Back to Journals » OncoTargets and Therapy » Volume 10
The voice quality after laser surgery versus radiotherapy of T1a glottic carcinoma: systematic review and meta-analysis
Authors Huang GJ , Luo MS, Zhang JX, Liu HB
Received 16 March 2017
Accepted for publication 11 April 2017
Published 3 May 2017 Volume 2017:10 Pages 2403—2410
DOI https://doi.org/10.2147/OTT.S137210
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr William C. Cho
Guanjiang Huang,1,* Mengsi Luo,2,* Jingxuan Zhang,1 Hongbing Liu1
1Department of Otolaryngology – Head and Neck Surgery, 2Department of Anesthesiology, The Second Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, People’s Republic of China
*These authors contributed equally to this work
Background and objectives: The voice quality assessment of laser surgery (LS) in comparison with radiotherapy (RT) remains uncertain in T1a glottic carcinoma treatment. This systematic review and meta-analysis were conducted to compare the voice quality of the two treatments.
Methods: Searches were conducted in PubMed, EMBASE, and Cochrane with the following index words: glotti*, layn*, vocal cord, vocal, surgery, cordectomy, laser, radiation, irradiation, radiotherapy, cancer, and carcinoma for relative studies that compared the voice quality between LS and RT. Random-effect models were used, and heterogeneity was assessed.
Results: A total of 14 studies were included in the analysis, consisting of 1 randomized controlled trial, 1 prospective study, and 12 retrospective studies. RT has increased the maximum phonation time (MPT; mean difference [MD] =-1.89, 95% confidence interval [CI] =-3.66 to -0.11, P=0.04) and decreased the fundamental frequency (MD =14.06, 95% CI =10.30–17.83, P<0.00001) in comparison with LS. No statistical difference was observed between the two groups in terms of Voice Handicap Index, Jitter, Shimmer, and airflow rate.
Conclusion: RT may be a better choice for T1a glottic carcinoma treatment compared with LS because patients undergoing RT may have the advantage of increased MPT and decreased fundamental frequency. However, more multicenter, randomized, controlled trials are urgently needed to verify these differences.
Keywords: laser therapy, radiotherapy, meta-analysis, glottis, laryngeal neoplasms
Introduction
Laryngeal carcinoma is the most common malignant tumors of head and neck, and the majority of laryngeal carcinoma are confined within the glottic area.1,2 Owing to the involvement of the vocal folds, patients with glottic carcinoma always present with hoarseness in early stages. Therefore, glottic carcinoma can usually be diagnosed at the early stage and related treatment can often be achieved early.3,4
Laser surgery (LS), radiotherapy (RT), and open surgery all are accepted modalities of treatment for T1a glottic carcinoma. Open laryngectomy has been applied for >100 years. This method is still being used to cure T1a glottic carcinoma in locations that do not have access. Open surgery provides excellent exposure and has a higher rate of locoregional control, but voice quality is generally worse than that after RT or after LS.5–7 Furthermore, with the development of RT and the improvements in LS, open surgery is gradually being substituted. Therefore, open surgery should not be used any more for primary treatment of T1a glottic carcinoma.
Nowadays, T1a glottic carcinoma is usually treated by LS or RT. Both LS and RT have good oncology and survival outcomes.8,9 Low et al displayed a retrospective review covering all consecutive patients from 2003 to 2013; patients of T1a glottic carcinoma were offered the options of either LS or RT.10 There were 105 patients, of whom 53 were treated with LS and 52 were treated with RT. The 5-year overall survival of patients with T1a glottic carcinoma treated with LM versus RT was 86% versus 85% (P=0.887), laryngectomy-free survival (LFS) was 65% versus 77% (P=0.198), laryngectomy-free disease-specific survival (LFS-DSS) was 100% versus 88% (P=0.030), disease-free survival was 69% versus 78% (P=0.151), and ultimate locoregional control was 100% versus 100%.
Thus, the treatment option of LS and RT for patients of T1a glottic carcinoma often depends on quality of life, particularly the voice quality.1,11–13 In this paper, this meta-analysis is conducted to compare the voice quality of LS and RT, which can help better patients of T1a glottic carcinoma to choose a reasonable treatment.
Methods
Data sources and literature search strategy
Literature review was separately conducted by two investigators (GJH and MSL) through online data sources PubMed, EMBASE, and Cochrane (up to October 2016), using the following index words: glotti*, layn*, vocal cord, vocal, surgery, cordectomy, laser, radiation, irradiation, radiotherapy, cancer, and carcinoma.
Study selection
Inclusion criteria were: 1) randomized controlled trials, prospective studies or retrospective studies; 2) patients who underwent first treatment for T1a glottic carcinoma; 3) comparing LS with RT on interest outcomes such as Voice Handicap Index (VHI), acoustic analysis, and perceptual analysis; and 4) written in English language.
Study quality assessment
Study quality assessment was all conducted by The Newcastle–Ottawa Quality Assessment Scale (NOS). The study that is considered as high quality is eligible for the research.
Data extraction
The data on characteristics of studies, VHI, and acoustic analysis were extracted from the selected studies by one author (GJH) and checked by another author (JXZ). Information included are study name, publication year, study design, number of patients, age, sex, tumor stage, follow-up time, VHI, and acoustic analysis.
Statistical analysis
Review Manager Version 5.3 was applied to perform this meta-analysis. Outcome data reported as mean ± standard deviation (SD) were adopted, and mean difference (MD) was calculated. Continuous outcome variables were compared using weighted MD and 95% confidence intervals (CIs). Heterogeneity of the studies was evaluated by the chi-squared statistic and publication bias by funnel plots, in which significance was set at P<0.1. The I2 test was involved to measure the extent of inconsistency among results. The z statistic was used to test the overall pooled effect, and significance was set at P<0.05. All the statistical results use random-effect models. The subgroup analysis was conducted based on the study design.
Results
Eligible studies and characteristics of studies
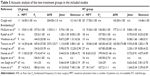
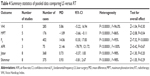
In this meta-analysis, 14 studies were included: 1 randomized controlled trial, 1 prospective study, and 12 retrospective studies (Figure 1). Only one randomized controlled trial is included. A total of 701 patients were included in the research, of whom 395 (56%) underwent LS and 306 (44%) underwent RT. The characteristics of the included studies are shown in Table 1, and detailed data are shown in Tables 2 and 3.
  | Figure 1 Stages of the systematic review of the trials. |
  | Table 2 VHI of the two treatment groups in the included studies |
Meta-analysis of postoperative outcomes
Voice Handicap Index
Among the included studies, only 5 studies provide detailed data on VHI with 162 patients in the LS group and 123 patients in the RT group. Heterogeneity was identified between the studies (Chi2 =25.26, P<0.0001, I2=84%); therefore, a random-effects model was used to calculate the pooled effect. Results of the pooled effect showed that the difference between LS and RT with respect to the VHI was not statistically significant (test for subgroup differences: MD =5.86, 95% CI =−5.22 to 16.84, P=0.30); in VHI (2004–2007) studies subgroup: MD =−5.32, 95% CI =−13.77 to 3.14, P=0.22, whereas in VHI (2008–2016) studies subgroup: MD =16.79, 95% CI =14.85 to 18.74, P<0.00001 (Figure 2).
Acoustic analysis
Among the included studies, 10 studies provide detailed data on acoustic analysis with 258 patients in the LS group and 224 patients in the RT group. RT has increased the maximum phonation time (MPT; MD =−1.89, 95% CI =−3.66 to −0.11, P=0.04; Figure 3A) and decreased the fundamental frequency (F0) (MD =14.06, 95% CI =10.30 to 17.83, P<0.00001; Figure 3B) in comparison with LS. There are no statistical significances in Jitter (MD =0.73, 95% CI =−0.37 to 1.83, P<0.00001; Figure 3C), Shimmer (MD =0.93, 95% CI =−0.81 to 2.67, P<0.00001; Figure 3D), and airflow rate (AFR) (MD =21.46, 95% CI =−78.79 to 121.72, P<0.00001; Figure 3E).
All outcomes of interest were listed in Table 4, and the funnel plots show the publication bias of the F0 (Figure 4).
  | Figure 4 Publication bias: funnel plots of F0. |
Perceptual analysis
One important method of voice quality evaluation is the perceptual analysis by GRBAS scale, and three studies were included. Voice quality was assessed on the GRBAS scale, consisting of grade (G), roughness (R), breathiness (B), asthenia (A), and strain (S). Ratings of these five aspects of voice quality varied from 0 (normal) to 3 (extremely abnormal).14–16 The higher the score, the more dysphonic the voice. Kono et al14 proved that tissue loss because of LS causes incomplete closure, which in turn is related to breathiness. Sjogren et al15 reported that patients showed mainly a mixed pattern of roughness and breathiness after RT, whereas patients were characterized as predominantly breathy after LS. They discussed that a possible explanation for these differences may be related to differences in classification of roughness. Aaltonen et al16 reported that breathiness improved after RT over the 2-year observation period, whereas no improvement in any of the five voice quality measures of the GRBAS scale occurred in the TLS group.
Discussion
In 2009, the European Laryngological Society developed a classification of transoral laser vocal cord resection.17 Type I: resection of vocal cord mucosa; Type II: resection of vocal cord mucosa and acoustic ligament; Type III: resection of vocal cord mucosa, acoustic ligament, and part of the vocal cord; Type IV: total vocal resection, including glottic fissure; Type V: total vocal resection, including anterior or arytenoid cartilage or part of the glottis or part of the subglottic structure. LS has plenty of unique advantages. It can achieve precise cutting, bloodless operation, short operation time, and significantly reduce the recurrence rate.11,18–20 Besides, the length of hospital stay will be shortened, and the cost of hospitalization is greatly reduced.21
At the same time, RT for T1a glottic carcinoma is more and more important, which has obvious therapeutic effects on T1a glottic carcinoma. RT can protect the laryngeal function and also can achieve similar therapeutic effects of surgery for patients of T1a glottic carcinoma.10,13,19 With the development of science and technology, modern RT technology tends to be more targeted accurately. Compared with conventional RT, modern RT technology can be accurately applied to the tumor location and reduce the damage to normal cells.22,23 Nowadays, RT has been the gold standard for T1a glottic carcinoma treatment, but gradually the use of LS has increased. Therefore, patient-related factors may be the most important when choosing the treatment option for T1a glottic carcinoma.
With respect to VHI, sensitivity testing was conducted by subgroup analysis because there is moderate heterogeneity among the studies. The studies are subgrouped by the published year. The pooled effect of studies published before 2007 shows no significant difference for VHI between the two treatment modalities. However, a different result is gained in the meta-analysis on studies published after 2008, which shows that VHI is significantly higher in patients treated with LS than that in those treated with RT, which proves that RT may be superior than LS on VHI. This demonstrates the fact that from the last decade, modern RT technology for T1a glottic carcinoma is becoming increasingly mature.
This meta-analysis of the parameters of acoustic analysis displayed that there is no significant difference between patients treated with LS and RT with respect to AFR, Jitter, and Shimmer. Only in the meta-analysis of MPT and F0, differences between patients treated with LS and RT are proved to be statistically significant. When comparing parameters of acoustic analysis between LS and RT, MPT is analyzed alone because MPT offers favorable outcomes, whereas the other parameters lead to unfavorable outcomes. Therefore, we could cautiously speculate that RT may be superior than LS on VHI.
With respect to perceptual analysis, overall voice quality was almost similar in RT group and LS group, however, indicating a need for careful consideration of patient-related factors to choose the treatment option. The vocal cord defect is caused by carcinoma, and TLS frequently causes long-lasting voice impairment.16 Yet, individual compensation is an important factor contributing to final voice quality, and it may sometimes lead to an excellent voice.15
However, we still have some limitations for such this meta-analysis: 1) the sample number of the analysis is relatively low, and selection bias could be excluded; 2) only one randomized controlled trial is included, and the proportion of the prospective study is relatively small. Most of them are retrospective studies, which undoubtedly led to the increase in the heterogeneity of our analysis; 3) the studies included lacked detailed information on the radiation dose for RT and different types of the laser equipment for LS, which may also cause additional heterogeneity; 4) the treatment of a patient generally depends on the doctors’ preferences or the patient’s wishes; the follow-up times and sample sizes were also inconsistent; 5) the aforementioned factors lacked unified standards, and thus, may have had an uncertain impact on the final results.
Our results show no statistically significant differences in most of VHI and the acoustic outcomes between patients of T1a glottic carcinoma treated with LS and those treated with RT. Although data do not reach a level of statistical significance, there is a mild tendency in all parameters that favors RT. This finding should be cautiously speculated because of significant heterogeneity among the included studies, which could be originated from limited quality attributed to variable reporting, small sample size, and various types of biases discussed. Therefore, the work needs to be improved when there are more large, multicenter, and randomized controlled trials.
Conclusion
Patients who had undergone RT have increased MPT and decreased F0 in comparison with LS. No statistical difference was observed between the two groups in terms of VHI, Jitter, Shimmer, and AFR. In conclusion, RT may be a better choice for T1a glottic carcinoma treatment, and patient-related factors may be the most important when choosing the treatment option for T1a glottic carcinoma. To confirm our findings, more large, multicenter, and randomized controlled trials are urgently needed.
Disclosure
The authors report no conflicts of interest in this work.
References
Lee HS, Kim JS, Kim SW, et al. Voice outcome according to surgical extent of transoral laser microsurgery for T1 glottic carcinoma. Laryngoscope. 2016;126(9):2051–2056. | ||
Ahn SH, Hong HJ, Kwon SY, et al. Guidelines for the Surgical Management of Laryngeal Cancer: Korean Society of Thyroid-Head and Neck Surgery. Clin Exp Otorhinolaryngol. 2017;10(1):1–43. | ||
Eskiizmir G, Baskin Y, Yalcin F, Ellidokuz H, Ferris RL. Risk factors for radiation failure in early-stage glottic carcinoma: a systematic review and meta-analysis. Oral Oncol. 2016;62:90–100. | ||
Peng Z, Li Y, Jin L, et al. Retrospective analysis of therapeutic effect and prognostic factors on early glottic carcinoma. Photodiagnosis Photodyn Ther. 2016;15:167–171. | ||
Lucioni M, Bertolin A, Lionello M, et al. Open partial horizontal laryngectomy for salvage after failure of CO2 laser-assisted surgery for glottic carcinoma. Eur Arch Otorhinolaryngol. 2016;273(1):169–175. | ||
Succo G, Crosetti E, Bertolin A, et al. Benefits and drawbacks of open partial horizontal laryngectomies, part A: early- to intermediate-stage glottic carcinoma. Head Neck. 2016;38(Suppl 1):E333–E340. | ||
El Ouakif F, Veresezan O. [Functional comparison of the voice quality after either open conservative surgery or only radiotherapy for early glottic carcinoma]. Rev Laryngol Otol Rhinol (Bord). 2015;136(1):17–20. French. | ||
Comert E, Tuncel U, Dizman A, Guney YY. Comparison of early oncological results of diode laser surgery with radiotherapy for early glottic carcinoma. Otolaryngol Head Neck Surg. 2014;150(5):818–823. | ||
Murono S, Endo K, Kondo S, Wakisaka N, Yoshizaki T. Oncological and functional outcome after transoral 532-nm pulsed potassium-titanyl-phosphate laser surgery for T1a glottic carcinoma. Lasers Med Sci. 2013;28(2):615–619. | ||
Low TH, Yeh D, Zhang T, et al. Evaluating organ preservation outcome as treatment endpoint for T1aN0 glottic cancer. Laryngoscope. 2016. Epub October 25, 2016. | ||
Day AT, Sinha P, Nussenbaum B, et al. Management of primary T1-T4 glottic squamous cell carcinoma by transoral laser microsurgery. Laryngoscope. 2017;127(3):597–604. | ||
Greulich MT, Parker NP, Lee P, Merati AL, Misono S. Voice outcomes following radiation versus laser microsurgery for T1 glottic carcinoma: systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2015;152(5):811–819. | ||
Canis M, Ihler F, Martin A, et al. Transoral laser microsurgery for T1a glottic cancer: review of 404 cases. Head Neck. 2014;37(6):889–895. | ||
Kono T, Saito K, Yabe H, Uno K, Ogawa K. Comparative multidimensional assessment of laryngeal function and quality of life after radiotherapy and laser surgery for early glottic cancer. Head Neck. 2016;38(7):1085–1090. | ||
Sjogren EV, van Rossum MA, Langeveld TP, et al. Voice outcome in T1a midcord glottic carcinoma: laser surgery vs radiotherapy. Arch Otolaryngol Head Neck Surg. 2008;134(9):965–972. | ||
Aaltonen LM, Rautiainen N, Sellman J, et al. Voice quality after treatment of early vocal cord cancer: a randomized trial comparing laser surgery with radiation therapy. Int J Radiat Oncol Biol Phys. 2014;90(2):255–260. | ||
Remacle M, Eckel HE, Antonelli A, et al. Endoscopic cordectomy. A proposal for a classification by the Working Committee, European Laryngological Society. Eur Arch Otorhinolaryngol. 2000;257(4):227–231. | ||
van Loon Y, Stiggelbout AM, Hakkesteegt MM, Langeveld TP, de Jong RJ, Sjogren EV. Utility approach to decision-making in extended T1 and limited T2 glottic carcinoma. Head Neck. 2017;39(4):779–785. | ||
Mo HL, Li J, Yang X, et al. Transoral laser microsurgery versus radiotherapy for T1 glottic carcinoma: a systematic review and meta-analysis. Lasers Med Sci. 2017;32(2):461–467. | ||
Chiesa EC, Reinoso FA, Velasquez AO, Fernandez JL, Conde JL, Hidalgo CS. Transoral CO2 laser microsurgery outcomes for early glottic carcinomas T1-T2. Int Arch Otorhinolaryngol. 2016;20(3):212–217. | ||
Prettyjohns M, Winter S, Kerawala C, Paleri V. Transoral laser microsurgery versus radiation therapy in the management of T1 and T2 laryngeal glottic carcinoma: which modality is cost-effective within the UK? Clin Otolaryngol. 2017;42(2):404–415. | ||
Ermis E, Teo M, Dyker KE, Fosker C, Sen M, Prestwich RJ. Definitive hypofractionated radiotherapy for early glottic carcinoma: experience of 55Gy in 20 fractions. Radiat Oncol. 2015;10:203. | ||
Higashino M, Kawata R, Lee K, Nishikawa S, Ichihara S, Uesugi Y. Radiotherapy concurrent with S-1 and radiotherapy alone for T2N0 glottic carcinoma: a retrospective comparative study. Auris Nasus Larynx. 2014;41(4):364–368. | ||
Cragle SP, Brandenburg JH. Laser cordectomy or radiotherapy: cure rates, communication, and cost. Otolaryngol Head Neck Surg. 1993;108(6):648–654. | ||
McGuirt WF, Blalock D, Koufman JA, et al. Comparative voice results after laser resection or irradiation of T1 vocal cord carcinoma. Arch Otolaryngol Head Neck Surg. 1994;120(9):951–955. | ||
Rydell R, Schalen L, Fex S, Elner A. Voice evaluation before and after laser excision vs radiotherapy of T1A glottic carcinoma. Acta Otolaryngol. 1995;115(4):560–565. | ||
Wedman J, Heimdal JH, Elstad I, Olofsson J. Voice results in patients with T1a glottic cancer treated by radiotherapy or endoscopic measures. Eur Arch Otorhinolaryngol. 2002;259(10):547–550. | ||
Tamura E, Kitahara S, Ogura M, Kohno N. Voice quality after laser surgery or radiotherapy for T1a glottic carcinoma. Laryngoscope. 2003;113(5):910–914. | ||
Krengli M, Policarpo M, Manfredda I, et al. Voice quality after treatment for T1a glottic carcinoma – radiotherapy versus laser cordectomy. Acta Oncol. 2004;43(3):284–289. | ||
Peeters AJ, van Gogh CD, Goor KM, Verdonck-de Leeuw IM, Langendijk JA, Mahieu HF. Health status and voice outcome after treatment for T1a glottic carcinoma. Eur Arch Otorhinolaryngol. 2004;261(10):534–540. | ||
Loughran S, Calder N, Macgregor FB, Carding P, MacKenzie K. Quality of life and voice following endoscopic resection or radiotherapy for early glottic cancer. Clin Otolaryngol. 2005;30(1):42–47. | ||
Goor KM, Peeters AJ, Mahieu HF, et al. Cordectomy by CO2 laser or radiotherapy for small T1a glottic carcinomas: costs, local control, survival, quality of life, and voice quality. Head Neck. 2007;29(2):128–136. | ||
Nunez BF, Caminero CM, Senaris GB, et al. Voice quality after endoscopic laser surgery and radiotherapy for early glottic cancer: objective measurements emphasizing the Voice Handicap Index. Eur Arch Otorhinolaryngol. 2008;265(5):543–548. | ||
van Gogh CD, Verdonck-De LI, Wedler-Peeters J, Langendijk JA, Mahieu HF. Prospective evaluation of voice outcome during the first two years in male patients treated by radiotherapy or laser surgery for T1a glottic carcinoma. Eur Arch Otorhinolaryngol. 2012;269(6):1647–1652. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.