Back to Journals » Journal of Inflammation Research » Volume 17
The Role of Infiltrated T Lymphocyte in Oral Squamous Cell Carcinoma: Insights into Clinicopathological Characteristics and Prognosis
Authors Liao W, Lu J , Xu Y, Yang C, Chen H, Cai S , Liu L, Chen S
Received 26 October 2023
Accepted for publication 12 March 2024
Published 11 April 2024 Volume 2024:17 Pages 2195—2204
DOI https://doi.org/10.2147/JIR.S446682
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Wei Liao,1,2,* Jiaxuan Lu,3,* Yuyuan Xu,4,* Chulin Yang,1,5 Hongjie Chen,4 Shaohang Cai,4 Lili Liu,1,6 Shuwei Chen1,5
1State Key Laboratory of Oncology in South China, Guangdong Provincial Clinical Research Center for Cancer, Collaborative Innovation Center for Cancer Medicine, Guangzhou, People’s Republic of China; 2Department of Intensive Care Unit, Sun Yat-sen University Cancer Center, Guangzhou, People’s Republic of China; 3Hospital of Stomatology, Guanghua School of Stomatology, Guangdong Provincial Key Laboratory of Stomatology, Sun Yat-sen University, Guangzhou, Guangdong, People’s Republic of China; 4Department of Infectious Diseases, Nanfang Hospital, Southern Medical University, Guangzhou, People’s Republic of China; 5Department of Head and Neck Surgery, Sun Yat-sen University Cancer Center, Guangzhou, People’s Republic of China; 6Department of Pathology, Sun Yat-sen University Cancer Center, Guangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Shaohang Cai, Department of Infectious Diseases, Nanfang Hospital, Southern Medical University, Guangzhou, 510515, People’s Republic of China, Email [email protected] Shuwei Chen, Department of Head and Neck Surgery, Sun Yat-sen University Cancer Center, Dongfeng East Road, Guangzhou, 510060, People’s Republic of China, Email [email protected]
Background: To compare and analyze the presence of CD4+ and CD8 + lymphocyte infiltrates in Oral squamous cell carcinoma (OSCC) tissue versus adjacent tissue and their clinical significance.
Methods: We enrolled a total of 152 patients diagnosed with OSCC, all of whom had confirmed diagnoses through pathological reports. Clinical and demographics data were extracted from medical records. Tissue microarrays were constructed and immunohistochemical staining for CD4 and CD8 was performed.
Findings: The average number of infiltrating CD4+ T cells in OSCC tumor tissue was 1026.22± 1163.36 cells/mm2, which did not significantly differ from the count in adjacent tissue, which was 1163.36± 1013.23 cells/mm2. However, the number of CD8+ T cell infiltration in tumor tissue was significantly higher than in adjacent tissue (655.25± 705.70 vs 504.56± 659.26 cells/mm2, p = 0.026). We observed that, among patients who consumed alcohol, the CD4+ T cell infiltration in tumor tissue being significantly lower than that in adjacent tissue (P=0.036). Moreover, the CD8+ T cell infiltration in cancer tissue was significantly higher than in adjacent tissue for T1-2 patients (p=0.005). Patients with higher CD8+ T cell in tumor tissue exhibited significantly improved overall survival (p = 0.043). Multivariate analyses revealed that alcohol consumption had a significant impact on the number of CD4+T lymphocytes in tumor tissue (OR = 0.403, P = 0.033) while T stage was the independent factor affecting CD8+ T lymphocyte infiltration in tumor tissue (OR = 0.459, P = 0.031).
Interpretation: OSCC patients with a higher number of CD8+ T lymphocyte infiltration in tumor tissue exhibited an improved prognosis.
Keywords: microenvironment, OSCC, CD8 T cells, CD4 T cells, prognosis
Introduction
Oral squamous cell carcinoma (OSCC) is the primary form of oral cancer.1,2 While the treatment of OSCC has evolved into comprehensive multimodal approaches, encompassing surgery, radiotherapy, chemotherapy, targeted therapy, and immunotherapy, the 5-year survival rate remains low at approximately 50%.3,4
OSCC is marked by a multi-stage progressive malignant transformation, characterized by a unique tumor microenvironment.5 This microenvironment comprises diverse cellular and non-cellular elements. The cellular constituents encompass immune cells, fibroblasts, endothelial cells, adipocytes. Among immune cells, there are including T lymphocytes, B lymphocytes, neutrophils, dendritic cells, macrophages, natural killer cells and others. The interplay between OSCC tumor cells and the microenvironment elements creates a complex tumor ecosystem.6 These components influence tumor cells or engage in interactions via cytokines, therefore establishing a complicated regulatory network pivotal in the onset, progress, metastasis, recurrence, and treatment of OSCC.
Nonetheless, owing to the varied causes of OSCC and the intricacies microenvironment of the oral cavity, different OSCCs may present different tumor microenvironments.7,8 Notably, the infiltration of T lymphocytes within tumor tissue differs from that in adjacent tumor regions. Gannot et al reported an elevation in CD4+ CD8+ T lymphocytes and B cells in cases of moderate and severe dysplasia, as well as in OSCC compared to hyperkeratotic lesions, implying an enhanced antitumor immune response during OSCC development.9 Strauss et al demonstrated a transition toward an infiltrating CD25+FoxP3+ CD4+ cells in patients with head and neck squamous cell carcinoma.10 Ratio of CD8+ T lymphocytes to CD4+ cells was observed to increase following dysplastic changes, potentially indicating an immune system response.11 Taken together, these findings may suggest that immune system play a crucial role in OSCC progression. But, however, the connection between T lymphocyte infiltration and its impact on the clinicopathological characteristics and prognosis of OSCC remains unclear.
Consequently, this study incorporated a serial of samples of OSCC tissues, aiming to investigate their potential relationship with the clinicopathological characteristics and prognosis. Our aim to compare and analyze the presence of CD4+ and CD8 + lymphocyte infiltrates in cancer tissue versus adjacent tissue and their potential clinical significance.
Subjects and Methods
Patient Enrollment
We enrolled a total of 152 patients diagnosed with OSCC, all of whom had confirmed diagnoses through pathological reports. Detailed data were collected, including lifestyle and clinicopathological information. Inclusion criteria including complete medical records, demographics and clinicopathological data. Patients were excluded if they met any of the following conditions: 1) Inadequate tissue samples or incomplete medical records, 2) A primary malignancy other than OSCC confirmed. The study was ethically approved by the Ethics Committee of Sun Yat-sen University Cancer Hospital (Approval No. SL-B2023-374-01), and informed consent was obtained from all participants.
Tissue Microarray Construction, Immunohistochemistry, and Pathological Scoring
Tissue microarrays were constructed using pairs of OSCC and adjacent tissue specimens. Immunohistochemical staining for CD4 and CD8 (CD4 antibody, 1:2000, ab133616, Abcam; CD8 antibody, 1:500, 10,980-R081, SinoBiological) was performed. As shown in Supplementary Figure 1. The quantification of tissue-infiltrating T lymphocytes was carried out by clinical pathologists from the Department of Pathology at Sun Yat-sen University Cancer Center.
Statistical Analysis
Normally distributed data were presented as mean ± standard deviation (SD), while categorical data were expressed as percentages. Comparative analyses were conducted using t-tests and Chi-square as appropriate. We employed Pearson correlation and logistic regression for data analysis. Statistical analyses were carried out using SPSS software (version 13.0), with significance levels set at p < 0.05.
Results
Association Between Clinicopathological Data and Infiltration of CD4+ T Cells
In our study comprising 152 OSCC patients, as detailed in Table 1, patients were categorized into two groups: one with a higher number of CD4+ T cells infiltrating the tumor tissue compared to adjacent tissue (CD4 N<T group), and the other with an equal or lower number (CD4 N≥T group). Most clinical data between these patient groups were similar, except for the prevalence of alcohol drinking habits. Notably, a higher proportion of patients in CD4 N≥T group had a history of drinking (p = 0.033).
 |
Table 1 Clinical Data of OSCC Patient with Different Infiltrating CD4+ Cells |
Association Between Clinicopathological Data and Infiltration of CD8+ T Cells
Similarly, the patients were divided into two groups based on the number of CD8+ T cells infiltrating tumor tissue relative to adjacent tissue, as presented in Table 2. Most clinicopathological characteristics were comparable between these groups, except for the T classification. Patients in CD8 N<T group had a higher proportion of early T stage (p = 0.029).
 |
Table 2 Clinical Data of OSCC Patient with Different Infiltrating CD8+ Cells |
Analysis of T Lymphocyte Infiltration in OSCC Tumor and Adjacent Tissue
Further analysis of the relationship between T lymphocyte infiltration and clinical pathology is illustrated in Figure 1. The average number of infiltrating CD4+ T cells in OSCC tumor tissue was 1026.22±1163.36 cells/mm2, which did not significantly differ from the count in para-cancerous tissue, which was 1163.36±1013.23 cells/mm2. However, the number of CD8+ T cell infiltration in tumor tissue (655.25±705.70 cells/mm2) was significantly higher than in adjacent tissue (504.56±659.26 cells/mm2, p = 0.026).
Given our previous observation of a potential link between alcohol consumption and CD4+ T cell infiltration, we conducted a comprehensive analysis. As demonstrated in Figure 1C and D, no significant differences were found in CD4+ T cell infiltration between drinkers or in non-drinkers both in adjacent and tumor tissue (P=0.171 and P=0.347, respectively). However, among the group of patients who consumed alcohol, a noteworthy distinction emerged, with CD4+ T cell infiltration in tumor tissue being significantly lower than that in adjacent tissue (P=0.036).
Similarly, patients were divided into T1-2 and T3-4 groups based on T stage. We observed no differences in the number of infiltrating CD8+ T cells in adjacent tissue between these two groups. However, in the tumor tissue, patients in the T1-2 group exhibited significantly higher CD8+ T cell infiltration than those in the T3-4 group. Moreover, by paired analysis, it was evident that CD8+ T cell infiltration in cancer tissue was significantly higher than in adjacent tissue for T1-2 patients. While there were no significant difference in CD8+ T cell infiltration between adjacent and cancer tissue in the T3-4 group.
Correlation Between Tissue Infiltrating T Lymphocytes and Prognosis
We examined the association between overall survival in the CD4 N≥T group and the CD4 N<T group. As depicted in Figure 2A, we found no statistically significant difference in overall survival between these two groups. However, in patients of CD8 N<T group and of the CD8 N≥T group, we observed a significant difference. Patients in the CD 8N<T group exhibited significantly improved overall survival compared to those in the CD8 N≥T group, as shown in Figure 2B (p = 0.043).
Next, we analyzed whether T lymphocytes infiltrating adjacent tissue have an impact on prognosis. We categorized patients into high adjacent tissue CD4+T lymphocyte infiltration and low adjacent tissue CD4+T lymphocyte infiltration groups, based on the median value of CD4+T lymphocytes infiltrating in adjacent tissue. We did not find any different in prognosis between these two groups. Similarly, when patients were divided into high adjacent tissue CD8+T lymphocyte and low adjacent tissue CD8+T lymphocyte groups, there were no significant differences in prognosis between these groups, as indicated in Figure 2C and D.
Regarding tumor recurrence, our analysis revealed that neither CD4+ T lymphocyte infiltration nor CD8+ T cell lymphocyte infiltration in tumor tissue had any impact on tumor recurrence. Similarly, the presence of CD4+ T lymphocytes and CD8+ T lymphocytes infiltrated in adjacent tissue did not influence tumor recurrence (Figure 2E–H).
Factors Related to Tumor-Infiltrating T Lymphocytes
We further explored variables linked to the number of T lymphocytes infiltrating tumor tissue. We observed a positive correlation between the numbers of CD4+ T lymphocytes and CD8+ T lymphocytes infiltrated in tumor tissue (p < 0.001, Figure 3A). Notably, data also revealed that increased CD4+ T lymphocyte infiltration into adjacent tissue was associated with a greater number of CD4+ T lymphocytes infiltrating tumor tissue (p = 0.027, Figure 3B). Similarly, CD8+ T lymphocyte infiltration into adjacent tissue corresponded to higher CD8+ T lymphocyte infiltration into the tumor tissue (p = 0.001, Figure 3C). And the increased number of CD4+T cell infiltrating cells in adjacent tissue correlated with a greater number of CD8+T cell infiltrating cells in the adjacent tissue (p < 0.001, Figure 3D).
Multivariable Analysis of T Lymphocyte Infiltration in Tumor Tissue
To access the independent factors affecting the numbers of CD4+ T lymphocyte infiltrations in tumor tissue, we conducted univariate and multivariate analyses. Our findings revealed that only alcohol consumption had a significant impact on the number of CD4+T lymphocytes in tumor tissue (OR = 0.403, P = 0.033), as shown in Table 3.
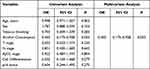 |
Table 3 Univariate and Multivariate Analyses for High Infiltrating CD4+ T Cells |
Similarly, for CD8+ T lymphocyte infiltration in tumor tissue, the multivariable analyses, as presented in Table 4, indicated that only T stage was the independent factor affecting CD8+ T lymphocyte infiltration in tumor tissue (OR = 0.459, P = 0.031).
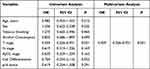 |
Table 4 Univariate and Multivariate Analyses for High Infiltrating CD8+ T Cells |
Discussion
Lymphocyte infiltration into tumor tissue has a strong association between immune response, tumor characteristics, and overall prognosis.12–14 In this study, we noted that patients with a higher number of CD8+ T lymphocyte infiltration in tumor tissue exhibited an improved prognosis. This finding aligns with the results of previous research studies.15,16 We also found that the number of CD4+ T lymphocytes in tumor tissue or the level of T lymphocyte infiltration in adjacent tissue did not significantly correlate with prognosis. Furthermore, we identified an association between alcohol consumption and the infiltration of CD4+ T lymphocytes in tumor tissue, as well as a relationship between T stage and the infiltration of CD8+ T lymphocytes in tumor tissue. However, the underlying mechanisms behind these associations remain unclear.
Previous studies have found that the migration of T lymphocyte into tumor tissue is influenced by numerous factors, including vascular formation, cytokine expression, and tumor antigens.17,18 Moreover, the level of T lymphocyte infiltration in tumor tissue may have implications for immune checkpoint therapy.19–21 In this study, we observed that patients who consumed alcohol exhibited lower levels of tumor-infiltrating CD4+ T lymphocytes. In contrast, patients with early T-stage OSCC presented with increased infiltration of CD8+ T lymphocytes. This result may implied that early-stage OSCC patients may benefit more from immunotherapy. Conversely, for advanced T-stage OSCC patients, it may advisable to implement closer monitoring and follow-up after immunotherapy. However, these hypotheses warrant further research for validation.
Interactions between different immune lymphocytes also influence the infiltration of T lymphocytes into tumor tissue. For instance, CD4+ T lymphocytes are known to participate in the activation and proliferation of CD8+ T lymphocytes, and CD4+ T lymphocytes can regulate the inflammatory microenvironment, facilitating the recruitment of CD8+ T lymphocytes.22,23 Wong et al24 reported that intratumoral CD4+ T lymphocytes promote the recruitment of CD8+ T lymphocytes. Other studies have suggested that CD4+ T lymphocytes in tumors can stimulate the expression of chemokines, such as CXCL9 and CXCL10, via IFN-γ production, thereby enhancing the infiltration of CD8+ T lymphocytes.22,23 Our study also showed that there was a positive correlation between the numbers of infiltrating CD4+ T lymphocytes and CD8+ T lymphocytes in tumor tissue. Targeting CD4+ T lymphocytes to enhance the infiltration of CD8+ T lymphocytes may offer a potential therapeutic strategy to improve treatment response rates of immune checkpoint inhibitor and prognosis in patients.
The underlying reasons for the diminished infiltration of CD4+ T lymphocytes into tumor tissue among patients who consume alcohol raise intriguing questions. Although we found no significant difference in the number of CD4+ T lymphocytes infiltrating adjacent cancer tissues, regardless of alcohol consumption, it is possible that alcohol diminishes the migratory capacity of CD4+ T lymphocytes into tumor tissue. Existing research suggests that alcohol toxicity can impact CD4+ T cell function.25 It may potentially reduce their infiltration into tumor tissue. In our study, we did not further classify the subsets of CD4+ T lymphocytes. However, we observed that patients with drinking habits exhibited a decreased number of CD4+ T lymphocytes infiltrating tumor tissue.
Patients with early T stage presented with increased CD8+ T lymphocyte infiltration in tumor tissue also raises questions. Previous research has indicated that the number of lymphocyte infiltrations changed as the disease progresses, reflecting immune evasion by tumor lymphocytes.26 Factors such as changes in tumor antigens, modifications in cytokine expression profiles, and other elements might contribute to dynamic change of infiltrated T lymphocytes. In our study, we did not further evaluate the functional aspects of CD8+ T lymphocytes infiltrating tumor tissue. It may be possible that the function of these tumor-infiltrating CD8+ T lymphocytes might also undergo alterations as the T stage advances. Therefore, it’s worth investigating whether the functionality of CD8+ T lymphocytes in tumor tissue is compromised as the T stage increases.
This study has some limitations, including a relatively small sample size, a single-center cohort, and an absence of analysis pertaining to further T lymphocyte subpopulations. These limitations need to be addressed and validated by large-sample multi-center studies.
In conclusion, this study unveiled the relationship between lymphocyte infiltration in OSCC tumor tissue. There is a positive correlation between the number of CD8+ T lymphocytes and CD4+ T lymphocytes infiltrating tumor tissue. Our study also revealed novel findings regarding the impact of alcohol drinking on the number of CD4+ T cells infiltrating tumor tissue and the influence of T stage on the number of CD8+ T cells infiltrating tumor tissue. OSCC patients who consume alcohol exhibit reduced infiltration of CD4+ T lymphocytes while patients with advanced T stage experience decreased infiltration of CD8+ T lymphocytes. A higher count of infiltrated CD8+ T cells within the tumor tissue is associated with better patient prognosis. These results offer insights the potential mechanism of tumor immune evasion and contribute to the development of precise and personalized immune checkpoint-based treatments.
Data Sharing Statement
Authors can confirm all relevant data are included in the article, materials are available on reasonable request from the authors and the data was deposited in the Research Data Deposit respository(NO. RDDA2024478017)
Ethics Approval and Consent to Participate
The study was performed in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Sun Yat-sen University Cancer Hospital endorsed the study (Approval No. SL-B2023-374-01). All patient provided written informed consent, agreed to follow the protocol and take specimens, and was willing to anonymously publish details of the medical record.
Acknowledgments
The authors would like to thank all the patients included in this study, and the nurses who assisted in patient management and collection of samples.
Funding
This study was supported by the Guangdong Basic and Applied Basic Research Fund (Natural Science Foundation of Guangdong Province) with No. 2023A1515010464, 2022A1515012631 and 2024A1515013244 and Guangdong Province Health Technology Promotion Project No. 202107021915135539.
Disclosure
None of the authors have competing interests to disclose.
References
1. Gharat SA, Momin M, Bhavsar C. Oral squamous cell carcinoma: current treatment strategies and nanotechnology-based approaches for prevention and therapy. Crit Rev Ther Drug. 2016;33(4):363–400. doi:10.1615/CritRevTherDrugCarrierSyst.2016016272
2. Bugshan A, Farooq I. Oral squamous cell carcinoma: metastasis, potentially associated malignant disorders, etiology and recent advancements in diagnosis. F1000Res. 2020;9:229. doi:10.12688/f1000research.22941.1
3. Sasahira T, Kirita T. Hallmarks of Cancer-Related Newly Prognostic Factors of Oral Squamous Cell Carcinoma. Int J Mol Sci. 2018;19(8). doi:10.3390/ijms19082413
4. Jiang M, Li B. STAT3 and its targeting inhibitors in oral squamous cell carcinoma. Cells-Basel. 2022;11:19.
5. Mughees M, Sengupta A, Khowal S, Wajid S. Mechanism of tumour microenvironment in the progression and development of oral cancer. Mol Biol Rep. 2021;48(2):1773–1786. doi:10.1007/s11033-020-06054-6
6. Pignatelli P, Romei FM, Bondi D, Giuliani M, Piattelli A, Curia MC. Microbiota and oral cancer as a complex and dynamic microenvironment: a narrative review from etiology to prognosis. Int J Mol Sci. 2022;23(15):8323. doi:10.3390/ijms23158323
7. Ai R, Tao Y, Hao Y, et al. Microenvironmental regulation of the progression of oral potentially malignant disorders towards malignancy. Oncotarget. 2017;8(46):81617–81635. doi:10.18632/oncotarget.20312
8. Eckert AW, Wickenhauser C, Salins PC, Kappler M, Bukur J, Seliger B. Clinical relevance of the tumor microenvironment and immune escape of oral squamous cell carcinoma. J Transl Med. 2016;14(1):85. doi:10.1186/s12967-016-0828-6
9. Gannot G, Gannot I, Vered H, Buchner A, Keisari Y. Increase in immune cell infiltration with progression of oral epithelium from hyperkeratosis to dysplasia and carcinoma. Br J Cancer. 2002;86(9):1444–1448. doi:10.1038/sj.bjc.6600282
10. Strauss L, Bergmann C, Szczepanski M, Gooding W, Johnson JT, Whiteside TL. A unique subset of CD4+CD25highFoxp3+ T cells secreting interleukin-10 and transforming growth factor-beta1 mediates suppression in the tumor microenvironment. Clin Cancer Res. 2007;13(15 Pt 1):4345–4354. doi:10.1158/1078-0432.CCR-07-0472
11. Flores-Hidalgo A, Murrah V, Fedoriw Y, Padilla RJ. Relationship of infiltrating intraepithelial T lymphocytes in the diagnosis of oral lichen planus versus oral epithelial dysplasia: a pilot study. Or Surg or Med or Pa. 2019;127(6):e123–e135. doi:10.1016/j.oooo.2019.02.004
12. Stanton SE, Disis ML. Clinical significance of tumor-infiltrating lymphocytes in breast cancer. J Immunother Cancer. 2016;4(1):59. doi:10.1186/s40425-016-0165-6
13. van der Leun AM, Thommen DS, Schumacher TN. CD8(+) T cell states in human cancer: insights from single-cell analysis. Nat Rev Cancer. 2020;20(4):218–232. doi:10.1038/s41568-019-0235-4
14. Farhood B, Najafi M, Mortezaee K. CD8(+) cytotoxic T lymphocytes in cancer immunotherapy: a review. J Cell Physiol. 2019;234(6):8509–8521. doi:10.1002/jcp.27782
15. Zhang Y, Li L, Zheng W, Zhang L, Yao N. CD8(+) T-cell exhaustion in the tumor microenvironment of head and neck squamous cell carcinoma determines poor prognosis. Ann Transl Med. 2022;10(6):273. doi:10.21037/atm-22-867
16. Yamaguchi T, Kinoshita J, Saito H, et al. High CD8/CD33 ratio in peritoneal metastatic lesions is associated with favorable prognosis in gastric cancer. Cancer Rep Us. 2021;4(5):e1389. doi:10.1002/cnr2.1389
17. Rahir G, Moser M. Tumor microenvironment and lymphocyte infiltration. Cancer Immunol Immun. 2012;61(6):751–759. doi:10.1007/s00262-012-1253-1
18. Paijens ST, Vledder A, de Bruyn M, Nijman HW. Tumor-infiltrating lymphocytes in the immunotherapy era. Cell Mol Immunol. 2021;18(4):842–859. doi:10.1038/s41423-020-00565-9
19. Gibney GT, Weiner LM, Atkins MB. Predictive biomarkers for checkpoint inhibitor-based immunotherapy. Lancet Oncol. 2016;17(12):e542–e551. doi:10.1016/S1470-2045(16)30406-5
20. Baba Y, Nomoto D, Okadome K, et al. Tumor immune microenvironment and immune checkpoint inhibitors in esophageal squamous cell carcinoma. Cancer Sci. 2020;111(9):3132–3141. doi:10.1111/cas.14541
21. Tay C, Tanaka A, Sakaguchi S. Tumor-infiltrating regulatory T cells as targets of cancer immunotherapy. Cancer Cell. 2023;41(3):450–465. doi:10.1016/j.ccell.2023.02.014
22. Nakanishi Y, Lu B, Gerard C, Iwasaki A. CD8(+) T lymphocyte mobilization to virus-infected tissue requires CD4(+) T-cell help. Nature. 2009;462(7272):510–513. doi:10.1038/nature08511
23. Castellino F, Huang AY, Altan-Bonnet G, Stoll S, Scheinecker C, Germain RN. Chemokines enhance immunity by guiding naive CD8+ T cells to sites of CD4+ T cell-dendritic cell interaction. Nature. 2006;440(7086):890–895. doi:10.1038/nature04651
24. Wong SB, Bos R, Sherman LA. Tumor-specific CD4+ T cells render the tumor environment permissive for infiltration by low-avidity CD8+ T cells. J Immunol. 2008;180(5):3122–3131. doi:10.4049/jimmunol.180.5.3122
25. Barve SS, Kelkar SV, Gobejishvilli L, Joshi-Barve S, McClain CJ. Mechanisms of alcohol-mediated CD4+ T lymphocyte death: relevance to HIV and HCV pathogenesis. Front Biosci. 2002;7:d1689–d1696. doi:10.2741/A872
26. Hu S, Lu H, Xie W, et al. TDO2+ myofibroblasts mediate immune suppression in malignant transformation of squamous cell carcinoma. J Clin Invest. 2022;132(19). doi:10.1172/JCI157649
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



