Back to Journals » Orthopedic Research and Reviews » Volume 12
Three Femoral Stem Designs Without Corrosion: A Review of 2095 Stems
Authors Naudie DDR , Ndoja S , Wood TJ, Somerville LE, Howard JL, McCalden RW, MacDonald SJ , Lanting BA
Received 1 May 2020
Accepted for publication 10 August 2020
Published 17 September 2020 Volume 2020:12 Pages 145—150
DOI https://doi.org/10.2147/ORR.S259337
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Douglas DR Naudie,1,2 Silvio Ndoja,1 Thomas J Wood,3 Lyndsay E Somerville,1 James L Howard,1,2 Richard W McCalden,1,2 Steven J MacDonald,1,2 Brent A Lanting1,2
1Division of Orthopaedic Surgery, Department of Surgery, London Health Sciences, London, Ontario, Canada; 2Bone and Joint Institute, Western University, London, Ontario, Canada; 3Division of Orthopaedic Surgery, Department of Surgery, Hamilton Health Sciences, McMaster University, Hamilton, Ontario, Canada
Correspondence: Douglas DR Naudie
Division of Orthopaedic Surgery, Department of Surgery, Western University, Schulich School of Medicine, London Health Sciences Centre, University Campus, A9-028,339 Windermere Road, London, Ontario N6A 5A5, Canada
Email [email protected]
Introduction: Corrosion at the head–neck interface of modular components in total hip arthroplasty (THA) has been reported as a cause of failure of modern total hip replacement implants. While this method of failure has been well described, it remains poorly understood. The purpose of this study is to review the three most commonly used uncemented femoral stems at our institution over the last fifteen years and to correlate any established risk factors with rates of revision, particularly corrosion.
Methods: We reviewed 2095 patients from March 2000 to September 2015 who underwent total hip arthroplasty with one of three uncemented femoral stem designs. All stems were made of a Ti6Al4V alloy with a 12/14 taper design. We included only those stems coupled with a CoCr head and a highly crosslinked polyethylene liner. We evaluated age, gender, body mass index (BMI), femoral head size, head length, neck angle and offset and correlated these to the incidence of all cause revision, as well as revision excluding infection.
Results: There were no recognized corrosion-related revisions identified. There was no association between age, BMI, gender, head length, neck angle and offset to all cause revision or revision with infection excluded (p> 0.05). Femoral head size less than 32mm was associated with higher all cause revision rates (OR 4.60 (95% CI 1.8, 11.8)) and when excluding infection as a reason for revision (OR 4.94 (95% CI 1.7, 14.41)).
Conclusion: Over the last fifteen years, we have not identified any cases of corrosion with the three most commonly used femoral stems used at out institution. While we acknowledge that no femoral stem is immune to corrosion, certain femoral stem designs may be uniquely resistant to this mode of failure.
Level of Evidence: III.
Keywords: corrosion, revision, total hip arthroplasty, femoral stems
Introduction
Total hip arthroplasty is a highly successful orthopedic procedure with long-term success largely dictated by implant longevity.1 Implant longevity is based on many factors including surgical technique, implant material, and implant design. The use of a modular head neck junction was designed to enhance accuracy in restoring limb length and offset. However, this modularity has come at the expense of potential corrosion of these interfaces.1 A 2015 systematic review suggests that clinically significant corrosion can occur in the intermediate follow-up period and presents with unexplained pain and loosening.2 In some instances, this has resulted in early catastrophic trunnion dissociation and failure.3–5
Corrosion at the femoral head-neck junction has been shown to be related to multiple design and patient factors including trunnion diameter, femoral stem offset, head size, head length, trunnion taper angular mismatch, stem material, femoral head material, BMI, gender and activity level.1,2,6-9 There have been reported trends of increased usage of larger diameter femoral heads which have been shown to improve the head neck ratio and overall stability of a total hip arthroplasty, but these have also been linked to greater trunnion corrosion.9–14 There have also been reported trends of increased usage of ceramic heads, which may be less susceptible to trunnion corrosion, but more expensive in some health-care environments.9,12,15-17
Several femoral stem designs have been implicated to have a particularly high prevalence of corrosion.18–20 Over the last fifteen years at our institution, about three quarters of our cementless total hip replacements have employed one of three femoral stem designs. The purpose of this study was to review these three most commonly used femoral stems matched with cobalt-chrome femoral heads to correlate any established risk factors with rates of revision, particularly corrosion.
Patient Population and Methods
Study Population
Patient consent was waived by the Western University and London Health Sciences Center ethics boards due to the retrospective nature of the study. All patient data were maintained in confidentiality and the research complied with the Declaration of Helsinki and the Tri-council Policy of Canada. All arthroplasty operations performed at our institution are captured in our institutional database. Patients are routinely followed at 6 weeks, 3 months, 1 year, and then every 2 years. Any revisions done at outside institutions would be rare, but would be captured in our routine patient follow-ups. Metal ion levels and advanced imaging are ordered in symptomatic patients, and this has been part of our institutional work up since the beginning of the study period.21
From our institutional database, we identified all patients over a 15-year period (March 2000 to September 2015) that underwent total hip arthroplasty with one of three femoral stems paired with cobalt-chrome femoral heads. These stems were selected for review because they comprised about three quarters of the cementless femoral stems we have used over the last 15 years. The stems included the Summit® (Depuy, Warsaw, Indiana), Synergy® (Smith and Nephew, Memphis, Tennessee) and Corail® (Depuy, Johnson and Johnson, Warsaw, Indiana) femoral components. All of the stems are made of titanium (Ti6Al4V alloy) with a 12/14 taper design. We included only metal (cobalt chromium) on highly cross-linked polyethylene articulations. We excluded any ceramic femoral heads, metal bearing surfaces, cemented stems, and patients with less than three years of clinical follow-up.
Statistical Analysis
We evaluated age, gender, body mass index (BMI), femoral head size, femoral head length, neck angle and offset as potential risk factors for all cause revision and revision excluding infection by univariate analysis. Neck angle and offset for each stem were obtained from manufacturer guides, with offset increasing with increasing stem size as well as stem type (standard or high offset). Neck angle was recorded in degrees and offset was recorded in millimeters. The Synergy® stem can be coupled with femoral head lengths of −3mm, 0 mm, +4 mm, +8 mm, +12 mm and +16 mm while Summit® and Corail® stems can be used with femoral head lengths of −2 mm, +1.5 mm, +5 mm, +8.5 mm, +12 mm and +15.5 mm. The minus head length is only available when using a 36 mm femoral head size. We categorized femoral head size as greater than or equal to 32 mm or less than 32 mm.
We performed a logistic regression analysis with odds ratios for each parameter for both all cause revision as well as with infection excluded. We used a p value of <0.05 as significant.
Results
A total of 2095 patients were included in this study. There were 1094 Synergy® stems, 208 Corail® stems and 793 Summit® femoral stems included (Table 1). There were 461 patients (22%) with 28 mm diameter femoral heads, 1286 patients (61%) with 32 mm diameter femoral heads and 344 patients (16%) with 36 mm diameter femoral heads. Four patients had femoral head sizes less than 28 mm or greater than 36 mm (1%). The mean follow-up time was 8.58 years (3–17.45). We did not identify any cases of corrosion requiring revision total hip arthroplasty identified across the three implants (Table 2).
 |
Table 1 Baseline Patient Characteristics |
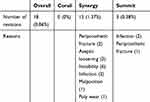 |
Table 2 Revision Characteristics |
Univariate logistic regression analysis demonstrated that head size was associated with increased risk of both all cause revision and revision excluding infection. Age, BMI, Gender, offset and neck angle did not have significant association to all cause revision or to revisions excluding infection (p>0.05). Multivariate logistic regression controlling for age and BMI demonstrated that a femoral head size less than 32mm was associated with increased likelihood of all cause revision (OR 4.60 (95% CI 1.8, 11.8)) and revision excluding infection (OR 4.94 (95% CI 1.7, 14.41)).
Discussion
Cooper et al (2012) were the first authors to describe corrosion at the head-neck taper occurring in patients with a contemporary metal-on-polyethylene bearing.22 However, these authors acknowledged that this occurred relatively rarely, accounting for only 1.8% of hip revisions performed at their institution. McGrory et al (2015) described a prevalence of 1.1% at an average time of presentation of 3.7 years with a contemporary non-cemented femoral hip component.19 His group subsequently reported an incidence of symptomatic corrosion in 43 of 1352 (3.2%) consecutive patients using a noncemented M/L taper® (Zimmer, Warsaw, IN) stem.20 These authors suggested the use of non-cobalt-chrome femoral heads until this high failure rate from corrosion was better understood. Since that time, there has been a dramatic rise in the use of ceramic on polyethylene bearings in the United States, with ceramic on polyethylene bearings now surpassing metal on polyethylene bearings as the most popular bearing surface.17
Similarly, Lash et al showed a 3% revision rate due to taper problems and secondary pseudotumour formation between 2006 and 2013.23 All ten reported cases occurred with the Accolade® (Stryker, Mahwah, New Jersey) or M/L® taper stems (Zimmer Inc. Warsaw, IN). Ko et al (2016) also reported catastrophic femoral head-stem trunnion dissociation secondary to corrosion with the Accolade® stem.3 We reported a similar cases series of catastrophic femoral head trunnion dissociation in cases referred to our institution with the same stem design.5 It has been postulated that this failure mode is due to mechanically assisted crevice corrosion (MACC).24,25 This may be related to the composition of the stem, which is a beta titanium alloy with a lower modulus of elasticity compared to standard titanium alloy.7 This material property results in bending of the trunnion with physiologic load5 and changing of the geometry of the taper causing significant micromotion, wear and eventual fracture.3,5
A substantial amount of research has been done in the area of trunnion corrosion, attempting to better understand its incidence and causative factors.1,9 Multiple risk factors for tribocorrosion have been identified including biomechanical factors such as increased femoral head length and femoral head size.7,11,26 The purpose of the present study was to review our 15 year experience with three femoral stems (combined with CoCr femoral heads) to identify whether we observed a similar incidence of corrosion leading to revision with a metal on polyethylene bearing as other authors have reported and to correlate any established risk factors with these rates of revision.
In the present study, we were unable to find a single case of trunnion corrosion requiring revision hip arthroplasty. We did find that smaller femoral head sizes (under 32mm) were associated with a greater likelihood of revision total hip arthroplasty excluding infection. Although there is some evidence that increased femoral head diameter may be a risk factor for corrosion, we were unable to identify any cases of corrosion requiring revision with larger femoral heads.26–28 The relation between tribocorrosion and adverse soft tissue reactions is not fully clear. Fillingham et al (2017) and Kwon et al (2011) have both shown that elevated serum Co levels have been shown to correlate with symptomatic and asymptomatic ALTR.29,30 In a random collection of 94 retrieved large diameter metal on polyethylene hips Hothi et al (2017) demonstrated corrosion without evidence of ALTR.27 Although 55% of hips had evidence of corrosion, there were no cases of adverse local tissue reactions and none were a cause for revision. The degree of corrosion leading to a symptomatic levels of Co remains unknown. Multiple studies suggest that factors such as trunnion geometry and flexural rigidity may be more influential in terms of incidence of corrosion.5,24,28,31 In a study of 92 retrieved femoral heads from primary metal on polyethylene total hips, larger femoral heads were actually correlated to less severe fretting and corrosion as compared to 28 mm femoral heads.28
The major strength of the current study is that it is a large patient cohort comparing three commonly used femoral stems over a 15-year period. We found that taper corrosion resulting in an adverse local tissue reaction and requiring revision surgery did not occur with the three most commonly used uncemented femoral stems at our institution. The obvious limitation to this study relates to the lack of corrosion cases identified. We presume that this is because of the strong taper design of these three stems. We do acknowledge that it is possible that we failed to identify patients with low levels of corrosion who remained largely asymptomatic. Another limitation is that we did not measure hip offset radiographically, but rather this was calculated based on the manufacturer’s dimensions of the individual prostheses. We recognize that other factors, namely the medialization of the acetabular component, can affect offset independent of the individual stem dimensions. We do follow all of our total hip arthroplasty patients every two to three years at our institution, and we routinely work-up any symptomatic patients up with serum metal ion levels and/or three-dimensional imaging. It was beyond the scope of this study, however, to report on the metal levels or advanced imaging on all patients in this cohort, although this may form the basis of future work in this area.
In some studies, ceramic heads have been reported to be less susceptible to trunnion corrosion, which has prompted some surgeons to routinely use ceramic heads in clinical practice to reduce the risk of trunnionosis.9,14,32 However, other studies have shown no difference in all-cause revision between ceramic and metal (CoCr) heads when used in combination with a highly cross-linked liner.33 While theoretical models comparing cost of metal toxicity work-up in the US health care system may justify a switch to ceramic heads, this has remained theoretical.34 Because there can be a significant cost differential with ceramic (compared to metal) heads, a wholesale switch to ceramic femoral heads to decrease the risk of corrosion may not be justified as this may result in an economic burden to socialized health-care systems.
Conclusion
In summary, over the last fifteen years, we have not identified any cases of corrosion with the three most commonly used femoral stems used at out institution. While we acknowledge that no femoral stem is immune to corrosion, we postulate that certain femoral stem designs are uniquely resistant (or susceptible) to this mode of failure. Furthermore, the universal use of ceramic heads on every femoral stem design to decrease the risk of corrosion may not be completely justified, particularly when these bearing surfaces come at an increased cost.
Disclosure
There was no funding obtained for this study. This paper has been presented at The Hip Society 2019 Summer meeting with interim findings. Poster’s abstract was published in Orthopaedic proceedings: https://online.boneandjoint.org.uk/doi/abs/10.1302/1358-992X.2019.12.009. Douglas D R Naudie reports personal fees, royalties, and institutional support from Smith and Nephew, and institutional support from Depuy and Stryker, outside the submitted work. Lyndsay E Somerville reports institutional support from Smith and Nephew, Depuy, Zimmer, and Stryker, outside the submitted work. James L Howard reports personal fees, non-financial support and institutional research support from Stryker, grants and institutional research support from DePuy, institutional research support from Smith and Nephew and Zimmer, and personal fees from Intellijoint, outside the submitted work. Richard W McCalden report consultancy for Smith & Nephew, outside the submitted work; and institutional research support from Stryker, Smith & Nephew and J&J Depuy. Steven J MacDonald reports personal fees from Depuy, a Johnson & Johnson Company, stock or stock options from Hip Innovations Technology, JointVue, Curvafix, and Parvizi Surgical Innovation, and research support from Smith & Nephew and Stryker, outside the submitted work. Brent A Lanting reports grants, personal fees, and institutional support from Smith and Nephew, DePuy, and Stryker, and institutional support from Zimmer, outside the submitted work. The authors report no other potential conflicts of interest for this work.
References
1. Lanting B, Naudie DDR, McCalden RW. Clinical impact of trunnion wear after total hip arthroplasty. JBJS Rev. 2016;4:8. doi:10.2106/JBJS.RVW.15.00096
2. Carli A, Politis A, Zukor D, Huk O, Antoniou J. Clinically significant corrosion at the head-neck taper interface in total hip arthroplasty: a systematic review and case series. Hip Int. 2015;25(1):7–14. doi:10.5301/hipint.5000180
3. Ko LM, Chen AF, Deirmengian GK, Hozack WJ, Sharkey PF. Catastrophic femoral head-stem trunnion dissociation secondary to corrosion. JBJS. 2016;98(16):1400–1404. doi:10.2106/JBJS.15.00914
4. Banerjee S, Cherian JJ, J V B, et al. Gross trunnion failure after primary total hip arthroplasty. J Arthroplasty. 2015;30(4):641–648. doi:10.1016/j.arth.2014.11.023
5. Wood TJ, Alzahrani M, Langohr D, et al. Catastrophic femoral head trunnion dissociation: a case series with surface wear analysis. Hip Int. 2019;29(5):NP1–5. doi:10.1177/1120700019860774
6. Plummer DR, Berger RA, Paprosky WG, Sporer SM, Jacobs JJ, Della Valle CJ. Diagnosis and management of adverse local tissue reactions secondary to corrosion at the head-neck junction in patients with metal on polyethylene bearings. J Arthroplasty. 2016;31(1):264–268. doi:10.1016/j.arth.2015.07.039
7. Jennings JM, Dennis DA, Yang CC. Corrosion of the head-neck junction after total hip arthroplasty. J Am Acad Orthop Surg. 2016;24(6):349–356. doi:10.5435/JAAOS-D-15-00111
8. Tan SC, Teeter MG, Del Balso C, Howard JL, Lanting BA. Effect of taper design on trunnionosis in metal on polyethylene total hip arthroplasty. J Arthroplasty. 2015;30(7):1269–1272. doi:10.1016/j.arth.2015.02.031
9. Weiser MC, Lavernia CJ. Trunnionosis in total hip arthroplasty. JBJS. 2017;99(17):1489–1501. doi:10.2106/JBJS.17.00345
10. Howie DW, Holubowycz OT, Middleton R, Group LAS. Large femoral heads decrease the incidence of dislocation after total hip arthroplasty: a randomized controlled trial. JBJS. 2012;94(12):1095–1102. doi:10.2106/JBJS.K.00570
11. Del Balso C, Teeter MG, Tan SC, Howard JL, Lanting BA. Trunnionosis: does head size affect fretting and corrosion in total hip arthroplasty? J Arthroplasty. 2016;31(10):2332–2336. doi:10.1016/j.arth.2016.03.009
12. Lehil MS, Bozic KJ. Trends in total hip arthroplasty implant utilization in the United States. J Arthroplasty. 2014;29(10):1915–1918. doi:10.1016/j.arth.2014.05.017
13. Dyrkacz RMR, Brandt J-M, Ojo OA, Turgeon TR, Wyss UP. The influence of head size on corrosion and fretting behaviour at the head-neck interface of artificial hip joints. J Arthroplasty. 2013;28(6):1036–1040. doi:10.1016/j.arth.2012.10.017
14. Lavernia CJ, Iacobelli DA, Villa JM, Jones K, Gonzalez JL, Jones WK. Trunnion–head stresses in tha: are big heads trouble? J Arthroplasty. 2015;30(6):1085–1088. doi:10.1016/j.arth.2015.01.021
15. Kurtz SM, Kocagöz SB, Hanzlik JA, et al. Do ceramic femoral heads reduce taper fretting corrosion in hip arthroplasty? A retrieval study. Clin Orthop Relat Res. 2013;471(10):3270–3282. doi:10.1007/s11999-013-3096-2
16. Carnes KJ, Odum SM, Troyer JL, Fehring TK. Cost analysis of ceramic heads in primary total hip arthroplasty. JBJS. 2016;98(21):1794–1800. doi:10.2106/JBJS.15.00831
17. Heckmann ND, Sivasundaram L, Stefl MD, Kang HP, Basler ET, Lieberman JR. Total hip arthroplasty bearing surface trends in the United States from 2007 to 2014: the rise of ceramic on polyethylene. J Arthroplasty. 2018;33(6):1757–1763. doi:10.1016/j.arth.2017.12.040
18. Martin AJ, Jenkins DR, Van Citters DW. Role of corrosion in taper failure and head disassociation in total hip arthroplasty of a single design. J Orthop Res. 2018;36(11):2996–3003. doi:10.1002/jor.24107
19. McGrory BJ, MacKenzie J, Babikian G. A high prevalence of corrosion at the head–neck taper with contemporary Zimmer non-cemented femoral hip components. J Arthroplasty. 2015;30(7):1265–1268. doi:10.1016/j.arth.2015.02.019
20. Hussey DK, McGrory BJ. Ten-year cross-sectional study of mechanically assisted crevice corrosion in 1352 consecutive patients with metal-on-polyethylene total hip arthroplasty. J Arthroplasty. 2017;32(8):2546–2551. doi:10.1016/j.arth.2017.03.020
21. MacDonald S, McCalden RW, Chess DG, et al. Metal-on-metal versus polyethylene in hip arthroplasty: a randomized clinical trial. Clin Orthop Relat Res. 2003;406(1):282–296. doi:10.1097/00003086-200301000-00039
22. Cooper HJ, Della Valle CJ, Berger RA, et al. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012;94(18):1655. doi:10.2106/JBJS.K.01352
23. Lash NJ, Whitehouse MR, N V G, Garbuz DS, Masri BA, Duncan CP. Delayed dislocation following metal-on-polyethylene arthroplasty of the hip due to ‘silent’trunnion corrosion. Bone Joint J. 2016;98(2):187–193. doi:10.1302/0301-620X.98B2.36593
24. Urish KL, Hamlin BR, Plakseychuk AY, et al. Trunnion failure of the recalled low friction ion treatment cobalt chromium alloy femoral head. J Arthroplasty. 2017;32(9):2857–2863. doi:10.1016/j.arth.2017.03.075
25. Morlock MM, Dickinson EC, Günther K-P, Bünte D, Polster V. Head taper corrosion causing head bottoming out and consecutive gross stem taper failure in total hip arthroplasty. J Arthroplasty. 2018;33(11):3581–3590. doi:10.1016/j.arth.2018.07.017
26. Triantafyllopoulos GK, Elpers ME, Burket JC, Esposito CI, Padgett DE, Wright TM. Otto Aufranc Award: large heads do not increase damage at the head-neck taper of metal-on-polyethylene total hip arthroplasties. Clin Orthop Relat Res. 2016;474(2):330–338. doi:10.1007/s11999-015-4468-6
27. Hothi HS, Kendoff D, Lausmann C, et al. Clinically insignificant trunnionosis in large-diameter metal-on-polyethylene total hip arthroplasty. Bone Joint Res. 2017;6(1):52–56. doi:10.1302/2046-3758.61.BJR-2016-0150.R2
28. Siljander MP, Baker EA, Baker KC, Salisbury MR, Thor CC, Verner JJ. Fretting and corrosion damage in retrieved metal-on-polyethylene modular total hip arthroplasty systems: what is the importance of femoral head size? J Arthroplasty. 2018;33(3):931–938. doi:10.1016/j.arth.2017.10.010
29. Fillingham YA, Della Valle CJ, Bohl DD, et al. Serum metal levels for diagnosis of adverse local tissue reactions secondary to corrosion in metal-on-polyethylene total hip arthroplasty. J Arthroplasty. 2017;32(9):S272–7. doi:10.1016/j.arth.2017.04.016
30. Kwon Y-M, Ostlere SJ, McLardy-Smith P, Athanasou NA, Gill HS, Murray DW. “Asymptomatic” pseudotumors after metal-on-metal hip resurfacing arthroplasty: prevalence and metal ion study. J Arthroplasty. 2011;26(4):511–518. doi:10.1016/j.arth.2010.05.030
31. Martin JR, Camp CL, Wyles CC, Taunton MJ, Trousdale RT, Lewallen DG. Increased femoral head offset is associated with elevated metal Ions in asymptomatic patients with metal-on-polyethylene total hip arthroplasty. J Arthroplasty. 2016;31(12):2814–2818. doi:10.1016/j.arth.2016.05.047
32. McPherson E, Dipane M, Sherif S. Massive pseudotumor in a 28mm ceramic-polyethylene revision THA: a case report. Reconstr Rev. 2014;4:1.
33. Cafri G, Paxton EW, Love R, Bini SA, Kurtz SM. Is there a difference in revision risk between metal and ceramic heads on highly crosslinked polyethylene liners? Clin Orthop Relat Res. 2017;475(5):1349–1355. doi:10.1007/s11999-016-4966-1
34. Wyles CC, McArthur BA, Wagner ER, Houdek MT, Jimenez-Almonte JH, Trousdale RT Ceramic femoral heads for all patients? An argument for cost containment in hip surgery. Am J Orthop. 2016; 45(6): E362–E366
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
