Back to Journals » Orthopedic Research and Reviews » Volume 14
The Relationship Between Body Mass Index and the Magnitude of Curve at Diagnosis of Adolescent Idiopathic Scoliosis: A Retrospective Chart Review
Authors Woods N, Wittmeier K , Mulder K , Dufault B, Black B
Received 22 January 2022
Accepted for publication 2 April 2022
Published 9 May 2022 Volume 2022:14 Pages 149—155
DOI https://doi.org/10.2147/ORR.S359394
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Natalie Woods,1,2 Kristy Wittmeier,1– 3 Kathy Mulder,1 Brenden Dufault,4 Brian Black5,6
1Physiotherapy Department, Health Sciences Centre Winnipeg – Shared Health, Winnipeg, MB, Canada; 2Children’s Hospital Research Institute of Manitoba, Winnipeg, MB, Canada; 3Department of Pediatrics and Child Health, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada; 4Data Sciences Platform, George & Fay Yee Centre for Healthcare Innovation, Winnipeg, MB, Canada; 5Department of Pediatric Orthopedic Surgery, University of Manitoba, Winnipeg, MB, Canada; 6Child Health Program, Health Sciences Centre Winnipeg – Shared Health, Winnipeg, MB, Canada
Correspondence: Brian Black, Child Health Program, Health Sciences Centre Winnipeg – Shared Health, 840 Sherbrook Street, Winnipeg, MB, R3A 1S1, Canada, Tel +1-204-787-4204, Fax +1-204-787-2460, Email [email protected]
Purpose: To evaluate the relationship between body mass index (BMI) and spinal curvature in patients presenting with idiopathic scoliosis at a major pediatric tertiary care centre.
Patients and Methods: Retrospective chart review (2015– 2019). Data extracted from patient’s first visit included age, sex, height, weight, spinal curvature (magnitude, location), referral source, physical activity participation (yes/no), pain (yes/no). Demographics were analyzed descriptively. The relationship between BMI and spinal curve magnitude was analyzed using Spearman correlation coefficient. Linear regression was applied to determine the relationship between BMI, curve magnitude, and curve location. Exploratory univariate analyses were conducted for BMI and referral source, pain, and skeletal maturity, and physical activity and pain.
Results: A total of 206 patient charts were included (177 females, 29 males). Patients presented with double major (41.3%), thoracic (26.7%), thoracolumbar (22.8%), and lumbar (9.2%) curves. Mean (SD) BMI percentile was 48.3 (30.5). No relationship existed between BMI percentile and curve magnitude with curve locations combined. However, a test for interaction revealed a positive relationship between BMI percentile and curve magnitude for adolescents with double major curves, and a negative relationship for adolescents with thoracic curves. Exploratory analyses suggested a relationship between BMI percentile and presence of pain, and between referral source and curve magnitude. No relationship was observed between BMI and skeletal maturity, or physical activity and pain.
Conclusion: The relationship between BMI varied by curve location within this cohort, in which most patients presented with a BMI < 85th percentile. Findings highlight the importance of sensitive history taking and careful physical examination for early detection of scoliosis.
Keywords: scoliosis, body mass index, curve magnitude, screening, chart review
Introduction
Scoliosis is characterized by a lateral curvature of the spine >10 degrees and a component of vertebral rotation. The magnitude of the spinal curve is measured using the Cobb angle on x-ray.1–3 Idiopathic scoliosis is classified into 3 categories (infantile, juvenile, and adolescent) based on the age of the patient at diagnosis. Adolescent idiopathic scoliosis (AIS) is the most common form of idiopathic scoliosis. It affects 2–4% of children and youth aged 10–18 and can often be identified on routine physical examination by a health care provider.1–3 Commonly used clinical screening methods for scoliosis include general visual inspection and the Adam’s Forward Bending Test.4
While the benefits of universal screening programs have been debated,4–6 early detection of AIS is important so that appropriate management pathways can be initiated, especially those at highest risk for progression.7 As summarized by the Scoliosis Research Society, risk of progression is higher in the in those who develop scoliosis at a young age, in the presence of skeletal immaturity, and when curve angle is ≥20 degrees at presentation.8 Recent research has identified additional factors, such as spinal flexibility, that may be important to predict curve progression/successful outcomes with bracing9,10 In addition to facilitating the initiation of bracing (when indicated11), early identification allows for earlier introduction of other conservative approaches. Schroth exercises (a type of physiotherapeutic scoliosis-specific exercise) for example have been reported to have a moderate to large effect size on outcomes depending on the pre-intervention curve angle.12 Therefore, early recognition of AIS may be an important factor in limiting the progression of scoliosis, and in some cases preventing the need for surgical management.11 Barriers to early identification and referral for further management should be identified and addressed.7
Several published studies have assessed the relationship between body mass index (BMI) and the magnitude of spinal curvature upon presentation to a specialized scoliosis clinic.13–15 These retrospective studies examined the charts of 150–279 adolescents and concluded that adolescent patients with a higher BMI or higher adiposity are more likely to have a larger magnitude of curve when they are first diagnosed with scoliosis compared to adolescents with a lower BMI or adiposity.13–15 The authors of these studies suggested that typical physical examination findings indicative of scoliosis may be less apparent in adolescents with a higher BMI, resulting in delayed identification of scoliosis. One of the studies also found that patients presenting with a higher BMI were more likely to present with a higher degree of skeletal maturity, which has implications for treatment options, and treatment success.8,14 It is important to understand whether there are limitations in our current screening methods for AIS that place children and adolescents with a higher BMI at higher risk of delayed identification of scoliosis, which could limit treatment options and negatively impact outcomes.
Given the results of the limited research on this topic to date, the purpose of this study was to examine the relationship between BMI percentile and the magnitude and location of spinal curvature at presentation within a pediatric scoliosis clinic at a tertiary care centre, to further inform local referral and practice recommendations. A secondary aim was to conduct exploratory analyses related to BMI percentile and how the spinal curvature was initially identified (referral source), the presence of pain, and skeletal maturity, and to explore potential relationships between pain and physical activity participation at presentation.
Materials and Methods
A retrospective chart review was conducted, including all eligible youth who presented to the single tertiary care centre for the initial assessment of scoliosis between the years of 2015–2019. Inclusion criteria were patients aged 10–18 years old, presenting to the scoliosis clinic for initial assessment with no prior treatment for scoliosis. Data from patients who were found not to have scoliosis, who presented with non-idiopathic scoliosis, or who were missing data related to the primary outcomes (height, weight, curve location, curve magnitude) were excluded. Inclusion and exclusion criteria, data abstraction forms and processes, and predictor and dependent variables were specified a priori as part of the overall approach to reduce bias.16
One member of the study team (BB) reviewed charts from all patients who presented between 2015–2019 to determine eligibility and extract routinely collected data from the patient’s first appointment, related to the variables of interest. A second team member (NW) independently verified data extraction. Extracted data included: sex, age, weight (kg), height (cm), magnitude of spinal curvature (Cobb angle), location of curve apex (thoracic, thoracolumbar, lumbar, double major). While a double major curve does not specifically refer to curve location, we analyzed these as a distinct group with the rationale that this presentation may present unique screening challenges (ie, postural compensation) when compared with a single curve presentation. For those presenting with a double major curve, the Cobb angle of the largest curve was used to determine magnitude.13,14,17 BMI was calculated from the patient’s body weight and height as measured at the initial appointment (kg/m2) and BMI-for-age-percentile was derived using an online calculator.18 Referral source and skeletal maturity data (Risser sign) were extracted when documented for the initial assessment. Pain at presentation (yes/no), regular physical activity participation (yes/no), and time from referral to initial appointment were also extracted.
This study (including the protocol, forms and processes, and steps to ensure data confidentiality) was reviewed and received approval from the Health Research Ethics Board at the University of Manitoba (HS23184), and local site impact approval (RI2019:116). Approved processes to maintain data confidentiality were adhered to by the research team. The requirement to obtain individual-level consent to collect data for this retrospective review was waived by the Ethics Board based on the low risk to participants, lack of additional data collection required, and feasibility issues related to gaining consent for all potential participants. This is in compliance with Principle 32 of the Declaration of Helsinki.
Analysis
Patient characteristics were summarized and reported using descriptive statistics (mean, median, range). Spearman correlation coefficient was used to quantify the relationship between spinal curvature (degrees) and BMI percentile. The Kruskal–Wallis test was used to examine the association between BMI percentile and curve location. A linear regression model was conducted to determine whether an interaction existed between BMI percentile and curve location with respect to curve magnitude, which would allow for the relationship between BMI and curve magnitude to depend on location. BMI data was analyzed as continuous data due to the small number of youth in the ≥85th percentile category within this sample. The Kruskal–Wallis test was used for exploratory analysis related to BMI and referral source, presence of pain, and skeletal maturity. For the referral source, data were collapsed into the two main referral sources (family physician, family member) and the category of “other” for this analysis due to low observations for many referral categories. Chi-Square testing was used for exploratory analyses related to pain and physical activity participation at presentation. Analyses were performed with SAS version 9.4 (SAS Institute, Cary NC).
Results
Two hundred and fifty patient charts were initially screened for study inclusion. After excluding charts of patients that did not meet inclusion criteria, 206 remained (177 females, 29 males). Patient characteristics are summarized in Table 1. The mean BMI of the 206 patients was 19.7 kg/m2 (SD 3.7); mean BMI percentile was 48.3 (SD 30.5); 91.3% of patients had a BMI <85th percentile.
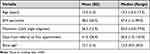 |
Table 1 Patient Characteristics |
Eighty-five patients presenting to the scoliosis clinic were diagnosed with a double major curve, 55 patients with a curve in the thoracic spine, 47 with a thoracolumbar curve, and 19 with a curve in the lumbar spine (Table 2). The mean maximum Cobb angle was 26.5 degrees (range 10.0–77.0, SD 12.9). The majority of patients had scoliosis initially detected by a family physician during routine physical exam (n=129; 62.6%). The next most common initial detection method was by a family member (n=45; 21.8%), followed by a health care provider other than a family physician (n=11; 5.4%). For the remaining 10.2% of patients, concern about spinal alignment was raised by a teacher, coach/dance instructor, or friend. Eighty-one (39.3%) patients reported pain related to scoliosis at presentation, and 134 patients (65.0%) reported participation in some form of regular physical activity. The mean time from receipt of referral to initial assessment at the scoliosis clinic was 41 days (SD 26.9).
 |
Table 2 Curve Location, Magnitude, and BMI Percentile |
BMI Percentile and Spinal Curvature
BMI is reported as percentile only due to clinical relevance. There was no correlation between degree of spinal curvature and BMI percentile with all curve locations combined (Spearman r=0.11, p=0.12), however an association was present between curve location and BMI percentile (Table 2). To test whether the relationship between BMI and degree of curvature differed by curve location, a linear regression model was created with spinal curvature angle as the dependent variable and BMI percentile, curve location, and their interaction as predictors. A significant interaction existed between BMI percentile and curve location (p=0.0017; Figure 1). In this cohort, there was a positive association between BMI percentile and curve magnitude in adolescents with a double major curve (β = 0.136, p=0.0019), and a negative association between these variables in adolescents with a thoracic curve (β = −0.125, p=0.015). The association between BMI percentile and curve magnitude was not significant for either lumbar (β = 0.049, p=0.57) or thoracolumbar (β = −0.005, p=0.94) locations.
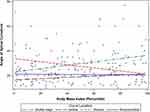 |
Figure 1 Scatterplot depicting relationship between BMI percentile, magnitude of curve, and curve location. |
Exploratory univariate analyses indicated borderline significance between BMI and who initially detected the child’s curve (referral source). Median BMI percentile for adolescents referred by family physicians, family members, or “other” was 46th, 33rd, and 64th percentile respectively (p=0.05). Similarly, there was a borderline significant relationship between BMI percentile and a history of pain at first assessment (yes/no) (p=0.06; Kruskal–Wallis test) such that adolescents with a higher BMI tended to be more likely to have pain at presentation. No significant relationship existed between BMI and skeletal maturity as measured by the Risser sign (p=0.58), and no there was no apparent relationship between active participation in physical activity (yes/no) and pain (yes/no) at initial assessment (p=0.67, Chi-Square test). Inferences may be limited by using crude binary measures of pain and physical activity, and missing documentation related to pain at presentation (missing for 31 patients) and skeletal maturity (missing for 137 patients).
Discussion
This retrospective review examined the charts of 206 adolescents who had been referred to a scoliosis clinic at a pediatric tertiary care facility, to determine the relationship between BMI percentile and curve magnitude at presentation to scoliosis clinic within this clinical cohort. When data from all included adolescents were analyzed together, no relationship between BMI percentile and degree of curvature was detected. However, when the data were analyzed by the location of the spinal curve, adolescents with a double major curve and a higher BMI percentile, or a thoracic curve and a lower BMI percentile were more likely to have a larger Cobb angle.
Other authors have not included double major curves within their primary analyses related to the location of the spinal curve, however Goodbody et al reported that patients in their study with a BMI ≥85th percentile were 12.6 times more likely to present with a double major curve when compared to those with a BMI <85th percentile.14 Relative to other curve types, these can be more difficult to detect with visual screening as the double curve acts to compensate for trunk asymmetries. In contrast, patients presenting with a thoracolumbar curve often demonstrate a shift in trunk posture or alignment, where the base of the skull is no longer in alignment with the center of the sacrum, making these curves easier to detect. In patients presenting with a double major curve, curve detection is more often based on more subtle asymmetries often seen in the shoulders or waist. Additionally, soft tissue, whether muscle or adipose, may be more likely to obscure typical skeletal examination findings such as rib hump and spinal prominences.
With that, it may seem counterintuitive that in our study and another by Matusik et al,15 adolescents with a lower BMI and thoracic curve were also more likely to present with a larger curve magnitude. A potential explanation could stem from literature reporting that adolescents with scoliosis reported liking “baggy clothes/nice clothes” compared with “clothes that fit right/expensive clothes/wearing the right clothes” as reported by adolescents without AIS.19 This study by Merenda et al was conducted with adolescents already confirmed to have AIS, thus it is not clear if reported clothing preference was influenced by efforts to conceal a curve/trunk shift, or to accommodate treatment with bracing. Regardless, it is a reminder to clinicians that baggy clothing may conceal a spinal curve that may otherwise be detected by parents or educators and highlights the role of routine clinical physical exam of spinal alignment for early detection. Of note, females with AIS have been reported to often have a lower BMI percentile compared to peers without scoliosis.20,21 Several reasons have been suggested for this, including eating behaviors or co-occurring eating disorders, however the research on this is not conclusive.22 Study in this area is ongoing, and endocrine dysregulation (considering the relationship between leptin, adiponectin, ghrelin, body composition, and bone development) as a precursor and contributor to AIS is offered as a more contemporary explanation for the typically lower BMI observed in adolescents with AIS.22,23 As in any clinical encounter, we advocate for the acknowledgement of the complex interplay between physical development, body image, psychological health, and physical health when screening for scoliosis. A 2018 review underlines this point, reporting that 35–50% of adolescents with AIS were found to have body image disturbances including self-consciousness and social limitation due to appearance in comparison to 15% in comparison groups of adolescents without AIS.23 Sensitive approaches to subjective and physical examination are warranted.
In our sample, most patients’ curves were initially detected by a primary care provider on annual routine screening, however exploratory analyses suggest that those referred by sources other than these were more likely to have a higher BMI. This aligns with other authors who have described a trend demonstrating that patients with a higher BMI were more likely to have their curve noticed by the school or by incidental findings.14 Exploratory analyses also suggest a relationship between the presence of pain at first assessment and BMI percentile. While these findings need to be further explored due to the simple yes/no format of clinical data collection related to pain and exploratory nature of the analysis, pain related findings may be considered by primary care providers as a symptom to help prompt assessment to ensure timely diagnosis of AIS. No relationship was found between presence of pain at first assessment and physical activity participation, and in contrast to previous studies, we did not find a significant relationship between BMI and skeletal maturity.14 This may have been because of missing data in our sample as skeletal maturity was not consistently documented upon initial assessment.
The present study was initiated after considering published reports of late referral to scoliosis clinics for adolescents with a higher BMI. We wanted to determine whether this was the case in our clinic, and whether targeted education was required for pediatricians, family physicians, and others who refer to the clinic to ensure that youth with a higher BMI were not systematically disadvantaged and limited in treatment options or outcomes by late referrals. While relationships were present, the nature of the relationship varied by the location of the curve. A limitation of this study is the small number of referred patients with a BMI >85th percentile, and the strength and nature of the associations reported must be interpreted relative to the characteristics of this sample. We cannot comment on who has not been referred to this clinic, a limitation inherent to a single-site retrospective study. It is possible that more subtly noticeable differences in spinal alignment (ie, for double major curves), weight bias, or other systemic factors known to limit access to the healthcare system may have prevented the referral of certain children, including those with a higher BMI, to the scoliosis clinic for evaluation. Further, we are unable to comment on who was referred directly to a surgical specialist as opposed to the clinic for evaluation and care. We were unable to obtain data on race, ethnic identity, or socioeconomic status as these data are not routinely recorded in the clinical setting, and thus could not perform analyses related to these important factors. It is well known that systemic barriers to accessing the healthcare system are an ongoing reality for many families. Clinicians should be aware that others have reported a negative association between median family income and the magnitude of thoracic curve for adolescents.13
Conclusion
Data from this retrospective review demonstrated two distinct relationships relating to a larger Cobb angle at presentation: i) adolescents presenting to the clinic with a double major curve and a relatively higher BMI percentile, and ii) adolescents with a thoracic curve and a relatively lower BMI percentile. When screening for a double major curve, clinicians need to be especially cognizant to assess for subtle asymmetries such as scapular and pelvic asymmetries as well as a rib hump on Adam’s forward bending test. While thoracic curves are typically more easily observed in adolescents with a lower BMI, our findings suggest that these too can be obscured and progress. Considering findings from other research related to scoliosis, body composition, and body image, and recognizing the presence of systemic barriers to accessing care, we present our findings alongside a reminder of the importance of sensitive history taking and careful physical examination for early detection of scoliosis.
Acknowledgments
This project was supported by funding received through the Health Sciences Centre Foundation Allied Health Research Award (2019). The funder had no role in data collection, interpretation, or reporting. KW is supported in part through the Dr. John M Bowman Chair in Pediatrics and Child Health, a partnership between the Winnipeg Rh Institute Foundation and the Department of Pediatrics and Child Health, University of Manitoba; and holds affiliations with the Children’s Hospital Research Institute of Manitoba, the Rehabilitation Centre for Children and SSCY Centre, Winnipeg Manitoba Canada.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Asher MA, Burton DC. Adolescent idiopathic scoliosis: natural history and long term treatment effects. Scoliosis. 2006;1(1):2. doi:10.1186/1748-7161-1-2
2. Horne JP, Flannery R, Usman S. Adolescent idiopathic scoliosis: diagnosis and management. Am Fam Physician. 2014;89(3):193–198.
3. Reamy BV, Slakey JB. Adolescent idiopathic scoliosis: review and current concepts. Am Fam Physician. 2001;64(1):111–116.
4. Dunn J, Henrikson NB, Morrison CC, Blasi PR, Nguyen M, Lin JS. Screening for Adolescent Idiopathic Scoliosis: evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2018;319(2):173–187. doi:10.1001/jama.2017.11669
5. Richards BS, Vitale MG. Screening for idiopathic scoliosis in adolescents. An information statement. J Bone Joint Surg Am. 2008;90(1):195–198. doi:10.2106/JBJS.G.01276
6. Grivas TB, Wade MH, Negrini S, et al. SOSORT consensus paper: school screening for scoliosis. Scoliosis. 2007;2:17. doi:10.1186/1748-7161-2-17
7. Kenner P, McGrath S, Woodland P. What Factors Influence Delayed Referral to Spinal Surgeon in Adolescent Idiopathic Scoliosis? Spine (Phila Pa 1976). 2019;44(22):1578–1584. doi:10.1097/BRS.0000000000003146
8. Richards BS, Bernstein RM, D’Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine. 2005;30(18):20682076. doi:10.1097/01.brs.0000178819.90239.d0
9. Ohrt-Nissen S, Hallager DW, Gehrchen M, Dahl B. Flexibility Predicts Curve Progression in Providence Nighttime Bracing of Patients With Adolescent Idiopathic Scoliosis. Spine (Phila Pa 1976). 2016;41(22):1724–1730. doi:10.1097/BRS.0000000000001634
10. Cheung JPY, Cheung PWH. Supine flexibility predicts curve progression for patients with adolescent idiopathic scoliosis undergoing underarm bracing. Bone Joint J. 2020;102-B(2):254–260. doi:10.1302/0301-620X.102B2.BJJ-2019-0916.R1
11. Sanders JO, Newton PO, Browne RH, Katz DE, Birch JG, Herring JA. Bracing for idiopathic scoliosis: how many patients require treatment to prevent one surgery? J Bone Joint Surg Am. 2014;96(8):649–653. doi:10.2106/JBJS.M.00290
12. Park JH, Jeon HS, Park HW. Effects of the Schroth exercise on idiopathic scoliosis: a meta-analysis. Eur J Phys Rehabil Med. 2018;54(3):440–449. doi:10.23736/S1973-9087.17.04461-6
13. Gilbert SR, Savage AJ, Whitesell R, Conklin MJ, Fineberg NS. BMI and magnitude of scoliosis at presentation to a specialty clinic. Pediatrics. 2015;135(6):e1417–24. doi:10.1542/peds.2014-2000
14. Goodbody CM, Sankar WN, Flynn JM. Presentation of Adolescent Idiopathic Scoliosis: the Bigger the Kid, the Bigger the Curve. J Pediatr Orthop. 2017;37(1):41–46. doi:10.1097/BPO.0000000000000580
15. Matusik E, Durmala J, Matusik P. Association of Body Composition with Curve Severity in Children and Adolescents with Idiopathic Scoliosis (IS). Nutrients. 2016;8(2):71. doi:10.3390/nu8020071
16. Kaji AH, Schriger D, Green S. Looking through the retrospectoscope: reducing bias in emergency medicine chart review studies. Ann Emerg Med. 2014;64(3):292–298. doi:10.1016/j.annemergmed.2014.03.025
17. Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med. 2013;369(16):1512–1521. doi:10.1056/NEJMoa1307337
18. Centre for Disease Control and Prevention. Healthy weight, nutrition, and physical activity. Available from: https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html#percentile.
19. Merenda L, Costello K, Santangelo AM, Mulcahey MJ. Perceptions of self-image and physical appearance: conversations with typically developing youth and youth with idiopathic scoliosis. Orthop Nurs. 2011;30(6):383–390. doi:10.1097/NOR.0b013e31823710a0
20. Barrios C, Cortés S, Pérez-Encinas C, et al. Anthropometry and body composition profile of girls with nonsurgically treated adolescent idiopathic scoliosis. Spine. 2011;36(18):1470–1477. doi:10.1097/BRS.0b013e3181f55083
21. Tam EMS, Liu Z, Lam TP, et al. Lower Muscle Mass and Body Fat in Adolescent Idiopathic Scoliosis Are Associated With Abnormal Leptin Bioavailability. Spine (Phila Pa 1976). 2016;41(11):940–946. doi:10.1097/BRS.0000000000001376
22. Clark EM, Taylor HJ, Harding I, et al. Association between components of body composition and scoliosis: a prospective cohort study reporting differences identifiable before the onset of scoliosis. J Bone Miner Res. 2014;29(8):1729–1736. doi:10.1002/jbmr.2207
23. Gallant JN, Morgan CD, Stoklosa JB, Gannon SR, Shannon CN, Bonfield CM. Psychosocial Difficulties in Adolescent Idiopathic Scoliosis: body Image, Eating Behaviors, and Mood Disorders. World Neurosurg. 2018;116(421–432.e1). doi:10.1016/j.wneu.2018.05.104
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
