Back to Journals » Journal of Inflammation Research » Volume 17
The Ratio of Red Blood Cell Distribution Width to Albumin as a Predictor for Rehospitalization Risk and Rehospitalization All-Cause Mortality in Middle-Aged and Elderly Survivors with Sepsis: An Ambispective ICU Cohort Study
Authors Tan Y, Li Y , Huang X, Zhai Z, Wang Q, Guo Y, Li J, Lu W
Received 5 December 2023
Accepted for publication 20 February 2024
Published 22 February 2024 Volume 2024:17 Pages 1227—1240
DOI https://doi.org/10.2147/JIR.S451769
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ning Quan
Yanni Tan,1,* Yameng Li,2,* Xiuxian Huang,3,* Zhenwei Zhai,3,* Qiu Wang,3,* Yanli Guo,4 Junjun Li,5 Wensheng Lu3,*
1Department of Endocrinology and Respiratory of the Third People’s Hospital of Nanning, Nanning, Guangxi, 530003, People’s Republic of China; 2Medical Department of Guangxi Academy of Medical Sciences and the People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning, Guangxi, 530021, People’s Republic of China; 3Department of Endocrinology and Metabolism of Guangxi Academy of Medical Sciences and the People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning, Guangxi, 530021, People’s Republic of China; 4Yuncheng Vocational and Technical University, Yuncheng, Shanxi, 044000, People’s Republic of China; 5Hospital Dean’s Office of Guangxi Academy of Medical Sciences and the People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning, Guangxi, 530021, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Wensheng Lu, Department of Endocrinology and Metabolism, Guangxi Academy of Medical Sciences and the People’s Hospital of Guangxi Zhuang Autonomous Region, No. 6, Taoyuan Road, Nanning, Guangxi, 530021, People’s Republic of China, Email [email protected] Junjun Li, Hospital Dean’s Office of Guangxi Academy of Medical Sciences and the People’s Hospital of Guangxi Zhuang Autonomous Region, No. 6, Taoyuan Road, Nanning, Guangxi, 530021, People’s Republic of China, Email [email protected]
Objective: To explore the relationship between red blood cell distribution width to albumin (RDW/ALB) ratio (RAR) and the risk of rehospitalization and rehospitalization all-cause mortality in middle-aged and elderly survivors with sepsis based on an ambispective longitudinal cohort from the Intensive Care Unit (ICU).
Methods: Between 2017 and 2022, 455 adults who survived the first-episode severe sepsis without recurrence for at least 3 months were included in this study. All participants were followed up every 4 weeks for 12 months. According to the tertiles of RAR, participants were divided into three groups: low-level (≤ 0.36, n = 152), moderate-level (0.37– 0.44, n = 152), and high-level (≥ 0.45, n = 151). The relationship between RAR and the risk of rehospitalization and rehospitalization all-cause mortality was evaluated.
Results: Out of 455 participants, 156 experienced rehospitalization (34.3%), of which 44 (28.2%) died. Receiver operating characteristic (ROC) analysis showed that the RAR cut-off values for rehospitalization and rehospitalization all-cause mortality were 0.4251 and 0.4743, respectively. Multivariate Cox regression analysis indicated that the RAR was positively associated with rehospitalization (P = 0.011) and all-cause mortality (P = 0.006). Compared with the low-level, the high-level RAR presented a higher dose-dependent rehospitalization risk (P = 0.02) and rehospitalization all-cause mortality (P = 0.044). The stratified analysis displayed that compared to the low-level, with the RAR increasing by 1.0, the risk for rehospitalization increased 3.602-fold in aged < 65 patients (P = 0.002) and 1.721-fold in female patients (P = 0.014). Kaplan–Meier survival analysis implied a significant positive association between the RAR and the cumulative incidence of rehospitalization and rehospitalization all-cause mortality (log-rank, all P < 0.001).
Conclusion: RAR has a reliable predictive value for the risk of rehospitalization and rehospitalization all-cause mortality in patients with sepsis. Consequently, monitoring RAR for at least 1 year after surviving sepsis in female patients aged < 65 in clinical practice is critical.
Keywords: sepsis, red blood cell distribution width, albumin, rehospitalization, rehospitalization all-cause mortality
Introduction
Sepsis is defined as a life-threatening multiple organ failure (MOF) and a fatal systemic inflammatory response syndrome (SIRS) that are caused by a dysregulated host response to infection.1 According to a recent Global Burden of Diseases report, of 48.9 million sepsis cases reported worldwide, 11 million died, accounting for 19.7% of all global deaths in 2017.2 The prevalence is still growing at a rate of 1.5% to 8.0% every year,3 of which approximately one-fifth of global deaths in that year were related to sepsis.4 In China, the prevalence and mortality of sepsis are roughly estimated to be 33.6% and 29.0%, respectively.5 From a global perspective, despite exciting advances to date in therapeutic strategies promptly controlling the spread of infection and restoring hemodynamic homeostasis, the mortality rate of sepsis has still surpassed that of acute myocardial infarction (AMI), becoming the leading cause of death in intensive care units (ICU).6 Although the true prevalence and mortality are unknown, without a doubt, sepsis has emerged as the primary cause of infection-related mortality as well as the most severe threat to public health, which puts a heavy financial, mental, and psychological burden on sufferers.7,8 Hence, the topic discussed in the current study is crucial for providing proper guidance information to routine clinical practice.
Septic shock, the deadliest complication of sepsis, is the leading cause of death in sepsis.6 The mechanism involves a series of rapid occurrences and continuous cascade amplification of intracellular molecular pathological events triggered by the activation of pro-inflammatory and anti-inflammatory mediators induced by pathogen invasion, leading to irreversible disruption of immune, neuroendocrine, and hemodynamic homeostasis.6,9 Sepsis significantly alters innate and adaptive immune responses after clinical rehabilitation, manifested as immune suppression, chronic inflammation, the persistent presence of bacteria, and even the recurrence of sepsis.10 Immune homeostasis disruption, characterized by immune suppression, is closely associated with sepsis mortality and multiple organ dysfunction.11,12 The primary pathophysiological mechanism for the recurrence of sepsis involves the restoration of immune homeostasis, which requires longer to eliminate immune suppression and re-establish metabolic adaptations in the host.13 An 8-year matched cohort study conducted by Hsiu-Nien Shen et al showed that the risk ratio of sepsis recurrence was as high as 8.89 (95% CI, 8.04–9.83) in 10,818 Taiwanese adult patients who survived at least 3 months after the first-episode sepsis.14
As essential innate immune modulators, erythrocytes bind to a broad scope of chemokines via the Duffy antigen receptor (DAR), which plays a weighty role in the functional regulation for immune suppression in sepsis.15,16 Erythrocyte deformability, in particular, is a crucial component in regulating immune suppression.17 Red cell distribution width (RDW), a measurement of heterogeneity in the size of circulating erythrocytes as part of the automated whole blood count, was found to have a negative connection with erythrocyte deformability.17 Increased RDW (decreased erythrocyte deformability) can impair the ability to pass rapidly through microcirculation channels in erythrocytes, which contributes to microcirculatory rheology disorders, cellular hypoxia, and excessive immune suppression in sepsis.17–19 RDW has been fully confirmed in association with the clinical prognosis outcomes of sepsis20,21 and cardiovascular and cerebrovascular diseases.22–24 Albumin (ALB), an essential component of human plasma, is necessary for maintaining osmotic pressure, inflammatory response, and antioxidant activity. RAR is a novel, superficial, and convenient biomarker for inflammation, which has predictive value for the prognosis in patients with acute illnesses such as severe pneumonia,25 diabetic foot,26 and acute renal injury in sepsis.27
However, previous studies have mainly focused on the prognosis of sepsis patients with short-term or long-term mortality, and few studies have explored the risk of suffering from sepsis again in survivors of the first-episode sepsis. Research on the relationship between RAR and the risk of rehospitalization and rehospitalization all-cause mortality in surviving individuals with sepsis remains sparse. The current analysis aims to explore the association between the RAR and the risk of rehospitalization and rehospitalization mortality in adult survivors with sepsis based on an ambispective cohort study from ICU for the first time.
Materials and Methods
Subjects Enrollment
Between January 2017 and December 2022, a total of 455 adult patients who survived the first-episode sepsis without recurrence for at least 3 months were eligible for inclusion in this study. This is an ambispective longitudinal clinical cohort from the Intensive Care Unit (ICU) of the Third People’s Hospital of Nanning. All participants were continuously followed up every 4 weeks for 12 months. The end-point events were rehospitalization and all-cause mortality during the readmission period. All rehospitalization patients were diagnosed with sepsis. According to the tertiles of RAR, participants were placed into three groups: low-level (≤0.36, n = 152), moderate-level (0.37–0.44, n = 152), and high-level (≥0.45, n = 151). The inclusion criteria were as follows: (1) sepsis was diagnosed according to The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3);1 (2) adult individuals who survived the first-episode sepsis without recurrence for at least 3 months. The exclusion criteria were as follows: (1) aged <18; (2) pregnant women; (3) blood transfusion and albumin replacement therapeutics history within six months before participating in this study; (4) acute phase of cardiovascular and cerebrovascular diseases, chronic heart failure, liver and kidney dysfunction, uremia hemodialysis, thyroid dysfunction, rheumatoid arthritis, malignant tumors, and other conditions that may affect RWD and ALB levels; (5) lost to follow-up, missing hospitalization data, and a follow-up time of less than a year. All patients agreed to participate in this study and signed written informed consent. The principles of the Declaration of Helsinki were followed. The ethics committees of the Guangxi People’s Hospital and the Third People’s Hospital of Nanning gave their approval for the trial’s conduct.
Data Collection
Demographic, anthropometric, laboratory biochemical indicators, and medical order data from hospitalization medical records were collected and anonymously analyzed. Only data, as baseline clinical characteristics, from the initial hospitalization were included for individuals in the analysis. The end-point events were the risk of rehospitalization and rehospitalization all-cause mortality. Information about end-point events was acquired through a review of hospitalization records and family fixed-line telephone interviews. All participants were continuously followed up every 4 weeks for 12 months.
Related Definitions
The relevant definitions in this study were as follows: (1) the end-point events referred to rehospitalization due to inflammatory fever, chills, and body aches, and all-cause mortality during the readmission period acquired through a review of hospitalization records, and family fixed-line telephone interviews; (2) RAR = red blood cell distribution width (%) ÷ albumin (g/L) was classified by low-level (≤0.36, n = 152), moderate-level (0.37–0.44, n = 152), and high-level (≥0.45, n = 151); (3) aged ≥18 defined as an adult; aged ≥65 defined as an elderly individual.
Statistical Analyses
The mean (±SD) was used to express variables with normal distributions, and the median (interquartile ranges) was used to express variables with non-normal distributions. Discontinuous variables were represented as frequencies. Normal distribution was tested using the Shapiro Wilk method. The normal distribution continuous variable group comparison was tested using analysis of variance. In contrast, a non-normal distribution was tested using Kruskal Wallis H. Categorical variables were compared between groups using the Chi-squared test. The univariate Cox regression analysis was initially used to identify the risk factors for the end-point events. Then, the factors with P < 0.1 in the univariate analysis were enrolled into the multivariate Cox regression analysis. We used tolerance and variance inflation factors to detect multicollinearity between variables. If the tolerance is less than 0.1 or the variance inflation factor is greater than 10, it indicates the existence of collinearity. This study’s tolerance was greater than 0.1, and the variance inflation factor was less than 10. So, there was no multicollinearity between variables. Three multivariate regression models were built and used to gradually adjust for potential confounding factors for the end-point events. Model I was adjusted for none. Model II was additionally adjusted for age and gender with Model I. Model III was further adjusted for diabetes mellitus, cardiovascular and cerebrovascular diseases, source of infection focus, duration of hospitalization, white blood cell count (WBC), total cholesterol (TC), triglycerides (TG), high-density lipoprotein (HDL), low-density lipoprotein (LDL), aspartate aminotransferase (AST), creatinine (Cr), and uric acid (UA) with Model II. Kaplan–Meier survival curve analysis and log rank test were used to evaluate the risk of rehospitalization and all-cause mortality during the readmission period in adults with sepsis who survived the first-episode severe sepsis. Sample size and power analysis were calculated using PASS 11.0 software (https://www.ncss.com/download/pass/updates/pass11/) to ensure that the number of cases met a high testing power of over 90%. Forest plots in subgroup analyses were performed with the R language software package version 4.2.2 (R Foundation for Statistical Computing, Vienna, Austria). Data analyses were performed using GraphPad Prism 9.3 (GraphPad Software, San Diego, CA) and the SPSS 26.0 statistical software package (IBM Corp., Armonk, NY, USA). Statistical significance was set at P < 0.05.
Results
Baseline Characteristics
The screening strategy for participants is shown in Figure 1. Finally, a total of 455 adult patients who survived the first-episode sepsis without recurrence for at least 3 months were enrolled in this study. The average age was 67, with 240 males (52.7%). The baseline characteristics are shown in Table 1. Of which, 152 individuals (33.41%) had a low-level RAR (≤0.36), 152 (33.41%) had a moderate-level RAR (0.37–0.44), and 151 (33.18%) had a high-level RAR (≥0.45). Among the three groups, age, history of diabetes, history of cardiovascular and cerebrovascular diseases, source of infection, rehospitalization, rehospitalization mortality, duration of first hospitalization, WBC, neutrophil percentage, TC, TG, HDL, LDL, ALB, AST, Cr, RDW, RAR were statistically significant (all P < 0.05). At the same time, gender, there were no statistically significant differences (P > 0.05) in hypertension, PLT, ALT, and UA. Additionally, infection is the leading cause of sepsis, while pneumonia is the main cause of infection in older age patients. Thus, the older age of the participants (age range from 50 to 80 years) in this study may also be one of the essential reasons why the respiratory system is the largest infection source in sepsis.
 |
Table 1 Baseline Clinical Characteristics of Subjects |
ROC Analysis for the RAR Optimal Cut-off Value Predicting the End-Point Events
To provide proper guidance information for routine clinical practice, ROC analyses were conducted to evaluate the predictive value of RAR for rehospitalization and rehospitalization mortality end-point events in sepsis. As shown in Figure 2, the RAR presents a predictive value for rehospitalization, with ROC curve areas of 0.673, an optimal cut-off value of 0.4251, a sensitivity of 58.3%, and a specificity of 71.2%, respectively. Similarly, Figure 3 indicates that the RAR is a valuable indicator in rehospitalization mortality, with ROC curve areas of 0.790, an ideal cut-off value of 0.4743, a sensitivity of 70.5%, and a specificity of 80.3%, respectively. The above results showed that the RAR was a valuable predictive biomarker for the risk of rehospitalization and rehospitalization mortality in patients with sepsis.
Cox Proportional Hazard Models for End-Point Events Risk
The risk of rehospitalization and rehospitalization mortality end-point events in subjects are displayed in Table 2. A univariate Cox regression analysis was conducted to identify the factors for the end-point events (see Supplementary Material 1). Next, variables with P < 0.1 in univariate Cox regression analysis were included in multivariate Cox regression. In model I (unadjusted), RAR was positively and independently correlated with the rehospitalization end-point event (HR = 1.836, 95% CI = 1.497–2.253, P for trend <0.001). Model II (Model I with adjusted for age and gender) (HR = 1.619, 95% CI = 1.306–2.006, P for trend <0.001) and model III (Model II with adjusted for diabetes mellitus, cardiovascular and cerebrovascular diseases, source of infection focus, duration of hospitalization, WBC, TC, TG, HDL, LDL, AST, Cr, and UA) (HR = 1.372, 95% CI = 1.076–1.749, P for trend = 0.011) also demonstrated a positive correlation between the RAR and rehospitalization risk, respectively. Similarly, the risk for all-cause mortality during the readmission period was positively associated with the RAR as well in model I (HR = 3.572, 95% CI = 2.165–5.893, P for trend <0.001), model II (HR = 2.83, 95% CI = 1.69–4.737, P for trend <0.001), and model III (HR = 2.246, 95% CI = 1.267–3.982, P for trend = 0.006), respectively. Compared with the low-level group, the high-level RAR group presented a higher dose-dependent rehospitalization incidence (HR = 1.816, 95% CI = 1.099–2.998, P = 0.02) and rehospitalization all-cause mortality (HR = 3.933, 95% CI = 1.038–14.901, P = 0.044), respectively. Multivariate Cox regression analyses indicated that the higher RAR level, the higher the risk for rehospitalization and rehospitalization all-cause mortality. Additionally, in Table 2, compared with low-level RAR, the moderate-level RAR P > 0.05 in Model II and Model III indicated insufficient predictive ability of the moderate-level RAR for endpoint events. Furthermore, as the RAR level increases, regardless of Model I, Model II, and Model III, the trend P-value < 0.05 displayed that the higher the RAR level, the greater predictive ability for endpoint events. Therefore, RAR is a valuable predictor for rehospitalization and hospitalization all-cause mortality.
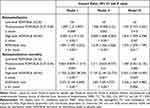 |
Table 2 Multivariate Cox Proportional Hazard Models for End-Point Events in Subjects |
Stratified Analyses in Subgroups
The results of the stratified analyses for rehospitalization events are shown in the forest plots (Figure 4). The stratified analysis displayed that compared to the low-level group, with the RAR increasing by 1.0, the risk for rehospitalization events increased 3.602-fold in aged <65 patients (HR = 4.602, 95% CI = 1.744–12.147, P = 0.002) and 1.721-fold in female patients (HR = 2.721, 95% CI = 1.223–6.052, P = 0.014), respectively. Therefore, stratified analyses state clearly that elevated RAR is closely associated with the risk of rehospitalization in young and middle-aged women patients with sepsis. Additionally, the results of the stratified analyses for rehospitalization all-cause mortality are presented in Supplementary Material 2. During the 12 months follow-up time, only one person died in the low-level RAR group, 8 in the moderate-level group, and 32 in the high-level group, which result in a significant difference among groups. Considering this, it is necessary extending the follow-up period such as from current one year to two years or even longer. Anyway, the trend of increasing rehospitalization all-cause mortality with increasing RAR levels is evident.
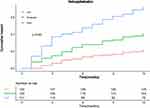
Kaplan–Meier Survival Analysis for the Cumulative Incidence of End-Point Events
The evaluation of the end-point events in the three groups is shown in Figure 5. Out of 455 participants, 156 patients experienced rehospitalization events (34.3%), of which 44 (28.2%) died over the readmission period. There was a dose–response relationship between the levels of RAR and the incidence rates of rehospitalization (19.1%, 32.9%, and 51.0% for low-level RAR, moderate-level RAR, and high-level RAR, respectively, all P for trend <0.01) and rehospitalization all-cause mortality (2.0%, 5.9%, and 21.2% for low-level RAR, moderate-level RAR, and high-level RAR, respectively, all P for trend <0.01). Kaplan–Meier survival curve analysis showed a significant positive association between the RAR levels and the incidence rates of rehospitalization (Figure 6) and rehospitalization all-cause mortality (Figure 7), respectively (log-rank, all P < 0.001). Kaplan–Meier analysis suggested that rehospitalization and rehospitalization all-cause mortality end-point events were more likely to occur in sepsis patients with a high-level RAR.
Discussion
Given the abuse of antibiotics in clinical practice, refractory bacterial infections are common, whether in internal medicine or surgical wards, which is one of the causes of sepsis in clinical practice. Sepsis, characterized mainly by shock, is the most severe state of bacterial and viral infections. Quickly and accurately identifying sepsis and taking effective therapeutic strategies is a challenging long-term task for clinical physicians. Previous studies have mainly focused on the prognosis of sepsis patients with short-term or long-term mortality, and few studies have explored the risk for rehospitalization and all-cause mortality outcomes during the readmission period after the first clinical recovery from sepsis. The present analysis aims to explore the relationship between RAR level and the risk for rehospitalization and rehospitalization all-cause mortality in middle-aged and elderly individuals with sepsis who survived the first-episode sepsis based on an ambispective longitudinal clinical cohort from ICU for the first time.
The current study showed that after adjusting covariate confounding factors for age, gender, diabetes mellitus, cardiovascular and cerebrovascular diseases, source of infection focus, duration of hospitalization, WBC, TC, TG, HDL, LDL, AST, Cr, and UA, RAR was positively and independently correlated with the risk for rehospitalization and rehospitalization all-cause mortality, respectively. Moreover, the correlation between the levels of RAR and endpoint events was presented as a dose-dependent feature. The stratified analysis displayed that compared to the low-level group, with the RAR increasing by 1.0, the risk for rehospitalization events increased 3.602-fold in aged <65 patients (HR = 4.602, 95% CI = 1.744–12.147, P = 0.002) and 1.721-fold in female patients (HR = 2.721, 95% CI = 1.223–6.052, P = 0.014), respectively. Kaplan–Meier survival analysis revealed that rehospitalization and all-cause mortality adverse events were more likely to occur in sepsis patients with a high-level RAR (log-rank, all P < 0.001). It should be noted that the age range of patients included in the final data analysis in this study was 50–80 years old. Compared to other populations, middle-aged and elderly patients may be more susceptible to infections, such as pneumonia, digestive system infection, and urinary system infection, which may be one of the leading causes of end-point events.
To date, the impact of gender and age on severe infections remains still highly controversial. Animal experimental data shows that female animals have a natural survival advantage,28,29 which contradicts human clinical data. A body of clinical evidence shows that the mortality in female patients with sepsis is higher than that in males.30–33 Interestingly, one of the reasons for the higher hospital mortality in single female patients with sepsis may be related to their marital status, which involves the ability to bear more considerable medical expenses.34 This is similar to the conclusion of the current study, which suggests that female sepsis patients have a more pronounced adverse clinical prognosis. Christophe Adrie et al reported the survival advantages in women over 50 years old with severe sepsis.35 This is partially similar to our finding that women aged <65 have a higher risk of poor prognosis.
Estrogenic hormones possess dual immunostimulatory and immunosuppressive characteristics, which may be related to the recurrence and progression of sepsis.36 As young and middle-aged female patients with sepsis who survive the first-episode severe sepsis enter the recovery phase, the estrogen immunosuppressive property is not conducive to the rapid correction from the immunosuppressive status, which may be the leading cause of sepsis recurrence. Additionally, in the rehospitalization stage, as the inflammation progresses rapidly, the estrogen immunostimulatory characteristic plays a crucial role in extensive immune damage (inflammatory storm), which may be one of the leading causes of increased hospitalization mortality in young and middle-aged female patients with sepsis.
Elevated RDW is associated with increased hematopoietic tissue activity.37 Sepsis can affect bone marrow function and iron metabolism and inhibit erythropoietin production and erythrocyte maturation related to an elevated proportion of immature red blood cells (elevated RDW) in blood, which leads to larger reticulocytes entering the circulation.38 In addition, cytokines can also affect red blood cell membrane glycoproteins and ion channels, leading to morphological changes in red blood cells.39 This series of physiological and pathological changes may lead to changes in red blood cell volume, increasing the RDW and damaging red blood cells’ deformability. Albumin, a sensitive and effective indicator of nutritional status, organ function, and physical activity in human plasma, can maintain normal osmotic pressure. The albumin level also affects the occurrence and prognosis of sepsis.40,41 RAR is a novel predictive indicator formulated by RDW/ALB in severe pneumonia (28-day mortality odds ratio: 1.338, 95% CI: 1.094–1.637, P = 0.005),25 diabetes foot ulcers (cut-off value of 0.3809),26 and tumor (overall mortality HR: 1.48, 95% CI: 1.06–2.07, P = 0.021),42 which can reflect not only the hematopoietic function but also the nutritional status of patients. In fact, these diseases are closely related to sepsis.43 Patients with bacterial infection often have hematopoietic dysfunction, especially in sepsis. Inflammatory cytokines can reduce iron utilization rate and promote red blood cell apoptosis, which leads to developing sepsis-related anemia and hypoproteinemia.44,45 Studies have shown that albumin has anti-inflammatory, nutritional, and hemorheological properties, which can inhibit platelet activation and aggregation.46 Sepsis patients with lower serum albumin levels are more prone to poor clinical prognosis.47 A prospective cohort study has shown that albumin levels are an essential predictor of 28-day mortality in sepsis, with a cut-off value of 29.2g/L, indicating good sensitivity and specificity.48 It may be related to the inflammatory response affecting vascular endothelial function, causing an increase in capillary permeability and albumin leakage to the outside of the blood vessels.49
Up to now, only one study on the relationship between RAR and sepsis prognosis mainly focuses on a short time (28-day) and a long time (90-day) mortality based on the Medical Information Mart for Intensive Care MIMIC-IV database in patients with first hospitalization.50 However, studies on the association between RAR and the risk of a second infection with sepsis and rehospitalization all-cause mortality in surviving adult individuals with sepsis remain absent. Recently, a large retrospective research conducted by the Ning Ding team based on the MIMIC-IV database in Beth Israel Deaconess Medical Center of Boston showed that RDW correlated with in-hospital mortality in septic shock. It might be a helpful predictor for septic shock patients’ clinical outcomes.51 Similarly, albumin level was associated with sepsis’s short- and long-term outcomes. Albumin supplementation might benefit septic patients with serum albumin <2.6 g/dL.52 Additionally, based on the same MIMIC-IV database, the Yang Xu team reported that in sepsis patients, the RAR was found to be independently correlated with the risk of acute kidney injury (AKI).27 Compared with the general population, patients with anemia and malnutrition are more prone to bacterial or viral infections due to weakened immune function and fragile immune homeostasis. They may even progress to sepsis, leading to severe adverse clinical outcomes such as recurrence of sepsis, second infection sepsis, and all-cause death. From this perspective, it is theoretically reasonable that RAR, characterized by two related nutritional status indicators, red blood cells, and albumin, has predictive value for sepsis. The results of the present study indicate that the higher the RAR level of sepsis patients, the significantly higher the likelihood of rehospitalization and rehospitalization all-cause mortality. Therefore, evaluating the nutritional status and hematopoietic function in patients with sepsis during hospitalization is crucial. Our study suggests that clinical physicians should pay more attention to the nutritional status and timely take necessary nutritional support strategies in patients with sepsis during the hospitalization period, in addition to active anti-infections.
Limitations
The main advantage of this study is the convenience and affordability of RAR indicators, which are suitable for different clinical stages and even grassroots hospitals in underdeveloped regions. However, there are still some limitations to consider. First, the nature of limitations in single-center retrospective studies determines the possibility of selection and sampling bias. Second, the sample size is limited, and the follow-up time may not be adequate. Third, this study solely evaluated baseline RAR values and ignored their variations over time. Fourth, the sensitivity and specificity of the cut-off values of RAR are not adequate. We think low sensitivity is caused by false-negative patients, which results from inadequate follow-up time. Future research needs to improve sensitivity by extending the follow-up period, such as from current one year to two years or even longer. However, the low specificity might be attributed to the false positive patients. Future research can improve the specificity by raising the enrollment time point in the inclusion criteria, for instance, elevating the time threshold from 3 to 6 months. Fifth, the age range of participants in this study is between 50 and 80 years old, and the conclusion may not be applicable to other age groups. Therefore, the conclusion of this study still needs to be confirmed by randomized, double-blind, multicenter, prospective longitudinal cohort studies; as we did before, the current ambispective longitudinal cohort study can continue to improve the conclusions of this study through long-term continuous follow-up.
Conclusion
In conclusion, RAR has a reliable predictive value for the risk of rehospitalization and rehospitalization all-cause mortality in patients with sepsis. Consequently, monitoring RAR levels for at least 1 year after surviving sepsis in female sepsis patients aged <65 in routine clinical practice is critical. Additionally, RAR, as a convenient and inexpensive biochemical indicator for predicting the prognosis of sepsis, can be carried out even in grassroots hospitals, which suggests that RAR has a potential promotion and application value in routine clinical practice.
Ethics Statement
All patients agreed to participate in this study and signed written informed consent. The principles of the Declaration of Helsinki were followed. The ethics committees of the Guangxi People’s Hospital and the Third People’s Hospital of Nanning approved the trial’s conduct.
Acknowledgments
We thank all participants for their contribution to the study. We thank the ICU and the Medical Record Department of the Third People’s Hospital of Nanning, and the Endocrine Metabolism Department of the Guangxi People’s Hospital for cooperating as partners.
Funding
The study was funded by the National Natural Science Foundation of China (82160052, 81560044, 30860113).
Disclosure
The authors report no conflicts of interest in this study.
References
1. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3. JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
2. Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395(10219):200–211. doi:10.1016/S0140-6736(19)32989-7
3. Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554. doi:10.1056/NEJMoa022139
4. Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi:10.1016/S0140-6736(20)30925-9
5. Liu Y-C, Yao Y, Yu -M-M. Frequency and mortality of sepsis and septic shock in China: a systematic review and meta-analysis. BMC Infect Dis. 2022;22(1):564. doi:10.1186/s12879-022-07543-8
6. Annane D, Bellissant E, Cavaillon JM. Septic shock. Lancet. 2005;365(9453):63–78. doi:10.1016/S0140-6736(04)17667-8
7. Fleischmann C, Scherag A, Adhikari NK, et al. International Forum of Acute Care Trialists. Assessment of global incidence and mortality of hospital-treated sepsis: current estimates and limitations. Am J Respir Crit Care Med. 2016;193(3):259–272. doi:10.1164/rccm.201504-0781OC
8. Vincent J-L, Marshall JC, Namendys-Silva SA, et al. ICON Investigators. Assessment of the worldwide burden of critical illness: the Intensive Care Over Nations (ICON) audit. Lancet Respir Med. 2014;2(5):380–386. doi:10.1016/S2213-2600(14)70061-X
9. Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369(9):840–851. doi:10.1056/NEJMra1208623
10. Delano MJ, Ward PA. The immune system’s role in sepsis progression, resolution and long-term outcome. Immunol Rev. 2016;274(1):330–353. doi:10.1111/imr.12499
11. Liu D, Huang S-Y, Sun J-H. Sepsis-induced immunosuppression: mechanisms, diagnosis and current treatment options. Military Med Res. 2022;9(1):56. doi:10.1186/s40779-022-00422-y
12. Boomer JS, To K, Chang KC, et al. Immunosuppression in patients who die of sepsis and multiple organ failure. JAMA. 2011;306(23):2594–2605. doi:10.1001/jama.2011.1829
13. Hotchkiss RS, Monneret G, Payen D. Sepsis-induced immunosuppression: from cellular dysfunctions to immunotherapy. Nat Rev Immunol. 2013;13(12):862–874. doi:10.1038/nri3552
14. Shen H-N, Lu C-L, Yang -H-H. Risk of recurrence after surviving severe sepsis: a matched cohort study. Crit Care Med. 2016;44(10):1833–1841. doi:10.1097/CCM.0000000000001824
15. Anderson HL, Brodsky IE, Mangalmurti NS. The evolving erythrocyte: red blood cells as modulators of innate immunity. J Immunol. 2018;201(5):1343–1351. doi:10.4049/jimmunol.1800565
16. Darbonne WC, Rice GC, Mohler MA, et al. Red blood cells are a sink for interleukin 8, a leukocyte chemotaxin. J Clin Invest. 1991;88(4):1362–1369. doi:10.1172/JCI115442
17. Lee JM, Suh JS, Kim YK. Red blood cell deformability and distribution width in patients with hematologic neoplasms. Clin Lab. 2022;68(10). doi:10.7754/Clin.Lab.2022.211260
18. Patel KV, Mohanty JG, Kanapuru B, Hesdorffer C, Ershler WB, Rifkind JM. Association of the red cell distribution width with red blood cell deformability. Adv Exp Med Biol. 2013;765:211–216. doi:10.1007/978-1-4614-4989-8_29
19. Piagnerelli M, Zouaoui Boudjeltia K, Vanhaeverbeek M, et al. Red blood cell rheology in sepsis. Intensive Care Med. 2003;29(7):1052–1061. doi:10.1007/s00134-003-1783-2
20. Wu H, Liao B, Cao T, Ji T, Huang J, Ma K. Diagnostic value of RDW for the prediction of mortality in adult sepsis patients: a systematic review and meta-analysis. Front Immunol. 2022;17(13):997853. doi:10.3389/fimmu.2022.997853
21. Dankl D, Rezar R, Mamandipoor B. Red cell distribution width is independently associated with mortality in sepsis. Med Princ Pract. 2022;31(2):187–194. doi:10.1159/000522261
22. Tonelli M, Sacks F, Arnold M, Moye L, Davis B, Pfeffer M. Relation between red blood cell distribution width and cardiovascular event rate in people with coronary disease. Circulation. 2008;117(2):163–168. doi:10.1161/CIRCULATIONAHA.107.727545
23. Pascual‐Figal DA, Bonaque JC, Redondo B. Red blood cell distribution width predicts long-term outcome regardless of anaemia status in acute heart failure patients. Eur J Heart Fail. 2009;11(9):840–846. doi:10.1093/eurjhf/hfp109
24. Ani C, Ovbiagele B. Elevated red blood cell distribution width predicts mortality in persons with known stroke. J Neurol Sci. 2009;277(1–2):103–108. doi:10.1016/j.jns.2008.10.024
25. Jeong JH, Heo M, Lee SJ, Jeong YY, Lee JD, Yoo J-W. Clinical usefulness of red cell distribution width/albumin ratio to discriminate 28-day mortality in critically ill patients with pneumonia receiving invasive mechanical ventilation, compared with lactate/albumin ratio: a retrospective cohort study. Diagnostics. 2021;11(12):2344. doi:10.3390/diagnostics11122344
26. Hong J, Hu X, Liu W. Impact of red cell distribution width and red cell distribution width/albumin ratio on all-cause mortality in patients with type 2 diabetes and foot ulcers: a retrospective cohort study. Cardiovasc Diabetol. 2022;21(1):91. doi:10.1186/s12933-022-01534-4
27. Xu Y, Qi W. Association between red cell distribution width to albumin ratio and acute kidney injury in patients with sepsis: a MIMIC population-based study. Int Urol Nephrol. 2023;55(11):2943–2950. doi:10.1007/s11255-023-03572-7
28. Zellweger R, Wichmann MW, Ayala A, et al. Females in proestrus state maintain splenic immune functions and tolerate sepsis better than males. Crit Care Med. 1997;25(1):106–110. doi:10.1097/00003246-199701000-00021
29. Koch MA. Sex Bias in Sepsis. Cell Host Microbe. 2018;24(5):613–615. doi:10.1016/j.chom.2018.10.014
30. Nachtigall I, Tafelski S, Rothbart A. Gender-related outcome difference is related to course of sepsis on mixed ICUs: a prospective, observational clinical study. Crit Care. 2011;15(3):R151. doi:10.1186/cc10277
31. Sunden-Cullberg J, Nilsson A, Inghammar M. Sex-based differences in ED management of critically ill patients with sepsis: a nationwide cohort study. Intensive Care Med. 2020;46(4):727–736. doi:10.1007/s00134-019-05910-9
32. Mercado-Martínez J, Rivera-Fernández R, Aguilar-Alonso E. APACHE-II score and Killip class for patients with acute myocardial infarction. Intensive Care Med. 2010;36(9):1579–1586. doi:10.1007/s00134-010-1832-6
33. Vincent J-L, Sakr Y, Sprung CL. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med. 2006;34(2):344–353. doi:10.1097/01.ccm.0000194725.48928.3a
34. Seymour CW, Iwashyna TJ, Cooke CR, Hough CL, Martin GS. Marital status and the epidemiology and outcomes of sepsis. Chest. 2010;137(6):1289–1296. doi:10.1378/chest.09-2661
35. Adrie C, Azoulay E, Francais A. Influence of gender on the outcome of severe sepsis: a reappraisal. Chest. 2007;132(6):1786–1793. doi:10.1378/chest.07-0420
36. Walker SE. Estrogen and autoimmune disease. Clin Rev Allergy Immunol. 2011;40(1):60–65. doi:10.1007/s12016-010-8199-x
37. van Koeverden ID, den Ruijter HM, Scholtes VPW. A single preoperative blood test predicts postoperative sepsis and pneumonia after coronary bypass or open aneurysm surgery. Eur J Clin Invest. 2019;49(3):e13055. doi:10.1111/eci.13055
38. Rogiers P, Zhang H, Leeman M, et al. Erythropoietin response is blunted in critically ill patients. Intensive Care Med. 1997;23(2):159–162. doi:10.1007/s001340050310
39. Piagnerelli M, Zouaoui Boudjeltia K, Brohee D. Alterations of red blood cell shape and sialic acid membrane content in septic patients. Crit Care Med. 2003;31(8):2156–2162. doi:10.1097/01.CCM.0000079608.00875.14
40. Caironi P, Tognoni G, Masson S. Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med. 2014;370(15):1412–1421. doi:10.1056/NEJMoa1305727
41. Tai H, Zhu Z, Mei H, Sun W, Zhang W. Albumin-to-fibrinogen ratio independently predicts 28-day mortality in patients with peritonitis-induced sepsis. Mediators Inflamm. 2020;6:7280708. doi:10.1155/2020/7280708
42. Sim J-H, Jang D-M, Cho H-S, Park JY, Choi W-J. Association of red cell distribution width/albumin ratio with intraoperative blood transfusion in cervical cancer patients. PLoS One. 2022;17(11):e0277481. doi:10.1371/journal.pone.0277481
43. Rhee C, Dantes R, Epstein L. Incidence and Trends of Sepsis in US Hospitals Using Clinical vs Claims Data, 2009–2014. JAMA. 2017;318(13):1241–1249. doi:10.1001/jama.2017.13836
44. Bateman R, Sharpe M, Singer M, Ellis C. The effect of sepsis on the erythrocyte. Int J Mol Sci. 2017;18(9):1932. doi:10.3390/ijms18091932
45. Ekregbesi P, Shankar-Hari M, Bottomley C, Riley EM, Mooney JP. Relationship between anaemia, haemolysis, inflammation and haem oxygenase-1 at admission with sepsis: a pilot study. Sci Rep. 2018;8(1):11198. doi:10.1038/s41598-018-29558-5
46. Gresele P, Deckmyn H, Huybrechts E, Vermylen J. Serum albumin enhances the impairment of platelet aggregation with thromboxane synthase inhibition by increasing the formation of prostaglandin D2. Biochem Pharmacol. 1984;33(13):2083–2088. doi:10.1016/0006-2952(84)90577-x
47. Li T, Li X, Liu X, et al. Association of procalcitonin to albumin ratio with the presence and severity of sepsis in neonates. J Inflamm Res. 2022;12(15):2313–2321. doi:10.2147/JIR.S358067
48. Yin M, Si L, Qin W. Predictive value of serum albumin level for the prognosis of severe sepsis without exogenous human albumin administration: a prospective cohort study. J Intensive Care Med. 2018;33(12):687–694. doi:10.1177/0885066616685300
49. Han T, Cheng T, Liao Y, et al. Analysis of the value of the blood urea nitrogen to albumin ratio as a predictor of mortality in patients with sepsis. J Inflamm Res. 2022;23(15):1227–1235. doi:10.2147/JIR.S356893
50. Xu W, Huo J, Chen G, et al. Association between red blood cell distribution width to albumin ratio and prognosis of patients with sepsis: a retrospective cohort study. Front Nutr. 2022;23(9):1019502. doi:10.3389/fnut.2022.1019502
51. Ding Q, Su Y, Li C, Ding N. Red cell distribution width and in-hospital mortality in septic shock: a public database research. Int J Lab Hematol. 2022;44(5):861–867. doi:10.1111/ijlh.13925
52. Cao Y, Su Y, Guo C, He L, Ding N. Albumin level is associated with short-term and long-term outcomes in sepsis patients admitted in the ICU: a large public database retrospective research. Clin Epidemiol. 2023;15:263–273. doi:10.2147/CLEP.S396247
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.