Back to Journals » Infection and Drug Resistance » Volume 16
The Safety and Efficacy of Prolonged Use of Bedaquiline for the Treatment of Patients with Pulmonary Multi-Drug Resistant/Rifampin-Resistant Tuberculosis: A Prospective, Cohort Study in China
Authors Ke H, Gui X, Sun W, Zhang S, Yang Y, Zhang Z, Fan L
Received 4 May 2023
Accepted for publication 20 July 2023
Published 7 August 2023 Volume 2023:16 Pages 5055—5064
DOI https://doi.org/10.2147/IDR.S419996
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Hui Ke,* Xuwei Gui,* Wenwen Sun, Shaojun Zhang, Yan Yang, Zhemin Zhang, Lin Fan
Department of Tuberculosis, Shanghai Pulmonary Hospital, Tongji University School of Medicine, Shanghai Clinic and Research Center of Tuberculosis, Shanghai Key Laboratory of Tuberculosis, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Lin Fan; Zhemin Zhang, Email [email protected]; [email protected]
Objective: To evaluate the safety, tolerability, and efficacy of prolonged bedaquiline (Bdq) treatment in patients with multi-drug/rifampin-resistant tuberculosis (MDR/RR-TB).
Methods: This prospective cohort study was performed from August 2018 to August 2021. Patients diagnosed with MDR/RR-TB who met the inclusion criteria were prospectively included. Patients were treated with individual regimens of 18– 20 months containing Bdq for six months or a prolonged course of nine or 12 months according to treatment demands, and the efficacy and safety with a different course of Bdq-containing regimens were compared and evaluated.
Results: A total of 159 MDR/RR-TB patients were included in the study, including 96 cases with six months of Bdq, 50 cases with nine months of Bdq, and 13 patients with 12 months of Bdq. The treatment success rates were 89.6%, 90%, and 84.6% in Bdq at six months, nine months, and 12 months, respectively, which were not statistically different (P = 0.85). The main adverse events (AEs) were anemia, thrombocytopenia, and liver dysfunction in all patients, with no significant difference among the three groups. Patients who had fewer drugs chosen, disseminated lesions or lesions that were slowly absorbed, and severe cavities were the common reasons for prolonged use of Bdq.
Conclusion: Prolonged course use of Bdq from six months to 12 months clinically proved to be safe and efficient, and patients with severe or disseminated lesions had the chance to prolong the use of Bdq for more than six months to achieve optimal treatment outcomes.
Keywords: bedaquiline, prolonged course, MDR-TB, RR-TB, safety
Introduction
The treatment of Multidrug-resistant Tuberculosis (MDR-TB) and Rifampin-resistant TB is challenging for TB control due to poor treatment outcomes, poor patient compliance, difficult management, more adverse events (AEs), high costs, and a lengthy period of treatment. In recent ten years, WHO reported that the average treatment success for MDR-TB worldwide was 50–60%,1–3 which was slowly improved. However, studies in different countries have reported varying treatment success rates, including a 63.5% success rate in Sudan,4 64.7% in cured and 13.9% in completed treatment in a study from Africa,5 78% of successful treatment outcomes in children from a meta-analysis,6 60% of the overall success rate in Brazil,7 and only a 38.6% success rate reported by one study in India.8 The reason for varied treatment success rates was in many ways, including differences in public policy, management, economics, health treatment ability, and patient compliance.
With the advancement of clinical studies in recent years, shorter regimens have become the main treatment direction owing to their many advantages, including fewer adverse events, better tolerance and compliance, and lower cost for patients.9 Bedaquiline (Bdq), a diarylquinoline compound with a novel mechanism against Mycobacterium tuberculosis (Mtb), has proven to be efficient and safe for the treatment of MDR/RR-TB, such as Nix-TB10 and Ze-Nix-TB.11 Numerous studies have proven its efficacy and safety through concomitant treatment with delamanid (Dlm) and other core drugs,12,13 and some short-course regimen studies.14 However, all studies refer to the duration of Bdq for six months, and only a few cases have reported prolonged use of Bdq in the treatment of MDR-TB in children or individual adults,15–17 the main adverse side effect of Bdq is QTc prolongation;18 therefore, to date, there have been no reports with large samples to prove the safety and efficacy of prolonged use of Bdq and the clinical factors associated with the need for prolonged use of Bdq in the treatment of MDR/RR-TB. The present study aimed to observe the efficacy and safety of a prolonged course of Bdq from common six months to nine months and twelve months in a real-world study.
Patients and Methods
Study Design and Patients
The study was designed as a prospective cohort study to observe the efficacy and safety of prolonged use of Bdq for more than six months in the treatment of patients with MDR/RR-TB, who were prospectively included from August 20, 2018, to June 30, 2021, receiving Bdq-containing regimens. The present study complies with the Declaration of Helsinki. Ethical approval was obtained from the Institutional Review Board of Shanghai Pulmonary Hospital (number:114JH) and informed consent was obtained from each patient.
The inclusion criteria were as follows: 1) patients diagnosed with MDR/RR-TB confirmed by sputum culture and drug susceptibility tests (DST) or Xpert MTB/RIF; 2) patients treated with regimens containing BDQ; and 3) patients who consented to participate in the study and signed the consent form.
The exclusion criteria were as follows: 1) patients who were culture-positive and identified as non-tuberculosis mycobacterium (NTM) one or more times and 2) patients who did not receive Bdq-containing regimens due to contraindications such as heart diseases, drug allergies, significant electrocardiographic abnormalities, or other reasons.
Removing criteria was those Patients who took the regimen containing Bdq at the initial stage of the treatment course but then discontinued the use of Bdq owing to AEs or other reasons were excluded.
Treatment Regimens
The treatment regimens of all patients were uniformly prepared by specialists in TB from Shanghai Pulmonary Hospital and managed by the Shanghai Municipal Center for Disease Control and Prevention (CDC). The regimens were prepared according to the WHO and Chinese guidelines,19,20 and individualized longer treatment regimens with a duration of 18–20 months were designed based on previous histories of anti-TB treatment and DST results. Bdq was administered for six to twelve months (loading dose, 400 mg once a day for the initial 2 weeks, followed by 200 mg three times a week for the remaining weeks). The background regimens consisted of at least four drugs in the intensive phase: fluoroquinolones (FQs) (levofloxacin, Lfx, moxifloxacin, Mfx), clofazimine (Cfz), linezolid (Lzd), cycloserine (Cs), injectable agents (amikacin, Ak), protionamide (Pto), ethambutol (EMB), pyrazinamide (PZA), or para-aminosalicylic (PAS). If Bdq needed to be prolonged, a specialist group organized by the hospital was consulted. The duration of Bdq had a common six months and prolonged use of nine months and 12 months.
Treatment Evaluation
During the course of treatment, imaging evaluation was performed using Chest CT and sputum culture, and the treatment outcomes included cure, treatment completion, treatment failure, defaults, and death according to WHO definitions,20,21 treatment success was combined with cure and treatment completion. “Cure” is a patient who complete treatment with consistently at least three negative culture results for the final 12 months of the treatment course and without treatment failure; “Completed treatment” is a patient who complete the treatment according to the regimen but did not complete the requirement for bacteriological results; “Treatment failure” is referred as a patient who had sputum culture positive in the final 12 months of the treatment course or if any one of the final three cultures was positive; “died” is a patient died from any reason during the treatment for MDR/RR-TB; “Defaulted” is defined as patients whose TB treatment is interrupted for at least two consecutive months for any reason. The favorable outcome included “cure” and “treatment completion”, and unfavorable outcome included “failure”, “default” and “died.”
According to TB treatment history, patients could be classified into newly diagnosed cases (patients who had never been treated for TB or had taken anti-TB medicines for less than one month) and re-treated cases (patients who had previously received anti-TB chemotherapy more than once a month). AEs were evaluated using laboratory-monitored parameters (leukopenia, liver function, renal function) and electrocardiography (QTcF interval prolongation). Significant QTcF interval prolongation was defined as any QTcF interval value ≥500 ms or any increase in QTcF interval value >60 ms from the baseline.22
MDR-TB, pre-XDR-TB, and XDR-TB were defined according to WHO guideline version 2019.20 During treatment, several situations concerning adjustment of the regimens and observation of lesion absorption were as follows: limited effective drugs in regimens, extensive lesions, extensive lesions slowly absorbed, and severe cavitary lesions. Limited effective drugs in regimens indicated in the present study were referred to patients with a regimen of less than three effective drugs due to resistance or intolerance due to adverse effects in regimens; extensive lesions were referred to patients with radiological extensive lesions ≥ lung fields of tuberculous lesions; extensive lesions slowly absorbed were referred to a patient with extensive lesions absorbed slowly during the treatment containing BDQ, which were evaluated by at least two chief physician on MDR/RR-TB treatment; severe cavitary lesions were referred to a patient with lesions having ≥3 cavities or any one cavity ≥3 cm in diameter, which was consistent with the definition in our previous studies.23,24
Mycobacterium tuberculosis (MTB) Culture and Drug Susceptibility Test
All included patients were mycobacterium culture positive and identified as MTB or Xpert MTB/RIF positive and RFP resistant (Cepheid, USA), BACTEC MGIT 960 culture was performed according to the manufactory instruction, and the positive MTB of isolates was performed drug susceptibility test (DST) by MIC (Minimum Inhibitory Concentration), MIC DST was performed using MycoTB system (MYCOTB; Trek Diagnostic Systems, Thermo Fisher Scientific Inc., USA).25,26
Quality Control in Clinical Treatment and Follow Up
Quality control was performed by the quality control group organized by the department and hospital, including the regimens made, handling the AEs during the treatment, patients’ re-tuned visits, and follow-up according to the plan of the requirement during the present observational study. Patients were required to return to the outpatient department at least once a month.
Statistical Analysis
Quantitative variables are expressed as Median and Interquartile range and compared using Wilcoxon Test and Kruskal–Wallis test. Qualitative data were expressed as numbers and percentages and were evaluated using Kruskal–Wallis H-test. Statistical analyses were performed using SPSS version 26.0 (SPSS, IL, USA), and statistical significance was set at p<0.05.
Results
Clinical Characteristics of Patients with MDR/RR-TB
A total of 163 patients diagnosed with pulmonary MDR/RR-TB met the inclusion criteria, among which three cases were excluded because of cessation of treatment due to social reasons, one case was excluded for lost follow-up within 1 month after starting the treatment, and 159 cases were included in the study. After the follow-up, there were 96 patients treated with Bdq containing regimens with Bdq use for six months, 50 patients were treated with Bdq containing regimens with Bdq use for nine months, 13 patients were treated with Bdq containing regimens with Bdq used for twelve months, the information was shown in the flow diagram (see Figure 1).
 |
Figure 1 Flow diagram of included patients. |
For all included patients, the mean age was 38.99 ± 14.19; 113 cases (71.1%) were male and 46 cases were female, 120 (75.5%) cases were re-treated, 43 (27%) patients were MDR-TB, 71 (44.7%) cases were Pre-XDR-TB with FQs resistance, 2 (1.3%) cases were Pre-XDR-TB with injectable agent resistance, 35 (22%) cases were XDR-TB, and the rest 8 (5%) cases were RR-TB but excluded MDR/XDR and Pre-XDR-TB. Twenty-eight (17.6%) patients had comorbidities of diabetes, and 43 patients had coexisting extra-pulmonary TB, including Pleural TB (11 cases), lymph node TB (2 cases), bronchial tuberculosis (27 cases), tuberculosis meningitis (1 case), and bone tuberculosis (1 case). The detailed baseline characteristics of the included patients are presented in Table 1
 |
Table 1 Clinical Characteristics of Patients with MDR/RR-TB (n = 159) |
Compared Clinical Characteristics Among Patients with BDQ Use for Six Months, Nine Months, and Twelve Months
After follow-up of all the treatment courses for 159 cases of MDR/RR-TB, we observed that only 60.37% of patients (96 cases) were treated with Bdq for six months, and the remaining patients had prolonged Bdq use for nine months (31.45%, 50 cases) and 12 months (8.18%, 13 cases).
By comparing the clinical characteristics, we found the common factors such as sex, newly or re-treated, hypoproteinemia, lower BMI, anemia, and extra-pulmonary TB, and final treatment success rate were even distributed among three groups (p > 0.05), the detailed information is shown in Table 2.
 |
Table 2 Compared Clinical Factors Among Regimens Containing Bdq for Different Times |
Clinical Factors Correlated with Prolonged Use of BDQ
There were 96 patients with Bdq use for six months and 63 with prolonged Bdq use for 9–12 months after treatment. Several clinical factors, including new or retreated, having limited effective drugs in regimens, extrapulmonary TB or not, co-existing DM or not, were compared between Bdq use for six months and prolonged use for 9–12 months. Results showed that patients with limited effective drugs in regimens were greatly more common in prolonged use of Bdq with 9–12 months and three times higher than those with the regular course of Bdq with six months (OR 95% CI was 3, 2.38–3.78); patients evaluated by extensive lesions and absorb slowly were also greatly more common in the use of Bdq with 9–12 months and 4 times higher than those with the regular course of Bdq for six months (OR 95% CI was 4.43, 3.20–6.14), p values of above two factors were both p < 0.001; patients with an extensive lesion or severe cavitary lesions were slightly more common in prolonged use of Bdq with 9–12 months, 0.23 times and 0.35 times higher than those with the regular course of Bdq for six months (OR 95% CI was 0.23, 0.11–0.48, 0.35, 0.18–0.69, respectively); other factors such as DM and extra-pulmonary TB were not found to be related with Bdq prolonged course use, p values had no statistical significance. The detailed information is presented in Table 3 and Figure 2A–H.
 |
Table 3 Clinical Factors with Correlations of Prolonged Use of BDQ |
The Safety of BDQ for Six Months and Prolonged Use for 9–12 Months
159 cases were observed to finish all the treatment courses, no severe adverse events occurred for all cases, a total of 252 person-times adverse effects occurred, including 123 person-times in 96 cases of patients with six months of Bdq, 102 person-timers of AEs in 50 cases with Bdq use for nine months, 26 person-times of AEs in 13 cases with Bdq use for twelve months. The most frequent adverse events were thrombocytopenia, liver dysfunction, and renal dysfunction in patients with Bdq 6 months, anemia, thrombocytopenia, and liver dysfunction in patients with Bdq use for 9 months, anemia, renal dysfunction and diminution of vision in patients with Bdq use for 12 months. A total of 59 person-times of QTc prolongation occurred, including 56 patients who had QTc >450 ms but <500 ms; the proportion of QT-c prolonged occurrences among the three groups was not statistically significant (P = 0.71). Each group had one patient with a QTc >500ms (P = 0.42), and bedaquiline was discontinued and continued to be used when QTc in the electrocardiogram returned to normal. Generally, patients were safe in whatever use Bdq for six months, nine months, or twelve months, and the detailed information is shown in Table 4.
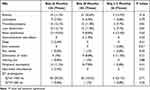 |
Table 4 Adverse Effects Among Regimens Containing Bdq for Different Times |
Discussion
Bdq has been listed as a Group A drug for the treatment of MDR/RR-TB and has been proven to be safe and efficient for patients and special groups, such as HIV-infected or children with TB,27–30 however, almost all the studies used Bdq with the standard dosing regimens of six months. The use of Bdq was faced with the issues of prolonged duration concerning the safety, efficacy, and indications. In areas with a high TB burden, many patients with refractory MDR/RR-TB have difficult clinical situations, including a limited number of effective drug alternatives or tolerances due to severe drug resistance, poor tolerance or severe AEs, severely destroyed lesions in both lungs, and severe comorbidities. These patients face a serious challenge in achieving optimal clinical treatment outcomes.
To observe the above treatment situation for patients with MDR/RR-TB, we conducted this real-world study to optimize treatment outcomes and explore the safety and efficacy of prolonged use of Bdq. Table 1 shows that the cure rate was 53.46% (85/159) and completed treatment was 35.85% (57/159); the total success rate was 89.31%, indicating that Bdq-containing regimens had a high success rate of treatment for six months, nine months and 12 months, confirming its high efficacy with the prolonged use of Bdq since there was no statistical difference among patients with Bdq for six months, nine months and 12 months, as shown in Table 2. The reason that patients needed to prolong six months of Bdq, we compared the underlying clinical factors between two groups of common six months and prolonged duration of 9–12 months of Bdq, the results showed that limited effective drugs in regimens, extensive lesions, extensive lesions absorbed slowly and severe cavity were the main four clinical factors resulting in prolonged use of Bdq. Limited effective drugs in regimens are usually due to patients experiencing AEs, such as allergy, drug-induced liver injury, renal dysfunction, and severe drug-resistant status, such as XDR-TB resistant to most second-line anti-TB drugs. For the treatment of these patients, the effective drugs were likely to turn less, such as two drugs, if Bdq was stopped after six months of treatment. As for how many drugs in the regimens should be effective for MDR/RR-TB, previous guidelines suggested that at least four effective drugs31,32 should be made; however, it is difficult to make effective regimens when patients have limited drugs selected, and Bdq is more likely to be prolonged under these conditions. A recent study showed that the addition of novel anti-TB drugs such as delamanid, a regimen comprising three drugs, was likely to be effective,33 but this has been based on the premise that novel-anti-TB drugs are involved when lesions are disseminated and severe, such as severe cavities, meaning more bacterial load in the lesions, severe lesions absorbed slowly, and the second phase in the regimens after stopping Bdq appears to be not strong enough to obtain the ideal treatment outcome. The second reason was that patients enrolled in the present study comprised the majority of previously treated patients, most of whom had a complicated history of anti-TB treatment and were more likely to be limited in selecting effective drugs. The recently published clinical trials included shorter regimens such as Nix-TB regimens, Ze-Nix-TB regimens, and BPaLMfx,11,34,35 which have a common characteristic of containing two novel drugs, Bdq and Pretomanid, which proved to be highly effective against MTB and had excellent evidence in clinical trials.36–38 However, in areas with limited sources, a lack of novel drugs might result in making the traditional longer regimens or selecting at least four effective drugs in the regimens to ensure a favorable outcome. Prolonged use of Bdq is likely to occur when Bdq is only one kind of novel anti-TB drug in the regimens in the current clinics, especially in areas or countries with high TB burden.
/The other three clinical factors, extensive lesions, extensive lesions absorbed slowly, and severe cavitary lesions, which indicate the severity of radiographic lesions and high bacterial burden in the lung, are more likely to have poor outcomes.39,40
The results of the present study showed that prolonged use of Bdq from six months to 12 months resulted in a highly efficient treatment outcome. The most important point was the similar safety for prolonged Bdq of 6–12 months as that for patients with Bdq of 6 months, as shown in Table 4. We can see that QTcF >450 ms was slightly higher in patients with Bdq for 12 months than Bdq for 6 and 9 months but had no statistical difference, while other types of AEs had no statistical differences among Bdq for 6 months, 9 months, and 12 months, and almost all AEs were similar in the occurrence rate among patients with six months, nine months and 12 months of Bdq use, implying that prolonged use of Bdq from 6 months to 12 months was safe for patients.
The present study has two limitations. First, the use of prolonged Bdq had some subjective judgment by physicians. Second, there was a lack of therapeutic drug monitoring (TDM) of Bdq during the administration of the regimens, which could guide the optimal duration and dose of drugs. The present study had limited conditions for Bdq TDM in the hospital, which should be investigated further in future studies.
In conclusion, in clinics, an increasing number of cases need to prolong the use of Bdq, which has been proven to be safe and efficient when administered from 9 months to 12 months, severe lesions, severe lesions absorbed slowly, less effective drugs in the regimens, and severe cavity in the lesions are common clinical factors that prolong the use of Bdq.
Ethical Approval and Consent to Participate
The study complies with the Declaration of Helsinki, which was approved by the Ethics Committee of Shanghai Pulmonary Hospital, Tongji University School of Medicine (approval number: 114JH). Written informed consent was obtained from all the included participants.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the National Natural Science Foundation of China (82170006), Shanghai Science and Technology Committee Fund (21Y11901000, 20ZR1446700), and Clinical Research Foundation of Shanghai Pulmonary Hospital (FKLY20017, SKPY2021003). The authors declare that they have no conflicts of interest. We confirmed that the information in the funding statement was accurate and met the requirements of the funder.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. World Health Organization. Global tuberculosis report 2014. Geneva: World Health Organization. 2014. Available from: www.who.int/about/licensing/copyright_form/en/index.html.
2. World Health Organization. Global tuberculosis report 2017. Licence: CC BY-NCSA 30 IGO. Geneva: World Health Organization; 2017.
3. World Health Organization. Global tuberculosis report 2022. License: CC BY-NC-SA 3.0 IGO. Geneva: World Health Organization; 2022.
4. Ali M, Alrasheedy A, Kibuule D, Godman B, Hassali M, Ali H. Assessment of multidrug-resistant tuberculosis (MDR-TB) treatment outcomes in Sudan; findings and implications. Expert Rev Anti Infect Ther. 2019;17(11):927–937. doi:10.1080/14787210.2019.1689818
5. Meressa D, Hurtado R, Andrews J, et al. Achieving high treatment success for multidrug-resistant TB in Africa: initiation and scale-up of MDR TB care in Ethiopia--an observational cohort study. Thorax. 2015;70(12):1181–1188. doi:10.1136/thoraxjnl-2015-207374
6. Harausz E, Garcia-Prats A, Law S, et al. Treatment and outcomes in children with multidrug-resistant tuberculosis: a systematic review and individual patient data meta-analysis. PLoS Med. 2018;15(7):e1002591. doi:10.1371/journal.pmed.1002591
7. Bastos ML, Cosme LB, Fregona G, Prado TND, Maciel ELN. Treatment outcomes of MDR-tuberculosis patients in Brazil: a retrospective cohort analysis. BMC Infect Dis. 2017;17(1):718. doi:10.1186/s12879-017-2810-1
8. Patel S, Nimavat K, Alpesh P, et al. Treatment outcome among cases of multidrug-resistant tuberculosis (MDR TB) in Western India: a prospective study. J Infect Public Health. 2016;9(4):478–484. doi:10.1016/j.jiph.2015.11.011
9. Trubnikov HA, Akopyan K, Ciobanu A, et al. Effectiveness and safety of a shorter treatment regimen in a setting with a high burden of multidrug-resistant tuberculosis. Int J Environ Res Public Health. 2021;18(8):4121. doi:10.3390/ijerph18084121
10. Nimmo C, Naidoo K, O’Donnell M. Treatment of highly drug-resistant pulmonary tuberculosis. N Engl J Med. 2020;382(24):2376–2377.
11. Nyang’wa B-T, Berry C, Kazounis E, et al. A 24-week, all-oral regimen for rifampin-resistant tuberculosis. N Engl J Med. 2022;387(25):2331–2343. doi:10.1056/NEJMoa2117166
12. Huerga H, Khan U, Bastard M, et al. Safety and effectiveness outcomes from a 14-country cohort of patients with multi-drug resistant tuberculosis treated concomitantly with bedaquiline, delamanid, and other second-line drugs. Clin Infect Dis. 2022;75(8):1307–1314. doi:10.1093/cid/ciac176
13. Hewison C, Khan U, Bastard M, et al. Safety of treatment regimens containing bedaquiline and delamanid in the endTB cohort. Clin Infect Dis. 2022;75(6):1006–1013. doi:10.1093/cid/ciac019
14. Nguyen T, Le T, Merle C, et al. Effectiveness and safety of bedaquiline-based, modified all-oral 9–11-month treatment regimen for rifampicin-resistant tuberculosis in Vietnam. Int J Infect Dis. 2023;126:148–154. doi:10.1016/j.ijid.2022.11.007
15. Gubkina M, Khokhlova J, Yukhimenko N, Petrakova I. Prolonged use of bedaquiline in the treatment for MDR-TB in a child. IDCases. 2021;26:e01311. doi:10.1016/j.idcr.2021.e01311
16. Lewis J, Hine P, Walker J, et al. First experience of effectiveness and safety of bedaquiline for 18 months within an optimized regimen for XDR-TB. Eur Respir J. 2016;47(5):1581–1584. doi:10.1183/13993003.01980-2015
17. Gao J, Xie L, Ma L, et al. Prolonged use of bedaquiline in two patients with pulmonary extensively drug-resistant tuberculosis: two case reports. World J Clin Cases. 2021;9(10):2326–2333. doi:10.12998/wjcc.v9.i10.2326
18. Darmayani I, Ascobat P, Instiaty I, Sugiri Y, Sawitri N. Bedaquiline effect on QT interval of drugs-resistant tuberculosis patients: real world data. Acta Med Indones. 2022;54(3):389–396. doi:10.1093/cid/ciz914
19. Association Ca-T. Chemotherapy guidelines on drug-resistant tuberculosis. Chin Anti TB J. 2019;2019(5):421–469.
20. World Health Organization. WHO Consolidated Guidelines on Drug-Resistant Tuberculosis Treatment. Geneva: world health organization; 2019.
21. World Health Organization. Definitions and reporting framework for tuberculosis–2013 revision: updated December 2014 and January 2020. Licence: CC BY-NC-SA 3.0 IGO. Geneva: World Health Organization. 2013.
22. Guideline IH. Clinical safety data management: definitions and standards for expedited reporting E2A.
23. Fan L, Xiao H, Mai G, Su B, Ernst J. tuberculosis antigen-specific IFN-γ response without IL-17 enhancement in patients with severe cavitary pulmonary tuberculosis. PLoS One. 2015;10(5):e0127087. doi:10.1371/journal.pone.0127087
24. Fan L, Shen H, Huang H, Yang R, Yao L. Impairment of Wnt/β-catenin signaling in blood cells of patients with severe cavitary pulmonary tuberculosis. PLoS One. 2017;12(3):e0172549. doi:10.1371/journal.pone.0172549
25. Yu X, Ma Y, Jiang G, Chen S, Wang G, Huang H. Sensititre® MYCOTB MIC plate for drug susceptibility testing of Mycobacterium tuberculosis complex isolates. Int J Tuberc Lung Dis. 2016;20(3):329–334. doi:10.5588/ijtld.15.0573
26. Lee J, Armstrong D, Ssengooba W, et al. Sensititre MYCOTB MIC plate for testing Mycobacterium tuberculosis susceptibility to first- and second-line drugs. Antimicrob Agents Chemother. 2014;58(1):11–18. doi:10.1128/AAC.01209-13
27. Mase S, Chorba T, Parks S, et al. Bedaquiline for the treatment of multidrug-resistant tuberculosis in the United States. Clin Infect Dis. 2020;71(4):1010–1016.
28. Govender T, Jham M, Zhang J, et al. Decentralized, integrated treatment of RR/MDR-TB and HIV using a bedaquiline-based, short-course regimen is effective and associated with improved HIV disease control. J Acquir Immune Defic Syndr. 2023;92(5):385–392. doi:10.1097/QAI.0000000000003150
29. Pai H, Ndjeka N, Mbuagbaw L, et al. Bedaquiline safety, efficacy, utilization and the emergence of resistance following treatment of multidrug-resistant tuberculosis patients in South Africa: a retrospective cohort analysis. BMC Infect Dis. 2022;22(1):870. doi:10.1186/s12879-022-07861-x
30. Hughes J, Solans B, Draper H, et al. Pharmacokinetics and safety of bedaquiline in Human Immunodeficiency Virus (HIV)-positive and negative older children and adolescents with rifampicin-resistant tuberculosis. Clin Infect Dis. 2022;75(10):1772–1780. doi:10.1093/cid/ciac252
31. World Health Organization. WHO treatment guidelines for drug-resistant Tuberculosis 2016 updates; 2016. Geneva: World Health Organization. Available from: wwwhoint/tb/areas-of-work/drug-resistant-tb/treatment/resources/.
32. World Health Organization. Companion Handbook to the WHO Guidelines for the Programmatic Management of Drug-Resistant Tuberculosis. Geneva: World Health Organization; 2014.
33. Rodriguez C, Lodi S, Horsburgh C, et al. Comparative effectiveness of adding delamanid to a multidrug-resistant tuberculosis regimen comprised of three drugs likely to be effective. PLOS Global Public Health. 2023;3(4):e0000818. doi:10.1371/journal.pgph.0000818
34. Conradie F, Diacon A, Ngubane N, et al. Treatment of highly drug-resistant pulmonary tuberculosis. N Engl J Med. 2020;382(10):893–902. doi:10.1056/NEJMoa1901814
35. Conradie F, Bagdasaryan TR, Borisov S, et al. Bedaquiline–pretomanid–linezolid regimens for drug-resistant tuberculosis. N Engl J Med. 2022;387(9):810–823. doi:10.1056/NEJMoa2119430
36. Li S, Converse P, Betoudji F, et al. Next-generation diarylquinolines improve sterilizing activity of regimens with pretomanid and the novel oxazolidinone TBI-223 in a mouse tuberculosis model. Antimicrob Agents Chemother. 2023;67(4):e0003523. doi:10.1128/aac.00035-23
37. Solans B, Imperial M, Olugbosi M, Savic R. Analysis of dynamic efficacy endpoints of the Nix-TB trial. Clin Infect Dis. 2023;76:1903–1910. doi:10.1093/cid/ciad051
38. Dooley K, Hendricks B, Gupte N, et al. Assessing Pretomanid for Tuberculosis (APT), a randomized phase 2 trial of pretomanid-containing regimens for drug-sensitive tuberculosis: 12-week results. Am J Respir Crit Care Med. 2023;207(7):929–935. doi:10.1164/rccm.202208-1475OC
39. Htun Y, Khaing T, Aung N, et al. Delay in treatment initiation and treatment outcomes among adult patients with multidrug-resistant tuberculosis at YangonRegional Tuberculosis Centre, Myanmar: a retrospective study. PLoS One. 2018;13(12):e0209932. doi:10.1371/journal.pone.0209932
40. Hicks R, Padayatchi N, Shah N, et al. Malnutrition associated with unfavorable outcome and death among South African MDR-TB and HIV co-infected children. Int J Tuberc Lung Dis. 2014;18(9):1074–1083. doi:10.5588/ijtld.14.0231
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

