Back to Journals » Infection and Drug Resistance » Volume 16
Thirty-Day Outcomes of Young and Middle-Aged Adults Admitted with Severe COVID-19 in Uganda: A Retrospective Cohort Study
Authors Kyagambiddwa T , Kintu TM , Miiro E , Nabalamba F, Asiimwe GS, Namutebi AM, Abeya FC, Lumori BA, Ijuka I, Muhindo RK, Mutekanga A , Musinguzi R , Natuhwera F, Ngonzi J, Nuwagira E
Received 18 January 2023
Accepted for publication 28 April 2023
Published 11 May 2023 Volume 2023:16 Pages 2923—2932
DOI https://doi.org/10.2147/IDR.S405256
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Tonny Kyagambiddwa,1,* Timothy Mwanje Kintu,1,* Emmanuel Miiro,1,* Franchesca Nabalamba,1 Gloria Suubi Asiimwe,1 Anne Marion Namutebi,2 Fardous C Abeya,3 Boniface A Lumori,3 Isaac Ijuka,4 Rose K Muhindo,1,3 Andrew Mutekanga,1,3 Richard Musinguzi,5 Francis Natuhwera,6 Joseph Ngonzi,1,7 Edwin Nuwagira3,8
1Faculty of Medicine, Mbarara University of Science and Technology, Mbarara, Uganda; 2Kabale Regional Referral Hospital, Kabale, Uganda; 3Department of Medicine, Mbarara University of Science and Technology, Mbarara, Uganda; 4Mayanja Memorial Hospital, Mbarara, Uganda; 5Masaka Regional Referral Hospital, Masaka, Uganda; 6Fort Portal Regional Referral Hospital, Fort Portal, Uganda; 7Department of Obstetrics and Gynecology, Mbarara University of Science and Technology, Mbarara, Uganda; 8Tuberculosis Treatment Unit, Mbarara Regional Referral Hospital, Mbarara, Uganda
*These authors contributed equally to this work
Correspondence: Tonny Kyagambiddwa; Edwin Nuwagira, Mbarara University of Science and Technology, Tel +256782980116 ; +256779096887, Email [email protected]; [email protected]
Background: There is scarcity of data regarding young and middle-aged adults hospitalized with severe Corona Virus Disease 2019 (COVID-19) in Africa. In this study, we describe the clinical characteristics and 30-day survival among adults aged 18 to 49 years admitted with severe COVID-19 in Uganda.
Methods: We reviewed treatment records of patients admitted with severe COVID-19 across five COVID-19 treatment units (CTU) in Uganda. We included individuals aged 18 to 49 years, who had a positive test or met the clinical criteria for COVID-19. We defined severe COVID-19 as having an oxygen saturation < 94%, lung infiltrates > 50% on imaging and presence of a co-morbidity that required admission in the CTU. Our main outcome was the 30-day survival from the time of admission. We used a Cox proportional hazards model to determine the factors associated with 30-day survival at a 5% level of significance.
Results: Of the 246 patient files reviewed, 50.8% (n = 125) were male, the mean ± (standard deviation) age was 39 ± 8 years, majority presented with cough, 85.8% (n = 211) and median C-reactive protein (interquartile range) was 48 (47.5, 178.8) mg/L. The 30-day mortality was 23.9% (59/246). At admission, anemia (hazard ratio (HR): 3.00, 95% confidence interval (CI), 1.32– 6.82; p = 0.009) and altered mental state (GCS < 15) (HR: 6.89, 95% CI: 1.48– 32.08, p = 0.014) were significant predictors of 30-day mortality.
Conclusion: There was a high 30-day mortality among young and middle-aged adults with severe COVID-19 in Uganda. Early recognition and targeted management of anemia and altered consciousness are needed to improve clinical outcomes.
Keywords: COVID-19, Uganda, mortality, young and middle-aged adults
Introduction
Severe Acute Respiratory Syndrome Corona virus 2 (SARS-CoV-2) was the leading cause of mortality from an infectious cause globally in 2021.1 To date, over 591 million people worldwide have been infected, and the number of deaths had reached almost 6.44 million by August 15, 2022 (WHO).2 Despite the limited understanding and heterogeneity of the COVID-19 pandemic in sub-Saharan Africa (SSA), reports still show a low pandemic’s toll in Africa, yet it is home to approximately 17% of the world’s population.3 This has been attributed to several reasons which include inconsistent case definitions,4 limited case surveillance5 and possibility of pre-existing immunity to SARS-CoV-2.6 However, in-hospital mortality has been noted to be comparatively high in Africa.7 The risk factors attributable to outcomes of severe disease vary across different populations in Africa8,9 and are similar to data reported by the RECOVERY study group.10 But, the SSA is also home to the world’s youngest population11 which limits the generalizability of data from other parts of the world. There is still limited knowledge in regards to characteristics of severe COVID-19 in young and middle-aged people in Africa. Increased age and presence of co-morbidities have been consistently reported as an important risk factor associated with severe disease and death.12–15
In Uganda, studies done to assess in-hospital outcomes were either single center, conducted with a small sample size of patients with mild disease or involved patients of all age groups.16–19 Among young and middle-aged patients, COVID-19 is thought to cause lower mortality rates, yet, the disease may have significant severity, cause critical infection and differ in some respects from the disease in the elderly.20,21 For example, obesity and under-weight have been noted as important risk factors for poor outcomes in young patients with COVID 19,22–25 and also linked to increased risk of complications such as acute kidney injury and acute respiratory distress syndrome in these patients.26 Other studies have reported hypertension, diabetes,25 asthma,27 hypoxemia, baseline heart disease and laboratory parameters such as lymphopenia to be associated with poor outcome in middle aged adults.21 The studies aforementioned were done in developed countries and we found no specific study previously done in sub-Saharan Africa focusing on the young and middle-aged population. However, Mwananyanda et al in a postmortem surveillance study done in Zambia reported up to 66% (46/70) of deaths were adults aged 20–59 years and mostly occurred in the community.28
Data regarding factors associated with clinical outcomes in young and middle-aged people hospitalized with severe COVID-19 is scarce. Moreover, this particular age-group has been noted to be a major driver of the pandemic in the African region.29 In order to guide development of locally relevant triaging and management protocols for future viral outbreaks, there is need to establish evidence based on clinical characteristics and short-term outcomes observed, especially in younger patient populations. This is especially important in sub-Saharan Africa where COVID-19 interventions such as vaccination programs have been less prioritized. In this study, we sought to describe clinical characteristics, in-hospital outcomes of severe COVID-19 and associated factors among patients between 18 and 49 years admitted at major treatment centers in Uganda.
Materials and Methods
Study Population and Study Setting
We reviewed medical records of patients admitted between March 2020 and August 2022 at five Ministry of Health approved CTUs in Uganda. The CTUs were at Mbarara, Fort Portal, Kabale and Masaka Regional Referral Hospitals which have bed capacities of 600, 333, 280 and 330, respectively. The fifth CTU was at Mayanja Memorial Hospital which is an urban private not-for-profit health facility with a quoted bed capacity of 100, serving patients in South Western Uganda. Our inclusion criteria were: adults aged 18 to 49 years, with a microbiologically confirmed COVID-19 by Polymerase Chain Reaction (PCR) or serological tests (Abbott Panbio® COVID-19 Antigen Rapid Tests) or clinical diagnosis of COVID-19 using a high-resolution CT scan and severe forms of COVID-19. Severe COVID was defined by; a). peripheral oxygen saturation < 90% at room air, comorbidity requiring admission in the CTU, lung imaging showing >50% lung involvement or respiratory rate >30 cycles per minute. We corrected data from all files that met the inclusion criteria. We excluded participants whose medical records/charts were missing, records available but had less than 50% of the required variables and those whose 30-day outcomes were not recorded.
Data Collection Procedure
We used an electronic data capture (EDC) tool to extract the required data from hospital patient records. We collected socio-demographic data (age, gender, weight, BMI, history of alcohol or smoking) and the date of admission. The clinical data included the patient’s presenting complaints (cough, sore throat, shortness of breath, wheezing, chest pain, headache, anorexia, and many others); any use of pre-hospital medications (such as antibiotics, antivirals); vital signs at admission (heart rate, blood pressure, oxygen saturation, temperature); presence of any comorbidities (Diabetes Mellitus, Hypertension, HIV/AIDS, TB, chronic respiratory disease (asthma, COPD), chronic kidney disease); patient’s laboratory results at admission (sodium, potassium, C-reactive protein, complete blood count, d-dimers, C-reactive protein, AST, ALT, urea); any oxygen therapy received (invasive or non-invasive); ICU admission; any complications during hospital stay (hyperglycemia, hypoglycemia, anemia, coagulation, seizures, stroke); duration of hospital stay and medication received in hospital. For every patient admitted to Ugandan CTUs, discharge status and 30-day outcomes were recorded. We recorded the dates of discharge and the 30-day survival status, which ever came first.
Data Analysis
From the EDC, data was initially exported into Microsoft Excel 2016 (Microsoft Corporation) for cleaning. To describe the overall baseline characteristics, categorical variables were summarized as frequencies and proportions whereas numerical data was summarized as means and standard deviations or median and corresponding interquartile ranges. Presenting symptoms were grouped per system, for example cough, hemoptysis and difficulty in breathing were presented as respiratory symptoms. Since we had a binary primary outcome, we compared the means and medians across deaths and alive at 30-days using the Kruskal–Wallis or Chi-square tests as appropriate stratified the baseline variables into two categories.
We used a Cox proportional hazards model to determine univariate and multivariate hazard ratios for explanatory variables with the associated 95% confidence interval. Outcomes were censored at 30 days and variables with statistically significant p-values in the univariate model were selected for the multivariate analysis. In the final multivariate model, only statistically significant variables were kept. Variables with more than 80% of their values missing were also not considered for multivariable analysis. To deal with multicollinearity, only admission oxygen saturation (as opposed to shortness of breath) was included in the regression model. In this study, a p-value less than 0.05 was considered statistically significant. All statistical inferential frameworks were based on the two-sided p-value and a 5% error margin. Missing values were considered informative. All statistical analysis was done in the statistical software R version 4.1.1.30
Results
Baseline Characteristics
Between May 2020 and August 2022, a total of 246 patients were enrolled in the study as shown in Figure 1. The mean age ± SD of the patients enrolled was 39 ± 8 years, there were slightly more men than women (125 vs 121) and 94.7% (n = 233) of the patients presented with respiratory symptoms. Admission to the CTU and the trends of admissions and deaths due to COVID-19 were unevenly distributed across the study period. Mortality was highest between June and August, 2021 as shown in Figure 2. The overall 30-day mortality was 24% (59/246) as shown in Table 1. Details of the admission symptoms, medication received and duration of hospitalization have been summarized in the (Supplementary Section Tables S1–S5). The most common admission complications in our cohort were hyperglycemia (14.2%), acute respiratory distress syndrome (ARDS) and anemia (7.7%). Majority of the patients died in the first two weeks of admission, and none after the 20th admission date as shown in Figure 3. We noted that admission oxygen saturation (aHR: 0.97, CI: 0.95–0.99, p = 0.002), anemia (aHR: 3.00, CI: 1.32–6.82, p = 0.009) and altered level of consciousness (aHR: 6.89, CI: 1.48–32.08, p = 0.014) were significant risk factors of 30-day mortality (Table 2 and Figure 4).
 |
Table 1 Demographic and Clinical Characteristics and Their Associations with Mortality |
 |
Table 2 Risk Factors Associated with 30-Day Mortality |
 |
Figure 1 Flow diagram showing number of patients enrolled in the study. |
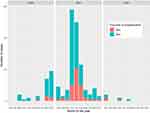 |
Figure 2 Trends in cases of severe COVID-19 in patients aged 18 to less than 50 years in South-western Uganda between May, 2020 to August 2022. |
 |
Figure 3 Kaplan Meier curve showing overall 30-day survival. |
 |
Figure 4 Hazard Ratio plot showing adjusted hazards ratios of 30-day mortality for peripheral oxygen saturation, anemia, GCS<15, Vitamin C treatment, coagulation disorder and chronic liver disease. |
Discussion
In this study, our main objective was to describe the clinical characteristics, in-hospital outcomes and factors associated with poor outcomes among patients less than 50 years admitted with severe COVID-19 in Uganda. We found that admission and mortality rates were highest between May and September 2021 and the overall 30-day mortality was 24%. Predictors of 30-day in-hospital mortality in patients admitted included altered level of consciousness and anemia at admission.
The first wave of the COVID-19 pandemic in Uganda was between March and August 2020 and had a handful number of severe cases and deaths.31 Most of the identified cases had mild or moderate disease.16,32 In our study, the highest number of deaths was recorded between June and August 2021, the same period when the second wave of COVID-19 was at its peak dominated by the delta variant.33 During this time, the health system in Uganda was overwhelmed by COVID-19 cases leading to shortage of human resource and medical services.34,35 The increase in mortality was not unique to Uganda, but also other parts of the world with significant deaths among young adults without comorbidities.36
We found an in-hospital mortality of 24% which was lower than 37% that was found in a study done at a national referral hospital and 28% found at a private facility in Uganda.17,19 The difference in mortality could be explained by the inclusion of older patients who were previously described to be at higher risk of mortality.37 Other studies from Africa reported an in-hospital mortality of less than 20%38,39 However, none of the these focused on young and middle-aged patients in an African setting.
In our study, anemia and altered mental state at admission were independent predictors of mortality. These findings are consistent with a meta-analysis that reported a 70% higher risk of short-term mortality in patients with anemia.40 Anemia in severe COVID-19 could be due to a hyperinflammatory state involving over-production of interleukin(IL)-641,42 that causes abnormal iron metabolism. Elevation of other pro-inflammatory cytokines such as; IL-1, IL-33 and tumor necrosis factor-α is associated with inhibitory effects on erythroid progenitor and precursor cells.43 Frequently, anemia worsens severe respiratory disease and the combination has been documented to be associated with poor outcomes and death.44 Other studies have listed anemia to be an important parameter playing a major role in severity and covid 19 mortality45 even in its mild form.46 In circumstances of respiratory compromise and increased oxygen demand in a hypermetabolic state like COVID-19, anemia can further reduce oxygen delivery to peripheral tissues.45,47 Similar to our findings, Xuong et al reported that COVID-19 deaths were mainly associated with lower GCS scores.48 A study done in the United States also found coma to be an independent predictor of death.49 Reduced levels of consciousness can be partly attributed to metabolic encephalopathy,50 seizures or demyelinating disease.51
Our study was limited by a lack of a standardized measure of altered level of consciousness across the different health facilities which may affect the reliability of this finding. The retrospective nature of the study limited the availability of study variables like respiratory rate, Body Mass Index and laboratory results. Also, there was lack of consistency in the diagnosis of severe COVID-19 by clinicians across the different participating health facilities. However, the study included data from four public regional referral COVID-19 treatment units and a single private hospital in western Uganda which makes the results generalizable.
Conclusion and Recommendations
This study highlights the significant risk of mortality due severe COVID-19 in young and middle-aged patients, hence the need for targeted interventions to improve clinical outcomes. The study identified altered level of consciousness and anemia at admission as independent predictors of mortality, underscoring the importance of early recognition and management of these factors. However, further research is needed to understand the mechanisms underlying anemia in severe COVID-19 and to identify effective interventions to reduce mortality in this vulnerable population. These findings could inform the development of triage mechanisms and clinical management protocols in low resource settings, and vaccination campaigns particularly in Africa where the COVID-19 pandemic has had a significant impact.
Abbreviations
COVID –19, Corina Virus Disease 2019; SARS-CoV-2, severe acute respiratory syndrome corona virus 2; SSA, sub-Saharan Africa; WHO, World Health Organization; PCR, Polymerase Chain Reaction; CT, Computed Tomography; TB, Tuberculosis; CTU, COVID-19 treatment units; GCS, Glasgow Coma Scale; EDC, Electronic Data Capture; BMI, Body Mass Index; COPD, Chronic Obstructive Pulmonary Disease; AST, Aspartate aminotransferase; ALT, Alanine aminotransferase; ICU, Intensive Care Unit; SD, Standard Deviation; aHR, adjusted Hazards Ratio; CI, Confidence Interval; ARDS, Acute Respiratory Distress Syndrome.
Data Sharing Statement
The datasets used during this study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The study was approved by the Research Ethics Committee of Mbarara University of Science and Technology under reference number MUST-2022-435. The ethics committee waived the requirement for consent. Permission for access to medical records was granted by the necessary boards at respective hospitals. Study codes were used to ensure the anonymity of participants’ data. Data generated from the study shall be used for research purposes only and shall be private and confidential at all times. All principles of data transfer and principles of protection of human research participants outlined in the Declaration of Helsinki were observed.
Acknowledgments
The authors acknowledge hospital directors; Dr. Celestino Barigye, Dr. Nathan Onyachi, Dr. Anne Marion Namutebi, Dr. Alex Adaku and Mr. Isaac Ijuka for granting approval to collect data from respective health facilities. We also acknowledge Ms. Charity Kakuru, Ms. Fausita Nakibuule, Mr. Jackline Tukwasibwe for participating in data collection.
Funding
This study was funded by the Mbarara University Faculty of Medicine Seed grant. Edwin Nuwagira is also supported by the American Thoracic Society (Diversity grant 2022) and the NIH’s Fogarty international Centre (D43TW011632).
Disclosure
The authors declare that they have no competing interests.
References
1. World Health Organization. Global Tuberculosis Report 2022. World Health Organization; 2022. Available from: https://apps.who.int/iris/handle/10665/363752.
2. World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available from: https://covid19.who.int.
3. Worldometer. Population of Africa (2022). Available from: https://www.worldometers.info/world-population/africa-population/.
4. World Health Organization. The future of WHO Covid-19 response operations in Africa in 2022. World Health Organization | Regional Office for Africa. Available from: https://www.afro.who.int/publications/future-who-covid-19-response-operations-africa-2022.
5. Adebisi YA, Rabe A, Lucero-Prisno III DE. COVID-19 surveillance systems in 13 African countries. Health Promot Perspect. 2021;11(4):382–392. doi:10.34172/hpp.2021.49
6. Snyman J, Sanders EJ, Ndung’u T. COVID-19 in Africa: preexisting immunity and HIV. AIDS. 2021;35(14):2391–2393. doi:10.1097/QAD.0000000000003079
7. African COVID-19 Critical Care Outcomes Study (ACCCOS) Investigators. Patient care and clinical outcomes for patients with COVID-19 infection admitted to African high-care or intensive care units (ACCCOS): a multicentre, prospective, observational cohort study. Lancet Lond Engl. 2021;397(10288):1885–1894. doi:10.1016/S0140-6736(21)00441-4
8. Salyer SJ, Maeda J, Sembuche S, et al. The first and second waves of the COVID-19 pandemic in Africa: a cross-sectional study. Lancet. 2021;397(10281):1265–1275. doi:10.1016/S0140-6736(21)00632-2
9. Anjorin AA, Abioye AI, Asowata OE, et al. Comorbidities and the COVID-19 pandemic dynamics in Africa. Trop Med Int Health TM IH. 2021;26(1):2–13. doi:10.1111/tmi.13504
10. Perazzo H, Cardoso SW, Ribeiro MPD, et al. In-hospital mortality and severe outcomes after hospital discharge due to COVID-19: a prospective multicenter study from Brazil. Lancet Reg Health Am. 2022;11:100244. doi:10.1016/j.lana.2022.100244
11. Young People’s Potential, the Key to Africa’s Sustainable Development. Office of the high representative for the least developed Countries, landlocked developing Countries and Small Island Developing States. Available from: https://www.un.org/ohrlls/news/young-people%E2%80%99s-potential-key-africa%E2%80%99s-sustainable-development.
12. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1239–1242. doi:10.1001/jama.2020.2648
13. Zhang H, Wu Y, He Y, et al. Age-related risk factors and complications of patients with COVID-19: a population-based retrospective study. Front Med. 2022;8. doi:10.3389/fmed.2021.757459
14. Statsenko Y, Al Zahmi F, Habuza T, et al. Impact of age and sex on COVID-19 severity assessed from radiologic and clinical findings. Front Cell Infect Microbiol. 2022;11. doi:10.3389/fcimb.2021.777070
15. Starke KR, Reissig D, Petereit-Haack G, Schmauder S, Nienhaus A, Seidler A. The isolated effect of age on the risk of COVID-19 severe outcomes: a systematic review with meta-analysis. BMJ Glob Health. 2021;6(12):e006434. doi:10.1136/bmjgh-2021-006434
16. Kirenga B, Muttamba W, Kayongo A, et al. Characteristics and outcomes of admitted patients infected with SARS-CoV-2 in Uganda. BMJ Open Respir Res. 2020;7(1):e000646. doi:10.1136/bmjresp-2020-000646
17. Apiyo M, Olum R, Kabuye A, et al. Clinical characteristics and outcomes of patients hospitalized with COVID-19 at case hospital, Uganda. Interdiscip Perspect Infect Dis. 2022;2022:e5477790. doi:10.1155/2022/5477790
18. Baguma S, Okot C, Alema NO, et al. Factors associated with mortality among the COVID-19 patients treated at Gulu Regional referral hospital: a retrospective study. Front Public Health. 2022;10. doi:10.3389/fpubh.2022.841906
19. Bongomin F, Fleischer B, Olum R, et al. High mortality during the second wave of the coronavirus disease 2019 (COVID-19) pandemic in Uganda: experience from a National Referral COVID-19 treatment unit. Open Forum Infect Dis. 2021;8:11. doi:10.1093/ofid/ofab530
20. Herrera-Esposito D, de Los Campos G. Age-specific rate of severe and critical SARS-CoV-2 infections estimated with multi-country seroprevalence studies. BMC Infect Dis. 2022;22(1):311. doi:10.1186/s12879-022-07262-0
21. Tabernero E, Ruiz LA, España PP, et al. COVID-19 in young and middle-aged adults: predictors of poor outcome and clinical differences. Infection. 2022;50(1):179–189. doi:10.1007/s15010-021-01684-9
22. In young adults with COVID-19, obesity is associated with adverse outcomes. Available from: https://pubmed.ncbi.nlm.nih.gov/32726235/.
23. Why COVID-19 is more deadly in people with obesity—even if they’re young. Available from: https://www.science.org/content/article/why-covid-19-more-deadly-people-obesity-even-if-theyre-young.
24. Apr 29 MVB| NW| CN|, 2021. Obesity studies highlight severe COVID outcomes, even in young adults. CIDRAP. Available from: https://www.cidrap.umn.edu/news-perspective/2021/04/obesity-studies-highlight-severe-covid-outcomes-even-young-adults.
25. Cunningham JW, Vaduganathan M, Claggett BL, et al. Clinical outcomes in young US adults hospitalized with COVID-19. JAMA Intern Med. 2021;181(3):379–381. doi:10.1001/jamainternmed.2020.5313
26. van Son J, Oussaada SM, Şekercan A, et al. Overweight and obesity are associated with acute kidney injury and acute respiratory distress syndrome, but not with increased mortality in hospitalized COVID-19 patients: a retrospective cohort study. Front Endocrinol. 2021;12. doi:10.3389/fendo.2021.747732
27. Sandoval M, Nguyen DT, Vahidy FS, Graviss EA. Risk factors for severity of COVID-19 in hospital patients age 18–29 years. PLoS One. 2021;16(7):e0255544. doi:10.1371/journal.pone.0255544
28. Mwananyanda L, Gill CJ, MacLeod W, et al. Covid-19 deaths in Africa: prospective systematic postmortem surveillance study. BMJ. 2021;372:n334. doi:10.1136/bmj.n334
29. News-Medical.net. Individuals under 65 years may be the predominant drivers of COVID-19 in West Africa; 2022. Available from: https://www.news-medical.net/news/20220706/Individuals-under-65-years-may-be-the-predominant-drivers-of-COVID-19-in-West-Africa.aspx.
30. R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria; 2021. Available from: https://www.r-project.org/.
31. Institute for Health Metrics and Evaluation. COVID-19 results briefing Uganda December 15 ; 2022. Available from: https://www.healthdata.org/sites/default/files/covid_briefs/190_briefing_Uganda.pdf.
32. Migisha R, Kwesiga B, Mirembe BB, et al. Early cases of SARS-CoV-2 infection in Uganda: epidemiology and lessons learned from risk-based testing approaches – march-April 2020. Glob Health. 2020;16(1):114. doi:10.1186/s12992-020-00643-7
33. World Health Organization. COVID-19 deaths in African region to fall by nearly 94% in 2022: WHO analysis. Regional Office for Africa. Available from: https://www.afro.who.int/news/covid-19-deaths-african-region-fall-nearly-94-2022-who-analysis.
34. English.news.cn. Uganda lacks medical oxygen as hospitals overwhelmed by COVID-19. Xinhua. Available from: http://www.xinhuanet.com/english/africa/2021-06/15/c_1310009112.htm.
35. Team M. Uganda: one ICU Bed for 188,000 Ugandans. The Monitor; 2021. Available from: https://allafrica.com/stories/202107130117.html.
36. Chinnaswamy S. Understanding the devastating second wave of
37. Dadras O, SeyedAlinaghi S, Karimi A, et al. COVID‐19 mortality and its predictors in the elderly: a systematic review. Health Sci Rep. 2022;5(3):e657. doi:10.1002/hsr2.657
38. Assal HH, Abdel-hamid HM, Magdy S, et al. Predictors of severity and mortality in COVID-19 patients. Egypt J Bronchol. 2022;16(1):1–9. doi:10.1186/s43168-022-00122-0
39. Predictors of mortality among hospitalized COVID-19 patients at a tertiary care hospital in Ethiopia. Available from: https://pubmed.ncbi.nlm.nih.gov/34938084/.
40. Prognostic role of anemia in COVID-19 patients: a meta-analysis. Available from: https://pubmed.ncbi.nlm.nih.gov/34842707/.
41. Chen LYC, Hoiland RL, Stukas S, Wellington CL, Sekhon MS. Confronting the controversy: interleukin-6 and the COVID-19 cytokine storm syndrome. Eur Respir J. 2020;56(4):2003006. doi:10.1183/13993003.03006-2020
42. Hu B, Huang S, Yin L. The cytokine storm and COVID-19. J Med Virol. 2021;93(1):250–256. doi:10.1002/jmv.26232
43. Bergamaschi G, Borrelli de Andreis F, Aronico N, et al. Anemia in patients with Covid-19: pathogenesis and clinical significance. Clin Exp Med. 2021;21(2):239–246. doi:10.1007/s10238-020-00679-4
44. Tao Z, Xu J, Chen W, et al. Anemia is associated with severe illness in COVID-19: a retrospective cohort study. J Med Virol. 2021;93(3):1478–1488. doi:10.1002/jmv.26444
45. Oh SM, Skendelas JP, Macdonald E, et al. On-admission anemia predicts mortality in COVID-19 patients: a single center, retrospective cohort study. Am J Emerg Med. 2021;48:140–147. doi:10.1016/j.ajem.2021.03.083
46. Mild anemia as a single independent predictor of mortality in patients with COVID‐19 – Tremblay. eJHaem - Wiley Online Library; 2021. Available from: https://onlinelibrary.wiley.com/doi/10.1002/jha2.167.
47. Jha M, Tak ML, Gupta R, et al. Relationship of anemia with COVID-19 deaths: a retrospective cross-sectional study. J Anaesthesiol Clin Pharmacol. 2022;38(Suppl1):S115–S119. doi:10.4103/joacp.joacp_63_22
48. Xiong W, Lu L, Zhang B, et al. Association of consciousness impairment and mortality in people with COVID-19. Acta Neurol Scand. 2021;144(3):251–259. doi:10.1111/ane.13471
49. SpringerLink. Disorders of consciousness in hospitalized patients with covid-19: the role of the systemic inflammatory response syndrome. Available from: https://link.springer.com/article/10.1007/s12028-021-01256-7.
50. SpringerLink. Altered mental status in COVID-19. Available from: https://link.springer.com/article/10.1007/s00415-021-10623-5.
51. Gupta R, Garg A, Sapra H, et al. Pathophysiological mechanisms and neurological manifestations in COVID-19. Indian J Crit Care Med. 2020;24(10):975–980. doi:10.5005/jp-journals-10071-23592
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
