Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
The Relationship Between Personal Factors, Smoke Exposure at Home, and Respiratory Problems in Early Childhood in Nakhon Si Thammarat Province, Thailand
Authors Phetruang A , Kusol K , Eksirinimit T, Jantasuwan R
Received 25 March 2023
Accepted for publication 16 August 2023
Published 28 August 2023 Volume 2023:16 Pages 2499—2511
DOI https://doi.org/10.2147/JMDH.S414172
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Apinya Phetruang,1 Kiatkamjorn Kusol,2 Thidarat Eksirinimit,2 Rachadaporn Jantasuwan2
1Chulabhorn Hospital, and Graduated Master of Nursing Science Program in Community Nurse Practitioner, School of Nursing, Walailak University, Nakhon Si Thammarat, Thailand; 2School of Nursing, and the Excellence Center of Community Health Promotion, Walailak University, Nakhon Si Thammarat, Thailand
Correspondence: Kiatkamjorn Kusol, Tel +66-81-979-65-65, Email [email protected]
Purpose: The purpose of this study was to examine the relationship between personal factors, smoke exposure at home, and respiratory problems in early childhood in Nakhon Si Thammarat Province, Thailand.
Samples and Methods: This study was retrospective. There was a total of 414 samples in the study. The instruments included the questionnaire about the personal data of early childhood and their caregivers, the smoke exposure assessment form, and the early childhood respiratory problem assessment form. The relationship between personal factors, smoke exposure at home, and respiratory problems in early childhood was analyzed by the Chi-squared test and binary logistic regression.
Results: The results revealed that smoke exposure at home in early childhood was moderate (52.2%). There 68.8% had respiratory problems. The relationship between birth weight, and smoke exposure at home in early childhood was found to be significantly related to respiratory problems (X2 =5.014 p< 0.05 and X2 = 85.711 p< 0.001, respectively). It was found that children with a birth weight ≤ 2500g had respiratory problems at 2.55 times of the samples with birth weight > 2500g (AOR = 2.55, 95% CI: 1.10– 5.96), and moderate-high smoke exposure had respiratory problems at 8.86 times of the samples with low smoke exposure (AOR = 8.86, 95% CI: 5.39– 14.60). Nutritional status and breastfeeding were not significantly related to respiratory problems in early childhood p > 0.05.
Conclusion: The birth weight and smoke exposure at home factors were found to be related to their respiratory problems in early childhood. Thus, it is necessary to reduce stimuli, especially smoking at home. Moreover, the standard birth weight of their early childhood will reduce the rate of respiratory problems.
Keywords: personal factors, smoke exposure, early childhood, respiratory problems
A Letter to the Editor has been published for this article.
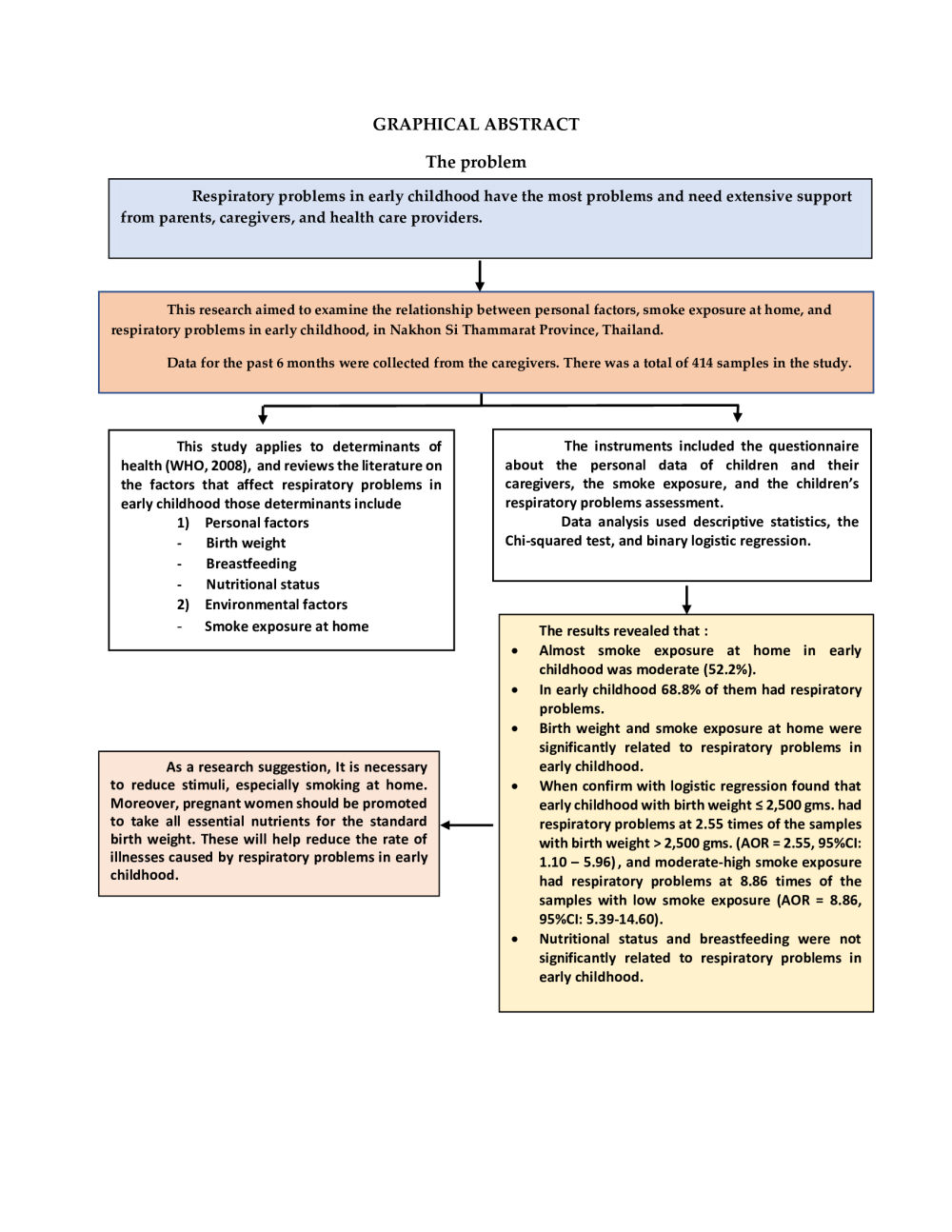
Graphical Abstract:
Introduction
According to the situation worldwide each year, at least 6 million children die of illnesses caused by respiratory problems and respiratory infections.1 A report in 2015 revealed that there were up to 50–80% of children with respiratory problems in developing countries went for treatment in hospitals, with mortality up to 15%.2 According to reports of respiratory problems in children have an incidence of 6–8 times per year.3 It mostly disturbs the daily life of children. But lower respiratory infection, particularly pneumonia, is found as a key cause of death in children aged below 5 years.4 This incidence of respiratory problems is found at the maximum in developing countries.5 In Thailand, pneumonia was found with an illness rate of 103 per population of 100,000 in 2017.6
Respiratory problems in children are caused by organ abnormalities in the nasal cavity, throat, epiglottis, larynx, trachea, bronchiole, alveolar sac, and lungs. When having respiratory problems, the body will show a cough reflex and sneezing reflex against foreign bodies that invade the respiratory tract to adjust the respiratory system balance back to its normal conditions. Thus, there will be symptoms of nasal irritation, nasal congestion, runny nose, cough, sneezing, sore throat, dyspnea, and possibly followed by infection.7 Caregivers must keep observing their children’s health problems, along with taking good care and environmental management that can reduce risk factors of the respiratory tract to prevent more severe health problems. That is because children usually have low immunity, resulting in easy infection and illnesses.
According to the review of relevant research, the factors related to respiratory problems in early childhood can be concluded as follows. First, personal factors include birth weight, breastfeeding, and nutritional status. It can be described that newborn babies weighing below 2500 g have a risk of chronic respiratory problems.8,9 Also, they tend to get more severe than those with normal weight, with a higher risk of LRI at 1.3 times.10 Babies with continuous breastfeeding in the first 6 months usually have the antibodies of their mothers that are transferred to help develop and increase their immune system, and to reduce the frequency of respiratory infection as well as diseases more efficiently than those with artificial feeding.11–14 Children with low weight and malnutrition tend to get ill with acute URI more easily than those with normal nutritional status15–17 because malnutrition generally worsens the immune system.18,19 Second, environmental factors and exposure to undesirable weather can reduce the functional efficiency of the lungs, resulting in the risk of URI and LRI in children, particularly in an environment with smoke exposure at home.20,21 Cigarette substances and smoke stimulate antibody formation inside the body, followed by allergic reactions to adaptation, finally resulting in nasal congestion and possibly dyspnea in some cases.22 Children with smoke exposure tend to have more respiratory problems than those without smoke exposure.23 More specifically, those in families with smoking parents tend to have bronchitis or pneumonia up to 47% and asthma up to 39%.24 Any family with at least 1 smoker can increase the risk of asthma in children by 1.8 times.25
Early childhood is the age of development in several dimensions of their life, with a tendency to exposure to close environments that can be risk factors for their health.26 As a result, their respiratory problems can occur more easily and more severely than adults because their respiratory tract is smaller, narrower, and shorter than adults. Children have Type-II rapid-twitch muscle fiber more than Type-I slow-twitch muscle fiber. Thus, their respiratory muscles can slightly endure elasticity. Their immune system is underdeveloped.27 As a result, in the case of illnesses, particularly respiratory problems, and inappropriate treatment, children may undergo disabilities, death, or chronic health problems in the long run.
According to previous studies, children with respiratory problems tend to increase in number.2,5,6 Research studies have revealed that their respiratory problems are mostly found in the form of respiratory infections.4,15,28 However, there is still a gap in studies on personal factors, with supporting and contradictory data on respiratory problems.10,16,17,19 Also, so far there have still been a few factors relating to smoke exposure at home and respiratory problems. For Nakhon Si Thammarat Province, there have been no studies on the relationship between personal factors and smoke exposure at home with respiratory problems in early childhood yet. For this reason, the researchers implemented a study on “The Relationship between Personal Factors, Smoke Exposure at Home, and Respiratory Problems in Early Childhood”. The aim of this study was designed to examine the relationship between personal factors, smoke exposure at home, and respiratory problems in early childhood in Nakhon Si Thammarat Province, Thailand.
Samples and Methods
Study Design, Setting, and Sample
This descriptive correlation study was a retrospective design. Data was collected in the past 6 months between May and July 2022 in early childhood at Nakhon Si Thammarat Province.
The population included 35,567 children aged 3–5 years with smokers in their families and who lived in Nakhon Si Thammarat Province. The acquisition of the sample size was calculated by the Krejcie and Morgan formula, with 95% reliability. The sample size was generating 380 research samples. The researchers added to prevent the collection of incomprehensive data. Thus, 414 samples were used in this research, obtained by multi-stage random sampling as follows.
Step 1: The districts in Nakhon Si Thammarat Province were randomized. The administration was divided by geographic features that were selected by simple random sampling, i.e., Chulabhorn District and Ron Phibun District.
Step 2: Chulabhorn District and Ron Phibun District have a total of 12 subdistricts, i.e., Kuanmud Subdistrict, Kuan Nong Kwa Subdistrict, Thung Pho Subdistrict, Na Moh Boon Subdistrict, Sam Tambon Subdistrict, Ban Cha Uad Subdistrict, Hin Tok Subdistrict, Sao Thong Subdistrict, Kuan Koei Subdistrict, Kuan Pang Subdistrict, Kuan Chum Subdistrict, and Ron Phibun Subdistrict. The 12 subdistricts contain 16 health-promoting hospitals and simple random sampling (drawing without replacement) of 5 health-promoting hospitals.
Step 3: Children were selected from the list of early childhood by simple random sampling as per the qualification of having smokers in their families until the number of children reached the determined criteria, as shown in Table 1.
 |
Table 1 Number of Samples in Each Health-Promoting Hospital (n = 414) |
The Questionnaire, Reliability, and Validity
The research instruments were as follows:
Part 1: Personal data of children in early childhood included 10 items, ie, sex, age, weight, height, nutritional status, labor history, post-labor complications, birth weight, breastfeeding history in the first 6 months, and underlying diseases. The questionnaire was developed as a checklist with open-ended questions.
Part 2: Personal data of main caregivers included 11 items, ie, sex, age, religion, marital status, present occupation, educational level, household monthly income, smoking history, the relationship between the caregiver and child, number of smokers in the family, and role of smokers in the family. The questionnaire was developed as a checklist with open-ended questions.
Part 3: Assessment of early childhood exposure to tobacco smoke was modified from the instrument of Wiparat Suwanwaiphattana, Chatthong Jaruphisitpaiboon, and Issarawan Sonthipumas, who studied the relationship between secondhand smoke exposure in households and respiratory tract infection of children below 5 years old.28 This part contained 6 questions, of which means were interpreted by setting the interval of means of smoke exposure score, compared with the 3-level scale, ie, 1) 6–12 points = Low smoke exposure, 2) 13–18 points = Moderate smoke exposure, and 3) 19–24 points = High smoke exposure. The instrument was tested for content validity and reliability by 5 experts. The test results revealed content validity (CVI) = 1.0, with Cronbach’s alpha coefficient of reliability = 0.8.
Part 4: The questionnaire for Respiratory Health Problems in Early Childhood was modified from the instrument of Sirithorn Duangsawat,29 whose questionnaire was developed by the American Thoracic Society (ATS-1987). The form/questionnaire included 9 questions as a checklist and was tested for content validity and reliability by 5 experts. The test results revealed CVI = 1.0, with KR-20 of reliability = 0.72.
Data Collection
In this research, the researchers collected data from the samples on our own according to the implementation procedures as follows.
- The researchers studied the number of early childhood population in Nakhon Si Thammarat Province who had smokers in their families.
- The researchers contacted Walailak University to request approval for research implementation from the human subject protection committee. After the request had been approved by the human subject protection committee, the researchers wrote a letter of request for support from the School of Nursing, Walailak University, to the directors of all 5 Tambon health-promoting hospitals. The researchers conducted the study following the Declaration of Helsinki. All procedures performed in this study involving human participants followed the ethical standards of the Ethical Institutional Consideration. This study received approval from the Ethics Committee on Human Research at Walailak University on 7 April 2022 (No. WU-EC-22-116-01) as required by the process before data collection. Informed consent was obtained by the researchers from all individual participants included in the study.
- The researchers contacted the directors of all 5 Tambon health-promoting hospitals, chief executives of the village, health volunteers, parents, and research participants to clarify the project details, objectives, processes, and expected benefits. They also confirmed that their participation must follow their consent. The researchers also requested their kind assistance to collect all data.
- The researchers collected data by handing the questionnaire to all participants at their homes in the community, with a detailed description of each question. Children were selected from the list of early childhood by simple random sampling as per the qualification of having smokers in their families until the number of children reached the determined criteria. The participants had 30–45 minutes to complete the questionnaire. The researchers asked for permission to wait until all questionnaires were completed, which would be regarded as the end of the questionnaire.
- The researchers examined the accuracy and completeness of all data. The codes were recorded as per the developed coding manual for data records in the program for further statistical analysis.
Statistics
- Personal data of children in early childhood and main caregivers were analyzed by descriptive statistics, ie, frequency, percentage, mean, and SD.
- Data on smoke exposure in early childhood and history of respiratory illnesses were analyzed by descriptive statistics, ie, frequency, percentage, mean, and SD.
- The relationship between personal factors, smoke exposure at home, and respiratory problems in early childhood was analyzed by the Chi-squared test.
- The relationship was analyzed, along with the prediction of the incidence between personal factors, smoke exposure at home, and respiratory problems in early childhood by binary logistic regression. The analysis is used for criterion variables that are divided into two subgroups such as the group, that shows respiratory problems event, will be a value of 1 with the group, that not showing respiratory problems event, will be 0. An independent variable was selected for the model by the Enter Method, determining statistical significance at 0.05.
Results
Personal Data in Early Childhood
The study samples were in early childhood, with 51% male and 49% female, aged 3.7 years on average (S.D. = 0.60). The minimum age was 3.5 years, while the maximum age was 5 years. The nutritional status of most children met the normal (80.2%) with full-term labor (81.9%), birth weight >2500 gm (94.4%), and ≥6 months of breastfeeding (69.8%) (Table 2).
 |
Table 2 Number and Percentage of Personal Data in Early Childhood (n = 414) |
Personal Data of Caregivers
According to the personal data of the caregivers, most of them were female (66.2%), aged 19–40 years (68.6%), with an average age of 40.28 years (S.D. = 12.03), the minimum age was 19 and the maximum age was 72 years). Almost all of them were Buddhist (99.3%), married (79.7%), agriculturist (24.4%), graduated from high school level or equivalent (49.8%), had a monthly income of 10,001–20,000 bath/month (34.1%), did not have a smoking history (72.5%), had a relationship with the children that was mostly a parental relationship (73.4%), had one smoker at home (76.6%), and had smokers who were mostly fathers, grandfather, and relatives (61.1%) (Table 3).
 |
Table 3 Number and Percentage of Personal Data of Caregivers and Smokers in Families (n = 414) |
Smoke Exposure in Early Childhood
According to the study on smoke exposure at home in early childhood in terms of frequency, they were often directly exposed to smoking (45.4%); often walked past smokers at home (47.6%); often did activities at smoking areas at home (40.6%); were usually exposed to smoke left on tables, chairs, sofas, clothing, curtains, and carpets (36.5%); touched body parts of smokers every day (39.4%); and frequently hugged smokers/kissed on the cheek (41.5%) (Table 4).
 |
Table 4 Number and Percentage of Smoke Exposure at Home in Early Childhood (n = 414) |
Symptoms of Respiratory Problems in Early Childhood
According to the study on the history of children’s illnesses caused by respiratory problems, it was found that in the past 6 months, children had nasal congestion, sneezing, and runny nose (59.7%); had coughs and phlegm (45.7%); had throat irritation and sore throat (41.3%); had eye irritation and tears (14.5%); had asthma, dyspnea, and panting (12.6%); had wheezes (11.8%); and had tightness in the chest (5.6%) (Table 5).
 |
Table 5 Number and Percentage of Symptoms of Respiratory Problems in Early Childhood (n = 414) |
According to the study on smoke exposure at home and health problems of children in early childhood, it was found that their smoke exposure was moderate (52.2%). In addition, 68.8% had illnesses caused by respiratory diseases. And in the past 6 months, children went for treatment at government or private service establishments due to respiratory symptoms (40.6%). Most of them were found with the common cold (47.6%) (Table 6).
 |
Table 6 Number and Percentage of Smoke Exposure, Illness, and Treatment in Early Childhood (n = 414) |
For the relationship between personal factors, smoke exposure at home, and respiratory problems in early childhood, it was found that the factors significantly related to respiratory problems in children included birth weight and smoke exposure at home (X2= 5.014, p < 0.05 and X2= 85.711, p < 0.001, respectively). In contrast, nutritional status and breastfeeding were not significantly related to respiratory problems in children (X2= 0.727, and X2= 0.877 p > 0.05, respectively) (Table 7). According to analysis, the relationship between personal factors, smoke exposure at home, and respiratory problems in early childhood, two factors were found to be related to their respiratory problems, ie, birth weight and smoke exposure at home. When analyzed using binary logistic regression, it was found that these factors were significantly related to respiratory problems in children as well. To clarify, the group with birth weight ≤2500 g tended to have respiratory problems at 2.55 times (p < 0.05) of the samples with birth weight >2500 g. Smoke exposure at home was significantly related to respiratory problems in early childhood. The group with moderate and high smoke exposure tended to have respiratory problems at 8.86 times (p < 0.001) of the samples with low smoke exposure (Table 8).
 |
Table 7 Relationship Between Personal Factors, Smoke Exposure at Home, and Respiratory Problems in Early Childhood (n = 414) |
 |
Table 8 Factors Related to Respiratory Problems in Early Childhood as Analyzed by Binary Logistic Regression (n = 414) |
Discussion
Among the samples in early childhood, 69.1% were found with respiratory problems. In the past 6 months, 40.6% went for treatment at government or private service establishments due to the common cold (47.6%). In addition, 52.2% of them had a history of moderate smoke exposure at home because children at this age mostly lived with their families. This is the age of development in several aspects of life, with a tendency of exposure to surroundings/environments nearby as a risk factor for their health.26 Particularly, if there were smokers in their families, children tended to be exposed to those family members. In addition, anatomical and physiological characteristics of the respiratory system in children were still small, with an underdeveloped immune system.7 Thus, they tended to have illnesses caused easily by respiratory diseases.
For the relationship between birth weight and respiratory problems in children, they were significantly related to each other (p < 0.05). The group with birth weight ≤2500 g tended to have respiratory problems at 2.55 times of the samples with birth weight >2500 g (AOR = 2.55, 95% CI: 1.10–5.96) because children with a birth weight below the standard were mostly those in preterm labor, resulting in inefficient function and underdevelopment of lungs, along with an underdeveloped immune system. Birth weight below the standard in preterm labor also resulted in getting infected easily, particularly respiratory problems that were usually more severe than in children with normal weight.4 It was also riskier to have a lower respiratory infection at 1.3 times.10 This conformed to the study in Vietnam which found that children with a birth weight below the standard could cause heart failure, and might need hospital admission due to the severity of the disease.30 To clarify, the disease commonly found in children with a history of birth weight below the standard is an abnormal respiratory system. It also conformed to the study on the relationship between low birth weight and acute respiratory infection in Telaga Health Care Clinic Gorontalo District, which found that both were significantly related to each other.31 Thus, reducing respiratory problems should start with health promotion in pregnant women to get full nutrients for a standard birth weight >2500 g to reduce the rate of illnesses caused by respiratory problems in children.
For the relationship between smoke exposure at home and respiratory problems in children, they were significantly related to each other (p < 0.001). The group with moderate to high smoke exposure tended to have respiratory problems at 8.86 times of the samples with low smoke exposure (AOR = 8.86, 95% CI: 5.39–14.60). This conformed to a study in particularly an environment with second-hand smoke, and smoke exposure at home, which found that resulted in the risk of URI and lung functions in children.20,21,23 More specifically, those in families with smoking parents tend to have bronchitis or pneumonia up to 47% and asthma up to 39%.24 Children with smokers in their families were directly affected by respiratory problems because their respiratory system contained Type-II rapid-twitch muscle fiber more than Type-I slow-twitch muscle fiber. Thus, their respiratory muscles can slightly endure elasticity.32,33 Their immune system was also underdeveloped. Thus, when their body was exposed to foreign bodies or any substances causing cough reflex and sneezing reflex, their body would adjust the balance of the respiratory system back to normal. As a result, there would be symptoms of nasal irritation, nasal congestion, runny nose, cough, sneezing, sore throat, dyspnea, and possibly followed by infection.27 In addition, it also caused chronic coughs, breathing difficulty, and more bronchitis.34 This conformed to the research that children living in smoking families tended to have URI and LRI more than those in non-smoking families. Thus, continuous smoke exposure in children could cause illnesses in the respiratory tract.20,34 This also conformed to the study on respiratory infection in Cameroon, which found that smoke could directly affect respiratory problems in children.35 Thus, it is necessary to plan health problem prevention in children together by reducing stimuli, particularly cigarette smoke. Also, awareness should be created for family members not to smoke at home to reduce the severity and the rate of respiratory problems in early childhood.
The personal factor of breastfeeding was not significantly related to respiratory problems in children (p > 0.05). This study found that children receiving 6 months of breastfeeding and those receiving less than 6 months did not have different respiratory problems despite full nutrients that affected the immune system against diseases and antioxidants that could reduce respiratory infection.14 However, it also depends on other intrinsic factors and environments affecting the respiratory system. However, post-labor breastfeeding in the first 6 months provided full nutrients for children and immunity from mothers, and breast milk contained secretory IgA (SIgA) and anti-food antibodies that help detect allergens.11,28 Antibodies of mothers to children would help develop and increase antibodies. They also helped prevent infection in different systems, particularly respiratory diseases.12–14 Although this study found that breastfeeding was not related to respiratory problems in early childhood, current public health policies mainly focus on promoting all children to drink breast milk from birth to 6 months, and they should drink continuously until the age of 2 years along with eating appropriate food for their age to increase the function of their immune system for better efficiency.36 The personal factor of nutritional status was not significantly related to respiratory problems in early childhood (p > 0.05). This study found that children with a nutritional status that met the standard and those with a nutritional status below the standard did not have different respiratory problems. Nutritional status below the standard referred to body growth that did not meet the standard. This conformed to the study on respiratory problems, which found that nutritional status was not related to respiratory problems. It described that nutritional status was slightly important to respiratory problems.35,37 However, this might be different from the result which found that children with malnutrition tended to have immune deficiency, lower immune function, and illnesses including respiratory infection.18 Children with very low to low weight, very short to short height, and very thin to thin bodies were related to an upper respiratory infection.15 The limitations In this study, the number of samples in the group with a nutritional status below the standard had nutritional status slightly below the standard.
Conclusions
The study on birth weight, smoke exposure at home, and respiratory problems in children were significantly related to one another. The group with birth weight ≤2500 g. tended to have respiratory problems at 2.55 times the samples with birth weight >2500 g. The group with moderate and high smoke exposure tended to have respiratory problems at 8.86 times the samples with low smoke exposure. In contrast, nutritional status and breastfeeding were not significantly related to respiratory problems in children. Thus, reducing the rate of illnesses and severity of respiratory problems in children requires highly reducing stimuli, particularly cigarettes, by creating awareness for family members not to smoke at home. There should also be health promotion among pregnant women to get full nutrients for standard birth weight to reduce the rate of illnesses caused by respiratory problems in children.
Ethics Statement
All procedures involving human participants that were performed in the studies followed the ethical standards of the Ethical Institutional Consideration. Ethical approval was obtained from the Office of the Human Research Ethics Committee of Walailak University, dated April 7, 2022, No. WU-EC-22-116-01.
Acknowledgments
We want to express our gratitude to the School of Nursing, Walailak University, for its support and advice. We would also like to sincerely thank the healthcare providers, presidents of the health-promoting hospitals, and the village health volunteers for their kind and active cooperation.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Funding for this study was supported and awarded to the first author or the corresponding author from the Excellence Center of Community Health Promotion, Nursing Institute, Walailak University.
Disclosure
The authors report no conflicts of interest for this work or regarding the publication of this paper.
References
1. World Health Organization. Pneumonia. Geneva, Switzerland: World Health Organization; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/pneumonia.
2. Mc Allister DA, Liu L, Shi T, et al. Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: a systematic analysis. Lancet Global Health. 2019;7:47–57. doi:10.1016/S2214-109X(18)30408-X
3. Thitithamjaroen S, In-klinphan N, Pongpanic P. The incidence and number length of stay of pediatric acute respiratory infection patients hospitalized at Jainad Narendra Hospital. Jainad Narendra Hospital; 2017. Available from: http://www.chainathospital.org/chainatweb/assets/research/research27.pdf.
4. Roux DM, Nicol MP, Myer L, et al. Lower respiratory tract infections in children in a well-vaccinated South African Birth Cohort: spectrum of disease and risk factors. Clin Infect Dis. 2019;69(9):1588–1596. doi:10.1093/cid/ciz017
5. The Thai Society of Pediatric Respiratory and Critical Care Medicine, The Royal College of Pediatricians of Thailand. Treatment Guidelines for Acute Respiratory Infections in Children 2019. Beyond Enterprise Co., Ltd; 2019.
6. Bureau of Epidemiology. Weekly epidemiological surveillance report. department of disease, ministry of public health; 2022. Available from: https://wesr-doe.moph.go.th/wesr_new/file/y65/H65282022-07-102022-07-16.pdf.
7. Srising K, Srijanthongsiri S. Pediatric Respiratory Disease. Naresuan University Publishing House; 2021.
8. Noynark P. Preterm neonates and low birth weight with respiratory distress syndrome. Singburi Hospital J. 2020;29:1–14.
9. Rajid C. Factors related to low birth weight in Health Region 5. J Public Health Nurs. 2020;34(3):1–17.
10. Dursun M, Zubarioglu UA, Bulbul A. Relationship between the respiratory severity score and extubation failure in very-low-birth-weight premature infants. Med Bulletin Sisli Etfal Hospital. 2021;55(3):382–390. doi:10.14744/SEMB.2021.92693
11. Khoonphe C, Kala S. The experience of breastfeeding intention among adolescent mothers. Princ Naradhiwas Univer J. 2019;11(2):1–11.
12. Bonkhunthod P, Saengngam T, Pimmanurak R, Manluan K. Role of nurses and families in the promotion of breastfeeding in adolescent mothers. Med J Srisaket Surin Buriram Hospital. 2021;36(2):275–282.
13. Sangbamrung P, Seubsirinukul W, Kokkratok K, et al. The roles of nurses caring for mothers with short nipples. J Health Nurs Educ. 2020;28(2):1–12.
14. Del Ciampo AL, Del Ciampo IRL. Breastfeeding and the benefits of lactation for women’s health. Rev Bras Ginecol. 2018;40(6):354–359. doi:10.1055/s-0038-1657766
15. Phaithong P. Nutritional status and acute upper respiratory infections in pre-school children of Hmong Tribe, Mae Ram Sub-district, Mae Rim District, Chiang Mai Province. Lanna Public Health J. 2019;15:14–25.
16. Derseh B, Mruts K, Demie T, Gebremariam T. Co-morbidity, treatment outcomes and factors affecting the recovery rate of under-five children with severe acute malnutrition admitted in selected hospitals from Ethiopia: retrospective follow-up study. Nutr J. 2018;17:116. doi:10.1186/s12937-018-0423-1
17. Poda GG, Hsu CY, Chao JC. Factors associated with malnutrition among children < 5 years old in Burkina Faso: evidence from the demographic and health surveys IV 2010. Int J Qual Health Care. 2017;29(7):901–908. doi:10.1093/intqhc/mzx129
18. Mosuwan L, Puwanant M, Phosuwattanaku J, et al. Clinical practice guidelines for the pediatric inpatient treatment of severe acute malnutrition. Nutrit Therap J. 2019;28:10–39.
19. Savitha MR, Prashanth MR, Thanuja B. The severity of malnutrition among children with pneumonia and diarrhea: moderate acute malnutrition- a neglected entity. Int J Pediatr Res. 2020;7(2):2349–5499.
20. Vanker A, Gie RP, Zar HJ. The association between environmental tobacco smoke exposure and childhood respiratory disease: a review. Expert Rev Respir Med. 2017;11(8):661–673. doi:10.1080/17476348.2017.1338949
21. Smith K, Pillarisetti A. Household air pollution from solid cookfuels and health. In: Mock CN, Nugent R, Kobusingye O, Smith K, editors. Disease Control Priorities, Injury Prevention and Environmental Health. Washington, DC: World Bank; 2022.
22. Department of Disease Control Particulate Matter. Invisible Hazardous Particles. Bureau of epidemiology, department of disease. Ministry of Public Health; 2019. Available from: https://ddc.moph.go.th/doe/journal_detail.php?publish=5504.
23. Elshazly FA, Abdelbasset WK, Elnaggar RK, Tantawy SA. Effects of second-hand smoking on lung functions in athlete and non-athlete school-aged children – an observational study. Afr Health Sci. 2020;20(1):368–375. doi:10.4314/ahs.v20i1.42
24. Thai Health Promotion Foundation. Report of Tobacco Consumption in Thailand 2019. Bangkok: Sintaveekit Printing Ltd. Partnership; 2019.
25. Taweepattana H. Protecting Children from Smoke. In:
26. National Collaborating Centre for Determinants of Health. The Impact of Inequities, Poverty, and Racism on the Health of Children; 2019. Available from: https://nccdh.ca/blog/entry/the-impact-of-inequities-poverty-and-racism-on-The-health-of-children.
27. Phianpijan N. Bonding promotion and breastfeeding in the delivery room. Faculty of Medicine, Siriraj Hospital, Mahidol University; 2015. Available from: https://www2.si.mahidol.ac.th/division/nursing/sins/attachments/article/222/sins_nursing_manual_2558_10.pdf.
28. Suwanwaiphattana N, Jaruphisitpaiboon C, Sonthipumas I. Relationship between secondhand smoke exposure in households and respiratory tract infection of children below five years old. J Nurs Educ. 2013;6(2):113–123.
29. Duangsawat S. Respiratory symptom prevalence rate and comparative lung capacity for students at primary schools in industrialized areas of Ang Thong province, Thailand. Independent study of Master of Public Health Major Field in Environmental Health and Safety Management Faculty of Public Health Thammasat University; 2016.
30. Nam NT, Dem PV, Tam NT, Dung NT. Preterm birth and low birth weight in neonates with postnatal respiratory failure at a tertiary hospital in Viet Nam. Biomed Res Ther. 2022;7(9):4010–4015. doi:10.15419/bmrat.v7i9.633
31. Kai MW, Tomayahu MB, Anggraini R. The relationship of low birth weight with acute respiratory infection on toddlers in Telega health care clinic of gorontalo district. In:
32. Wang Y, Huang Z, Luo D, Tian L, Hu M, Xiao S. Respiratory symptoms and urinary cotinine levels in preschool children exposed to environmental tobacco smoke. Front Public Health. 2020;26(8). doi:10.3389/fpubh.2020.587193
33. Zhuge Y, Qian H, Zheng X, et al. Effects of parental smoking and indoor tobacco smoke exposure on respiratory outcomes in children. Sci Rep. 2020;10(4311):1–9. doi:10.1038/s41598-020-60700-4
34. Francis L, DePriest K, Wilson M, Gross D. Child poverty, toxic stress, and social determinants of health: screening and care coordination. Online J Issues Nure. 2018;23(3):1–13.
35. Tazinya AA, Halle-Ekane GE, Mbuagbaw LT, Abanda M, Atashili M, Obama MT. Risk factors for acute respiratory infections in children under five years attending the Bamenda Regional Hospital in Cameroon. BMC Pulm Med. 2018;1–8. doi:10.1186/s12890-018-0579-7
36. Department of Health. “Breast Milk” Genuine Natural Benefits; 2018. Available from: https://multimedia.anamai.moph.go.th/help-knowledgs/benefits-of-breastfeeding.
37. Parimanon C, Chaimay B, Woradet S. Nutritional status and factors associated with nutritional status among children aged under 5 Years: a literature review. Southern Coll Network J Nurs Public Health. 2018;15:329–342.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
