Back to Journals » Orthopedic Research and Reviews » Volume 11
The role of joint distraction in the treatment of knee osteoarthritis: a systematic review and quantitative analysis
Authors Goh EL , Lou WCN, Chidambaram S, Ma S
Received 4 April 2019
Accepted for publication 10 July 2019
Published 7 August 2019 Volume 2019:11 Pages 79—92
DOI https://doi.org/10.2147/ORR.S211060
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
En Lin Goh,1 Winston Choong Ngan Lou,2 Swathikan Chidambaram,1 Shaocheng Ma3
1Oxford University Clinical Academic Graduate School, Medical Sciences Division, University of Oxford, Oxford, UK; 2Faculty of Medicine, Imperial College London, London, UK; 3City and Guilds Building, Imperial College London, London, UK
Introduction: Knee osteoarthritis is a major cause of pain and disability for which joint distraction is a potential treatment to delay the need for knee arthroplasty. This systematic review aims to assess the short- and long-term clinical and structural outcomes following knee joint distraction (KJD).
Methods: MEDLINE, EMBASE, Scopus, and Web of Science databases were searched from the date of inception to 26th June 2019. Clinical studies investigating joint distraction for knee osteoarthritis with outcomes including ∆WOMAC index, ∆VAS pain score, and ∆joint space width were included. The review protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) – CRD42018087032.
Results: Nine studies comprising a total of 507 patients were included. There were four randomized controlled trials (RCTs), five open prospective cohort studies, and one case series. Overall, there were significant improvements in WOMAC index, VAS pain score and joint space width following KJD, which persisted up to 9 years. KJD also demonstrated comparable clinical outcomes with high tibial osteotomy and total knee arthroplasty.
Conclusion: There is moderate quality evidence supporting the beneficial outcomes of joint distraction for knee osteoarthritis. Larger RCTs with longer follow-up (>1 year) are necessary to establish the true effect size of this procedure.
Keywords: osteoarthritis, knee joint distraction, total knee arthroplasty, high tibial osteotomy, clinical outcomes, structural outcomes
Introduction
Osteoarthritis is the most prevalent chronic joint condition worldwide, affecting 10% of the individuals over the age of 60 years.1 This disorder is characterized by articular cartilage destruction, synovial membrane inflammation, and subchondral bone remodeling.2 Knee osteoarthritis forms the largest proportion of all cases of osteoarthritis, causing significant pain and disability.3 Treatment aims to alleviate pain and stiffness as well as maintain function, with current consensus guidelines recommending the use of a combination of conservative measures including physical therapy, analgesia, and surgical interventions such as arthroplasty.1 Nonetheless, there remains a lack of treatments available that are effective at stopping or reversing this disease.4
Knee arthroplasty is effective in the treatment of osteoarthritis in patients in whom optimal conservative treatment is inadequate. Consequently, there has been a rise in the number of procedures performed annually, with over 40% of all procedures and 44% of the revisions performed in individuals under the age of 65 years.5 However, there is a higher risk of failure in younger patients as a result of higher functional demands.6 The lifetime risk of revision surgery in men in their early 50s is estimated at 35%, with a median time to revision surgery of 4.08 years.7 In recent years, joint distraction has emerged as a potential treatment of knee osteoarthritis to delay knee arthroplasty. This surgical procedure aims to temporarily unload the joint cartilage by eliminating contact between the joint surfaces.8
Joint distraction has been utilized in the treatment of osteoarthritis of a variety of joints including the ankle, hip, and hand, with favorable outcomes.9–13 Studies focusing on knee joint distraction (KJD) in stopping and potentially reversing joint degeneration to delay knee arthroplasty in young patients have shown promise.14–19 However, it has been postulated that joint distraction could be detrimental to patients with osteoarthritis, as immobilization promotes cartilage degeneration.20 The evidence-base behind the use of this procedure remains limited by a small number of publications on the topic.
The aim of this systematic review is to assess the short- and long-term outcomes following KJD and compare this with currently available treatment modalities.
Methods
Literature search methods, inclusion and exclusion criteria, outcome measures, and statistical analysis were defined according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines. Ethical approval was not required as patients were not involved in the conception, design, analysis, drafting, interpretation, or revision of this research. The review protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) – CRD42018087032 and published.21
Electronic search
The following databases were searched: (a) MEDLINE in-process and other non-indexed citations (latest issue) via OvidSP, last search on 26th June 2019; (b) Ovid EMBASE (1974 to latest issue), last search 26th June 2019; and (c) Scopus, last search 26th June 2019; (d) Web of Science, last search 26th June 2019. Search terms used three strings, which were then linked by an AND modifier. The first string included: osteoarthritis OR osteoarthrosis OR degenerative joint disease; the second string: joint distraction; and the third string: knee. The search was broadened with the use of truncated search terms utilizing the wildcard character and the “related articles” function. Additionally, the references of included articles were hand-searched to identify any additional studies.
Study selection
All clinical studies investigating the use of joint distraction as a treatment for knee osteoarthritis were selected. Additionally, all included studies met the following criteria: (a) radiographic signs of joint damage and primarily tibiofemoral osteoarthritis; (b) no history of inflammatory or septic arthritis; (c) patients were under the age of 65 years; (d) valgus/varus malalignment of less than 10º; (e) reporting of at least the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Visual Analogue Scale (VAS), or joint space width (JSW) of the most affected compartment assessed as outcome measures of the effect of the treatment; and (f) full-length article published. Non-human studies, experimental trials, review articles, editorials, case reports, letters, conference abstracts, and unpublished studies were excluded.
Outcome measures
Outcomes assessed were: ∆WOMAC index, ∆VAS pain score, and ∆JSW of the most affected compartment. Other additional outcomes reported were also reviewed.
Data extraction
Two independent reviewers (E.L.G and S.C.) screened all the titles and abstracts for inclusion, both of whom were blinded to authors, journals, institutional affiliations, and dates of publication. Both reviewers evaluated each selected reference independently and summarized relevant study characteristics. In case of disagreement, a consensual decision between the two reviewers under involvement of a third independent reviewer (S.M.) was reached. The following data items were extracted: the year of publication, study design, sample size, country of study, type of patients, patient characteristics, outcome measures, and conclusions. Authors of the original publications were contacted in the event of insufficient data, but this was not the case in this analysis. Data were entered into Review Manager 5.3 (Cochrane Collaboration, Oxford, United Kingdom).
Quality assessment and risk of bias
The quality of the studies was assessed using the Modified Coleman Methodology Score. The risk of bias was evaluated using the Newcastle–Ottawa Scale (NOS) for observational studies and Cochrane Collaboration tool for randomized controlled trials (RCTs).22,23
Data synthesis and analysis
Descriptive statistics were calculated for variables of interest. Continuous measures were summarized with the use of means and standard deviations, while categorical data were summarized with the use of counts and percentages.
Results
Study characteristics
Nine studies comprising of four RCTs, five prospective cohort studies, and one case series published between 2007 and 2019 were included in this systematic review (Figure 1) (Table 1).14–19,24–26 The sample size of each study ranged from 6 to 138, giving rise to a total of 507 patients. The outcomes reported in four studies were based on follow-up of the same cohort of patients at 12, 24, 60, and 108 months.15,16,18 One study reported outcomes of two previous studies at 24 months.26 Patients under the age of 65 years underwent KJD following referral by an orthopedic surgeon, which was based on clinical examination (VAS for pain of ≥60 mm) and radiographic examination (primarily tibiofemoral cartilage tissue loss). All but one study utilized the distraction method proposed by Intema et al.14,15 Three studies used 6 weeks of continuous distraction, one study used 8– 12 weeks of continuous distraction and four studies used 8 weeks of intermittent distraction. One of the studies compared 6 weeks of continuous distraction with 8 weeks of intermittent distraction.17 There were two RCTs, one of which compared KJD with total knee arthroplasty (TKA), and the other which compared KJD with high tibial osteotomy (HTO).24,25
 |
Figure 1 Flow diagram illustrating screening and selection process. |
 |
Table 1 Study characteristics |
Quality assessment and risk of bias of included studies
The Modified Coleman Methodology Score was used to assess the quality of included studies (Table 2). The mean score for all included studies was 82.8 out of 100, with all studies scoring between 66 and 89. The areas identified as methodologically weak included study size, sampling and observational bias, and duration of follow-up. Four observational studies had a NOS score of 8/9, which was due to the lack comparison group, while one of the studies had a score of 9/9. Meanwhile, both RCTs were found to be at a high risk of performance and detector bias due to lack of blinding which is inherent to the nature of this treatment (Figure 2).
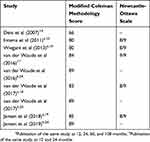 |
Table 2 Quality assessment using Modified Coleman Methodology Score and Newcastle–Ottawa Scale |
 |
Figure 2 Cochrane Collaboration tool assessing risk of bias. |
∆WOMAC index
Four studies reported on follow-up data of 20 patients who underwent KJD up to 9 years (Table 3).15,16,18,19 All patients reported a significant clinical improvement from baseline, which persisted for the 9-year period. This was noted by an increase in the WOMAC index from a baseline of 45–77 points (71%) at 1-year follow-up, 78 points (74%) at 2-year follow-up, 66 points (47%) at 5-year follow-up, and 75 points (67%). One RCT compared the outcomes following KJD and TKA in 56 patients.25,26 There significant improvements in the WOMAC index reported in both groups at 1-year follow-up with a rise of 30 points (60%) from a baseline of 50 points in the KJD group and 36 points (78%) from a baseline of 46 points in the TKA group. These persisted at 2-year follow-up at 29 points (58%) above baseline in the KJD group and 42 points (91%) above baseline in the TKA group. No significant difference was noted in change in the WOMAC index between the two groups at one and 2 years.
 |  |
 |
Table 3 Clinical and patient-reported outcome measures |
The outcomes following KJD and HTO were compared 69 patients in another RCT.24,26 In this study, the WOMAC index increased by 22 points (41%) from a baseline of 54 points in the KJD group and 38 points (73%) from a baseline of 52 points in the HTO group after 1 year, both of which were statistically significant. At 2 years, these changes were maintained at 25 points (46%) higher than the baseline in the KJD group and 29 points (55.6%) higher than baseline in the HTO group. There was no significant difference in the change in the WOMAC index between the KJD and HTO groups. Comparison of 8 weeks of intermittent distraction with 6 weeks of continuous distraction demonstrated a comparable increase in the WOMAC index of 24 points (57%) from a baseline of 42 points in the former and 32 points (62%) from a baseline of 52 points in the latter.17 Both changes were statistically significant.
∆VAS pain score
Significant improvements in the VAS pain scores were observed following KJD, which were sustained up to 9 years (Table 3).15,16,18 At 1-year follow-up following KJD, there was a decrease in the VAS pain score by 42 mm (58%) from a baseline of 73 mm, which was sustained at 2-year follow-up, where the VAS pain score was 45 mm (61%) lower than the baseline. Compared to the baseline, the VAS pain score was 28 mm (38%) lower at 5-year follow-up and 47 mm (64%) lower at 9-year follow-up. In the case series, there was a significant improvement in the VAS pain score of 50 mm (56%) from a baseline of 90–40 mm.14 In the RCT comparing KJD with TKA, a significant decrease in the VAS pain score of 53 mm (75%) from a baseline of 71 mm was reported after 1 year in the KJD group.25 A significant, albeit marginally smaller decrease of 36 mm (55%) from a baseline of 65 mm was noted in the TKA group. There was no statistical difference in the ∆VAS pain score between both groups. After 2 years, the VAS pain score was 32 mm (45%) lower than baseline in the KJD group and 56 mm (86%) lower than baseline in the TKA group. This difference was statistically significant.
In the RCT comparing KJD with HTO, there was a significant reduction in VAS pain score of 19 mm (35%) from a baseline of 55 mm at 1 year.24 HTO was associated with a significant reduction in VAS pain score of 38 mm (58%) from a baseline of 65 mm. A statistically significant difference was present between both groups. At 2 years, the VAS pain score was 21 mm (39%) below baseline in the KJD group and 39 mm (59%) below baseline in the HTO group. No statistical difference was found between the two groups. Following 8 weeks of intermittent distraction, the VAS pain score decreased significantly by 43 mm (58%) from a baseline of 74 mm after 1 year of follow-up. In contrast, there was a significant decrease of 23 mm (38%) from a baseline of 60 mm after 6 weeks of continuous distraction.17 The difference between the two groups was statistically significant after 1 year.
∆JSW of the most affected compartment
There was a significant increase of 0.9 mm (33%) from a baseline of 2.7 mm in the JSW of the most affected compartment at 1-year follow-up (Table 4). At 2-, 5-, and 7-years follow-up, the JSW was 0.5 mm (19%), 0.3 mm (11%), and 0.3 mm (11%) greater than at the baseline, although these were not statistically significant.15,16,18,19 In the RCT comparing KJD to TKA, a significant increase of 1.3 mm (68%) in the JSW of the most affected compartment was noted 1 year after KJD.25 This was maintained after 2 years at 1.0 mm (59%) above baseline.26 In the case series, there was a significant increase of 1.1 mm (275%) from a baseline of 0.4 mm in the JSW of the most affected compartment.14
 |
Table 4 Structural parameters |
In the RCT comparing KJD to HTO, KJD was associated with a significant increase in JSW of 0.8 mm (40%) at 1 year, which persisted at 2 years.24,26 In contrast, the HTO group demonstrated a smaller, albeit statistically significant increase of 0.4 mm (20%). After 2 years, the JSW in the HTO group was 0.6 mm (30%) above baseline. There was no significant difference between the change in JSW between the two groups. There were significant increases in the JSW after 8 and 6 weeks of distraction of 0.9 mm (35%) and 1.1 mm (61%) respectively, although no difference was present between the two groups.
Complications
Pin-tract infections were the most frequently reported complication associated with KJD in all studies. Two (10%) cases of pulmonary embolism were documented in the KJD group. There were two (4.4%) cases of post-operative wound infection following HTO. TKA was associated with five (12.5%) cases of postoperative stiffness and one (2.5%) case of myocardial infarction.
Discussion
The present systematic review provides a summary of the short-term outcomes of KJD compared to TKA and HTO as well as the long-term outcomes up to 9 years. In this review, the clinical and structural benefits of KJD were sustained till 9 years. KJD demonstrated similar outcomes with current surgical techniques such as TKA and HTO for the treatment of knee osteoarthritis. The KJD group demonstrated greater increase in JSW at 1 year although the HTO group experienced greater improvements in clinical outcomes, thereby suggesting lack of correlation between JSW and clinical outcome. In the Bristol ‘OA500ʹ study, Dieppe and colleagues followed-up 415 patients with osteoarthritis over 3 years, to monitor disease progression.27 The authors reported no correlation between structural joint changes and clinical outcome after 3 years.
Based on these findings, it is evident that KJD is slightly less effective than TKA in restoring function in the short term. Unlike TKA, KJD unloads the cartilage temporarily and this may have important implications on patient choice. van der Woude et al, note that patients were able to work during the distraction period, with most of them indicating that they would undergo the procedure again.24 It must be emphasized that there are different indications for each procedure; TKA is advocated in patients with loss of the native joint and demonstrates better results at older age, while HTO is typically performed in patients with unilateral osteoarthritis with leg axis deviation. Thus, KJD may prove to be a viable alternative in certain groups of patients by enabling all subsequent surgeries.
Three complications have been reported following KJD, of which pin-tract infections are the most common. These infections have a predilection for the femur, where the thick soft tissue layer allows pin mobility, thereby increasing the risk of infection.28,29 However, oral antibiotic therapy with flucloxacillin has been shown to be successful in treating these infections, and no cases of osteomyelitis have been documented.18 Pulmonary embolism was reported in a proportion of patients, which although non-fatal, necessitated anti-coagulant therapy for 6 months. Finally, one patient experienced limited flexion range following removal of the external fixator but this resolved within 1 year.18 Pin-tract infections associated with the external fixator remain a challenge in the implementation of KJD in clinical practice. These infections potentially complicate secondary prosthesis surgery although no such cases have been reported in the studies.30 Furthermore, Wiegant and colleagues present data supporting the safety of TKA following KJD.31 Nonetheless, these patients need close prospective monitoring and follow-up during the distraction period to ensure early identification and treatment of infection.
A mechanical component is likely involved in the underlying mechanism. Kajiwara and colleagues showed subchondral drilling, joint motion and distraction were associated with cartilage regeneration in rabbits.32 Additionally, Wiegant et al, postulate that intermittent fluid pressure changes during loading and unloading of the distracted joint may stimulate cartilage repair in their canine model.33 The downstream effects of joint distraction at the molecular level are currently being investigated further. Chen et al, showed that rats treated with KJD displayed less severe osteoarthritic lesions, significantly lower levels of interleukin-1ß and fewer chondrocytes positive for type X collagen and matrix metalloproteinase 13, thereby suggesting reduced inflammation and cartilage destruction following joint distraction.34 Meanwhile, a recent study in canine models by Baboolal et al, reported that joint distraction was associated with increased mesenchymal stromal cell adhesion to cartilage, a process necessary for colonization and differentiation of these cells, consequently, leading cartilage repair.35
Limitations
There are several limitations that must be considered when interpreting the findings of this analysis. Firstly, there is a limited amount of data available regarding joint distraction for knee osteoarthritis, with small sample sizes in each study. Thus, the generalisability of these findings to the wider population of patients with knee osteoarthritis should be treated with caution. There are also several inherent methodological limitations to the studies, which render them liable to observational bias; specifically, the lack of participant and assessor blinding, which is due to the nature of the procedure. Nonetheless, this bias is applicable to clinical but not structural outcomes. Furthermore, this bias is unlikely to persist for up to 9 years.
Conclusion
The present systematic review demonstrates that joint distraction confers short-term clinical and structural benefit in patients with knee osteoarthritis, with the clinical benefits persisting till 9 years. Furthermore, KJD confers comparable clinical improvements with currently used procedures such as TKA and HTO. The current evidence-base is limited by a small number of studies, which are susceptible to observational bias. Larger RCTs with longer follow-up of more than 1 year are necessary to establish the true effect size of this procedure.
Disclosure
The abstract of this paper was presented at the World Congress on Osteoporosis, Osteoarthritis, and Musculoskeletal Diseases 2018 as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in Osteoporosis International: World Congress on Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (WCO-IOF-ESCEO 2018): Poster Abstracts (https://link.springer.com/article/10.1007%2Fs00198-018-4465-1). The authors report no other conflicts of interest in this work.
References
1. Bijlsma JW, Berenbaum F, Lafeber FP. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377(9783):2115–2126. doi:10.1016/S0140-6736(11)60243-2
2. Glyn-Jones S, Palmer AJR, Agricola R, et al. Osteoarthritis. Lancet. 2015;386(9991):376–387. doi:10.1016/S0140-6736(14)60802-3
3. Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010;26(3):355–369. doi:10.1016/j.cger.2010.03.001
4. Wu Y, Goh EL, Wang D, Ma S. Novel treatments for osteoarthritis: an update. Open Access Rheumatol. 2018;10:135. doi:10.2147/OARRR.S176666
5. Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res®. 2009;467(10):2606–2612. doi:10.1007/s11999-009-0834-6
6. Dahl AW, Robertsson O, Lidgren L. Surgery for knee osteoarthritis in younger patients: a Swedish Register Study. Acta Orthop. 2010;81(2):161–164. doi:10.3109/17453670903413186
7. Bayliss LE, Culliford D, Monk AP, et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet. 2017;389(10077):1424–1430. doi:10.1016/S0140-6736(17)30059-4
8. Van Valburg A, Van Roermund P, Marijnissen A, et al. Joint distraction in treatment of osteoarthritis (II): effects on cartilage in a canine model. Osteoarthritis Cartilage. 2000;8(1):1–8. doi:10.1053/joca.1999.0263
9. Spaans AJ, Minnen L, Braakenburg A, Mink van der Molen AB. Joint distraction for thumb carpometacarpal osteoarthritis: a feasibility study with 1-year follow-up. J Plast Surg Hand Surg. 2017;51(4):254–258. doi:10.1080/2000656X.2016.1241789
10. Van Valburg A, Van Roermund P, Lammens J, et al. Can Ilizarov joint distraction delay the need for an arthrodesis of the ankle? A preliminary report. Bone Joint J. 1995;77(5):720–725.
11. Van Valburg A, Van Roermund P, Marijnissen A, et al. Joint distraction in treatment of osteoarthritis: a two-year follow-up of the ankle. Osteoarthritis Cartilage. 1999;7(5):474–479. doi:10.1053/joca.1998.0242
12. Aldegheri R, Trivella G, Saleh M. Articulated distraction of the hip. Conservative surgery for arthritis in young patients. Clin Orthop Relat Res. 1994;(301):94–101.
13. Thacker MM, Feldman DS, Madan SS, Straight JJ, Scher DM. Hinged distraction of the adolescent arthritic hip. J Pediatr Orthop. 2005;25(2):178–182.
14. Deie M, Ochi M, Adachi N, Kajiwara R, Kanaya A. A new articulated distraction arthroplasty device for treatment of the osteoarthritic knee joint: a preliminary report. Arthroscopy. 2007;23(8):833–838. doi:10.1016/j.arthro.2007.02.014
15. Intema F, Van Roermund PM, Marijnissen AC, et al. Tissue structure modification in knee osteoarthritis by use of joint distraction: an open 1-year pilot study. Ann Rheum Dis. 2011;70(8):1441–1446. doi:10.1136/ard.2010.142364
16. Wiegant K, Van Roermund P, Intema F, et al. Sustained clinical and structural benefit after joint distraction in the treatment of severe knee osteoarthritis. Osteoarthritis Cartilage. 2013;21(11):1660–1667. doi:10.1016/j.joca.2013.08.006
17. van der Woude J, van Heerwaarden R, Spruijt S, et al. Six weeks of continuous joint distraction appears sufficient for clinical benefit and cartilaginous tissue repair in the treatment of knee osteoarthritis. Knee. 2016;23(5):785–791. doi:10.1016/j.knee.2016.05.001
18. van der Woude J-TA, Wiegant K, Van Roermund PM, et al. Five-year follow-up of knee joint distraction: clinical benefit and cartilaginous tissue repair in an open uncontrolled prospective study. Cartilage. 2017;8(3):263–271. doi:10.1177/1947603516665442
19. Jansen MP, van der Weiden GS, Van Roermund PM, Custers RJ, Mastbergen SC, Lafeber FP. Initial tissue repair predicts long-term clinical success of knee joint distraction as treatment for knee osteoarthritis. Osteoarthritis Cartilage. 2018;26(12):1604–1608. doi:10.1016/j.joca.2018.08.004
20. Hunziker E. Articular cartilage repair: basic science and clinical progress. A review of the current status and prospects. Osteoarthritis Cartilage. 2002;10(6):432–463. doi:10.1053/joca.2002.0801
21. Goh EL, Lou WCN, Chidambaram S, Ma S. Joint distraction for knee osteoarthritis: protocol for a systematic review and meta-analysis. Syst Rev. 2018;7(1):162. doi:10.1186/s13643-018-0837-z
22. Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality if Nonrandomized Studies in Meta-analyses. 2013. Available at http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 11 October 2018.
23. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi:10.1136/bmj.d5928
24. van der Woude J, Wiegant K, van Heerwaarden R, et al. Knee joint distraction compared with high tibial osteotomy: a randomized controlled trial. Knee Surg Sports Traumatol Arthroscopy. 2017;25(3):876–886. doi:10.1007/s00167-016-4131-0
25. van der Woude J, Wiegant K, van Heerwaarden R, et al. Knee joint distraction compared with total knee arthroplasty. Bone Joint J. 2017;99(1):51–58. doi:10.1302/0301-620X.99B1.BJJ-2016-0099.R3
26. Jansen MP, Besselink NJ, van Heerwaarden RJ, et al. Knee joint distraction compared with high tibial osteotomy and total knee arthroplasty: two-year clinical, radiographic, and biochemical marker outcomes of two randomized controlled trials. Cartilage. 2019;1947603519828432.
27. Dieppe PA, Cushnaghan J, Shepstone L. The Bristol ‘OA500’study: progression of osteoarthritis (OA) over 3 years and the relationship between clinical and radiographic changes at the knee joint. Osteoarthritis Cartilage. 1997;5(2):87–97.
28. Lethaby A, Temple J, Santy‐Tomlinson J. Pin site care for preventing infections associated with external bone fixators and pins. Cochrane Database of Systematic Reviews.2013;(12).
29. Flouzat-Lachaniette C-H, Roubineau F, Heyberger C, Bouthors C. Distraction to treat knee osteoarthritis. Joint Bone Spine. 2017;84(2):141–144. doi:10.1016/j.jbspin.2016.03.004
30. Mastbergen SC, Saris DB, Lafeber FP. Functional articular cartilage repair: here, near, or is the best approach not yet clear? Nature Rev Rheumatol. 2013;9(5):277. doi:10.1038/nrrheum.2013.29
31. Wiegant K, van Roermund P, van Heerwaarden R, et al. Total knee prosthesis after joint distraction treatment. J Surg Surgical Res. 2015;1(3):66–71. doi:10.17352/2455-2968.000016
32. Kajiwara R, Ishida O, Kawasaki K, Adachi N, Yasunaga Y, Ochi M. Effective repair of a fresh osteochondral defect in the rabbit knee joint by articulated joint distraction following subchondral drilling. J Orthop Res. 2005;23(4):909–915. doi:10.1016/j.orthres.2004.12.003
33. Wiegant K, Intema F, van Roermund PM, et al. Evidence of cartilage repair by joint distraction in a canine model of osteoarthritis. Arthritis Rheumatol. 2015;67(2):465–474. doi:10.1002/art.v67.2
34. Chen Y, Sun Y, Pan X, Ho K, Li G. Joint distraction attenuates osteoarthritis by reducing secondary inflammation, cartilage degeneration and subchondral bone aberrant change. Osteoarthritis Cartilage. 2015;23(10):1728–1735. doi:10.1016/j.joca.2015.05.018
35. Baboolal TG, Mastbergen SC, Jones E, Calder SJ, Lafeber FPJG, McGonagle D. Synovial fluid hyaluronan mediates MSC attachment to cartilage, a potential novel mechanism contributing to cartilage repair in osteoarthritis using knee joint distraction. Ann Rheum Dis. 2016;75(5):908. doi:10.1136/annrheumdis-2014-206847
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
