Back to Journals » Neuropsychiatric Disease and Treatment » Volume 16
The Relationship Between Symptoms of Anxiety and Somatic Symptoms in Health Professionals During the Coronavirus Disease 2019 Pandemic
Authors Li H, Zhang Y, Wang H, Liang J, Zhou Y, Huang Y , Zhai T, Yang Q, Yang M, Ning Y, He H, Wu K , Chen F, Wu F , Zhang X
Received 15 September 2020
Accepted for publication 4 December 2020
Published 18 December 2020 Volume 2020:16 Pages 3153—3161
DOI https://doi.org/10.2147/NDT.S282124
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
Hehua Li,1,* Yaping Zhang,2,3,* Honggang Wang,4 Jing Liang,4 Yongjie Zhou,2,3 Yuanyuan Huang,1 Tianyi Zhai,1 Qiong Yang,1 Mingzhe Yang,1 Yuping Ning,1,5 Hongbo He,1 Kai Wu,6 Fengjuan Chen,7 Fengchun Wu,1,5,8 Xiangyang Zhang1,9
1Department of Psychiatry, The Affiliated Brain Hospital of Guangzhou Medical University, Guangzhou, People’s Republic of China; 2Research Center for Psychological and Health Sciences, China University of Geosciences, Wuhan, People’s Republic of China; 3Affiliated Wuhan Mental Health Center, Tongji Medical College of Huazhong University of Science & Technology, Wuhan, People’s Republic of China; 4Qingdao Mental Health Center, Qingdao University, Qingdao, People’s Republic of China; 5The First School of Clinical Medicine, Southern Medical University, Guangzhou, People’s Republic of China; 6Department of Biomedical Engineering, School of Materials Science and Engineering, South China University of Technology (scUT), Guangzhou, People’s Republic of China; 7Department of Medical, Guangzhou Eighth People’s Hospital, Guangzhou Medical University, Guangzhou, People’s Republic of China; 8Guangdong Engineering Technology Research Center for Translational Medicine of Mental Disorders, Guangzhou, People’s Republic of China; 9CAS Key Laboratory of Mental Health, Institute of Psychology, Chinese Academy of Sciences, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Fengchun Wu
Institute of Psychology, The Affiliated Brain Hospital of Guangzhou Medical University, Liwan District, Guangzhou 510370, People’s Republic of China
Email [email protected]
Xiangyang Zhang
Institute of Psychology, Chinese Academy of Sciences, Chaoyang District, Beijing 100101, People’s Republic of China
Email [email protected]
Background: The pandemic of coronavirus disease 2019 (COVID-19) has posed a threat to global health. Increasing studies have shown that the mental health status of health professionals is very poor during the COVID-19 epidemic. At present, the relationship between somatic symptoms and symptoms of anxiety of health professionals during the COVID-19 has not been reported. The purpose of this study was to explore the frequency of somatic symptoms and its related factors in health professionals with symptoms of anxiety during COVID-19 in China.
Methods: A total of 606 health professionals were assessed online with the Chinese version of the 7-item Generalized Anxiety Disorder (GAD-7) scale, 7-item Insomnia Severity Index (ISI) and the somatization subscale of Symptom Checklist 90 (SCL-90).
Results: The percentage of symptoms of anxiety, somatic symptoms and insomnia in all health professionals was 45.4%, 12.0%, and 32%, respectively. The frequency of somatic symptoms in health professionals with symptoms of anxiety was 22.9%. The SCL-90 somatization subscale score was significantly positively correlated with history of somatic diseases, GAD-7 score and ISI score in participants with symptoms of anxiety.
Conclusion: During the COVID-19, symptoms of anxiety, insomnia, and somatic symptoms are commonly observed in health professionals. Insomnia and symptoms of anxiety are independently associated with somatic symptoms of health professionals with symptoms of anxiety.
Keywords: somatic symptoms, coronavirus disease 2019, health professionals, frequency, related factors
Introduction
A new type of severe acute respiratory syndrome (SARS) type 2 (SARS-CoV-2) disease (COVID-19) was identified as a pandemic by the World Health Organization (WHO) on March 11, 2020,1 which is one of the most serious epidemics since the 2002–2003 SARS and the 2012 Middle East respiratory syndrome (MERS) pandemic. In recent days, the epidemic has spread rapidly in many countries around the world, posing a threat to global health. According to the data of WHO on April 5, more than 1.13 million cases of COVID-19 have been confirmed, and more than 200 countries and regions have been affected by the epidemic. However, to date, specific antiviral drugs and vaccines for COVID-19 control are still not available.2
Due to the sudden outbreak of the epidemic, health professionals have been facing huge pressure to be infected with COVID-19. They are very prone to physical fatigue, fear, mood disorders, and insomnia.3 A study including 1563 medical workers recently reported that 50.7% of them had depression, 44.7% had symptoms of anxiety and 36.1% suffered from sleep disorder.4 Another study involving 1257 medical workers showed that depression, symptoms of anxiety, pain, and insomnia accounted for 50.4%, 44.6%, 71.5%, and 34.0%, respectively.5 One most recent study reported that 36.9% of the health professionals suffered from mental health problems.6 A recent systematic review and meta-analysis of 13 studies showed that the comprehensive prevalence rates of anxiety, depression, and insomnia were 23.2%, 22.8%, and 38.9%, respectively. Moreover, 36.3%, 50.4%, and 17.5% of all participants had access to psychological information, psychological resources available through media, and counseling or psychotherapy.6 During the epidemic of MERS and SARS, the psychological burden of health professionals was also reported, showing that health professionals were worried about family members, friends, and colleagues being infected.8,9 In addition, studies during MERS showed that a large proportion of health professionals were afraid of being infected with MERS.10
With the increasing severity of international epidemic, there is still no hope of ending the epidemic, so they are still under increasing pressure. Stress may reduce the synthesis and release of monoamines in the brain, leading to increased anxiety behavior.11 The latest research conducted on patients with mood disorders during COVID-19 showed that low serum 25-hydroxyvitamin D levels were significantly associated with higher psychological stress.12 There is growing evidence to support the link between pressure and somatic symptoms. Somatic symptoms are the manifestations of psychological stress, which is manifested as physiological symptoms.13 Higher levels of somatic symptoms are related to generalized anxiety disorder (GAD).14,15 In addition, the study in the Chinese population has reported that high symptoms of anxiety and severe insomnia are important stressors that may add the danger of somatic symptoms.16 Anxiety is closely related to somatic symptoms. Means-Christensen et al showed that patients who reported pain symptoms were more likely to develop anxiety, while those patients reported pain may have undiagnosed anxiety.17 However, to date, patients with multiple somatic symptoms are still a challenge for clinicians.18
Currently, studies on the mental health status of health professionals during the COVID-19 epidemic, including meta-analyses, mostly focus on depression, anxiety, and insomnia. During the COVID-19 epidemic, there are few reports on the combination of anxiety symptoms and somatic symptoms among health professionals, and the research on its influencing factors is even rarer. Understanding the relationship between different mental states can help improve the mental health of health professionals. Therefore, this study aimed to explore the prevalence and related factors of somatic symptoms, anxiety symptoms, and insomnia among health professionals in many regions in China, and provide an important basis for guiding and improving the mental health of health professionals.
Methods
Participants and Study Design
We used an anonymous online questionnaire to assess the health professional’s mental health status through a cross-sectional design. The Ethics Committee of the Institute of Psychology, Chinese Academy of Sciences reviewed and approved this design. Our study was conducted in accordance with the Declaration of Helsinki. This online survey was originally distributed among health professionals across the country. The questionnaire was passed on through mutual transmission between health professionals. All survey participants provided informed consent before answering questions, and they could terminate the investigation as they wished at any time. The data collection was carried out during the period when the Chinese government decided to gradually resume work and production (February 14 to March 22, 2020).
Self-Measurement
The socio-demographic collection included: gender, age, height, weight, ethnicity, marital status, education level, city of residence, occupation (physician, medical technician, or nurse), daily working hours, annual family income, history of somatic diseases, experience of SARS epidemic), and infection with COVID-19 in relatives and friends. In addition, body mass index (BMI) was calculated according to height and weight. Moreover, health professionals came from a tertiary hospital or a secondary hospital. According to the hospital’s policy during COVID-19, the staff of the emergency department and the infection department directly faced patients with fever, and they were more likely to contact COVID-19 patients. Therefore, they were classified as first-line workers, while others were classified as second-line workers.
In this study, symptoms of anxiety, somatic symptoms, and insomnia of health professionals were evaluated with the Chinese version of the 7-item Generalized Anxiety Disorder (GAD-7) scale, somatization subscale of Symptom Checklist 90 (SCL-90), and 7-item Insomnia Severity Index (ISI). They have been tested for reliability and validity and have been widely used in Chinese research.5,19–22
GAD-7 is a self-rating scale, which is used to screen for generalized symptoms of anxiety and assess the severity of symptoms. GAD-7 has 7 items with a score of 0 (not at all) ~3 (almost every day). The total score ranges from 0 (nonexistent) to 21 (very serious), and a person with a total score of more than 5 is identified as having symptoms of anxiety.20,23
ISI is used to assess insomnia. The scale’s total score ranges from 0 to 28, and total scores greater than or equal to 8 is defined as insomnia.23
Somatic symptoms are assessed by SCL-90 somatization subscale, including 12 items with a total score of 12 to 60. The severity of somatic symptoms is assessed on a scale of 1 to 5. Each item’s score greater than or equal to 2 indicates potential psychological problems.24 A participant with the somatization subscale of SCL-90 scores greater than or equal to 24 points is identified as having somatic symptoms. The higher the response score, the higher the frequency and intensity of symptoms.
Statistical Analysis
SPSS 18.0 statistical software was used to process the data. Data following a normal distribution were expressed as mean ± standard deviation (SD), and were compared between groups by one-way analysis of variance (ANOVA). The counting data were expressed as proportion (percentage), and the chi-square test was used for the comparison between groups. Rank sum test (Mann–Whitney U) was used to compare rank data. Spearman correlation was used to analyze the relationship between the two variables that were non-normally distributed. Finally, the binary regression equation analysis was used to screen out the relevant factors affecting the occurrence of somatic symptoms in symptoms of anxiety. The statistical significance is set to double-tailed p < 0.05.
Results
Demographic Characteristics
Totally, 606 health professionals were recruited from 73 cities in China. Only 9.4% of the participants came from Hubei Province, whose capital city, Wuhan, reported the first case. Their average age was 35.77±8.13 years. Among the participants, there were much more women (492,81.2%) than men (114,18.8%), including 208 (34.3%) doctors, 334 (55.1%) nurses and 64 (10.6%) medical technicians; 460 (75.9%) participants had bachelor degree or below, and 146 (24.1%) participants had master degree or above; 141 (23.3%) were first-line workers. More than half of participants (322,53.1%) worked more than 8 hours a day; 262 (43.2%) participants had experienced SARS incident; 137 (22.6%) participants suffered from somatic diseases. Only a very small number (13,2.1%) of relatives and friends of the participants were infected with COVID-19.
Among the entire health professionals, the percentage of symptoms of anxiety, somatic symptoms and insomnia was 45.4% (275/606), 12.0% (73/606), and 32% (194/606), respectively. Further, the frequency of somatic symptoms in participants with symptoms of anxiety was 22.9% (63/275). In health professionals with symptoms of anxiety, there was a significant difference in the history of somatic diseases between those with and without somatic symptoms (p=0.007).
However, there were no any significant differences in sex, age, BMI, nationality, marital status, position, education level, daily working hours, annual household income, history of somatic diseases, experience of SARS incident, and infection of COVID-19 in their relatives or friends between participants with and without somatic symptoms (All p>0.05) (Table 1).
 |
Table 1 Socio-Demographics and Self-Measurement Characteristics in Participants of Anxiety Symptoms with and without Somatic Symptoms |
Self-Measurement Characteristics in Participants with Symptoms of Anxiety Combined or Not Combined Somatic Symptoms
Since the original Kolmogorov–Smirnov tests for all scales were p < 0.05, the data were expressed as the median with a interquartile range. In participants with symptoms of anxiety, the Mann–Whitney U-test displayed that scores of GAD-7, SCI-90 somatization subscale, and ISI were significantly higher in participants with somatic symptoms than without somatic symptoms (all p < 0.010) (Table 1). Among participants with symptoms of anxiety combined somatic symptoms, Spearman correlation analysis showed that the SCL-10 somatization subscale score was significantly positively correlated with location (r=0.328, p=0.009), history of somatic diseases (r=0.276, p = 0.029), GAD-7 score (r=0.361, p = 0.004) and ISI score (r=0.451, p < 0.001). However, SCL-10 somatization subscale score was significantly negatively correlated with education level (r=−0.274, p= 0.030).
Among in participants with symptoms of anxiety combined non-somatic symptoms, the SCL-90 somatization subscale score was only positively correlated with history of somatic diseases (r=0.175, p = 0.011) and ISI (r=0.188, p = 0.006).
Factors Related to Somatic Symptoms of Participants with Symptoms of Anxiety
Binary logistic regression was carried out, taking somatic symptoms in participants with symptoms of anxiety as the dependent variable, and statistically significant factors in ANOVA (including ISI score, GAD-7 score and history of somatic diseases) as the independent variables. The results showed that GAD-7 score (OR=1.15; 95% CI: 1.06–1.24) and ISI score (OR=1.14; 95% CI: 1.08–1.21) were independently associated with somatic symptoms (Table 2).
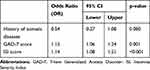 |
Table 2 Factors Related to Somatic Symptoms of Participants with Symptoms of Anxiety by Logistics Regression |
Discussion
To our best knowledge, this study firstly reported the somatic symptoms and related factors in health professionals with symptoms of anxiety in the process of returning to work nationally in China. Our findings included: (1) the frequency of symptoms of anxiety, somatic symptoms and insomnia of health professionals was 45.4%, 12.0%, and 32.0%, respectively. (2) The percentage of somatic symptoms in participants with symptoms of anxiety was 22.9%. (3) The related factors of somatic symptoms in participants with symptoms of anxiety were GAD-7 score and ISI score.
First, our result showed that the percentage of insomnia and symptoms of anxiety was consistent with previous studies among the health professionals mainly in Hubei at the early stage of onset,4,5 but much higher than the frequency (11.9%) of unhealthy psychological tendencies among nurses in China.25 Thus, our finding showed that regardless of whether health professionals in all over China suffered huge psychological pain in the early stage of the COVID-19 epidemic as well as during the resumption of work and production. We should continue to pay attention to mental health status of the health professionals. In addition, few studies have reported the frequency of somatic symptoms in health professionals, whether or not during the outbreak of COVID-19. The percentage of somatic symptoms among the entire health professionals (12.0%) was lower than that of previous studies, such as the general population-based study in China (19.8%),16 and the study of clinical patients in Chinese general hospitals (19.0%–28.0%).26,27 However, it was much higher than the percentage (0.9%) reported by a recent study during the COVID-19 epidemic.28 The frequency of somatic symptoms fluctuates greatly, which was consistent with previous literature reports (range 7.6% to 36.8%).5,29,30 This may be related to the following reasons: (1) Somatic symptoms are complex phenomena, including both physical and psychological aspects.31 In patients with chronic diseases, somatic symptoms are uncomfortable physical symptoms that cannot be entirely attributed to the underlying diseases.32,33 (2) Whether there was a history of somatic diseases among the participants may also be a factor. Our result showed that the somatic history was associated with somatic symptoms in participants with symptoms of anxiety. (3) At present, somatic symptoms were assessed by self-rating scale rather than standardized psychiatric interviews. Creed et al pointed out the limitation of their results that they did not use standardized interviews to determine the existence of mental disorders, so the results could not be compared with the results of such diagnosis.34 In addition, the use of the different rating scales may lead to inconsistent results.35
Our second finding was that the frequency of somatic symptoms in participants with symptoms of anxiety was 22.9%. Our study firstly investigated the frequency of somatic symptoms in health professionals with symptoms of anxiety. A previous survey in the Dutch general population showed that the prevalence rate of somatic symptoms in patients with anxiety disorder, mood disorder and substance use disorder were 19.0%, 13.5%, and 7.1%, respectively.36 One study reported that the frequency of somatic symptoms in patients with anxiety and depression was as high as 50%.37 In addition, there were other studies on the frequency of somatic symptoms in non-mental disorders. Zhang et al reported that the frequency of somatic symptoms of patients with cardiovascular disease in a general hospital in China was 93.1%.22 Ishikawa et al reported that the prevalence of somatic symptoms of general outpatients in a university hospital in Japan was 14.2%.38 Taken together, these results showed that somatic symptoms coexisting in other diseases were an exceptionally common phenomenon. Our results indicated that the frequency of somatic symptoms was relatively high in health professionals with symptoms of anxiety. Löwe et al reported that there was no clear boundary between depression, anxiety, and somatic symptoms.39 In China, somatization was considered to be a manifestation of underlying anxiety and depression.40 However, previous genetics and related studies showed that somatic symptoms occurred independently from anxiety and depression.41–44 In addition, somatic symptoms were correlated with the diagnosis of somatoform disorders.45,46 In DSM and ICD classification, somatoform disorder was still classified as an independent disease.47 Therefore, it was still necessary to explore the influencing factors for somatic symptoms in anxious individuals. Our third finding was that GAD-7 and ISI scores were influential factors for somatic symptoms in health professionals with symptoms of anxiety. So far, there were many studies on factors related to somatic symptoms. However, there has been no research on the risk factors of somatic symptoms comorbid with symptoms of anxiety. Similar results were reported in the somatic symptoms research of the general Chinese population: reducing symptoms of anxiety and improving sleep quality can help relieve somatic symptoms.16 Zhang et al reported that GAD-7 score, PHQ-9 score and women were the related factors for somatic symptoms in outpatients in a general hospital in China.22 Regev et al reported that women showed higher psychological distress in somatic symptoms compared with men, but not in terms of depression and anxiety.48 In addition, a previous study showed that women, the elderly, people with lower levels of education and family income, and fairly remote rural areas were more likely to be associated with somatic symptoms.49 Taken together, these studies indicated that the consistent factor associated with somatic symptoms was gender. However, our results show that the sex difference in somatic symptoms among participants with symptoms of anxiety was not statistically significant. The possible reasons for the inconsistency were that women accounted for a large proportion of our sample, and they all had symptoms of anxiety. The following aspects could explain the effects of symptoms of anxiety on somatic symptoms: (1) in the state of anxiety, the sympathetic nerve is activated and the parasympathetic nerve is inactivated, which is characterized by increased heart rate, decreased heart rate variability, and increased blood pressure.50 Small changes in blood pressure and heart rate may not be noticed, but they may cause discomfort, such as cardiac stress.51 (2) Anxiety may reduce gastric peristalsis, delay gastric emptying, and increase colonic motility by promoting the release of corticotropin-releasing hormone and changes in the activity of the autonomic nervous system. This may cause stomach discomfort. In addition, anxiety may exacerbate gastrointestinal discomfort by causing visceral allergies.52 (3) Individuals with anxiety were more sensitive to physical changes.53 (4) Anxiety may lead to the increase of cortisol level, the change of cortisol secretion rhythm, and the decrease of melatonin synthesis, thus reducing the sleep quality.54,55 In addition, increased anxiety may result in insomnia, which may increase anxiety;56 hence, insomnia may affect somatic symptoms through anxiety. Improvements in symptoms of anxiety and insomnia may help improve somatic symptoms.16
It is worth mentioning the main limitations of our study. First, the study was conducted online, and it is impossible to know who opened our connection but did not complete questionnaire, so the response rate cannot be reported. This also leaded to the bias in the selection of research samples. Second, the cross-sectional study design can only explain the factors related to the somatic symptoms in health professionals with symptoms of anxiety during the COVID-19, but cannot make the direct casual relationship between the relevant factors and somatic symptoms. Third, the survey tool was a self-assessment scale, rather than a structured psychiatric interview, which may lead to a higher frequency than clinical practice. Fourth, our participants lacked health professional managers, and it would have been helpful to have heard the voice of those who managed the health professionals, what support could be offered for the workforce in the setting of pandemic, as the health professionals worked in a stressful setting, with high patient demand and no vaccine, no end in sight, and as a precious resource, it needs to be well cared for, as were the patients. Future research in this area will be urgently recommended. Fifth, compared with other Chinese studies of healthcare workers, our sample size is relatively small. Therefore, our findings in this study should be considered as preliminary and should be replicated in a large sample before a definitive conclusion can be drawn. Sixth, depression and stress related to somatic symptoms were not evaluated.
Conclusions
This is the first time that a sample of health professionals during COVID-19 to study the frequency of somatic symptoms and related factors in symptoms of anxiety. We found that symptoms of anxiety, insomnia, and somatic symptoms were common among these health professionals. Moreover, insomnia and symptoms of anxiety were independently associated with somatic symptoms of health professionals with symptoms of anxiety during COVID-19. It is necessary to pay attention to the somatic symptoms and sleep problems of health professionals during COVID-19. When they have somatic symptoms and insomnia, it is best to ask mental health professionals for evaluation and treatment in time so that they can better participate in the work of the epidemic. However, due to this study’s limitations, such as sample selection bias, small sample size, absence of structural psychiatric interview, and cross-sectional design, our findings should be considered preliminary. A wider range of health professionals such as health professional managers and longitudinal design should be used in future research.
Acknowledgments
The authors thank the Ethics Committee of the Institute of Psychology of the Chinese Academy of Sciences for the supports. Hehua Li and Yaping Zhang are co-first authors for this study.
Funding
This research was supported by the National Natural Science Foundation of China (Grant No.31771074), the Science and Technology Plan Project of Guangdong Province (Grant No.2019B030316001), the Scientific Research Project of Traditional Chinese Medicine of Guangdong (Grant No. 20201306), and the Science and Technology Plan Project of Guangzhou (Grant No.201807010064 and 201804010259).
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. COVID-19 can be characterized as a pandemic. Cited March 11, 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020.
2. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi:10.1016/S0140-6736(20)30185-9
3. Kang L, Li Y, Hu S, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7(3):e14. doi:10.1016/S2215-0366(20)30047-X
4. Liu S, Yang L, Zhang C, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e17–e18. doi:10.1016/S2215-0366(20)30077-8
5. Jianbo L, Simeng M, Ying W, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3).
6. Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11–17. doi:10.1016/j.bbi.2020.03.028
7. Pappa S, Ntella V, Giannakas T, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020.
8. Robert M, Jonathan H, Leslie V, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168(10).
9. YaMei B, Chao-Cheng L, Chih-Yuan L, Jen-Yeu C, Ching-Mo C, Pesus C. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. 2004;55(9).
10. Sarah A, Mohamad HT, Al-Eyadhy Ayman A, et al. Middle East respiratory syndrome coronavirus epidemic impact on healthcare workers’ risk perceptions, work and personal lives. J Infect Dev Ctries. 2019;13(10).
11. Lee EH, Han PL. Reciprocal interactions across and within multiple levels of monoamine and cortico-limbic systems in stress-induced depression: a systematic review. Neurosci Biobehav Rev. 2019;101:13–31. doi:10.1016/j.neubiorev.2019.03.014
12. Di Nicola M, Dattoli L, Moccia L, et al. Serum 25-hydroxyvitamin D levels and psychological distress symptoms in patients with affective disorders during the COVID-19 pandemic. Psychoneuroendocrinology. 2020;122:104869. doi:10.1016/j.psyneuen.2020.104869
13. McEwen Bruce S, Gianaros Peter J. Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. Ann N Y Acad Sci. 2010;1186:190.
14. Ella B, Lynn B, Rosmalen Judith GM, Schoevers Robert A. Differential associations of specific depressive and anxiety disorders with somatic symptoms. J Psychosom Res. 2015;78(2).
15. Rosmalen JGM, Tak LM, de Jonge P. Empirical foundations for the diagnosis of somatization: implications for DSM-5. Psychol Med. 2011;41(6):1133–1142. doi:10.1017/S0033291710001625
16. Wong JY, Fong DY, Chan KK. Anxiety and insomnia as modifiable risk factors for somatic symptoms in Chinese: a general population-based study. Qual Life Res. 2015;24(10):2493–2498. doi:10.1007/s11136-015-0984-9.
17. Means-Christensen AJ, Roy-Byrne PP, Sherbourne CD, et al. Relationships among pain, anxiety, and depression in primary care. Depress Anxiety. 2008;25:593–600. doi:10.1002/da.20342
18. Czachowski S, Piszczek E, Sowinska A, Olde Hartman TC. Challenges in the management of patients with medically unexplained symptoms in Poland: a qualitative study. Fam Pract. 2012;29(2):228–234. doi:10.1093/fampra/cmr065
19. Yu DS. Insomnia severity index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs. 2010;66(10):2350–2359. doi:10.1111/j.1365-2648.2010.05394.x
20. Liu X, Jiang D, Hou Z, He M, Lu Y, Mao Z. Mental health of the prison medical workers (PMWs) and influencing factors in Jiangxi, China. Int J Environ Res Public Health. 2017;14(12):1459. doi:10.3390/ijerph14121459
21. Zhang YN, Jin C, Ning L, Gong S, Xiao Y, Yu GL. Clinical characteristics and related factors of somatization symptoms in outpatients with psychiatric disorders of the department of cardiology in general hospitals. Zhonghua Xin Xue Guan Bing Za Zhi. 2019;47(11).
22. Jin H, Wu W, Zhang M. Norm of symptom checklist (SCL-90) in normal Chinese. Chin J Nerv Ment Dis. 1986;12(5):260–263.
23. Kraepelien M, Svanborg C, Lallerstedt L, Sennerstam V, Lindefors N, Kaldo V. Individually tailored internet treatment in routine care: a feasibility study. Internet Interv. 2019;18:100263. doi:10.1016/j.invent.2019.100263
24. Xia C, Ping L, Fei W, Guozhong J, Lin M, Sihong Y. Psychological results of 438 patients with persisting gastroesophageal reflux disease symptoms by symptom checklist 90-revised questionnaire. Euroasian J Hepatogastroenterol. 2017;7(2).
25. Du ML, Deng WX, Sun W, Chien CW, Tung TH, Zou XC. Assessment of mental health among nursing staff at different levels. Medicine (Baltimore). 2020;99(6):e19049. doi:10.1097/MD.0000000000019049
26. Schaefert R, Höner C, Salm F, et al. Psychological and behavioral variables associated with the somatic symptom severity of general hospital outpatients in China. Gen Hosp Psychiatry. 2013;35(3):297–303. doi:10.1016/j.genhosppsych.2012.11.001
27. Zhu C, Ou L, Geng Q, et al. Association of somatic symptoms with depression and anxiety in clinical patients of general hospitals in Guangzhou, China. Gen Hosp Psychiatry. 2012;34(2):113–120. doi:10.1016/j.genhosppsych.2011.09.005
28. Wen-Rui Z, Kun W, Lu Y, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020.
29. de Waal Margot WM, Arnold Ingrid A, Eekhof Just AH, van Hemert Albert M. Somatoform disorders in general practice: prevalence, functional impairment and comorbidity with anxiety and depressive disorders. Br J Psychiatry. 2004;184:470–476. doi:10.1192/bjp.184.6.470
30. Rob H, Boudien K, Nettie B, Koopmans Petra C, Groothoff Johan W. Severe MUPS in a sick-listed population: a cross-sectional study on prevalence, recognition, psychiatric co-morbidity and impairment. BMC Public Health. 2009;9.
31. Kate S, Dijkstra-Kersten Sandra MA, Mokkink Lidwine B, et al. Systematic review of measurement properties of questionnaires measuring somatization in primary care patients. J Psychosom Res. 2017;103.
32. Thomas H, Panagiota G, Carvalho Andre F. Personality traits, defense mechanisms and hostility features associated with somatic symptom severity in both health and disease. J Psychosom Res. 2013;75(4).
33. Zijlema Wilma L, Stolk Ronald P, Bernd L, Winfried R, White Peter D, Rosmalen Judith GM. How to assess common somatic symptoms in large-scale studies: a systematic review of questionnaires. J Psychosom Res. 2013;74(6).
34. Creed FH, Davies I, Jackson J, et al. The epidemiology of multiple somatic symptoms. J Psychosom Res. 2012;72(4):311–317. doi:10.1016/j.jpsychores.2012.01.009
35. Porcelli P, De Carne M, Leandro G. Distinct associations of DSM-5 somatic symptom disorder, the diagnostic criteria for psychosomatic research-revised (DCPR-R) and symptom severity in patients with irritable bowel syndrome. Gen Hosp Psychiatry. 2020;64:56–62. doi:10.1016/j.genhosppsych.2020.03.004
36. van Eck van der Sluijs J, Ten Have M, Rijnders C, van Marwijk H, de Graaf R, van der Feltz-cornelis C. Medically unexplained and explained physical symptoms in the general population: association with prevalent and incident mental disorders. PLoS One. 2015;10(4):e0123274. doi:10.1371/journal.pone.0123274
37. de Waal Margot WM, Arnold Ingrid A, Philip S, Eekhof Just AH, Assendelft Willem JJ, van Hemert Albert M. The role of comorbidity in the detection of psychiatric disorders with checklists for mental and physical symptoms in primary care. Soc Psychiatry Psychiatr Epidemiol. 2009;44(1).
38. Ishikawa Y, Takeshima T, Mise J, Ishikawa S, Matsumura M. Physical symptoms in outpatients with psychiatric disorders consulting the general internal medicine division at a Japanese university hospital. Int J Gen Med. 2015;8:261–266. doi:10.2147/IJGM.S82006
39. Löwe B, Spitzer RL, Williams JB, Mussell M, Schellberg D, Kroenke K. Depression, anxiety and somatization in primary care: syndrome overlap and functional impairment. Gen Hosp Psychiatry. 2008;30(3):191–199. doi:10.1016/j.genhosppsych.2008.01.001
40. Jessica D, Jiahong S, Yue Z, et al. Beyond “somatization” and “psychologization”: symptom-level variation in depressed Han Chinese and Euro-Canadian outpatients. Front Psychol. 2013;4.
41. Ball Harriet A, Siribaddana Sisira H, Athula S, et al. Genetic and environmental contributions to the overlap between psychological, fatigue and somatic symptoms: a twin study in Sri Lanka. Twin Res Hum Genet. 2011;14(1).
42. Kato K, Sullivan PF, Evengård B, Pedersen NL. A population-based twin study of functional somatic syndromes. Psychol Med. 2009;39(3):497–505. doi:10.1017/S0033291708003784
43. Kendler Kenneth S, Aggen Steven H, Peggy KG, Espen R, Neale Michael C, Ted R. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and all axis II disorders. Am J Psychiatry. 2011;168(1).
44. Roman K, Ruggero Camilo J, Krueger Robert F, David W, Qilong Y, Mark Z. New dimensions in the quantitative classification of mental illness. Arch Gen Psychiatry. 2011;68(10).
45. Alejandro I, Allen Lesley A, Gara Michael A, Escobar Javier I, Díaz-Martínez Angélica M. Somatic complaints in primary care: further examining the validity of the Patient Health Questionnaire (PHQ-15. Psychosomatics. 2006;47(5).
46. Stephanie K, Dirk F, Natalie S, Wolfgang H. Classification characteristics of the Patient Health Questionnaire-15 for screening somatoform disorders in a primary care setting. J Psychosom Res. 2011;71(3).
47. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders.
48. Regev S, Odes S, Slonim-Nevo V, et al. Differential relationships of somatization, depression, and anxiety to severity of Crohn’s disease. J Health Psychol. 2020:1359105320909879. doi:10.1177/1359105320909879
49. Hiller W, Rief W, Brähler E. Somatization in the population: from mild bodily misperceptions to disabling symptoms. Soc Psychiatry Psychiatr Epidemiol. 2006;41(9):704–712. doi:10.1007/s00127-006-0082-y
50. Kreibig Sylvia D. Autonomic nervous system activity in emotion: a review. Biol Psychol. 2010;84(3).
51. WHO. International Statistical Classification of Diseases and Related Health Problems.
52. Wilson Patrick B. The psychobiological etiology of gastrointestinal distress in sport: a review. J Clin Gastroenterol. 2020;54(4).
53. Rudolf H, McLeod Daniel R, Frank F, Pamela K. Somatic symptoms and physiologic responses in generalized anxiety disorder and panic disorder: an ambulatory monitor study. Arch Gen Psychiatry. 2004;61(9).
54. Cardinali Daniel P, Venkataramanujan S, Amnon B, Brown Gregory M. Melatonin and its analogs in insomnia and depression. J Pineal Res. 2012;52(4).
55. Johnson Eric O, Thomas R, Naomi B. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40(8).
56. Babson Kimberly A, Badour Christal L, Feldner Matthew T, Liviu B. The relationship of sleep quality and PTSD to anxious reactivity from idiographic traumatic event script-driven imagery. J Trauma Stress. 2012;25(5).
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
