Back to Journals » Journal of Inflammation Research » Volume 16
The Role of Albumin in the Diagnosis of Neonatal Sepsis Over the Last 11 Years: A Retrospective Study
Authors Shi J , Lu ZQ, Lin QM, Zeng W, Gu PJ, Yu Q, Long J, Huang DG, Dai YH
Received 2 May 2023
Accepted for publication 27 June 2023
Published 19 July 2023 Volume 2023:16 Pages 2855—2863
DOI https://doi.org/10.2147/JIR.S414611
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ning Quan
Jipeng Shi,1 Zhen-Qi Lu,1 Qing-Mei Lin,2 Wang Zeng,1 Ping-Jiao Gu,1 Qing Yu,3 Jing Long,1 Da-Gui Huang,1 Yi-Heng Dai1
1Department of Neonatal, Affiliated Foshan Maternity & Child Healthcare Hospital, Southern Medical University (Foshan Maternity & Child Healthcare Hospital), Foshan, Guangdong, 528000, People’s Republic of China; 2Affiliated Foshan Maternity & Child Healthcare Hospital, Southern Medical University (Foshan Maternity & Child Healthcare Hospital), Foshan, Guangdong, 528000, People’s Republic of China; 3Department of Clinical Laboratory, Affiliated Foshan Maternity & Child Healthcare Hospital, Southern Medical University (Foshan Maternity & Child Healthcare Hospital), Foshan, Guangdong, 528000, People’s Republic of China
Correspondence: Yi-Heng Dai, Email [email protected]
Background: There are many difficulties and uncertainties in the early diagnosis of neonatal sepsis. The aim of this study was to determine whether albumin (ALB) is useful for the early diagnosis of neonatal sepsis using ALB, C-reactive protein (CRP) and procalcitonin (PCT) together.
Methods: ALB, CRP, PCT and white blood cell (WBC) data from 732 patients with neonatal sepsis and 1317 neonatal infection patients hospitalized in Foshan Maternal and Child Health Hospital from 2011 to 2022 were collected. Receiver operating characteristic (ROC) and logistic regression analyses were performed to assess the diagnostic value of ALB, CRP, PCT and the WBC count for neonatal sepsis. The roles of ALB, CRP, PCT and the WBC count in the diagnosis of neonatal sepsis were analysed by using subject working characteristics (ROC) and areas under the curve (AUCs), and the variables were combined to determine which combination had the best diagnostic efficacy.
Results: In the sepsis group, the ALB, CRP, and PCT levels and the WBC count were significantly higher than those in the infection group (P< 0.001). In all infants, the sensitivities and specificities of ALB, CRP, PCT, and WBC count were 0.411, 0.596, 0.483 and 0.411, respectively, and 0.833, 0.846, 0.901 and 0.796, respectively. With a sensitivity of 0.646, a specificity of 0.929, and an AUC of 0.834, the best combination was that of ALB, CRP, and PCT, which was better than that of CRP + PCT, CRP + ALB and PCT + ALB.
Conclusion: In neonatal sepsis, in the absence of blood culture results, the combination of ALB, CRP, and PCT is more reliable than CRP, PCT, or CRP+PCT alone. These results suggest that ALB is a useful inflammatory biomarker for the early diagnosis of neonatal sepsis, and can improve the diagnostic efficiency.
Keywords: albumin, C-reactive protein, procalcitonin, diagnosis, neonatal sepsis
Introduction
Sepsis in newborns is a serious disease that causes high mortality rates, accounting for 15.2% of all neonatal deaths worldwide.1 However, the clinical manifestations of neonatal sepsis lack early clinical specificity and are easily confused with those of other diseases. Early diagnosis is very difficult, especially for premature infants, who are easily overlooked, may receive delayed treatment and may even die. In neonatal sepsis, early diagnosis and treatment can save many lives. There are often many difficulties in the early detection of neonatal sepsis. At present, the diagnosis of neonatal sepsis is still based on blood culture. Because blood culture takes a long time and the positive rate is not high, it is difficult to obtain early clinical diagnosis and treatment for neonatal sepsis. Therefore, there is an urgent need to obtain more accurate infection indicators to enhance the accuracy of diagnosis.
At present, the commonly used clinical infection indicators are C-reactive protein (CRP), procalcitonin and white blood cell (WBC) count. CRP is the most readily available inflammatory biomarker of infection, and CRP tests are the most commonly used laboratory test.2 However, it takes approximately 10–12 hours for the CRP level to increase, so in early neonatal sepsis diagnosis, CRP tests are not conducive. Procalcitonin (PCT) is an acute-phase, reactive protein. Compared with CRP levels, PCT levels rise rapidly within 2–4 hours of bacterial endotoxin exposure and reach their peak within 6–8 hours after exposure. PCT has become an important inflammatory biomarker in the early diagnosis of neonatal septicaemia.3
However, CRP and PCT are also affected by many factors. CRP levels may also be elevated due to maternal fever, foetal distress and stress, meconium aspiration syndrome (MAS), haemolysis, and tissue damage.4,5 Most studies report that CRP has low sensitivity and specificity and is associated with misdiagnosis and missed diagnosis.6 PCT also varies with various conditions, such as premature birth, intracranial haemorrhage, birth asphyxia, neonatal hypoxemia, and maternal chorioamnionitis (without neonatal infection) within 72 hours after birth.4,5,7 Therefore, CRP, PCT, and the WBC count each have their own shortcomings in neonatal sepsis diagnosis, so combining these inflammatory biomarkers could be helpful for the early diagnosis of neonatal sepsis.
Studies have shown that albumin (ALB) is also a routine detection item in the clinic, and it is not only a nutritional index but also closely related to inflammatory reactions.8–11 Reportedly, compared with patients without sepsis, in patients with sepsis, plasma ALB is reduced.12–14 We hypothesized that ALB combined with CRP, PCT and the WBC count can distinguish neonatal infection from neonatal sepsis, which is of great value in the early diagnosis of neonatal sepsis. We hope that by combining these inflammatory biomarkers, we can diagnose neonatal sepsis early and reduce the mortality rate of neonatal sepsis patients.
Materials and Methods
Patients
A retrospective analysis across a 11-year period was conducted on data from neonates suspected of neonatal sepsis who were admitted to the neonatology department at the Affiliated Foshan Maternity & Child Healthcare Hospital, Southern Medical University from December 27, 2011 to October 2, 2022.
The first group was the sepsis group, which included 732 patients (455 males, 277 females, ranging in age from 2 to 16 days, with a median age of 4 days) with blood culture-proven or clinically diagnosed sepsis. The second group was the neonatal infection group (nonsepsis group). These newborns had elevated inflammatory biomarkers but did not meet the diagnostic criteria for neonatal sepsis, and a total of 1317 patients were included in this group (819 males and 498 females, ranging in age from 1 to 3 days, with a median age of 2 days). The diagnosis of neonatal septicaemia depended on clinical features, infection indexes and blood culture results.15–18 Exclusion criteria were as follows: (1) patients with incomplete data, including CRP, PCT, ALB, WBC count data; and (2) subjects with other medical conditions, such as major congenital malformations and cyanotic congenital heart disease, haematological disorders, cancers, and major congenital malformations.
This study protocol complied with the Declaration of Helsinki and was approved by the Ethics Committee of Affiliated Foshan Maternity & Child Healthcare Hospital. All data were anonymized and maintained in a confidential manner. Since the study was retrospective, informed consent was not needed.
Clinical Evaluation and Definition
Diagnoses of neonatal sepsis and infection were made by two independent physicians according to the 2019 Expert Consensus on Diagnosis and Treatment of Neonatal Sepsis and the International Pediatric Sepsis Consensus.15,18 The definition of neonatal sepsis from the 2019 Expert Consensus on Diagnosis and Treatment of Neonatal Sepsis was used.18 Sepsis is a systemic inflammatory response syndrome caused by various pathogens, including bacteria, viruses, and parasites. In septicaemia, pathogens (including bacteria and fungi) that can cause systemic inflammatory response syndrome can be cultured from blood (or aseptic cavities such as cerebrospinal fluid).18 Diagnosis is suspected if any one of the following conditions are met within 3 days of birth: (1) abnormal clinical symptoms, (2) maternal chorioamnionitis, and (3) a premature rupture of membranes (PROM) duration ≥18 hours. Sepsis can be ruled out if there are no abnormal clinical symptoms, the blood culture is negative, and two nonspecific blood tests conducted 24 hours apart are positive for less than two items. Alternatively, the clinical diagnosis of sepsis can be made if any one of the following conditions are met along with abnormal clinical symptoms: (1) two or more positive nonspecific blood tests, (2) purulent meningitis changes observed in cerebrospinal fluid samples, and (3) pathogenic bacterial DNA is detected in the blood. Finally, a definite diagnosis can be made if clinical symptoms are present and there is a positive blood culture or cerebrospinal fluid (or other sterile fluid) culture. Infection refers to a suspected or proven infection caused by any pathogen or clinical syndrome associated with a high probability of infection. Evidence of infection includes positive clinical exam, imaging, or laboratory test findings.15
Collection and Biochemical Analyses
The collected data included the following: 1) clinical data including age, sex, weight, temperature, respiratory rate, heart rate, systolic blood pressure, and diastolic blood pressure; and 2) laboratory data at admission, which included PCT, CRP, aspartate aminotransferase (AST), alanine aminotransferase (ALT), total protein (TP), ALB, blood urea nitrogen (BUN), creatinine (CREA), and uric acid (UA) levels. Blood samples were collected when a newborn was suspected of having an infection, and an automatic blood cell counter (Sysmex Company, Kobe, Japan) measured the WBC count, neutrophil count, and lymphocyte count. The CRP level was measured using a dry fluorescence immunoanalyzer (Baditai), and CRP levels below 0.8 mg/L were statistically treated as 0.7 mg/L. PCT levels were measured using fluorescence immunochromatography on a dry fluorescence immunoanalyzer. The measurement range was 0.1–100. In this study, PCT levels above 100 ng/mL were considered 101 ng/mL, and those below 0.02 ng/mL (lower limit of measurement) were considered 0.01 ng/mL.Serum total ALB, AST, ALT, bilirubin (TBIL), urea nitrogen (UREA), CREA and UA levels were measured using an automated biochemical analyser (AU5800 clinical chemical analyser, Beckman Kurt, California). Over the past 10 years, the instruments used for these indicators have been partially upgraded and replaced, but the instrument platform (brand) has remained the same, and the reference ranges have not changed.
Statistical Analysis
Continuous variables are expressed as the mean±standard deviation (SD) or median (interquartile range) and were compared using an independent t-test or the Wilcoxon-rank sum test according to their distribution. Categorical variables are presented as percentages (n, %) and were analysed using the chi-square test. Multivariate logistic regression analysis was performed to identify the independent risk factors for the presence of neonatal sepsis, adjusting for the potential confounders of age, sex and weight. Receiver operating characteristic (ROC) curves were constructed to evaluate the diagnostic value of the serum biomarkers for the presence of neonatal sepsis. Youden’s index was calculated (sensitivity + specificity − 1) to determine the optimal cut-off point. The area under the ROC curve (AUC) of two different indicators was compared using Delong’s test. A two-sided P value less than 0.05 was considered statistically significant. All statistical analyses were performed using R language (version 4.1.3).
Results
ALB, CRP, PCT and WBC Results of the Study Subjects
This study included 2049 newborns who were divided into an infection group and a sepsis group. Among the newborns, 732 were diagnosed with neonatal sepsis, and 1317 were diagnosed with neonatal infection. Table 1 shows the baseline clinical and laboratory data for both groups. The median age of the neonates with sepsis was 4.00 (2.0–16.0) days and that of neonates with infection was 2.0 (1.0–3.0) days (P<0.001). Clinical data showed that the respiratory rate and heart rate of the newborns with sepsis were increased compared with those of the newborns with infection (P <0.001). The serum PCT, CRP and urea levels in the neonates with sepsis were significantly higher than those in the neonates with infection (P<0.001), while the serum TBIL, ALT, TP, ALB, CREA and UA levels were lower (P<0.001). Other indexes, such as the leukocyte count, neutrophil count, lymphocyte count and platelet count, were also significantly different between the two groups (P<0.001) (Table 1).
 |
Table 1 Baseline Characteristics of the Infection and Sepsis Group |
The Association of Inflammatory Biomarker Levels with the Risk of Neonatal Sepsis
To investigate the association of the ALB, CPR, PCT levels and WBC count with the diagnosis of neonatal sepsis, we classified the study participants into four groups according to ALB, CPR, and PCT levels and the WBC count. The crude odds ratio (OR) in logistic regression analysis was used to evaluate the importance of the inflammatory biomarkers in the diagnosis of neonatal sepsis (Table 2). After adjusting for birth age, sex, and weight (Table 2), we obtained adjusted ORs to avoid possible adverse effects of age, sex, and weight. Except for the WBC count, age, sex, and weight had no effect on the ALB, CRP, and PCT levels.
 |
Table 2 Multivariate Logistic Regression Analysis for Prediction of Neonatal Sepsis |
Analysis of the Role of the Inflammatory Biomarkers in the Diagnosis of Neonatal Sepsis by Subject Operation Characteristic Curve Analysis
ROC analysis was used to evaluate the utility of the ALB, CPR, and PCT levels and the WBC count in the prediction of neonatal sepsis. Based on the area under the ROC curve (AUC), the CRP+PCT+ALB combination had good discriminatory power (AUC=0.834, 95% CI (0.813–0.855)), P<0.001) (Figure 1). The CRP+PCT+ALB combination had a sensitivity of 0.646 and a specificity of 0.929 for the prediction of neonatal sepsis (Table 3).
 |
Table 3 Cut-off Values of Inflammatory Biomarkers for Neonatal Sepsis Diagnosis |
 |
Figure 1 Receiver operating characteristic (ROC) curves of ALB, PCT, and CRP levels and the WBC count as inflammatory biomarkers of neonatal sepsis. |
Comparison of Infection Indicators After Association
We combined these inflammatory biomarkers to improve the diagnosis of neonatal sepsis. This study compared the combinations of infection biomarkers and found that the CRP + PCT + ALB combination had the best diagnostic efficacy (AUC=0. 834), which was better than that of the CRP + PCT (AUC=0. 826), CRP + ALB (AUC=0. 795) and PCT + ALB (AUC=0. 749) combinations. Although the diagnostic efficacy of the CRP + PCT + ALB + WBC count (AUC=0. 837) combination was higher than that of the CRP + PCT + ALB (AUC=0. 834) combination, there was no significant difference between them (Z value, P=0.19), as shown in Table 4.
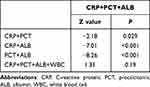 |
Table 4 Test for a Difference in Two ROC Curves |
Discussion
Severe infection is the main cause of early neonatal death.19 Neonatal sepsis is a fatal systemic and severe infection in the neonatal period that is related to adverse outcomes in neonates, such as nervous system injury and chronic lung diseases. However, the early clinical manifestations of neonatal sepsis lack clinical specificity and are easily confused with those of noninfectious diseases, and early diagnosis is very difficult. At present, blood culture is a very important standard for diagnosing neonatal sepsis, but the waiting time for the results is long, and the positive rate is low. Often, this affects the early clinical diagnosis and treatment of neonatal sepsis. On the other hand, newborns with suspected sepsis are usually treated with antibiotics at an early stage.20 Although this treatment strategy will reduce neonatal deaths, it may contribute to the overuse of antibiotics and even induce the emergence of multidrug-resistant bacteria in neonatal wards.21 Therefore, early diagnosis of neonatal sepsis is very important to prevent microbial drug resistance caused by empirical treatment.22
In recent years, researchers of neonatal sepsis have paid more attention to cytokines and other inflammatory biomarkers. However, it is undeniable that CRP, PCT and the WBC count, which are commonly used inflammatory biomarkers, still play an important role, so it may be beneficial to combine these infection inflammatory biomarkers to improve the diagnostic rate of neonatal sepsis. It is well known that in most individuals, CRP and PCT levels increase significantly after bacterial infection, but due to various factors, CRP and PCT levels cannot completely and accurately reflect infection.4 As a result, it is difficult to diagnose neonatal sepsis using CRP and PCT levels alone, especially in separating neonatal infection from neonatal sepsis.
This study compared the levels of these four indexes between patients with neonatal sepsis and neonatal infection and found that ALB, CRP, and PCT levels and the WBC count in patients with neonatal sepsis were significantly higher than those in patients with neonatal infection. In this study, when these inflammatory biomarkers were used alone, their sensitivity was between 41.1% and 59.6%, their specificity was between 79.6% and 90.1%, and their AUC was between 0.598 and 0.767. Therefore, it is obvious that these inflammatory biomarkers are not effective for diagnosis when used alone. In this research, the sensitivity of CRP was 0.596 (0.56–0.631), which was similar to that of the European population (0.63 (0.47–0.79)) but lower than that of the Asian population (0.72 (0.63–0.80)).23 Although these differences between the European population and Asian population are believed to be related to genetic factors, there are few data to prove this, so more research is needed for verification. The sensitivity of PCT in this study (0.483 (0.447–0.52)) was significantly lower than that in the Asian study (0.85 (0.80–0.91)).23 The sensitivity of the CRP + PCT combination in this study was 0.638 (0.603–0.673), similar to that of the European population (0.69 (0.51–0.87)) but significantly lower than that of the Asian population (0.93 (0.90–0.97)).23
The results showed that the combination of ALB, CRP and PCT increased the sensitivity from 48.3% to 64.6% and the specificity from 84.6% to 92.9%. As shown in Table 4, the combination of ALB, CRP, and PCT was more effective in diagnosing neonatal sepsis than CRP alone or CRP and PCT alone. The combination of CRP, PCT, and ALB was compared with combinations of other infection indicators, and the AUC of the CRP+PCT+ALB (AUC=0.834) combination was found to be superior to that of the CRP+PCT (AUC=0.826), CRP+ALB (AUC=0.795), and PCT+ALB (AUC=0.749) combinations. Therefore, the CRP+PCT+ALB combination had better diagnostic efficacy. Importantly, although the AUC of the CRP+PCT+ALB combination was smaller than that of the CRP+PCT+ALB+WBC (AUC=0.837) combination, there was no significant difference between the two, and the specificity of the CRP+PCT+ALB (92.9%) combination was higher than that of the CRP+PCT+ALB+WBC (89.5%) combination, indicating that the combination of CRP+PCT+ALB was more valuable. In conclusion, the ALB index is useful for the diagnosis of neonatal sepsis, especially when combined with CRP and PCT levels and the WBC count. In the baseline data of this study, the differences in age, sex and weight were statistically significant. Our study analysed the influence of these factors on ALB, CRP, and PCT levels and the WBC count in neonatal sepsis diagnosis to avoid interference caused by these factors. Age, sex, and weight were corrected in the multivariate logistic regression analysis. The results indicated that age, sex, and weight did not affect the diagnostic efficacy of ALB, CRP and PCT levels for neonatal sepsis, but the WBC count did.
There are also some limitations in this study. The neonatal infection group in this study was relatively young, and there may be selection bias. In addition, this study did not analyse full-term infants versus premature infants or early-onset sepsis versus late-onset sepsis separately, which may have affected the results because there are differences in the values between preterm and full-term infants. The next step for our research group is to perform stratified analysis based on gestational age.
Conclusions
ALB is valuable in diagnosing neonatal sepsis, especially in distinguishing neonatal infection from neonatal sepsis. In the absence of blood culture results, the combined detection of ALB, CRP, and PCT levels has relatively high sensitivity and specificity. Therefore, the combination of these inflammatory biomarkers can be used to diagnose neonatal sepsis early, which can help clinicians distinguish neonatal infection from neonatal sepsis early and use antibiotics rationally. Although the application of this combined index has certain value, blood culture remains the gold standard for the diagnosis of neonatal sepsis.
Data Sharing Statement
Upon reasonable request, the corresponding author can provide the datasets used and/or analysed during the current study.
Ethics Approval and Consent to Participate
The Affiliated Foshan Maternity & Child Healthcare Hospital’s Ethics Committee approved this study. The data collected for this study were retrospectively collected, and the datasets were completely anonymized before analysis. The Hospital’s Academic Board waived the need for consent.
Acknowledgments
We thank Da-zhi Fan for his many suggestions regarding this article.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Foshan Self-funded Science and Technology Plan Project (No: 2220001004133).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Artigas A, Wernerman J, Arroyo V, Vincent J-L, Levy M. Role of albumin in diseases associated with severe systemic inflammation: pathophysiologic and clinical evidence in sepsis and in decompensated cirrhosis. J Crit Care. 2016;33:62–70. doi:10.1016/j.jcrc.2015.12.019
2. Chauhan N, Tiwari S, Jain U. Potential biomarkers for effective screening of neonatal sepsis infections: an overview. Microb Pathog. 2017;107:234–242. doi:10.1016/j.micpath.2017.03.042
3. Dandona P, Nix D, Wilson MF, et al. Procalcitonin increase after endotoxin injection in normal subjects. J Clin Endocrinol Metab. 1994;79:1605–1608. doi:10.1210/jcem.79.6.7989463
4. Sharma D, Farahbakhsh N, Shastri S, Sharma P. Biomarkers for diagnosis of neonatal sepsis: a literature review. J Maternal-Fetal Neonatal Med. 2018;31:1646–1659. doi:10.1080/14767058.2017.1322060
5. Eschborn S, Weitkamp J-H. Procalcitonin versus C-reactive protein: review of kinetics and performance for diagnosis of neonatal sepsis. J Perinatol. 2019;39:893–903. doi:10.1038/s41372-019-0363-4
6. Brown JVE, Meader N, Wright K, Cleminson J, McGuire W. Assessment of C-reactive protein diagnostic test accuracy for late-onset infection in newborn infants. JAMA Pediatr. 2020;174:260. doi:10.1001/jamapediatrics.2019.5669
7. Patel K, McElvania E. Diagnostic challenges and laboratory considerations for pediatric sepsis. J Appl Lab Med. 2019;3:587–600. doi:10.1373/jalm.2017.025908
8. Donini LM, Savina C, Ricciardi LM, et al. Predicting the outcome of artificial nutrition by clinical and functional indices. Nutrition. 2009;25:11–19. doi:10.1016/j.nut.2008.07.001
9. Eckart A, Struja T, Kutz A, et al. Relationship of nutritional status, inflammation, and serum albumin levels during acute illness: a prospective study. Am J Med. 2020;133:713–722.e7. doi:10.1016/j.amjmed.2019.10.031
10. Soeters PB, Wolfe RR, Shenkin A. Hypoalbuminemia: pathogenesis and clinical significance. J Parenteral Enteral Nutr. 2019;43:181–193. doi:10.1002/jpen.1451
11. Don BR, Kaysen G. Poor nutritional status and inflammation: serum albumin: relationship to inflammation and nutrition. Semin Dial. 2004;17:432–437. doi:10.1111/j.0894-0959.2004.17603.x
12. Omiya K, Sato H, Sato T, et al. Albumin and fibrinogen kinetics in sepsis: a prospective observational study. Crit Care. 2021;25:436. doi:10.1186/s13054-021-03860-7
13. Arnau-Barrés I, Güerri-Fernández R, Luque S, Sorli L, Vázquez O, Miralles R. Serum albumin is a strong predictor of sepsis outcome in elderly patients. Eur J Clin Microbiol Infect Dis. 2019;38:743–746. doi:10.1007/s10096-019-03478-2
14. Qian S, Liu J. 脓毒症/严重脓毒症/脓毒性休克患儿血清白蛋白水平与预后关系的研究 [Relationship between serum albumin level and prognosis in children with sepsis, severe sepsis or septic shock]. Zhonghua Er Ke Za Zhi. 2012;50:184–187. Chinese.
15. Goldstein B, Giroir B, Randolph A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics*. Pediatr Crit Care Med. 2005;6:2–8. doi:10.1097/01.PCC.0000149131.72248.E6
16. Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet. 2017;390:1770–1780. doi:10.1016/S0140-6736(17)31002-4
17. Kim F, Polin RA, Hooven TA. Neonatal sepsis. BMJ. 2020;m3672. doi:10.1136/bmj.m3672
18. Subspecialty Group of Neonatology, the Society of Pediatric, Chinese Medical Association, Professional Committee of Infectious Diseases, Neonatology Society, Chinese Medical Doctor Association. Expert consensus on the diagnosis and management of neonatal sepsis (version 2019). Zhonghua Er Ke Za Zhi. 2019;57:252–257. doi:10.3760/cma.j.issn.0578-1310.2019.04.005
19. Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: when? Where? Why? Lancet. 2005;365:891–900. doi:10.1016/S0140-6736(05)71048-5
20. American College of Emergency Physicians Clinical Policies Committee, American College of Emergency Physicians Clinical Policies Subcommittee on Pediatric Fever. Clinical policy for children younger than three years presenting to the emergency department with fever. Ann Emerg Med. 2003;42:530–545. doi:10.1067/S0196-0644(03)00628-0
21. Bouadma L, Luyt C-E, Tubach F, et al. Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet. 2010;375:463–474. doi:10.1016/S0140-6736(09)61879-1
22. PubMed. Diagnostic value of simultaneous measurement of procalcitonin, interleukin-6 and hs-CRP in prediction of early-onset neonatal sepsis; 2022. Available from: https://pubmed.ncbi.nlm.nih.gov/22708043/.
23. Ruan L, Chen G-Y, Liu Z, et al. The combination of procalcitonin and C-reactive protein or presepsin alone improves the accuracy of diagnosis of neonatal sepsis: a meta-analysis and systematic review. Crit Care. 2018;22:316. doi:10.1186/s13054-018-2236-1
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
