The 3.6% with two or more trajectories in 2018 accounted for 27.7% of all trajectory contacts (Table 3). The Lorenz diagram showed that the 10% with most trajectory contacts accounted for 80% of all trajectory-related contacts (Figure 2). Cancer trajectories involved the highest number of trajectory contacts (median: 4 (IQI: 2–10)), accounting for 31.7% of all trajectory contacts (Table 4), although only 8.6% of the study population was diagnosed with cancer (Table 1).
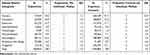 |
Table 4 Outpatient Trajectories According to Disease System Categories in Adults with Multimorbidity in 2018 |
 |
Figure 2 Lorenz diagram of the cumulated proportion of individuals with multimorbidity on 1 January 2019 according to the cumulated proportion of trajectory-related contacts in 2018. |
Concurrent Trajectories
Figure 3 shows the number of individuals in concurrent trajectories according to different time intervals in 2018. In all, 48,078 individuals had two or more trajectories in 2018 (see Table 3). Of these, 32.5% = 15.624 individuals had concurrent trajectories (with contacts related to their trajectory) within a 6-week period, as shown in Figure 3. This amounted to 1.2% of the study population and involved 31,815 contacts. When the time interval was expanded to a 10-week period, the proportion increased to 47.2% = 22,690 individuals with concurrent trajectories. This amounted to 1.7% of the study population and involved 46,576 contacts. The number of concurrent trajectories increased with increasing time intervals. Only 4000 individuals (<0.1%) were in three or more concurrent trajectories during the studied time intervals, which ranged from 2 weeks to 26 weeks since the latest outpatient contact in 2018 (Figure 3).
 |
Figure 3 Histogram displaying the number of individuals in concurrent trajectories in 2018 according to different observation times, stratified by the number of concurrent trajectories. |
The most frequently seen concurrent trajectories included patients with cancer or diseases of the circulatory system, endocrine system, and neurological system; these were seen over all the different time intervals observed (Figure 4).
 |
Figure 4 Bar plot of concurrent trajectories for 2018 according to different observation times, stratified by disease system category and the number of weeks since the most recent contact. |
Discussion
Main Results
This population-based study showed that 68.2% of individuals with multimorbidity had at least one hospital outpatient contact during a 1-year period, and 25.9% were involved in at least one outpatient trajectory. The 3.6% with multimorbidity and two or more trajectories accounted for almost one third of the trajectory contacts, and one-third of these experienced concurrent trajectories within a 6-week period. Thus, 1.2% of all individuals with multimorbidity were found to be in concurrent trajectories within a 6-week period.
Comparison with Existing Research
Research investigating the utilization of hospital outpatient clinics among individuals with multimorbidity is sparse,9,13,18–21,34,48–50 and the existing studies do not explore healthcare utilization in patients in outpatient trajectories and the concurrence of these trajectories.
A Danish study demonstrated a consistent increase in healthcare utilization that rose by the number of chronic conditions.9 Individuals with multimorbidity had a mean of 3.9 outpatient visits. Although the study included only 16 diseases in the definition of multimorbidity,9 the number of visits was in line with our median result of two outpatient contacts.
The Danish public health and research institution SSI estimated that 85% of individuals with multimorbidity had an outpatient contact to a somatic hospital in 2014 and a mean of 9.1 outpatient contacts.49 Only chronic obstructive pulmonary disease, rheumatoid arthritis, osteoporosis, diabetes mellitus, heart failure, and asthma were included in the estimates of multimorbidity and utilization. Our findings support that a high proportion of people with multimorbidity have outpatient contacts. Previous studies included conditions associated with regular healthcare contacts.20,21 Additionally, we included only conditions with a minimum duration of 6 months in our definition of chronicity before inclusion.
Another Danish study demonstrated a time-related increase in the number of adults attending one or multiple outpatient clinics.13 The numbers doubled over a 10-year period, representing 6% of the adult Danish population in 2014. This corresponds to our result showing that 25.9% with multimorbidity had at least one outpatient trajectory, which is equivalent to 8% of the adult Danish population. The two studies resemble each other in terms of source population (Danes) and contacts related to ICD-10 codes.
Many chronic conditions will not require a patient to be in an outpatient trajectory with specialist treatment, whereas others will mandate extensive outpatient care. This is confirmed by our results, as three-fourths of the individuals with multimorbidity were not involved in an outpatient trajectory. Increasing numbers and specific combinations of conditions may increase the burden of illness, which can lead to extensive use of specialist services.9,16,17,20,21,51
We found no studies similar to ours that explore the modifying effect of time intervals on the number of concurring outpatient trajectories and trajectory contacts. Previous studies used a fixed 1-year time interval to assess outpatient contacts.9,13,49
Strengths and Limitations
The key strength of this study is the considerable size of the study population and the use of data recorded in nationwide Danish registers, because this allowed us to follow the entire cohort owing to their individual identification numbers.40 The data have high validity and completeness because they are continuously collected, and the provided clinical care is quality controlled and recorded by specialized healthcare professionals in diverse medical fields.39,40,42–44
The Danish Multimorbidity Index has previously been used to establish multimorbidity.41,52 The inclusion of redeemed drug prescriptions ensured that only active and relevant diagnoses were included. Additionally, this enabled identification of individuals with conditions that had not yet been diagnosed by a hospital specialist.
Moreover, we developed a novel approach by looking backwards in time to assess concurrent trajectories. This method enabled total follow-up and full-length analysis of the time periods. As patients may bounce in and out of trajectories, our method ensured relevance and continuity in the estimation of a patient’s outpatient trajectory.
The data are limited to individuals who had been diagnosed or treated for a condition and who had been in contact with hospital healthcare services. Although all Danish hospitals and outpatient clinics report to the NPR, chronic conditions with less severity are not registered until the individual seeks medical treatment at a hospital or redeems a prescription for medication related to the condition. Thus, the study population is likely to have been underestimated. Information on severity of conditions is not available through the registers, however, we feel confident that we included the individuals with the most severe chronic conditions.
This study does not contribute to determining how the response variables are affected by different covariates. The covariates serve solely to describe the study population of individuals with multimorbidity, yet previous research points to demographic and social disparities in healthcare utilization.9 Our focus was on estimating the frequency of outpatient attendance, but we also provided stratified results on the specialties that were the largest contributors of outpatient trajectories and related outpatient contacts.
The categorization of outpatient trajectories according to a limited number of specific conditions is likely to have underestimated the number of actual hospital outpatient trajectories, because outpatient clinics provide a variety of services for a wide range of different diagnoses. However, this was done because of the diverse organization of outpatient clinics in Danish hospitals. Some outpatient clinics cover a broad range of conditions, including conditions treated across several medical specialties. Some conditions can be managed and treated by more than one outpatient specialty, which makes it difficult to categorize conditions into trajectories. Most patients are in one outpatient trajectory per condition, and one medical specialty will be responsible for the treatment.33 Furthermore, if a patient has several conditions treated within the same specialty, they will often be combined into the same outpatient trajectory. However, our categorization into outpatient trajectories is a pragmatic solution to determining healthcare utilization, and this approach resembles the method applied in a previous study.13
Implications
The indices for multimorbidity were founded on both secondary care diagnoses and pharmacy data from redeemed drug prescriptions. Redeemed drug prescriptions may serve as a proxy for diagnoses managed in primary care. Hence, this was not a hospital-based population, and the patients were not selected based on use of outpatient clinics. A large segment of individuals with no interest in outpatient contact was included, which made this a mapping of multimorbidity that can be generalized to all adults.
Our results indicate that a small proportion of individuals with multimorbidity place heavy demands on outpatient clinics because of frequent attendance. Many of those with concurrent trajectories have frequent contacts within short-term intervals. Multimorbidity is associated with high outpatient expenditures, and the number of outpatient contacts increase with the number of chronic conditions.9,19,49 The average regional healthcare expenditures are 3.5 higher for individuals with multimorbidity than for the general population, and hospital outpatient care constitutes 30% of all regional healthcare expenditures in Denmark.49 Thus, introducing a more uniform way of organizing outpatient trajectories may prove beneficial. This could be done by aligning parallel trajectories with combined visits and augmented collaboration across medical specialties, which has been attempted and reported in previous research.33 This research demonstrated that is was possible in 15% of all outpatient contacts that occurred within 6 weeks to align attendances to the same day, along with integration of medical specialties.33 Our present study showed that a small group of patients with multimorbidity may be candidates for having an incorporation of outpatient trajectories that makes possible alignment of outpatient visits into joint visits across specialties as attempted in previous research.
Using different time intervals to identify concurrent outpatient trajectories enables alignment of outpatient contacts, which is likely to reduce hospital attendance. Our results point to a potential for alignment of contacts, because large numbers of patients were seen repeatedly, at short intervals, in multiple trajectories. This may promote cooperation and collaboration between medical specialties, which could contribute to fewer hospital encounters and integrated healthcare for individuals with multimorbidity.
More research is needed to understand the utilization of hospital healthcare services according to patient characteristics because such knowledge could benefit healthcare planning and prioritization of healthcare service resources. Furthermore, the introduction of an integrated care scheme may provide a more efficient provision of outpatient healthcare for individuals with multimorbidity.
Conclusion
In 2018, 68.2% of individuals with multimorbidity had at least one outpatient contact, and 25.9% were followed in an outpatient trajectory. The majority had a single trajectory, and 3.6% had two or more. While 10% of individuals with multimorbidity accounted for 80% of all trajectory contacts, individuals with two or more trajectories accounted for one fourth of all trajectory contacts. Concurrence of trajectories depended on the time intervals investigated. During a 6-week time interval, 32.5% of individuals in two or more trajectories in 2018 had concurrent outpatient trajectories (during a 10-week time interval, this amounted to 47%), which constituted 1.2% of the study population. More research is needed to understand who the patients are in outpatient trajectories, to integrate medical healthcare services, and to improve care organization.
Highlights
- Two thirds of adult Danes with multimorbidity attended an outpatient clinic in 2018, and one fourth had at least one outpatient trajectory.
- Patients with two or more outpatient trajectories represent a small proportion (4%) of individuals with multimorbidity, yet they place heavy demands on outpatient clinics because of frequent attendance.
- Within a 6-week period, 33% of those with two or more outpatient trajectories were in concurrent trajectories with outpatient attendance.
- The major contributors to hospital outpatient trajectories are people with chronic conditions related to cancer or the circulatory, endocrine, and neurological systems.
Abbreviations
ACT, Anatomical Therapeutic Chemical (classification system); CRS, Civil Registration System; DPCR, Danish Psychiatric Central Register; ICD-10, International Classification of Diseases, 10th revision; IQI, Interquartile interval; NDPR, National Drug Prescription Register; SSI, Statens Serum Institut (Danish public health surveillance institution); STROBE, STrengthening the Reporting of OBservational studies in Epidemiology; WHO, World Health Organization.
Acknowledgments
The authors would like to acknowledge the contributions and give thanks to legal advisor Tommy K. Simonsen for setting up legal agreements related to this research project, to data manager Marianne Pedersen for providing register data and advice on data management, to Asger R. Pedersen for statistical assistance, and language editor Lone Niedziella and Edwin Spencer for revising the manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Novo Nordisk Foundation (agreement number: NNF18OC0052136), Aarhus University, and the Toyota Foundation, Denmark. The authors have no affiliation with the funders, and the funders had no role in initiating or in carrying out this research.
Disclosure
The authors report no conflicts of interest in this work.
References
1. van den Akker MBF, Knottnerus JA, Knottnerus JA. Comorbidity or multimorbidity: what’s in a name? A review of literature. Eur J Gen Pract. 1996;2:65–70. doi:10.3109/13814789609162146
2. Johnston MC, Crilly M, Black C, Prescott GJ, Mercer SW. Defining and measuring multimorbidity: a systematic review of systematic reviews. Eur J Public Health. 2019;29:182–189. doi:10.1093/eurpub/cky098
3. World Health Organization. Multimorbidity. Geneva: World Health Organization; 2016. ISBN:978-92-4-151165-0.
4. Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43. doi:10.1016/S0140-6736(12)60240-2
5. Fortin M, Stewart M, Poitras ME, et al. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med. 2012;10:142–151. doi:10.1370/afm.1337
6. Violan C, Foguet-Boreu Q, Flores-Mateo G, et al. Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLoS One. 2014;9:e102149. doi:10.1371/journal.pone.0102149
7. Xu X, Mishra GD, Jones M. Evidence on multimorbidity from definition to intervention: an overview of systematic reviews. Ageing Res Rev. 2017;37:53–68. doi:10.1016/j.arr.2017.05.003
8. Willadsen TG, Bebe A, Koster-Rasmussen R, et al. The role of diseases, risk factors and symptoms in the definition of multimorbidity - a systematic review. Scand J Prim Health Care. 2016;34:112–121. doi:10.3109/02813432.2016.1153242
9. Frølich A, Ghith N, Schiøtz M, et al. Multimorbidity, healthcare utilization and socioeconomic status: a register-based study in Denmark. PLoS One. 2019;14:e0214183. doi:10.1371/journal.pone.0214183
10. Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10:430–439. doi:10.1016/j.arr.2011.03.003
11. Sundhedsstyrelsen [The National Board of Health]. Danskernes Sundhed - Den Nationale Sundhedsprofil 2017 [Danes health - the national health profile 2017]. 2018.
12. Freid VM, Bernstein AB, Bush MA. Multiple chronic conditions among adults aged 45 and over: trends over the past 10 years. NCHS Data Brief. 2012;7:1–8.
13. Wolff DL, Von Plessen C, Waldorff FB, et al. Time trends in patients managed simultaneously in multiple hospital outpatient specialty clinics for chronic diseases: a register-based cross-sectional study. J Comorb. 2019;9:2235042x19831907. doi:10.1177/2235042X19831907
14. James SL, Abate D, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858.
15. Soley-Bori M, Ashworth M, Bisquera A, et al. Impact of multimorbidity on healthcare costs and utilisation: a systematic review of the UK literature. Br J Gen Pract. 2021;71:e39–e46. doi:10.3399/bjgp20X713897
16. Zhao Y, Zhang P, Oldenburg B, et al. The impact of mental and physical multimorbidity on healthcare utilization and health spending in China: a nationwide longitudinal population-based study. Int J Geriatr Psychiatry. 2021;36:500–510. doi:10.1002/gps.5445
17. Palladino R, Tayu Lee J, Ashworth M, et al. Associations between multimorbidity, healthcare utilisation and health status: evidence from 16 European countries. Age Ageing. 2016;45:431–435. doi:10.1093/ageing/afw044
18. Marthias T, Anindya K, Ng N, et al. Impact of non-communicable disease multimorbidity on health service use, catastrophic health expenditure and productivity loss in Indonesia: a population-based panel data analysis study. BMJ Open. 2021;11:e041870. doi:10.1136/bmjopen-2020-041870
19. Muggah E, Graves E, Bennett C, et al. The impact of multiple chronic diseases on ambulatory care use; a population based study in Ontario, Canada. BMC Health Serv Res. 2012;12:452. doi:10.1186/1472-6963-12-452
20. Juul-Larsen HG, Christensen LD, Bandholm T, et al. Patterns of multimorbidity and differences in healthcare utilization and complexity among acutely hospitalized medical patients (≥65 Years) - A latent class approach. Clin Epidemiol. 2020;12:245–259. doi:10.2147/CLEP.S226586
21. Sum G, Salisbury C, Koh GC, et al. Implications of multimorbidity patterns on health care utilisation and quality of life in middle-income countries: cross-sectional analysis. J Glob Health. 2019;9:020413. doi:10.7189/jogh.09.020413
22. Nissen NK, Aarhus R, Ørtenblad L. Dynamics of a specialized and complex health care system: exploring general practitioners’ management of multimorbidity. Chronic Illn. 2020;4:1742395320928403.
23. Ørtenblad L, Meillier L, Jønsson AR. Multi-morbidity: a patient perspective on navigating the health care system and everyday life. Chronic Illn. 2018;14:271–282. doi:10.1177/1742395317731607
24. Pedersen AF, Noroxe KB, Vedsted P. Influence of patient multimorbidity on GP burnout: a survey and register-based study in Danish general practice. Br J Gen Pract. 2020;70:e95–e101. doi:10.3399/bjgp20X707837
25. Guthrie B, Payne K, Alderson P, et al. Adapting clinical guidelines to take account of multimorbidity. BMJ. 2012;345:e6341. doi:10.1136/bmj.e6341
26. Kastner M, Hayden L, Wong G, et al. Underlying mechanisms of complex interventions addressing the care of older adults with multimorbidity: a realist review. BMJ open. 2019;9:e025009–2018. doi:10.1136/bmjopen-2018-025009
27. Sondergaard E, Willadsen TG, Guassora AD, et al. Problems and challenges in relation to the treatment of patients with multimorbidity: general practitioners’ views and attitudes. Scand J Prim Health Care. 2015;33:121–126. doi:10.3109/02813432.2015.1041828
28. Hughes LD, McMurdo ME, Guthrie B. Guidelines for people not for diseases: the challenges of applying UK clinical guidelines to people with multimorbidity. Age Ageing. 2013;42:62–69. doi:10.1093/ageing/afs100
29. Boyd CM, Wolff JL, Giovannetti E, et al. Healthcare task difficulty among older adults with multimorbidity. Med Care. 2014;52:S118–25. doi:10.1097/MLR.0b013e3182a977da
30. Rosbach M, Andersen JS. Patient-experienced burden of treatment in patients with multimorbidity - A systematic review of qualitative data. PLoS One. 2017;12:e0179916. doi:10.1371/journal.pone.0179916
31. Kailasam M, Guo W, Hsann YM, et al. Prevalence of care fragmentation among outpatients attending specialist clinics in a regional hospital in Singapore: a cross-sectional study. BMJ Open. 2019;9:e022965. doi:10.1136/bmjopen-2018-022965
32. Wang C, Kuo HC, Cheng SF, et al. Continuity of care and multiple chronic conditions impact frequent use of outpatient services. Health Informatics J. 2020;26:318–327. doi:10.1177/1460458218824720
33. Bell C, Appel CW, Frølich A, et al. Improving health care for patients with multimorbidity: a mixed-methods study to explore the feasibility and process of aligning scheduled outpatient appointments through collaboration between medical specialties. Int J Integr Care. 2022;22:17. doi:10.5334/ijic.6013
34. Zulman DM, Pal Chee C, Wagner TH, et al. Multimorbidity and healthcare utilisation among high-cost patients in the US veterans affairs health care system. BMJ Open. 2015;5:e007771. doi:10.1136/bmjopen-2015-007771
35. Pinaire J, Azé J, Bringay S, et al. Patient healthcare trajectory. An Essent Monit Tool. 2017;5:1–8.
36. Vetrano DL, Roso-Llorach A, Fernández S, et al. Twelve-year clinical trajectories of multimorbidity in a population of older adults. Nat Commun. 2020;11:3223. doi:10.1038/s41467-020-16780-x
37. Statistics Denmark. Population and Election. StatBank Denmark; 2019.
38. Olejaz M, Juul Nielsen A, Rudkjøbing A. Denmark: Health System Review. European Observatory on Health Systems and Policies. World Health Organization. Regional Office for Europe; 2012.
39. Schmidt M, Schmidt SAJ, Adelborg K, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563–591. doi:10.2147/CLEP.S179083
40. Pedersen CB. The Danish civil registration system. Scand J Public Health. 2011;39:22–25. doi:10.1177/1403494810387965
41. Prior A, Fenger-Grøn M, Larsen KK, et al. The association between perceived stress and mortality among people with multimorbidity: a prospective population-based cohort study. Am J Epidemiol. 2016;184:199–210. doi:10.1093/aje/kwv324
42. Lynge E, Sandegaard JL, Rebolj M. The Danish national patient register. Scand J Public Health. 2011;39:30–33. doi:10.1177/1403494811401482
43. Mors O, Perto GP, Mortensen PB. The Danish psychiatric central research register. Scand J Public Health. 2011;39:54–57. doi:10.1177/1403494810395825
44. Rasmussen L, Valentin J, Gesser KM, et al. Validity of the prescriber information in the Danish national prescription registry. Basic Clin Pharmacol Toxicol. 2016;119:376–380. doi:10.1111/bcpt.12610
45. Statistics Denmark. Classification of diagnoses based on organisation of hospital care [DIAG23 sygehusafdelingers organisering af behandlingen]; 2021. Available from: http://www.dst.dk/da/Statistik/dokumentation/Times/sygehusbenyttelse/diag23.
46. UNESCO. International standard classification of education 11th revision. Available from: http://uis.unesco.org/en/topic/international-standard-classification-education-isced.
47. Statistics Denmark. Documentation. Available from: https://www.dst.dk/da/Statistik/dokumentation/.
48. Saaby M, Kongstad SL, Lydiksen NVC, et al. Health Economic Costs for People with Multimorbidity and Complex Multimorbid Patients. University of Southern Denmark, Danish Centre for Health Economics - COHERE; 2017.
49. Statens Serum Institut. High costs associated with multimorbidity [Store udgifter forbundet med multisygdom]. 2015.
50. Joshi R, Santoshi JA, Rai N, et al. Prevalence and patterns of coexistence of multiple chronic conditions: a study from Indian urban outpatient setting. J Family Med Prim Care. 2015;4:411–415. doi:10.4103/2249-4863.161340
51. Zhao Y, Atun R, Oldenburg B, et al. Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: an analysis of population-based panel data. Lancet Glob Health. 2020;8:e840–e9. doi:10.1016/S2214-109X(20)30127-3
52. Momen NC, Plana-Ripoll O, Agerbo E, et al. Association between mental disorders and subsequent medical conditions. N Engl J Med. 2020;382:1721–1731. doi:10.1056/NEJMoa1915784
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

