Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
The Reduction of After-Hours and Weekend Effects in Upper Gastro-intestinal Bleeding Mortality During the COVID-19 Pandemic Compared to the Pre-Pandemic Period
Authors Cazacu SM , Turcu-Stiolica A, Florescu DN, Ungureanu BS , Iovanescu VF, Neagoe CD, Burtea DE, Genunche-Dumitrescu AV, Avramescu TE, Iordache S
Received 24 July 2023
Accepted for publication 27 September 2023
Published 26 October 2023 Volume 2023:16 Pages 3151—3165
DOI https://doi.org/10.2147/JMDH.S427449
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Sergiu Marian Cazacu,1,* Adina Turcu-Stiolica,2,* Dan Nicolae Florescu,1,* Bogdan Silviu Ungureanu,1,* Vlad Florin Iovanescu,1,* Carmen Daniela Neagoe,3,* Daniela Elena Burtea,1,* Amelia Valentina Genunche-Dumitrescu,3,* Taina Elena Avramescu,4,* Sevastita Iordache1,*
1Gastroenterology Department, University of Medicine and Pharmacy Craiova, Clinical Emergency Hospital Craiova, Dolj County, Romania; 2Biostatistics Department, University of Medicine and Pharmacy Craiova, Dolj County, Romania; 3Internal Medicine Department, University of Medicine and Pharmacy Craiova, Clinical Emergency Hospital Craiova, Dolj County, Romania; 4Individual Sports, and Medical Disciplines Departments, University of Craiova, Dolj County, Romania
*These authors contributed equally to this work
Correspondence: Carmen Daniela Neagoe, Tel +40723767106, Email [email protected]; [email protected]
Background: In upper gastrointestinal bleeding (UGIB), admissions after normal working hours and during weekends may be associated with increased mortality.
Aim: To assess the evolution of the after-hours and weekend effects during the COVID-19 pandemic as a result of progressive improved management despite management challenges during the pandemic.
Methods: We performed an observational study of patients admitted for UGIB at a tertiary academic center between March 2020 and December 2021, compared to the corresponding timeframe before the pandemic. Admissions were assessed based on regular hours versus after-hours and weekdays versus weekends. We stratified patients based on demographic data, etiology, prognostic scores, the time between symptom onset and admission, as and between admission and endoscopy. The outcomes included mortality, rebleeding rate, the requirement for surgery and transfusion, and hospitalization days.
Results: 802 cases were recorded during the pandemic, and 1006 cases before the pandemic. The overall mortality rate was 12.33%. Patients admitted after hours and during weekends had a higher mortality rate compared to those admitted during regular hours and weekdays (15.18% versus 10.22%, and 15.25% versus 11.16%), especially in cases of non-variceal bleeding. However, the difference in mortality rates was reduced by 2/3 during the pandemic, despite the challenges posed by COVID-19 infection. This suggests that there was an equalization effect of care in UGIB, regardless of the admission time. The differences observed in mortality rates for after-hours and weekend admissions seem to be primarily related to a higher proportion of patients who did not undergo endoscopy, while the proportion of severe cases remained similar. Blood requirements, hospital days, and rebleeding rate were similar between the two groups.
Conclusion: Admissions during weekends and after-hours have been associated with increased mortality, particularly in cases of non-variceal bleeding. However, the impact of this association was significantly reduced during the pandemic.
Keywords: gastrointestinal bleeding, after-hours care, COVID-19 pandemic
Introduction
Acute upper gastrointestinal bleeding (UGIB) is associated with significant morbidity, mortality, and hospitalizations, with an estimated incidence of 40–150 cases in 100000 persons;1,2 most studies have shown a declining trend of the incidence of upper gastrointestinal bleeding in recent years.2–9 Mortality rates of 5 to 10% were noted in most centers,3,5,10–12 while even values of up to 14–15% were noted in other studies;4,13,14 a systematic review found a mortality rate between 1.1 and 11% in the analyzed studies.14 The mortality at 6 weeks in variceal bleeding is 10–20%.10 Most deaths are related mainly to significant comorbidities and poorly tolerated blood loss.4,10 Rebleeding rate is estimated between 5–20% and is associated with increased mortality.4
The etiology of acute UGIB is dominated by peptic ulcer disease, eso-gastric varices, inflammation (esophagitis, gastritis, and duodenitis), Mallory-Weiss syndrome, and tumors.4 The antithrombotic treatment represents an important etiological factor in UGIB, because of its increasing use in cardiovascular and cerebrovascular disease.15 Obscure bleeding (when no cause of bleeding was found) can be recorded in 5 to 21% of cases.7,16
Identifying severe cases is important for prognostic stratification because it can impose an earlier therapeutic intervention and be a determinant factor for admission to the intensive care unit. Several scores are used today: Rockall score and Glasgow-Blatchford score are most used,1,3,10,17 and AIM65, Baylor, Cedar Sinai, PNED, T-score, ANN, and Cambridge score were other proposed scores.3,11,17–19 The scores were used for predicting rebleeding, mortality, and the need for intervention.3,11 Machine-learning algorithms such as hyperparameter-tuned K-NN classifier may combine several scores and can increase the accuracy of mortality prediction up to 98%.20
Endoscopic therapy represents the cornerstone for the management of gastrointestinal bleeding; current guidelines recommend endoscopy within 24 hours of admission.1,4,21 In cases with severe bleeding or variceal bleeding a very early endoscopy (<12 hours of admission) may be recommended,1,3 although other studies found no advantage compared to standard 12–24h endoscopy.22–24 2–3% of patients may need surgery and, when available, 1–3% may undergo embolization.3
Admissions during weekends or after normal working hours may be associated with a slight increase in mortality, especially in cases of non-variceal bleeding.8,13,25–27 This phenomenon is commonly referred to as the “weekend effect” and “after-hours (or off-hours) effect”, respectively, with an odds ratio of 1.06–1.09 for in-hospital mortality.26,28–30 In the case of non-variceal UGIB, a meta-analysis showed an OR of 1.09 for mortality patients admitted on weekends.30 Another review found that weekend admission for UGIB was associated with higher in-hospital and 30-day mortality rates.31 Several explanations have been proposed, such as reduced availability of trained personnel implied in therapeutic endoscopic and non-endoscopic procedures in UGIB during after-hours and weekend admissions, fewer staff available for the same workload compared with working days, reduced performance of intensive care procedures, and possible an increased admission of more severe cases during weekends;31 the effect is negligible in hospitals that provide out-of-hours endoscopy on-call rotation.26
The global COVID-19 pandemic emerged in early 2020 and quickly spread worldwide.32–35 It has led to multiple negative consequences on the healthcare system due to the initial lockdown, subsequent restrictions, the need for dedicated personnel and circuits for SARS-COV2 patients, medical staff redistribution (including out-of-work personnel), the need for patients’ triage, and the impact of patient’s fears regarding hospital presentations and admissions.33,34 An increased mortality rate among COVID-19-positive patients with UGIB was noted,36 as well as the redistribution of medical staff, delays in presentation, admissions to the hospital, and medical procedures. This, in turn, could exacerbate the after-hours and weekend effects during the pandemic period. However, it is worth noting that improvements in personnel training on endoscopy and medical care, better scheduling, and enhanced organizational measures may counterbalance these effects over time. These advancements can lead to a reduction in both mortality and the impact of weekend and after-hours admissions, as a result of better care for UGIB patients.
The purpose of the study was to assess the impact of admission time and day, as well as the influence of the pandemic period on the outcomes of the patients admitted for UGIB (mortality rate, rebleeding rate, endoscopic hemostasis failure rate, need for transfusion, and hospitalization duration).
Methods
We performed an observational study on all patients admitted for acute UGIB at the Clinical Emergency Hospital Craiova (a tertiary academic hospital that admitted all cases of UGIB in our county and severe cases from neighboring counties). Data from patients were extracted from the Hippocrates computerized system of the hospital. We selected patients aged 16 years and older admitted for UGIB with specific ICD-10-AM codes, including esophageal disease with bleeding (K22.0 and K22.2), gastric, duodenal, peptic or gastro-jejunal ulcer with bleeding (K25.0, K25.4 K26.0, K26.4, K27.0, K27.4, K28.0, K28.4), hemorrhagic gastritis or duodenitis (K29.0), bleeding angiodysplasia (K31.82), hematemesis (K92.0), melena (K92.1), gastrointestinal bleeding (K92.2), esophageal varices with bleeding (I85.0). Patients with lower gastrointestinal bleeding were excluded by reviewing the admission data for patients. Informed consent was obtained from all admitted patients, and the study protocol received approval from the local ethical committee of the Clinical Emergency Hospital Craiova (Protocol no 11977/24 March 2020). In patients aged below 18 years (two patients), the informed consent was also signed by the parents.
Two groups of patients were identified for the study: those admitted during the period from March 2020 to December 2021 period (referred to as the pandemic period) and those admitted during the period from March 2018 to December 2019 (matched pre-pandemic period). For each patient, we recorded the following data: demographic information (age, gender), comorbidities, clinical parameters at admission (such as hematemesis, melena, syncope, altered level of consciousness, blood pressure, pulse, ascites, and encephalopathy for cirrhotic patients), antithrombotic therapy, alcohol and non-steroidal anti-inflammatory drugs, and various biological parameters (including hemoglobin level, blood urea nitrogen, INR, serum albumin, and total bilirubin), blood units transfused, information related to endoscopy. The analysis was conducted by stratifying the patients based on risk factors for mortality, utilizing pre-endoscopic and post-endoscopic scores (such as the original and modified Glasgow-Blatchford score, Rockall and Baylor bleeding scores, AIMS65, Cedar-Sinai, and T-score).11 We also assessed the Charlson comorbidity index in patients with UGIB and employed the Child classification for patients with cirrhosis. The date and time of admission and endoscopy, as well as the date of discharge, and the time between onset and admission and between admission and endoscopy were recorded. UGIB cases were categorized into four groups: variceal, non-variceal, obscure (when no lesion was noted during endoscopy and no risk factors, such as antithrombotic therapy, were identified), and unknown (when endoscopy was not performed due to patient refusal, dementia, immediate death, or other contraindications).
Regular endoscopy was performed between 8 am and 8 pm during working days (with emergency endoscopies performed until 11 pm) and between 8 am and 3 pm during weekends and holidays (also with emergency endoscopies performed until 11 pm). After-hours cases were considered as weekday admission between 8 pm and 8 am and weekend admissions after 3 pm (after the regular endoscopy schedule). Weekend admissions included cases admitted Saturday, Sunday, and legal holidays.
During the pandemic period, the Gastroenterology Department in our hospital has admitted all cases presenting with upper gastrointestinal bleeding from our county, including patients with COVID-19 infection. Patients were evaluated by epidemiologic triage, by pulmonary X-Ray, by rapid antigen testing and by PCR testing in case of suspected cases; most patients were examined by endoscopy in the first 24 hours; hemodynamically unstable cases or with ongoing bleeding who were positive or suspected for COVID infection were evaluated by emergency endoscopy in dedicated endoscopy room.
The main outcome assessed in this study was in-hospital mortality. Secondary outcomes included the rebleeding rate, endoscopy failure rate, the rate of emergency surgery, the need for transfusion, and mean hospitalization days.
Statistical data were analyzed and provided using GraphPad Prism v.9.5.1 for Windows (GraphPad Software, San Diego, California USA, www.graphpad.com). Continuous variables were compared using the Mann–Whitney test, while the Chi-square test was used for categorical variables. Descriptive data were generated to describe patient characteristics, including percentages for categorical variables and means with standard deviations, as well as medians with interquartile range for continuous variables. The association between mortality and various factors was quantified with odds ratio (OR). Univariate and multivariate analysis, employing binomial logistic regression, were conducted to evaluate the associations between mortality risk and factors such as age, gender, the use of anti-thrombotic drugs, alcohol abuse, cirrhosis, endoscopy, endoscopic treatment, the interval between admission and endoscopy, bleeding type, pandemic or pre-pandemic period, the presence of COVID-19 infection during the pandemic, week-in or weekend admission, regular hours versus after-hours admission and Glasgow-Blatchford bleeding score. In the statistical modelling, the dependent variable was adjusted for other factors with a p-value less than 0.1. Hosmer and Lemeshow test was applied to examine the fit of all the models. Large values of the log-likelihood statistic indicate poorly fitting statistical models, because the larger the value of the log-likelihood, the more unexplained observations there are. A two-tailed p<0.05 was considered to be statistically significant.
Results
Characteristics of the Patients Were Presented inTable 1
During the pandemic period, a total of 802 cases were recorded, compared to 1006 cases in a similar pre-pandemic period. The total rebleeding rate was 4.65%; emergency surgery was necessary for 1.22%. The mortality rate for patients who did not undergo endoscopy was 45.73%; in contrast, the mortality rate for patients who underwent endoscopy was 7.37% (OR=10.5896, 95% CI 7.6956 to 14.5719; p< 0.0001). Among patients who received endoscopy, the mortality rates were as follows: 8.7% for those with endoscopy performed within the first 6 hours, 8.2% for those within the first 12 hours, 7.3% for those within the first 24 hours, and 7.9% for those who underwent endoscopy after 24 hours.
 |
Table 1 The Main Characteristics of Patients Admitted During Regular Hours /After-Hours and Weekends/Weekdays |
UGIB and the Time of Admission for the Whole Analyzed Period
Outcomes
The mortality rate was higher for after-hours admission (15.18%) compared to those admitted during regular hours (10.22%) (OR=1.5713, 95% CI, 1.1861–2.0815, p=0.0016), similarly, the mortality rate was higher for weekend admissions (15.25%) compared to admissions during working days (11.16%) with an OR of 1.4321 (95% CI 1.0656 to 1.9248, p=0.0173). The effect was mainly noted for non-variceal bleeding for after-hours versus regular hours admissions (9.49 versus 5.33%, OR 1.8613, 95% CI 1.1974 to 2.8932, p=0.0058) and in weekend versus working days admissions (11.02 versus 5.47%, OR 2.1462, 95% CI 1.3809 to 3.3355, p=0.0007). However, in cases of variceal bleeding, statistical significance was not obtained for both after-hours (OR=1.0768, 95% CI 0.6378 to 1.8180, p=0.7818) and weekend admissions (OR=0.7166, 95% CI 0.3847 to 1.3346, p=0.2935). Among patients who did not undergo endoscopy, the mortality rate seems higher in those admitted after hours and during weekends compared to those admitted during regular hours and weekdays, although statistical significance was not achieved.
Surprisingly, the rebleeding rate was higher for patients admitted during weekdays compared to those admitted during weekends. However, the rebleeding rate was similar between patients admitted during after-hours and regular hours. Failure of endoscopic hemostasis, mean hospital days, percentage of transfused patients, and the mean number of blood units administered were similar regardless of admission timing.
Factors That Can Explain Mortality Differences Related to Admission Time/Date
Gender distribution was similar among different admission timings. However, a higher percentage of patients above 80 years old were admitted during the weekend compared to weekdays (14.5% versus 9.8%, p-value=0.0084). The etiology of bleeding was similar, except for a higher proportion of bleeding associated with anti-thrombotic therapy in both after-hours (OR=1.9304, 95% CI 1.2220–3.0494, p=0.0048) and weekend admissions (OR=1.25, 95% CI 1.0498–1.4884, p=0.0122). The proportion of cirrhosis was similar across different admission timings.
Regarding endoscopy, it was found that for after-hours admissions, a higher percentage of patients (19.1% versus 8.4%) did not undergo endoscopy. Additionally, fewer patients performed endoscopies within the first 12 hours, and the percentage of endoscopies performed at 24 hours was also lower. The average time between admission and endoscopy was longer for after-hours admissions compared to regular hours (21.96h versus 14.23h, p<0.0001). In the case of weekend admissions, more patients had no endoscopy performed (20.08 versus 10.08%, OR=2.2415, 95% CI 1.69 to 2.97, p<0.0001). However, the proportion of therapeutic endoscopies was similar between weekends and working days (24.5% vs 24.6%, p=0.9498). Fewer patients performed endoscopy within the first 12 hours, but a similar proportion of patients performed endoscopy within the first 24 hours (81.2% during weekends versus 84.1% during working days, p=0.2409). The percentage of therapeutic endoscopies was also similar between weekends and working days.
The interval between the onset of symptoms and presentation to the emergency room was similar for both weekend (57.5 hours) and weekdays admissions (58.9 hours), with no significant difference observed (p=0.7407) However, a notable 19% reduction in the mean time between admission and endoscopy was noted for weekend admissions compared to weekdays (16.3 hours versus 20.2 hours, p=0.0327).
We also analyzed average prognostic scores about admission time to assess if there is a difference in case severity in relation to admission time. Mean values for the original and modified Glasgow-Blatchford scores were slightly higher in patients admitted after-hours while Rockall post-endoscopic score was slightly higher in patients admitted during regular hours and weekdays; Baylor, Cedars-Sinai, AIM65 T-score, and Charlson comorbidity index were similar. We can appreciate that the severity of UGIB was similar for after-hours and regular hours and for weekday and weekend admitted patients (Table 2).
 |
Table 2 Characteristics of UGIB for Admission During Regular Hours/After-Hours and Weekends/ Weekdays |
In order to further study the differences regarding mortality in patients with non-variceal bleeding, we analyze the differences regarding potentially risk factors in relation to the admission time. Age and gender distribution was similar regardless of admission time; rebleeding rate was higher in weekday admissions. Prognostic scores were similar; the proportion of patients with endoscopy performed during the first 24 hours was similar, but the average time between admission and endoscopy was higher in after-hours versus regular hours (21.2 versus 14.8, P=0.0006) but not in weekend versus weekdays (18.5 versus 17, P=0.4742).
Multivariate Analysis for the Differences Related to Admission Time/Date
To assess if admissions during weekends and after-hours were an independent factor for mortality, we performed a multivariate analysis using logistic regression to examine the differences between regular hours and after-hours admissions, as well as between weekday and weekend admissions. The following risk factors were included in the analysis: rebleeding (yes/no), emergency surgery(yes/no), type of bleeding (variceal versus non-variceal, and obscure versus non-variceal), age, gender (male versus female), cirrhosis (yes/no), use of antithrombotic therapy (yes/no), alcohol abuse (yes/no), endoscopy performed (yes/no), endoscopic therapy (yes/no), Glasgow-Blatchford score, period (COVID-19 pandemic versus pre-pandemic period).
For admissions during weekends, Hosmer and Lemeshow Test for the final model demonstrated its significant value (Chi-square = 1.143, df = 2, p-value = 0.565). The results indicated a significant association with less rebleeding, lack of endoscopy performed and pre-pandemic versus pandemic period, and no association between weekend admission and age, GBS, gender, type of rebleeding, antithrombotic drugs, cirrhosis, alcohol, and endoscopic treatment. However, after adjusting by multivariate analysis, weekend admissions were associated with a higher risk of surgery (OR=3.08, 95% CI=1.14–8.28, p-value=0.026) and no endoscopy performed (OR=4.25, 95% CI=2.8–6.4, p-value<0.0001), and with a lower risk for rebleeding (OR=0.47, 95% CI=0.25–0.9, p-value=0.022) Table 3.
 |
Table 3 Multivariate Analysis in UGIB for Admissions During Weekends/ Weekdays |
For admissions during after-hours, the Hosmer and Lemeshow Test conducted on the final model demonstrated its significant value as a prediction model (Chi-square = 0.936, df = 3, p-value = 0.817), indicating a good fit of the logistic regression model. After-hours admission was found to be associated with cirrhosis, the COVID-19 period, and endoscopy. Upon adjusting for confounding factors through multivariate analysis, after-hours admission was associated with no endoscopy performed (OR=4.25, 95% CI=2.8-6.4, P<0.0001), with the pre-pandemic period (OR=1.42, 95% CI=1.16–1.74, p-value=0.001), and with the presence of cirrhosis (OR=1.34, 95% CI=1.08–1.67, p-value=0.008), Table 4.
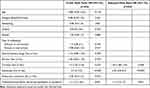 |
Table 4 Multivariate Analysis in UGIB for Admissions During Regular Hours/ After-Hours |
We also analyzed the mortality risk related to the weekend/weekday and after-hours/regular hours admissions in multivariate analysis. The Hosmer and Lemeshow Test conducted on the final model demonstrated its significant value (Chi-square = 12.72, df = 8, p-value = 0.122). Death was found to be associated with rebleeding, type of bleeding, the presence of cirrhosis, and high GBS. No significant association was found between death and age, gender, antithrombotic drugs, alcohol, surgery, the COVID-19 period, weekend/weekday and after-hours/regular hours admissions, and also with endoscopic treatment. After adjusting for confounding factors through multivariate analysis, a significantly increased risk of death was observed in cases of rebleeding (OR=5.9, 95% CI=3.3–10.6, p-value<0.0001), obscure type of rebleeding (OR=2.8, 95% CI=1.2–6.5, p-value=0.017), surgery (OR=3.08, 95% CI=1.1–8.3, p-value=0.026), cirrhosis (OR=2.8, 95% CI=1.6–5.1, p-value=0.001), and high GBS (OR=1.2, 95% CI=1.1–1.3, p-value<0.0001). A significantly increased risk of death was also observed in cases with no endoscopy (OR=14.98, 95% CI=9.09–24.67, p-value<0.0001) Table 5.
 |
Table 5 Mortality Risk in UGIB Multivariate Analysis |
We calculated adjusted mortality in patients admitted after-hours/regular hours and during weekends/weekdays, respectively, by assuming an equal rate of endoscopy in both regular hours/after-hours or weekday/weekend settings. Adjusted mortality was 10.37/10.22% for admissions during after-hours/regular hours (P-value 0.9149) and 10.66/11.16% for admissions during weekends/weekdays (P-value 0.7378), which demonstrated that lack of endoscopy may be a main culprit for mortality differences.
The Evolution of After-Hours and Weekend Effects During the Pandemic Period
During the pandemic period, a higher proportion of patients with UGIB were admitted after hours than during regular hours (47.9 versus 38.5%, OR=1.4694, 95% CI 1.2176 to 1.7732, P=0.0001); the proportion of admissions during weekends was, however, similar (27.3% during pandemic and 29.7% before pandemic, P=0.2593). Age, gender, and etiology were similar. More patients had no endoscopy performed in after-hours admissions and the time from admission to endoscopy was over 10h higher, which may be related to the lower number of emergency endoscopies in after-hours settings.
By comparing the pandemic period with the similar pre-pandemic period, the difference in global mortality between after-hours and regular-hour admissions was 6.8% in the pre-pandemic period and 2.4% in the pandemic period (a decrease of 64.7%) Figure 1; during the pandemic, we noted no statistically significant difference regarding global mortality, variceal bleeding mortality, non-variceal bleeding mortality, and the only difference was recorded regarding non-variceal mortality in cirrhotic patients (with no statistical significance, possibly because of the small number of cases). In after-hours admissions, we also noted reduced mortality for patients with non-variceal bleeding and for those without endoscopy during the pandemic period, with increased mortality during regular hours for non-variceal bleeding cases (an equalization effect). In patients with no endoscopy performed, the difference in mortality has decreased and had no statistical significance during the pandemic (P=0.1763). The differences regarding the percentage of patients without endoscopy and admission to endoscopy time were maintained during the pandemic period (Table 6).
 |
Table 6 UGIB Characteristics, Outcomes, and Endoscopic Timing Characteristics for Patients Admitted During Regular Hours/After-Hours and Pandemic/Pre-Pandemic Period |
Similar data were obtained by analyzing admissions during weekends compared with weekdays during the pandemic period. The difference in global mortality between weekend and weekday admissions has decreased from 5.7% to 2% (65% reduction) Figure 2. During the pandemic period, there was a smaller and statistically not significant difference in overall mortality, variceal bleeding mortality, and non-variceal bleeding mortality, suggesting an equalization effect. In weekend admissions, a higher number of patients had no endoscopy performed, but the time from admission to endoscopy was similar to weekday admissions. During the pandemic, in non-variceal bleeding cases, a decreased mortality in weekend admissions was associated with an increased mortality in weekday admissions, which contributed to the equalization effect (Table 7). The percentage of variceal bleeding and cirrhosis cases was similar between weekend and weekday admissions. There were no differences regarding average prognostic scores for both after-hours/regular hours and weekend/weekdays admissions, respectively.
 |
Table 7 UGIB Outcomes and Endoscopic Timing Characteristics for Patients Admitted During Weekdays/Weekends and Pandemic/Pre-Pandemic Period |
Discussions
The total mortality rate in our study was 12.33%. Specifically, it was 7.12% for non-variceal bleeding, 18.9% for variceal bleeding, and 7.43% for patients who performed endoscopy. The need for emergency surgery was 1.22%. In a previously published study conducted in a center with a permanent 24/7 endoscopy service, the global mortality rate from all causes of UGIB was reported as 10.43%, with a mortality rate of 13.4% for variceal bleeding. The rebleeding rate in that study was 12.02% and the rate of emergency surgery for non-variceal bleeding was 3.68%.37 In our study, the global rebleeding rate was 4.65% and was associated with a mortality rate of 29.8%, similar to a study that noted that 27% of patients with rebleeding died.9
In our study, both after-hours and weekend admissions were related to higher mortality, with a difference ranging from 36% to 49%. However, this difference was mainly observed in cases of non-variceal bleeding and was not significant in variceal bleeding. After-hours admission was noted in some studies as a risk factor for higher mortality,26,27,37,38 while other studies did not show any difference;39–41 some studies8,25 also suggest a “weekend effect” for UGIB with higher mortality (up to 10–20%) and higher rates of rebleeding, while other studies found no such effect.5,28,36,39,42 A meta-analysis of 96 studies found an increased risk for mortality in weekend admissions (relative risk, 1.19; 95% confidence interval, 1.14–1.23).43 The presence of an emergency on-call 24h endoscopy service may be an explanation for the lack of difference observed in some studies.30 Studies in variceal bleeding have shown no difference in mortality between weekend and weekday admissions, possible because patients with variceal bleeding have usually more severe disease, and the time of admission may have only a minor role in mortality;31 early treatment with vasoactive agents and a perception of urgent endoscopy which lower the time before esophageal band ligation therapy may be also involvement in reducing mortality regardless of admission time.26
The differences in mortality between after-hours/regular-hour admissions and weekend/weekday admissions seem to be explained in our study mainly by a higher proportion of cases with no endoscopy performed in after-hours/weekend admissions (19.1 versus 8.4% in after-hours versus regular-hour patients and 20.08 in weekend versus 10.08% in weekdays) and possibly by a higher time between admission and endoscopy. In our study, patients with no endoscopy performed had higher mortality regardless of admission timing (45.73 compared with 7.37%). In a large, country-scale study that included all UGIB admitted in the USA between 2007–2013, patients without endoscopy are three times more likely to die than those with endoscopy.21
The need for emergency endoscopy has been suggested as a risk factor for increased mortality,44 although other studies did not find a significant association.30 Several explanations have been proposed for the increased mortality observed on weekends, including factors such as staffing and resource limitations (such as less experienced healthcare providers, poor continuity of care), lower quality of care, lack of availability of urgent endoscopy,5,25 higher prevalence of comorbidities, or more severe illness.8 On the other hand, the availability of 24/7 endoscopy services has been identified as the main contributing factor in studies where no difference in mortality was observed.26,44
In our study, the difference in staff experience was not considered a contributing factor to the observed difference in mortality, because the same medical personnel were involved in both regular and after-hours endoscopy and the overall clinical care of the patients. Additionally, there were no significant differences in the rebleeding rate or the rate of therapeutic endoscopies between the two groups. Furthermore, the severity of UGIB was also ruled out as a potential explanation since key characteristics such as age, mean scores, percent of cirrhosis, prognostic scores, and occurrence of variceal bleeding were similar between the groups.
The average time from admission to endoscopy in our study was 17.3 hours, which aligns with existing literature findings. In an audit conducted across 20 centers in the UK, the median time until endoscopy was reported as 21.2 hours, with early endoscopy performed in 58.9% of cases.45
Compared to the pre-pandemic period, both after-hours and weekend effects have been reduced by 64–65% during the pandemic, despite the challenges posed by the COVID-19 infection and the implementation of epidemiological triage protocol. However, the differences regarding the endoscopy rates and the mean time from admission to endoscopy persisted during the pandemic. These findings suggest an improved applications of current treatment protocols for UGIB, and also an increasing experience for gastroenterology and intensive care unit teams during the pandemic, although further progress in endoscopy access for patients with UGIB is required to further reduce mortality; future studies for post-pandemic period (2022–2023) may be useful in order to see if the improvements can further reduce the mortality differences related to the admission time. During the pandemic, there was also a significant reduction in mortality between after-hours/weekends admissions and working hours/weekdays admissions in cases of non-variceal bleeding, indicating an improvement in the management of these patients.
Several studies suggested that patients admitted during the weekend were more prone to experience shock, and hematemesis, and require blood transfusions.28,39 In our study, we found a higher percentage of patients with hematemesis on weekends compared to weekdays (58.8% versus 52.6%, OR= 1.2825, 95% CI 1.0436 to 1.5761, p=0.0180). The presence of shock was similar between weekends and weekdays (6.55% versus 6.37%, p= 0.8786), but there was a higher percentage of patients requiring blood transfusions.
Conclusions
In our study, both after-hours and weekend admissions were associated with a higher mortality especially for non-variceal bleeding, with a difference ranging from 36% to 49%. The main contributing factor appears to be the increased proportion of patients with no endoscopy performed, which was twice as high in after-hours and weekend admissions. Additionally, there was an increased mortality observed in patients admitted after hours with no endoscopy performed, and a potential delay in the time admission between admission and endoscopy for after-hours admissions, which can be an explanation for the differences regarding the mortality in non-variceal bleeding.
Compared to the pre-pandemic period, both after-hours and weekend effects have been reduced during the pandemic by 64–65%, despite the problems occurring because of COVID-19 infection and epidemiological triage protocol. Although still more patients had no endoscopy performed in after-hours admissions and the time from admission to endoscopy was higher, no statistically significant difference was noted regarding global mortality, variceal mortality, non-variceal mortality, which suggests an equalization of management over time in UGIB related to admission timing and a continued improvement of UGIB protocol implementation, associated with an increased experience for all healthcare specialists involved in UGIB management.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of the EMERGENCY HOSPITAL OF CRAIOVA (protocol code 11977/24.03.2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the ERASMUS + Programme, Key Action 2, Cooperation partnerships in higher education, the project “Development of New Skills for Medical Students in Pandemic Context”, under the Grant Agreement 2022-1-RO01-KA220-HED-000085385.
Disclosure
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
1. Gralnek IM, Dumonceau JM, Kuipers EJ, et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European society of gastrointestinal endoscopy (ESGE) guideline. Endoscopy. 2015;47(10):a1–46. doi:10.1055/s-0034-1393172
2. Garber A, Jang S. Novel therapeutic strategies in the management of non-variceal upper gastrointestinal bleeding. Clin Endosc. 2016;49(5):421–424. PMID: 27744662; PMCID: PMC5066413. doi:10.5946/ce.2016.110
3. Lu Y, Loffroy R, Lau JY, Barkun A. Multidisciplinary management strategies for acute non-variceal upper gastrointestinal bleeding. Br J Surg. 2014;101(1):e34–50. PMID: 24277160. doi:10.1002/bjs.9351
4. Holster IL, Kuipers EJ. Management of acute nonvariceal upper gastrointestinal bleeding: current policies and future perspectives. World J Gastroenterol. 2012;18(11):1202–1207. PMID: 22468083; PMCID: PMC3309909. doi:10.3748/wjg.v18.i11.1202
5. Youn YH, Park YJ, Kim JH, Jeon TJ, Cho JH, Park H. Weekend and nighttime effect on the prognosis of peptic ulcer bleeding. World J Gastroenterol. 2012;18(27):3578–3584. PMID: 22826623; PMCID: PMC3400860. doi:10.3748/wjg.v18.i27.3578
6. Button L, Roberts S, Evans P, et al. Hospitalized incidence and case fatality for upper gastrointestinal bleeding from 1999 to 2007: a record linkage study. Aliment Pharmacol Ther. 2011;33:64–76. PMID: 21128984. doi:10.1111/j.1365-2036.2010.04495.x
7. Masoodi M, Saberifiroozi M. Etiology and outcome of acute gastrointestinal bleeding in Iran: a review article. Middle East J Dig Dis. 2012;4(4):193–198. PMID: 24829656; PMCID: PMC3990128.
8. Ahmed A, Armstrong M, Robertson I, Morris AJ, Blatchford O, Stanley AJ. Upper gastrointestinal bleeding in Scotland 2000–2010: improved outcomes but a significant weekend effect. World J Gastroenterol. 2015;21(38):10890–10897. PMID: 26478680; PMCID: PMC4600590. doi:10.3748/wjg.v21.i38.10890
9. Hearnshaw SA, Logan RF, Lowe D, Travis SP, Murphy MF, Palmer KR. Use of endoscopy for management of acute upper gastrointestinal bleeding in the UK: results of a nationwide audit. Gut. 2010;59(8):1022–1029. PMID: 20357318. doi:10.1136/gut.2008.174599
10. Jafar W, Jafar AJN, Sharma A. Upper gastrointestinal haemorrhage: an update. Frontline Gastroenterol. 2016;7(1):32–40. doi:10.1136/flgastro-2014-100492
11. Stanley AJ. Update on risk scoring systems for patients with upper gastrointestinal haemorrhage. World J Gastroenterol. 2012;18(22):2739–2744. PMID: 22719181; PMCID: PMC3374976. doi:10.3748/wjg.v18.i22.2739
12. Ahn DW, Park YS, Lee SH, et al. Clinical outcome of acute nonvariceal upper gastrointestinal bleeding after-hours: the role of urgent endoscopy. Korean J Intern Med. 2016;31(3):470–478. PMID: 27048253; PMCID: PMC4855084. doi:10.3904/kjim.2014.099
13. Biecker E. Diagnosis and therapy of non-variceal upper gastrointestinal bleeding. World J Gastrointest Pharmacol Ther. 2015;6(4):172–182. PMID: 26558151; PMCID: PMC4635157. doi:10.4292/wjgpt.v6.i4.172
14. Jairath V, Martel M, Logan RF, Barkun AN. Why do mortality rates for nonvariceal upper gastrointestinal bleeding differ around the world? A systematic review of cohort studies. Can J Gastroenterol. 2012;26(8):537–543. PMID: 22891179; PMCID: PMC3414476. doi:10.1155/2012/862905
15. Popa P, Iordache S, Florescu DN, et al. Mortality rate in upper gastrointestinal bleeding associated with anti-thrombotic therapy before and during covid-19 pandemic. J Multidiscip Healthc. 2022;15:2679–2692. PMID: 36425876; PMCID: PMC9680964. doi:10.2147/JMDH.S380500
16. Saleem SA, Kudaravalli P, Riaz S, et al. Outcomes of upper gastrointestinal bleeding based on time to endoscopy: a retrospective study. Cureus. 2020;12(3):e7325. PMID: 32313766; PMCID: PMC7164718. doi:10.7759/cureus.7325
17. Ebrahimi Bakhtavar H, Morteza Bagi HR, Rahmani F, Shahsavari Nia K, Ettehadi A. Clinical scoring systems in predicting the outcome of acute upper gastrointestinal bleeding; a narrative review. Emerg. 2017;5(1):e36. PMID: 28286843; PMCID: PMC5325906.
18. Thandassery RB, Sharma M, John AK, et al. Clinical application of AIMS65 scores to predict outcomes in patients with upper gastrointestinal hemorrhage. Clin Endosc. 2015;48(5):380–384. PMID: 26473120; PMCID: PMC4604275. doi:10.5946/ce.2015.48.5.380
19. Monteiro S, Gonçalves TC, Magalhães J, Cotter J. Upper gastrointestinal bleeding risk scores: who, when and why? World J Gastrointest Pathophysiol. 2016;7(1):86–96. PMID: 26909231; PMCID: PMC4753192. doi:10.4291/wjgp.v7.i1.86
20. Ungureanu BS, Gheonea DI, Florescu DN, et al. Predicting mortality in patients with nonvariceal upper gastrointestinal bleeding using machine-learning. Front Med. 2023;10:1134835. PMID: 36873879; PMCID: PMC9982090. doi:10.3389/fmed.2023.1134835
21. Garg SK, Anugwom C, Campbell J, et al. Early esophagogastroduodenoscopy is associated with better outcomes in upper gastrointestinal bleeding: a nationwide study. Endosc Int Open. 2017;5(5):E376–E386. PMID: 28512647; PMCID: PMC5432117. doi:10.1055/s-0042-121665
22. Iqbal U, Anwar H, Patel H, Chaudhary A, Raymond P. Does early endoscopy improve mortality in patients with acute non-variceal gastrointestinal bleeding? A retrospective review. Cureus. 2018;10(2):e2246. PMID: 29719748; PMCID: PMC5922500. doi:10.7759/cureus.2246
23. Kim Y, Kim SG, Kang HY, et al. 비정규시간 상부위장관 출혈 환자에서 응급 내시경이 예후에 미치는 영향 [Effect of after-hours emergency endoscopy on the outcome of acute upper gastrointestinal bleeding]. Korean J Gastroenterol. 2009;53(4):228–234. Korean. Korean.
24. Jairath V, Kahan BC, Logan RF, et al. Outcomes following acute nonvariceal upper gastrointestinal bleeding in relation to time to endoscopy: results from a nationwide study. Endoscopy. 2012;44(8):723–730. PMID: 22752889. doi:10.1055/s-0032-1309736
25. de Groot NL, Bosman JH, Siersema PD, et al. Admission time is associated with outcome of upper gastrointestinal bleeding: results of a multicentre prospective cohort study. Aliment Pharmacol Ther. 2012;36:477–484. PMID: 22747509. doi:10.1111/j.1365-2036.2012.05205.x
26. Xia XF, Chiu PWY, Tsoi KKF, Chan FKL, Sung JJY, Lau JYW. The effect of off-hours hospital admission on mortality and clinical outcomes for patients with upper gastrointestinal hemorrhage: a systematic review and meta-analysis of 20 cohorts. United European Gastroenterol J. 2018;6(3):367–381. PMID: 29774150; PMCID: PMC5949970. doi:10.1177/2050640617732651
27. Dorn SD, Shah ND, Berg BP, Naessens JM. Effect of weekend hospital admission on gastrointestinal hemorrhage outcomes. Dig Dis Sci. 2010;55(6):1658–1666. PMID: 19672711. doi:10.1007/s10620-009-0914-1
28. Liu L, Hao D, Liu W, Wang L, Wang X. Does weekend hospital admission affect upper gastrointestinal hemorrhage outcomes?: A systematic review and network meta-analysis. J Clin Gastroenterol. 2020;54(1):55–62. PMID: 30119093. doi:10.1097/MCG.0000000000001116
29. Gupta A, Agarwal R, Ananthakrishnan AN. “Weekend Effect” in patients with upper gastrointestinal hemorrhage: a systematic review and meta-analysis. Am J Gastroenterol. 2018;113(1):13–21. PMID: 29134968. doi:10.1038/ajg.2017.430
30. Weeda ER, Nicoll BS, Coleman CI, Sharovetskaya A, Baker WL. Association between weekend admission and mortality for upper gastrointestinal hemorrhage: an observational study and meta-analysis. Intern Emerg Med. 2017;12(2):163–169. PMID: 27534406. doi:10.1007/s11739-016-1522-7
31. Shih PC, Liu SJ, Li ST, Chiu AC, Wang PC, Liu LY. Weekend effect in upper gastrointestinal bleeding: a systematic review and meta-analysis. PeerJ. 2018;6:e4248. doi:10.7717/peerj.4248
32. Martin TA, Wan DW, Hajifathalian K, et al. Gastrointestinal bleeding in patients with coronavirus disease 2019: a matched case-control study. Am J Gastroenterol. 2020;115(10):1609–1616. doi:10.14309/ajg.0000000000000805
33. Duan Z, Duan Q, Liu K, Zhang X, Zhou S. On behalf of Xingtai society of digestive endoscopy. Impact of the COVID-19 pandemic on acute upper gastrointestinal bleeding in Xingtai city. Gastroenterol Res Pract. 2021:5586030. PMID: 33727916; PMCID: PMC7938257. doi:10.1155/2021/5586030
34. Chiriac S, Stanciu C, Cojocariu C, et al. The impact of the COVID-19 pandemic on gastrointestinal endoscopy activity in a tertiary care center from northeastern Romania. Healthcare. 2021;9(1):100. PMID: 33477942; PMCID: PMC7833369. doi:10.3390/healthcare9010100
35. Schmiderer A, Schwaighofer H, Niederreiter L, et al. Decline in acute upper gastrointestinal bleeding during COVID-19 pandemic after initiation of lockdown in Austria. Endoscopy. 2020;52(11):1036–1038. PMID: 32408356; PMCID: PMC7653543. doi:10.1055/a-1178-4656
36. Cazacu SM, Burtea DE, Iovănescu VF, et al. Outcomes in patients admitted for upper gastrointestinal bleeding and COVID-19 infection: a study of two years of the pandemic. Life. 2023;13(4):890. PMID: 37109419; PMCID: PMC10146262. doi:10.3390/life13040890
37. Botianu A, Matei D, Tantau M, Acalovschi M. Mortality and need of surgical treatment in acute upper gastrointestinal bleeding: a one year study in a tertiary center with a 24 hours / day-7 days / week endoscopy call. Has anything changed? Chirurgia. 2013;108(3):312–318. PMID: 23790778.
38. Mohammed N, Rehman A, Swinscoe MT, Mundre P, Rembacken B. Outcomes of acute upper gastrointestinal bleeding in relation to timing of endoscopy and the experience of endoscopist: a tertiary center experience. Endosc Int Open. 2016;4(3):E282–6. PMID: 27004244; PMCID: PMC4798939. doi:10.1055/s-0042-100193
39. Jairath V, Kahan BC, Logan RF, et al. Mortality from acute upper gastrointestinal bleeding in the United Kingdom: does it display a “weekend effect”? Am J Gastroenterol. 2011;106(9):1621–1628. PMID: 21606977. doi:10.1038/ajg.2011.172
40. Abougergi MS, Travis AC, Saltzman JR. Impact of day of admission on mortality and other outcomes in upper GI hemorrhage: a nationwide analysis. Gastrointest Endosc. 2014;80(2):228–235. PMID: 24674354. doi:10.1016/j.gie.2014.01.043
41. Li Y, Han B, Li H, et al. Effect of admission time on the outcomes of liver cirrhosis with acute upper gastrointestinal bleeding: regular hours versus off-hours admission. Can J Gastroenterol Hepatol. 2018;3541365. PMID: 30631756; PMCID: PMC6304553. doi:10.1155/2018/3541365
42. Fujita M, Manabe N, Murao T, et al. Differences in the clinical course of 516 Japanese patients with upper gastrointestinal bleeding between weekday and weekend admissions. Scand J Gastroenterol. 2017;52(12):1365–1370. PMID: 28925290. doi:10.1080/00365521.2017.1377762
43. Pauls LA, Johnson-Paben R, McGready J, Murphy JD, Pronovost PJ, Wu CL. The weekend effect in hospitalized patients: a meta-analysis. J Hosp Med. 2017;12(9):760–766. PMID: 28914284. doi:10.12788/jhm.2815
44. Haas JM, Gundrum JD, Rathgaber SW. Comparison of time to endoscopy and outcome between weekend/weekday hospital admissions in patients with upper GI hemorrhage. WMJ. 2012;111(4):161–165. PMID: 22970530.
45. Siau K, Hodson J, Ingram R, et al. Time to endoscopy for acute upper gastrointestinal bleeding: results from a prospective multicentre trainee-led audit. United European Gastroenterol J. 2019;7(2):199–209. PMID: 31080604; PMCID: PMC6498807. doi:10.1177/2050640618811491
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


