Back to Journals » International Journal of General Medicine » Volume 15
The Relationship Between Vitamin D and Activity of Daily Living in the Elderly
Authors Li H, Han D, Wang H, Shu D, Xu L, Hou L, Xu Y , Lai X
Received 12 March 2022
Accepted for publication 13 July 2022
Published 1 August 2022 Volume 2022:15 Pages 6357—6364
DOI https://doi.org/10.2147/IJGM.S366203
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Han Li,1 Dongmei Han,1 Haiyan Wang,2 Dan Shu,1 Lei Xu,1 Liufang Hou,1 Ying Xu,2 Xueli Lai2
1The Rehabilitation Department of Nephrology, The First Rehabilitation Hospital of Shanghai, Shanghai, People’s Republic of China; 2Department of Nephrology, Shanghai Changhai Hospital, Shanghai, People’s Republic of China
Correspondence: Ying Xu; Xueli Lai, Department of Nephrology, Shanghai Changhai Hospital, Shanghai, 200433, People’s Republic of China, Email [email protected]; [email protected]
Objective: To analyze the association between vitamin D and the performance of activity of daily living in the elderly.
Methods: A total of 94 patients over the age of 65 were eligible to participate if they had undergone a bone mineral density test and if they were in a stable health condition. Subjects were further divided into two groups according to activity of daily living (ADL): the score over 40 of the patients as the high ADL group and the below as the low ADL group.
Results: According to univariate analysis, the mean of total hip T score, serum creatinine/cystatin C ratio (CCR), and vitamin D were significantly different between the two groups (P=0.024, 0.008, 0.010). Multivariate ORs showed that the CCR (OR: 0.948; 95%CI: 0.910– 0.989; P=0.013) and vitamin D (OR: 865; 95%CI: 0.752– 0.994; P=0.047) were inversely associated with having low ADL. Furthermore, on multiple linear regression analysis, the Barthel ADL index was related to geriatric nutritional risk index (GNRI), CCR and vitamin D but independent of patients’ age with the slope of 0.732, 0.539, and 0.689 separately, reflected the stronger relative within the variables.
Conclusion: We demonstrated that there is a negative correlation of CCR and vitamin D with having low ADL in elderly population. Monitoring the trend of serum vitamin D and CCR, may have a role in the early detection of low ADL with loss of muscle mass and strength in the population of the elderly.
Keywords: vitamin D, CCR, elderly, ADL, muscle mass
Introduction
With the improvement of the public health and lifestyle, human life expectancy has doubled in most developed countries1 and is projected to continue to increase.2 Caring for the elderly and their physical activities in their remaining life expectancy are deficiently addressed and growing emphasis on the life quality of the elderly is appreciated. Progressive and generalized loss of skeletal muscle mass and strength resulting in the risk of adverse outcomes such as function decline, poor quality of life and mortality is widely put forward in the elderly.3,4 Optimized methods to evaluate the frailty accurately and rapidly in the elderly are critical for prediction, diagnosis and treatment of the potential and explicit physical disability.
Activities of daily living (ADL) play a crucial role in the determination of the health status of elderly and are used extensively as measurement tools in clinical approaches.5 Ten personal activities involved include feeding, personal toileting, bathing, dressing and undressing, getting on and off a toilet, controlling bladder, controlling bowel, moving from wheelchair to bed and returning, walking on level surface (or propelling a wheelchair if unable to walk) and ascending and descending stairs.6,7 Hence, such activities are considered significant in revealing the underlying functional status of elderly and functional mobility is used as an assessment tool for risk of fall and frailty.5
Skeletal muscle mass is essential for maintaining physical function and performing ADL.8 Vitamin D is becoming a common trend and a much-discussed topic in skeletal muscle mass, even sarcopenia research. In cellular models, a variety of mechanisms by which vitamin D interferes with skeletal muscle function has been elucidated: (1) genomic effects arising from the interaction of the 1,25-VDR-RXR heterodimer at specific nuclear receptors that influence gene transcription; (2) non-genomic effects, characterized by rapid activation followed by other complex pathways of intracellular signal transduction after binding of 1,25- (OH)-D to its non-nuclear receptor.9 There are systematic review and meta-analysis of randomized controlled trials raised that vitamin D supplementation has a small positive impact on muscle strength,10 even vitamin D supplementation did not improve any sarcopenia indices in community-dwelling older adults and may compromise some aspects of physical performance.11 However, a lack of clinically compelling evidence linking to muscle mass and even muscle metabolism and a lack of consensus on the pathological serum level and supplements of vitamin D on the muscle aspects still exist.
The current study was designed to investigate the association between the serum level of vitamin D and musculoskeletal-related factors and ADL to assess the vitamin D-deficient loss of muscle mass and ADL disability.
Method
Study Design and Participants
The cross-sectional study was conducted at The First Rehabilitation Hospital of Shanghai. A total of 94 patients over the age of 65 were eligible to participate if they had undergone a bone mineral density test and if they were in a stable health condition. Key exclusion criteria were disturbance of consciousness, severe dementia, and the acute phase of disease.
The informed consent was signed by all the patients or their legally representative if they could not sign it. The study protocol was approved by The First Rehabilitation Hospital Ethics Committee and was performed in accordance with the Helsinki Declaration.
Investigation
Demographic and clinical information collected for all patients included gender, age, habits of smoking and alcohol, history of hypertension and diabetes mellitus, and fracture status.
Each patient underwent blood drawing for laboratory parameters including albumin (Alb), blood urea nitrogen (BUN), uric acid (UA), serum creatine (SCr), cystatin C (CysC), serum calcium (Ca), serum phosphorus (P), parathyroid hormone (PTH), osteocalcin, vitamin D (VitD), homocysteine (HCY), thyroid stimulating hormone (TSH), total cholesterol (TC), fasting glucose (FP), and alkaline phosphatases (ALP). Urine specimen was obtained to measure urine protein (UP) and uromicroprotein (UMP).
Height, weight, waist circumference, and hip circumference of all the participants were measured by the well-trained nurses in a standard process. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Waist/hip ratio (WHR) was calculated as waist circumference divided by hip circumference. A skinfold caliper was used for the measurement of waist skinfold thickness for the estimation of the total amount of body fat.
Bone Mineral Density
Regional BMD, including lumbar spine, femoral neck, and total hip, were measured using dual-energy X-ray absorptiometry (DXA). To minimize interobserver variation, all scans and analyses were conducted by the same investigator. The densitometer was standardized by a standard phantom prior to each measurement. Osteopenia is diagnosed by a −2.5<T score<−1.0 standard deviation (SD), and osteoporosis by a T score≤−2.5 SD at any of the sites on the lumbar spine, femoral neck, or total hip.12
Assessment of Activities of Daily Living
The performance of participants in ADL was measured by the Barthel index (BI), commonly used in rehabilitation facilities, which is an ordinal scale comprised of 10 variables of mobility and selfcare to assess the degree of assistance. The original Index is a three-item ordinal rating scale completed by the observer. Each item is rated in terms of whether the patient can perform the task independently, with some assistance, or is dependent on help based on observation (0=unable, 1=needs help, 2=independent). The final score based on the obtained number to time 5 ranged in a 100-point score. The proposed method of interpreting BI is that scores of less than 20 indicate totally dependent, 20–39 indicate very dependent, 40–59 indicate partially dependent, 60–79 indicate minimally dependent and 80–100 indicate independent.13 Therefore, we designated the score over 40 of the patients as the high ADL group and the below as the low ADL group.
Assessment of Nutritional Status
Geriatric nutritional risk index was applied with the formula of GNRI=1.489×albumin (g/L) +41.7× (current/ ideal weight), with which individuals less than 92 were assigned to the malnutrition group and more than 92 were assigned to the normal group with mild or no risk of malnutrition.14
Karnofsky Performance Scale
The Karnofsky performance scale (KPS) is an 11-point rating scale that ranges from normal functioning (100) to dead (0), increasing by 10 points. It is a widely used assessment tool for functional impairment to predict the length of survival in terminally ill patients. The permanent observer assessed the status of these patients based on the rating criteria.
Statistical Analysis
Statistical analysis was performed with software SPSS 22.0. First of all, Shapiro–Wilk normality test was performed to verify whether data followed normal distribution. The continuous variables are presented in means ± standard deviation (SD) or medians with interquartile range (IQR) when distributions were not normal. Categorical variables are reported in number and percentage. Comparisons between groups were made by Student’s t-test with normally distributed variables, whereas the Mann–Whitney U-test was used otherwise. Categorical data was compared using the chi-squared test. Univariate and multiple logistic regression analysis and stepwise analysis were used. Statistical significance for all analyses was set at P<0.05.
Results
Of 94 people screened for eligibility, 32 male (34.0%) and 62 female participants were included in the study. The clinical information of the study population was summarized in Table 1. Although they were elderly, the difference of the mean age with 85.28 years old in the low ADL group and 82.39 years old in the high ADL group, was statistically significant (P=0.026). There was no significant difference between the groups in median total score of the GNRI. Similarly, there was no difference between the groups regarding history of hypertension, diabetes or fracture. What stands out in the table was that the mean of total hip T score, CCR, and vitamin D were significantly different between two groups (P=0.024, 0.008, 0.010). It was worth emphasizing that total hip T in the low ADL group was less than −2.50 and was −2.30 in the high ADL group, which represented the osteoporosis and osteopenia in both research group.
 |
Table 1 Patients Characteristics |
Multivariate ORs for having low ADL are shown in Table 2. Although age was not associated with an incremental risk of low ADL (OR: 1.014; 95%CI: 0.956–1.075; P=0.647), the CCR (OR: 0.948; 95%CI: 0.910–0.989; P=0.013) and vitamin D (OR: 865; 95%CI: 0.752–0.994; P=0.047) were inversely associated with having low ADL.
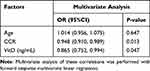 |
Table 2 Factors Associated with the Risk of Low ADL |
The Barthel ADL index was related to GNRI, CCR and vitamin D (Table 3) but independent of patients’ age with the slope of 0.732, 0.539, and 0.689 separately, reflected the stronger relative within the variables (Table 3).
 |
Table 3 Multiple Linear Regression Analysis of ADL |
Discussion
This study provided a basis and thinking method for assessing low level activity of daily living with serum vitamin D in elderly population. To our knowledge there are few reports in the literature with the aspect of serological markers, musculoskeletal-related factors and ADL. The current study showed that CCR and vitamin D were negatively related with having low ADL.
Recently, CCR has been postulated as the surrogate marker of sarcopenia in diverse populations.15–17 As is well known, serum creatinine is a waste product left over from energy-producing processes in the muscle, occurring in the muscle cells of vertebrates as the only intermediate product of creatine metabolism.18 Cystatin C is produced in the nucleated cells in a constant amount, and its serum concentration does not depend on muscle mass and protein intake.19 That is to say, the considerable muscle tissue that can metabolize Scr, the better the muscle strength and coordination, the less low ADL appears. As an indicator rarely used in clinical, the research of CCR brings us a new sight of muscle mass and strength, laying a new foundation for subsequent molecular research.
In the previous observational study enrolling 4630 community-dwelling adults proposed that dynapenia only and dynapenia combined with low 25 (OH) D serum levels were important risk factors for ADL disability in middle-aged individuals and older adults in two years of follow-up.20 The association between low ADL and vitamin D is often overlooked in the elderly population over 80 years of age. Although there are many factors that contribute to ADL disability and decreased muscle strength in the elderly population for various reasons, vitamin D cannot be ignored. A certain amount of mechanism of vitamin D on skeletal muscle function has been elaborated on the cellular level. A previous study examined the concentration and time-dependent effects of calcitriol on the capacity of muscle cells to take up and release 25(OH) D3, showed an evidence that skeletal muscle cells indeed contain a mobile pool of 25(OH) D3 which accumulates from and returns to the extracellular environment.21 Furthermore, they hypothesized that storage and gradual release from muscles would increase the level of circulating 25(OH) D3 and this would maintain adequate status during the months when vitamin D supply was low giving skeletal muscles a pivotal role in the maintenance of vitamin D status.21–23 Much of the biological function of the active form of vitamin D3 is mediated by vitamin D receptor (VDR), a protein that effectively binds 1α,25(OH)2 D3 at a sub-nanomolar concentration.24,25 However, serum 25(OH) D3 levels and the expression of VDR in muscle cells decline with age,26 which may lead to muscle weakness and onset of sarcopenia.27 VDR is predominantly on the fast-twitch muscle fibers, which respond first in rapid actions, thus adequate vitamin D may improve the strength and coordination.28,29 A study of human muscles showed that vitamin D deficiency induced atrophy and decreases the concentration of intramyonucelar VDR and VDR gene expression level.30 Thus, low level of vitamin D may reduce muscle mass, strength and coordination, or lower level activity of daily living. Vitamin D may regulate oxygen consumption and dynamics of mitochondria. Prior research has documented that skeletal muscle cells treated with 1α,25(OH)2 D3 increased oxygen consumption rate (OCR), suggesting that vitamin D increases the function of mitochondria in muscle.31 The vitamin D influence on mitochondria was also reported by Sinha et al who showed that treatment of vitamin D deficient humans with cholecalciferol improves the maximal mitochondrial oxidative phosphorylation rate measured by 31P-NMR spectroscopy.32 Moreover, a recent study on patients with chronic low back pain showed that vitamin D deficiency increases antioxidative enzymes activities and after five-week vitamin D supplementation, oxidative stress decreased in skeletal muscle.33 Another relevant study34 indicated that rats treated with vitamin D showed reduced tissue damage and attenuated oxidative stress after exhaustive exercise, supporting that vitamin D is involved not only in calcium homeostasis and mitochondrial function, but also is responsible for oxidative stress in skeletal muscle. By reason of the foregoing, a low level of serum vitamin D acts as an indispensable and direct factor that contributes to the skeletal muscle dysfunction and lessened muscle mass even sarcopenia.
In addition, decreased vitamin D intake and metabolism due to decreased physical strength, eating disorders, and activity limitations in older adults. Hibler et al put forward that physical activity and serum 1,25(OH)2D levels has positive relationship35 which suggested behavior change is essential.
There are several limitations that should be mentioned. First, because we did not have data of muscle mass or strength, we could not directly investigate a relationship of vitamin D and CCR with it. Second, the present study had a cross-sectional design with the small sample size. Third, we did not take the daily nutrients intake into consideration.
Conclusion
In summary, we demonstrated that there is a negative correlation of CCR and vitamin D with having low ADL in elderly population. Low serum level of vitamin D appears to be the marker of risk of functional decline in ADL for elderly. Monitoring the trend of serum vitamin D and CCR, may have a role in the early detection for low ADL with loss of muscle mass and strength in the elderly population.
Acknowledgments
This research was funded by National Natural Science Foundation of China (61801329 and 81800678); Project of the Science and Technology Commission of Yangpu District, Shanghai, and Key Specialist of Yangpu District, Shanghai (YP19ZB05), China; Youth Cultivation Project of Naval Medical University Nursing Science (18QPFH10).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Partridge L, Deelen J, Slagboom PE. Facing up to the global challenges of ageing. Nature. 2018;561(7721):45–56. doi:10.1038/s41586-018-0457-8
2. Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet. 2017;389(10076):1323–1335. doi:10.1016/S0140-6736(16)32381-9
3. Delmonico MJ, Harris TB, Lee JS, et al. Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. J Am Geriatr Soc. 2007;55(5):769–774. doi:10.1111/j.1532-5415.2007.01140.x
4. Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393(10191):2636–2646. doi:10.1016/S0140-6736(19)31138-9
5. Panhwar YN, Naghdy F, Naghdy G, Stirling D, Potter J. Assessment of frailty: a survey of quantitative and clinical methods. BMC Biomed Eng. 2019;1:7. doi:10.1186/s42490-019-0007-y
6. Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–65.
7. Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989;42(8):703–709.
8. Buford TW, Anton SD, Clark DJ, Higgins TJ, Cooke MB. Optimizing the benefits of exercise on physical function in older adults. PM R. 2014;6(6):528–543. doi:10.1016/j.pmrj.2013.11.009
9. Garcia M, Seelaender M, Sotiropoulos A, Coletti D, Lancha AH
10. Beaudart C, Buckinx F, Rabenda V, et al. The effects of vitamin D on skeletal muscle strength, muscle mass, and muscle power: a systematic review and meta-analysis of randomized controlled trials. J Clin Endocrinol Metab. 2014;99(11):4336–4345. doi:10.1210/jc.2014-1742
11. Prokopidis K, Giannos P, Katsikas Triantafyllidis K, et al. Effect of vitamin D monotherapy on indices of sarcopenia in community-dwelling older adults: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2022;13(3):1642–1652. doi:10.1002/jcsm.12976
12. Siris ES, Adler R, Bilezikian J, et al. The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporos Int. 2014;25(5):1439–1443. doi:10.1007/s00198-014-2655-z
13. Sinoff G, Ore L. The Barthel activities of daily living index: self-reporting versus actual performance in the old-old (> or = 75 years). J Am Geriatr Soc. 1997;45(7):832–836. doi:10.1111/j.1532-5415.1997.tb01510.x
14. Bouillanne O, Morineau G, Dupont C, et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005;82(4):777–783. doi:10.1093/ajcn/82.4.777
15. Osaka T, Hamaguchi M, Hashimoto Y, et al. Decreased the creatinine to cystatin C ratio is a surrogate marker of sarcopenia in patients with type 2 diabetes. Diabetes Res Clin Pract. 2018;139:52–58. doi:10.1016/j.diabres.2018.02.025
16. Lin YL, Chen SY, Lai YH, et al. Serum creatinine to cystatin C ratio predicts skeletal muscle mass and strength in patients with non-dialysis chronic kidney disease. Clin Nutr. 2020;39(8):2435–2441. doi:10.1016/j.clnu.2019.10.027
17. Tetsuka S, Morita M, Ikeguchi K, Nakano I. Creatinine/cystatin C ratio as a surrogate marker of residual muscle mass in amyotrophic lateral sclerosis. Neurol Clin Neurosci. 2013;1(1):32–37. doi:10.1002/ncn3.11
18. Feher J. 7.4 - Tubular reabsorption and secretion. In: Feher J, editor. Quantitative Human Physiology.
19. Čabarkapa V. CYSTATIN C - More than the marker of the glomerular filtration rate. Med Pregl. 2015;68(5–6):173–179. doi:10.2298/MPNS1506173C
20. Borim FSA, Alexandre TDS, Neri AL, Máximo RO, Silva MF, de Oliveira C. Combined effect of dynapenia (Muscle Weakness) and low Vitamin D status on incident disability. J Am Med Dir Assoc. 2019;20(1):47–52. doi:10.1016/j.jamda.2018.06.006
21. Abboud M, Puglisi DA, Davies BN, et al. Evidence for a specific uptake and retention mechanism for 25-hydroxyvitamin D (25OHD) in skeletal muscle cells. Endocrinology. 2013;154(9):3022–3030. doi:10.1210/en.2012-2245
22. Abboud M, Rybchyn MS, Ning YJ, et al. 1,25-Dihydroxycholecalciferol (calcitriol) modifies uptake and release of 25-hydroxycholecalciferol in skeletal muscle cells in culture. J Steroid Biochem Mol Biol. 2018;177:109–115. doi:10.1016/j.jsbmb.2017.10.018
23. Abboud M, Rybchyn MS, Liu J, et al. The effect of parathyroid hormone on the uptake and retention of 25-hydroxyvitamin D in skeletal muscle cells. J Steroid Biochem Mol Biol. 2017;173:173–179. doi:10.1016/j.jsbmb.2017.01.001
24. Haussler MR, Haussler CA, Jurutka PW, et al. The vitamin D hormone and its nuclear receptor: molecular actions and disease states. J Endocrinol. 1997;154(Suppl):S57–73.
25. Dusso AS, Brown AJ, Slatopolsky E. Vitamin D. Am J Physiol Renal Physiol. 2005;289(1):F8–28. doi:10.1152/ajprenal.00336.2004
26. Bischoff-Ferrari HA, Borchers M, Gudat F, Dürmüller U, Stähelin HB, Dick W. Vitamin D receptor expression in human muscle tissue decreases with age. J Bone Miner Res. 2004;19(2):265–269. doi:10.1359/jbmr.2004.19.2.265
27. Lips P, Binkley N, Pfeifer M, et al. Once-weekly dose of 8400 IU vitamin D(3) compared with placebo: effects on neuromuscular function and tolerability in older adults with vitamin D insufficiency. Am J Clin Nutr. 2010;91(4):985–991. doi:10.3945/ajcn.2009.28113
28. Suzuki T, Kwon J, Kim H, et al. Low serum 25-hydroxyvitamin D levels associated with falls among Japanese community-dwelling elderly. J Bone Miner Res. 2008;23(8):1309–1317. doi:10.1359/jbmr.080328
29. Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–1930. doi:10.1210/jc.2011-0385
30. Bang WS, Lee DH, Kim KT, et al. Relationships between vitamin D and paraspinal muscle: human data and experimental rat model analysis. Spine J. 2018;18(6):1053–1061. doi:10.1016/j.spinee.2018.01.007
31. Ryan ZC, Craig TA, Folmes CD, et al. 1α,25-Dihydroxyvitamin D3 regulates mitochondrial oxygen consumption and dynamics in human skeletal muscle cells. J Biol Chem. 2016;291(3):1514–1528. doi:10.1074/jbc.M115.684399
32. Sinha A, Hollingsworth KG, Ball S, Cheetham T. Improving the vitamin D status of vitamin D deficient adults is associated with improved mitochondrial oxidative function in skeletal muscle. J Clin Endocrinol Metab. 2013;98(3):E509–513. doi:10.1210/jc.2012-3592
33. Dzik K, Skrobot W, Flis DJ, et al. Vitamin D supplementation attenuates oxidative stress in paraspinal skeletal muscles in patients with low back pain. Eur J Appl Physiol. 2018;118(1):143–151. doi:10.1007/s00421-017-3755-1
34. Ke CY, Yang FL, Wu WT, et al. Vitamin D3 reduces tissue damage and oxidative stress caused by exhaustive exercise. Int J Med Sci. 2016;13(2):147–153. doi:10.7150/ijms.13746
35. Hibler EA, Sardo Molmenti CL, Dai Q, et al. Physical activity, sedentary behavior, and vitamin D metabolites. Bone. 2016;83:248–255. doi:10.1016/j.bone.2015.11.016
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
