Back to Journals » Journal of Pain Research » Volume 16
The Twenty-Five Most Cited Articles About Adductor Canal Block: A Bibliometric Analysis from 1980 to 2022
Authors Coviello A , Iacovazzo C, Cirillo D , Diglio P, Bernasconi A , D'Abrunzo A, Barone MS, Posillipo C, Vargas M, Servillo G
Received 31 March 2023
Accepted for publication 7 August 2023
Published 2 October 2023 Volume 2023:16 Pages 3353—3365
DOI https://doi.org/10.2147/JPR.S415184
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jinlei Li
Antonio Coviello,1,* Carmine Iacovazzo,1,* Dario Cirillo,1 Pasquale Diglio,1 Alessio Bernasconi,2 Anella D’Abrunzo,1 Maria Silvia Barone,1 Concetta Posillipo,1 Maria Vargas,1 Giuseppe Servillo1
1Department of Neurosciences, Reproductive and Odontostomatological Sciences, “Federico II” University of Naples, Naples, Italy; 2Department of Public Health, School of Medicine, “Federico II” University of Naples, Unit of Orthopedics and Traumatology, Naples, Italy
*These authors contributed equally to this work
Correspondence: Antonio Coviello, Department of Neurosciences, Reproductive and Odontostomatological Sciences, “Federico II” University of Naples, Via Sergio Pansini, 5, Naples, NA, 80131, Italy, Tel +39 3497013533, Fax +39 0817462281, Email [email protected]
Introduction: Loco-regional anesthesia role is increasingly important in surgery, especially in postoperative pain control. Using ultrasound-guided techniques has made the loco-regional approach increasingly safe and manageable, guaranteeing excellent analgesic results and patient compliance. This bibliometric research aimed to identify the most influential papers on the adductor canal blocks and outline their characteristics.
Methods: All articles published from 1980 to 2022 were included in the Web of Science, PubMed, and Scopus databases and found using the keywords “Adductor canal block” or “Saphenous nerve block” or “Peripheral nerve block” or “Hunter canal block” or “Subsartorial canal block” or “ACB” or “Knee” or “TKR” or “TKA” or “Analgesia” or “Arthroplasty” or “Replacement” in the title section had bibliometric analysis performed. The first 25 papers were selected and analyzed by the number of citations. The correlation between numerical variables was evaluated using the Pearson Correlation coefficient.
Results: Literature screening found 252 publications. One hundred ten were only about the adductor canal block. Of these, 25 articles were selected for our bibliometric study, published in 8 different journals and with a total number of citations equal to 1.457. “Regional Anesthesia and pain medicine” journal – with 9 articles – was the one that produced the most. There was a significant strong correlation between the n. of citations and the citation rate (R = 0.84, p < 0.001).
Conclusion: The purpose of this study is to be a guide on regional anesthesia and, particularly, on adductor canal block, making the most effective as well as the most cited articles available to anesthesiologists or other researchers interested in this topic.
Keywords: adductor canal block, peripheral nerve block, bibliometric, TKA, TKR, analgesia
Introduction
Locoregional anesthesia, especially postoperative analgesia, is increasingly being performed for surgeries executed under both neuraxial and general anesthesia.1 In the postoperative period, neuraxial anesthesia has a lower risk of complications and mortality than general anesthesia.2 Any type of surgery is performed, locoregional anesthesia – with an ultrasound-guided technique – results in excellent analgesia and reduced complications.1–4 Total knee replacement surgery for orthopedic surgery causes postoperative pain that is difficult to manage and, in this case, a continuous epidural block is still an effective anesthesiologic approach. However, this approach cannot be performed in all patients because of coagulopathies and technique difficulty.3–5 Ultrasound-guided locoregional anesthesia is a more selective and patient-tailored method that consists of a sensory block of the saphenous nerve in Hunter’s canal.6 Many anesthesiologists perform this type of technique but the difficulty is often finding the right sources to understand how to approach it as best they can from both anatomical and procedural points of view.
Adductor canal block represents a viable alternative regarding postoperative analgesia in knee surgery.6 The adductor canal is an aponeurotic structure located in the medial part of the thigh that extends from the apex of Scarpa’s triangle to the adductor hiatus. The femoral vessels and saphenous nerve run through it.7 There are well-defined ultrasound findings to establish the origin of Hunter’s canal that allow us to avoid motor block involvement of the vastus medialis muscle.8 Therefore, the adductor canal block is a purely sensory peripheral nerve block. As such, it is an effective technique for fast-track surgery protocols because it could provide some benefits: improved mobility, reduced risk of falls, and significantly reduced hospitalization time.9
In recent times, there has been an increasing trend of bibliometric studies performed in healthcare.10–15 Employing quantitative measures, bibliometric analyses aim to examine the trend in publications about a specific topic, defining the characteristics of most influential manuscripts and identifying potential correlations regarding the type of study, its quality, its level of evidence, etc.10–13 Bibliometric studies are important tools in evaluating research performance and identifying influential papers in a particular field. By comparing changes in the citation trends of published papers, it is possible to better understand the current research situation and determine the direction for future efforts.14,15
The purpose of this study is to provide anesthesiologists with a collection of articles related to adductor canal block and to summarize what has been shown so far by the most influential papers produced on this topic.
Materials and Methods
Literature scanning was performed with the Web of Science (WoS: by Clavariate Analytics), PubMed and Scopus databases selected anesthesiology journals (access date: 03.01.2022). All articles containing the search keywords in the “Title” section, published from 1980 to 2022 in the WoS, PubMed, and Scopus databases, had performed bibliometric analysis. The search keywords used the following codes: “Adductor canal block” or “Saphenous nerve block” or “Peripheral nerve block” or “Hunter canal block” or “Subsartorial canal block” or “ACB” or “Knee” or “TKR” or “TKA” or “Analgesia” or “Arthroplasty” or “Replacement”.
The research was not limited only to English-language articles. Articles comparing saphenous nerve block in Hunter’s canal with other types of techniques were kept out of the exclusion criteria because there could be a citation bias (Figure 1).
 |
Figure 1 Flowchart of the study. |
The research was performed by two authors independently of each other.
About the articles concerning only the adductor canal block, we researched the following information: year of publication, authors, journal of publication and number of citations, geographic area, study type and citation density, and subject.
Data were reported as mean value, standard deviation, and range values (minimum and maximum). The correlation between variables was assessed using the Pearson Correlation Coefficient. The correlation was considered strong if the coefficient value lay between ± 0.50 and ± 1, moderate between ± 0.30 and ± 0.49, and poor below ± 0.29. The statistical analysis was performed using Stata (Version 16).
The outcomes of this study were the number of citations and the citation rate.
Results
Literature screening found a total of 252 published items. One hundred and ten of them were focused on the adductor canal block. These were published from 1993 to 2022 with a peak of interest in the topic occurring in 2014 (Figure 2). The active journals produced most of the articles as shown in Figure 3.
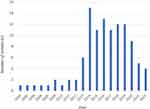 |
Figure 2 Number of publications by years on adductor canal block. |
 |
Figure 3 Active journals on adductor canal block. |
The top 10 authors published most papers for adductor canal block and the number of citations appeared in Table 1.
 |
Table 1 Authors with Top-10 Number of Papers Included in the 110 Most-Cited |
The 25 most-cited papers have been depicted in Table 2.6–8,16–37
 |
Table 2 25 Most Cited Articles About ACB |
The research only performed a bibliometric analysis of the 25 published articles.6–8,16–37
It was selected because the citation density of the other found articles was very low. There were a total of 1.457 citations of the 25 articles, with an average citation per item of 58.28. The keywords of the 25 most cited articles are shown in Figure 4.
 |
Figure 4 The keywords of the 25 most cited articles. |
The 25 articles were published in 8 journals.6–8,16–37 Among these journals, “Regional Anesthesia and pain medicine” - with 9 articles – was the one that produced the most (Figure 5).7,8,31–37
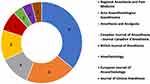 |
Figure 5 Active journals in 25 most cited articles. |
The impact factors and quartile of the journals which were the most interested in the topic are shown in Table 3. Figure 6 shows that most of these journals were in the first quartile.
 |
Table 3 The IF of the Journals About 25 Most Cited Articles |
 |
Figure 6 Quartile analysis of the 25 most cited articles. Abbreviation: Q, Quartile. |
The publication year of the 25 most cited articles ranges from 1993 to 2017.6–8,16–37
Denmark, the United States, and Canada were respectively the active countries that produced the most (Figure 7).6–8,16–22,24–33,35–37
 |
Figure 7 The distribution of the 25 most cited articles according to countries in the world. |
Nine articles concerned only with analgesia,6,16–18,20,25,29,30,32 4 only with anatomy,31,33,36,37
1 only with ultrasonography,26 2 with ultrasonographic anatomy,19,23 4 with analgesia and ultrasonography,7,8,21,28 3 with analgesia and anatomy,27,34,35 2 with analgesia and ultrasonographic anatomy.22,24
We found a strong correlation between the n. of citations of a study and its citation rate (R = 0.84, p < 0.001) (Table 4 and Figure 8). Conversely, no correlation was identified between the year of publication and the number of citations of a study (p = 0.62) nor its citation rate (p = 0.15). No correlation between the level of evidence and the number of citations (p = 0.23) nor the citation rate (p = 0.26) was found.
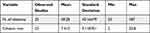 |
Table 4 Correlation Between the N. of Citations and the Citation Rate |
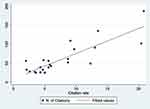 |
Figure 8 Scatterplot n. of citations/citation rate. |
Discussion
According to our research findings, a significant increasing trend was found for the number of articles about the topic of adductor canal block with a peak of interest occurring in 2014.20,21,25,32,35,37
When the article distribution by country was investigated, it was observed that Denmark, the USA, and Canada were respectively the active countries that produced the most.6–8,16–22,24–33,35–37
Our research highlighted the main topics on the adductor canal: anatomy of the adductor canal, ultrasound-anatomy, ultrasound-guided approach for ACB, and postoperative analgesia.6–8,16–37
Seventy-two percent of the examined articles were concerned with analgesia: they focused on various anesthetic mixtures and the analgesic efficacy of the block in knee surgery.6–8,16–18,20–22,24,25,27–30,32,34,35
None of the 25 most cited papers focused on the comparison of the single-shot technique versus continuous infusion with a perineural catheter, the devices to be used, or the incidence of major and minor complications. In addition, it was noted that in the 25 most cited studies there were few with high scientific evidence such as systematic reviews or meta-analysis.
In the past, postoperative analgesia was mostly peridural, whereas in recent years peripheral regional echo-guided loco-regional is increasingly chosen especially the adductor canal block in knee surgery.3,4 Probably, the increased incidence of echo-guided loco-regional anesthesia, compared with continuous neuraxial anesthesia, is explained by the easiest reproducibility of the technique. Also, continuous peridural analgesia is often not feasible in all patients due to a lack of clinical skills or because of an expected technique that is difficult to perform.
Postoperative analgesia by adductor canal block, compared with neuraxial analgesia, allows a lower incidence of the motor block because the saphenous nerve is purely sensory and consequently allows early mobilization.9 Loco-regional anesthesia has a cost impact compared with general anesthesia.38 It must be remembered that sensory blocks, as well as fascia blocks, are not without complications.39 In patients undergoing primary total knee implantation, a single-shot block in the context of multimodal analgesia is also optimal for pain management in the first 24 hours after surgery.16 Neuromuscular diseases, such as multiple sclerosis, are not contraindications to loco-regional anesthesia.40,41
The adductor canal block can be performed as a single-shot puncture, resulting in temporary analgesia depending on the concentration of local anesthetic in the mixture or it can be performed with a continuous infusion by catheter placement in the perineural site.42
Antonio Coviello et al, in this retrospective single-center study, compared different positions of the catheter tip concerning the saphenous nerve in terms of efficacy and complications, concluding that positioning the catheter tip posteriorly to the saphenous nerve may lead to greater postoperative analgesia and reduce the risk of pump block compared to placing the catheter tip anteriorly to the nerve.43
In this human cadaver study, Pierre Goffin et al observed that after injection of 20 mL of local anesthetic, it diffused through the interfascial planes into the popliteal fossa, hypothesizing that this volume of anesthetic could also determine analgesia of the posterior part of the knee.44
Scientific articles that help best approach the technique both with anatomical indications on cadavers and especially with information on ultrasound-anatomy and the type of drug mixtures to be used are increasingly available in the literature and can be helpful to those using to these techniques. The analysis of the appropriate literature is essential and time-consuming to find the appropriate information. This is the reason why this study was conducted.
A limitation of our study is that there are only articles published in anesthesia journals. Additionally, in situations where more than one database is used for bibliometric studies analyzing large numbers of articles, the inclusion of the same article more than once in the analysis may affect the reliability of the results.
We can do some suggestions for future research. A bibliometric study is primarily intended to offer research suggestions. Outcome analysis is a key aspect of the research. The most important gap to be addressed is the standardization of methods and the definition of protocols, this gap is shown in other analgesic technique areas.45 In other words, the lack of uniform application criteria can limit the judgment on the effectiveness of the technique. Although adductor canal block is a simple intervention, practitioners must customize their treatment strategy based on several variables. Therefore, good practice guidelines are needed. Finally, the absence of an analysis of adverse events is a serious gap.
Conclusion
This bibliometric analysis showed that the produced literature on the topic is progressively increasing. There were no metanalysis and few systemic reviews among the 25 most cited papers on the topic. This summary will allow an anesthesiologist or other researcher to see the most effective articles, most cited articles, and perhaps the articles that should initially be read about this topic. Observing which journals produce the most articles in this scope and which journals contain articles receiving the most citations will allow easy assessment of current data. A bibliometric analysis is a profitable opportunity for highlighting potential gaps in the literature. Concerning adductor canal block, more studies with a high level of scientific evidence need to be produced. On the other hand, there is the necessity to increase clinical research as well as scientific collaboration between researcher teams and institutions from different countries.
Data Sharing Statement
Research data supporting this publication are available from the Web of Science, PubMed, and Scopus. All charts and analysis in this article are derived based on these original data.
Ethical Approval
The authors confirmed that no ethical approval is required.
Acknowledgments
The authors would like to thank the reviewer, Anna Onza, for the effort and the time spent on the linguistic revision of the manuscript.
Author Contributions
A. Coviello: Conceptualization, Reviewing, and Writing
C.Iacovazzo: Reviewing and Writing
D.Cirillo: Conceptualization, Writing
P.Diglio: Data curation, Writing
A.Bernasconi: Acquisition data, Writing
Anella D’Abrunzo: Analysis and/or interpretation of data, Writing
M.S. Barone: Study design, Writing
C. Posillipo: Drafting, Execution, Writing
M. Vargas: Choice of the journal to which the article will be submitted and Writing
G. Servillo: Critically reviewed the article and Writing
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kamel I, Ahmed MF, Sethi A. Regional anesthesia for orthopedic procedures: what orthopedic surgeons need to know. World J Orthop. 2022;13(1):11–35. doi:10.5312/wjo.v13.i1.11
2. Memtsoudis SG, Cozowicz C, Bekeris J, et al. AnestheticAnesthetic care of patients undergoing primary hip and knee arthroplasty: consensus recommendations from the international consensus on anaesthesia-related outcomes after surgery group (ICAROS) based on a systematic review and meta-analysis. Br J Anaesth. 2019;123(3):269–287. doi:10.1016/j.bja.2019.05.042
3. Coviello A, Spasari E, Ianniello M, et al. Intra-procedural catheter displacement for continuous adductor canal block: catheter-through-needle method vs catheter-through-split cannula method. Perioper Care Oper Room Mang. 2022;27:100255. doi:10.1016/j.pcorm.2022.100255
4. Coviello A, Spasari E, Ianniello M, et al. Corrigendum to Intra-procedural catheter displacement for continuous adductor canal block: catheter-through-needle method vs catheter-through-split-cannula method. Perioper Care Oper Room Mang. 2022;28:100265. doi:10.1016/j.pcorm.2022.100265
5. Rawal N. Current issues in postoperative pain management. Eur J Anaesthesiol. 2016;33(3):160–171. doi:10.1097/EJA.0000000000000366
6. Vora MU, Nicholas TA, Kassel CA, Grant SA. Adductor canal block for knee surgical procedures: review article. J Clin Anesth. 2016;35:295–303. doi:10.1016/j.jclinane.2016.08.021
7. Bendtsen TF, Moriggl B, Chan V, Børglum J. Basic topography of the saphenous nerve in the femoral triangle and the adductor canal. Reg Anesth Pain Med. 2015;40(4):391–392. PMID: 26079358. doi:10.1097/AAP.0000000000000261
8. Manickam B, Perlas A, Duggan E, Brull R, Chan VW, Ramlogan R. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Reg Anesth Pain Med. 2009;34(6):578–580. PMID: 19916251. doi:10.1097/aap.0b013e3181bfbf84
9. Macrinici GI, Murphy C, Christman L, et al. Prospective, double-blind, randomized study to evaluate single-injection adductor canal nerve block versus femoral nerve block: postoperative functional outcomes after total knee arthroplasty. Reg Anesth Pain Med. 2017;42(1):10–16. PMID: 27811526. doi:10.1097/AAP.0000000000000507
10. Mi X, Wang X, Yang N, et al. Hundred most cited articles in perioperative neurocognitive disorder: a bibliometric analysis. BMC Anesthesiol. 2021;21(1):186. doi:10.1186/s12871-021-01408-4
11. Demir E, Comba A. The evolution of celiac disease publications: a holistic approach with bibliometric analysis. Ir J Med Sci. 2020;189(1):267–276. doi:10.1007/s11845-019-02080-x
12. Doğan G, Kayır S. Global scientific outputs of brain death publications and evaluation according to the religions of countries. J Relig Health. 2020;59(1):96–112. doi:10.1007/s10943-019-00886-8
13. Doğan G. The effect of religious beliefs on the publication productivity of countries in circumcision: a comprehensive bibliometric view. J Relig Health. 2020;59(2):1126–1136. doi:10.1007/s10943-020-00985-x
14. Demir E. The evolution of spirituality, religion and health publications: yesterday, today and tomorrow. J Relig Health. 2019;58(1):1–13. doi:10.1007/s10943-018-00739-w
15. Muslu Ü, Demir E. Development of rhinoplasty: yesterday and today. Med Sci. 2019;23:294–301.
16. Jenstrup MT, Jæger P, Lund J, et al. Effects of adductor-canal-blockade on pain and ambulation after total knee arthroplasty: a randomized study. Acta Anaesthesiol Scand. 2012;56(3):357–364. PMID: 22221014. doi:10.1111/j.1399-6576.2011.02621.x
17. Lund J, Jenstrup MT, Jaeger P, Sørensen AM, Dahl JB. Continuous adductor-canal-blockade for adjuvant post-operative analgesia after major knee surgery: preliminary results. Acta Anaesthesiol Scand. 2011;55(1):14–19. PMID: 21039357. doi:10.1111/j.1399-6576.2010.02333.x
18. Jaeger P, Grevstad U, Henningsen MH, Gottschau B, Mathiesen O, Dahl JB. Effect of adductor-canal-blockade on established, severe post-operative pain after total knee arthroplasty: a randomised study. Acta Anaesthesiol Scand. 2012;56(8):1013–1019. PMID: 22834681. doi:10.1111/j.1399-6576.2012.02737.x
19. Andersen HL, Andersen SL, Tranum-Jensen J. The spread of injectate during saphenous nerve block at the adductor canal: a cadaver study. Acta Anaesthesiol Scand. 2015;59(2):238–245. PMID: 25496028. doi:10.1111/aas.12451
20. Veal C, Auyong DB, Hanson NA, Allen CJ, Strodtbeck W. Delayed quadriceps weakness after continuous adductor canal block for total knee arthroplasty: a case report. Acta Anaesthesiol Scand. 2014;58(3):362–364. PMID: 24372058. doi:10.1111/aas.12244
21. Hanson NA, Allen CJ, Hostetter LS, et al. Continuous ultrasound-guided adductor canal block for total knee arthroplasty: a randomized, double-blind trial. Anesth Analg. 2014;118(6):1370–1377. PMID: 24842182. doi:10.1213/ANE.0000000000000197
22. Kent ML, Hackworth RJ, Riffenburgh RH, et al. A comparison of ultrasound-guided and landmark-based approaches to saphenous nerve blockade: a prospective, controlled, blinded, crossover trial. Anesth Analg. 2013;117(1):265–270. PMID: 23632054. doi:10.1213/ANE.0b013e3182908d5d
23. Gautier PE, Hadzic A, Lecoq JP, Brichant JF, Kuroda MM, Vandepitte C. Distribution of injectate and sensory-motor blockade after adductor canal block. Anesth Analg. 2016;122(1):279–282. PMID: 26678473. doi:10.1213/ANE.0000000000001025
24. Benzon HT, Sharma S, Calimaran A. Comparison of the different approaches to saphenous nerve block. Anesthesiology. 2005;102(3):633–638. PMID: 15731603. doi:10.1097/00000542-200503000-00023
25. Grevstad U, Mathiesen O, Lind T, Dahl JB. Effect of adductor canal block on pain in patients with severe pain after total knee arthroplasty: a randomized study with individual patient analysis. Br J Anaesth. 2014;112(5):912–919. PMID: 24401802. doi:10.1093/bja/aet441
26. Jæger P, Jenstrup MT, Lund J, et al. Optimal volume of local anaesthetic for adductor canal block: using the continual reassessment method to estimate ED95. Br J Anaesth. 2015;115(6):920–926. PMID: 26582853. doi:10.1093/bja/aev362
27. van der Wal M, Lang SA, Yip RW. Transsartorial approach for saphenous nerve block. Can J Anaesth. 1993;40(6):542–546. PMID: 8403121. doi:10.1007/BF03009739
28. Tsai PB, Karnwal A, Kakazu C, Tokhner V, Julka IS. Efficacy of an ultrasound-guided subsartorial approach to saphenous nerve block: a case series. Can J Anaesth. 2010;57(7):683–688. PMID: 20428987. doi:10.1007/s12630-010-9317-1
29. Hanson NA, Derby RE, Auyong DB, et al. Ultrasound-guided adductor canal block for arthroscopic medial meniscectomy: a randomized, double-blind trial. Can J Anaesth. 2013;60(9):874–880. PMID: 23820968. doi:10.1007/s12630-013-9992-9
30. Espelund M, Fomsgaard JS, Haraszuk J, Mathiesen O, Dahl JB. Analgesic efficacy of ultrasound-guided adductor canal blockade after arthroscopic anterior cruciate ligament reconstruction: a randomised controlled trial. Eur J Anaesthesiol. 2013;30(7):422–428. PMID: 23549123. doi:10.1097/EJA.0b013e328360bdb9
31. Burckett-St Laurant D, Peng P, Girón Arango L, et al. The nerves of the adductor canal and the innervation of the knee: an anatomic study. Reg Anesth Pain Med. 2016;41(3):321–327. PMID: 27015545. doi:10.1097/AAP.0000000000000389
32. Chen J, Lesser JB, Hadzic A, Reiss W, Resta-Flarer F. Adductor canal block can result in motor block of the quadriceps muscle. Reg Anesth Pain Med. 2014;39(2):170–171. PMID: 24553306. doi:10.1097/AAP.0000000000000053
33. Horn JL, Pitsch T, Salinas F, Benninger B. Anatomic basis to the ultrasound-guided approach for saphenous nerve blockade. Reg Anesth Pain Med. 2009;34(5):486–489. PMID: 19920424. doi:10.1097/AAP.0b013e3181ae11af
34. Saranteas T, Anagnostis G, Paraskeuopoulos T, et al. Anatomy and clinical implications of the ultrasound-guided subsartorial saphenous nerve block. Reg Anesth Pain Med. 2011;36(4):399–402. PMID: 21697687. doi:10.1097/AAP.0b013e318220f172
35. Wong WY, Bjørn S, Strid JM, Børglum J, Bendtsen TF. Defining the location of the adductor canal using ultrasound. Reg Anesth Pain Med. 2017;42(2):241–245. PMID: 28002228; PMCID: PMC5318152. doi:10.1097/AAP.0000000000000539
36. Bendtsen TF, Moriggl B, Chan V, Pedersen EM, Børglum J. Defining adductor canal block. Reg Anesth Pain Med. 2014;39(3):253–254. PMID: 24747312. doi:10.1097/AAP.0000000000000052
37. Bendtsen TF, Moriggl B, Chan V, Pedersen EM, Børglum J. Redefining the adductor canal block. Reg Anesth Pain Med. 2014;39(5):442–443. PMID: 25140514. doi:10.1097/AAP.0000000000000119
38. De Robertis E, Zito Marinosci G, Romano GM, et al. The use of sugammadex for bariatric surgery: analysis of recovery time from neuromuscular blockade and possible economic impact. Clinicoecon Outcomes Res. 2016;8:317–322. PMID: 27418846; PMCID: PMC4934482. doi:10.2147/CEOR.S109951
39. Coviello A, Golino L, Maresca A, Vargas M, Servillo G. Erector spinae plane block in laparoscopic nephrectomy as a cause of involuntary hemodynamic instability: a case report. Clin Case Rep. 2021;9:e04026. doi:10.1002/ccr3.4026
40. Lanzillo R, Cennamo G, Moccia M, et al. Retinal vascular density in multiple sclerosis: a 1-year follow-up. Eur J Neurol. 2019;26(1):198–201. PMID: 30102834. doi:10.1111/ene.13770
41. Cennamo G, Carotenuto A, Montorio D, et al. Peripapillary vessel density as early biomarker in multiple sclerosis. Front Neurol. 2020;11:542. PMID: 32625163; PMCID: PMC7311750. doi:10.3389/fneur.2020.00542
42. Hussain N, Brull R, Zhou S, et al. Analgesic benefits of single-shot versus continuous adductor canal block for total knee arthroplasty: a systemic review and meta-analysis of randomized trials. Reg Anesth Pain Med. 2023;48(2):49–60. PMID: 36351742. doi:10.1136/rapm-2022-103756
43. Coviello A, Bernasconi A, Balato G, et al. Positioning the catheter tip anterior or posterior to the saphenous nerve in continuous adductor canal block: a mono-centric retrospective comparative study. Local Reg Anesth. 2022;15:97–105. PMID: 36601486; PMCID: PMC9807124. doi:10.2147/LRA.S383601
44. Goffin P, Lecoq JP, Ninane V, et al. Interfascial spread of injectate after adductor canal injection in fresh human cadavers. Anesth Analg. 2016;123(2):501–503. PMID: 27442773. doi:10.1213/ANE.0000000000001441
45. Monaco F, Coluccia S, Cuomo A, et al. Bibliometric and visual analysis of the scientific literature on percutaneous electrical nerve stimulation (PENS) for pain treatment. Appl Sci. 2023;13:636. doi:10.3390/app13010636
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
