Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
The Rate of Postoperative Mortality and Renal and Respiratory Complications are Increased in Patients with Extreme Obesity Undergoing Cardiac Surgery – A Retrospective Observational Cohort Study of 8848 Patients
Authors Pacholewicz J , Kuligowska E, Szylińska A , Walerowicz P, Biskupski A, Sielicki P, Kotfis K , Listewnik M
Received 12 December 2022
Accepted for publication 10 April 2023
Published 24 April 2023 Volume 2023:16 Pages 1155—1166
DOI https://doi.org/10.2147/DMSO.S400597
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Gian Paolo Fadini
Jerzy Pacholewicz,1,* Ewelina Kuligowska,1,* Aleksandra Szylińska,2 Paweł Walerowicz,1 Andrzej Biskupski,1 Piotr Sielicki,1 Katarzyna Kotfis,3 Mariusz Listewnik1
1Department of Cardiac Surgery, Pomeranian Medical University, Szczecin, Poland; 2Department of Medical Rehabilitation and Clinical Physiotherapy, Pomeranian Medical University, Szczecin, Poland; 3Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University, Szczecin, Poland
*These authors contributed equally to this work
Correspondence: Katarzyna Kotfis, Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University, Szczecin, Poland, Email [email protected]
Introduction: The importance of obesity as a potential risk factor in open heart surgery is well known. The epidemic of extreme obesity is an increasing public health concern and raises alerts regarding postoperative complications and mortality in patients undergoing cardiac surgery. The study aimed to analyze the impact of extreme obesity (BMI≥ 40) on the frequency of postoperative complications, as well as early and delayed mortality compared to patients with a lower body mass.
Materials and Methodology: This retrospective observational cohort study involved patients, over the age of 18, undergoing cardiac surgery with cardiopulmonary bypass at the Cardiac Surgery Department of the Pomeranian Medical University in Szczecin, Poland between January 1st, 2010 and December 31st, 2018. The patients included in the study were allocated into two subgroups depending on the BMI index (Group I BMI≥ 40 vs Group II BMI< 40).
Results: A total of 8848 adult patients of both genders were included. Baseline characteristics for Group I and Group II were mean age 64.07± 7.76 vs 65.10± 9.68 years (p=0.123), mean BMI 42.13± 2.44 vs 28.55± 4.23 (p< 0.001), with more females in Group I (58.04% vs 29.06%) and more males in Group II (70.94% vs 29.06%), p< 0.001. The predicted perioperative risk using the EuroScore Logistics scale was higher in a group with BMI≥ 40 (p< 0.001). Regression analysis with adjustment for confounding factors showed a statistically significant relationship between BMI≥ 40 and postoperative respiratory failure (OR=1.760, p=0.043), acute kidney injury AKIN2 (OR=2.082, p=0.044) and AKIN3 (OR=2.743, p=0.039). 30-day mortality in the univariate analysis showed a statistically significant relationship, however, after modifying the results with interfering factors, no statistical significance was obtained.
Conclusion: The risk of postoperative acute respiratory failure and acute renal injury was increased in patients with BMI≥ 40. The probability of 30-day survival of patients after cardiac surgery was much lower in people with extreme obesity, although it was related to the dominant comorbidities. The 10-year survival was comparable in both groups.
Keywords: obesity, cardiac surgery, BMI, complications, mortality, outcome
Introduction
Obesity, defined as an excessive amount of adipose tissue, has been called the „Civilization Syndrome” and is an increasing public health concern that raises alerts regarding postoperative complications and mortality in patients undergoing cardiac surgery.1 The importance of obesity as a potential risk factor in open heart surgery is well known. Obesity is a chronic condition, without a tendency for self-treatment and a tendency for recurrence, moreover, it leads to the progression of many other severe diseases, including dyslipidemia, derangement of carbohydrate metabolism – including type 2 diabetes, hypertension, coronary artery disease, diastolic heart failure, atrial fibrillation, chronic renal disease, stroke, apnea, chronic obstructive pulmonary disease, podagra, lithiasis, and degenerative spine disease.1–5 It is not only the excessive aliment supply that influences the extremely positive energy balance that causes an increase in body weight, but also low fitness activity, stress, smoking, and alcohol intake that further increase the risk for patients.6
Moreover, severe obesity may be associated with the development of generalized clinical and subclinical atherosclerosis, visible as increased pericardial fat, remodeling of major arteries, aortic valve sclerosis (AVS), and mitral valve sclerosis (MVS).7 These disorders contribute to a shortening of the lifespan and are a cause of higher mortality for patients suffering from cardiovascular diseases.
There is no doubt that nutrition disorders have a crucial effect on the perioperative risk and outcome in cardiac surgery procedures. Every operation performed with the use of cardio-pulmonary bypass constitutes a challenge for the body and exposes the patient to multilevel pathophysiological derangement during the postoperative period.
The fast increase in extreme obesity rates, defined by a BMI ≥40, has severe repercussions, not just medical, but also economic and psychosocial, especially for industrialized countries.8 Many independent indicators define obesity and its levels in a comparable manner, with the most prevalent being the body mass index (BMI).9 The problem of increased perioperative risk due to nutrition disorders, determined by BMI or Quelet index, is accelerating.10 Yet, the most common cardiac surgery operation risk scale – EuroScore II – does not take the nutritional state of the patient or body habitus into consideration.11 On the other hand, a recently developed novel surgical site infection risk index used in cardiac surgery stressed the importance of either diabetes or obesity.12 Despite accumulating knowledge, the effects of extreme obesity on postoperative outcomes in cardiac surgery patients is still a matter of vivid discussion. This study aimed to analyze the differences in the postoperative course, as well as early and late mortality of patients with extreme obesity (BMI≥40), undergoing cardiac surgery with the use of cardiopulmonary bypass (CPB) as compared to patients with a lower weight (BMI<40).
Study Cohort and Methodology
This retrospective observational cohort study included 8848 consecutive patients of both genders, above the age of 18 years, undergoing cardiac surgery with the use of cardiopulmonary bypass at the Department of Cardiac Surgery of the Pomeranian Medical University in Szczecin, Poland, between the 1st of January 2010 and 31st of December 2018.
Data Collection
Demographical data and past medical history including concomitant diseases were obtained from the anamnesis and medical records. We evaluated the intensity of coronary artery disease symptoms using the 4-stage CCS scale (Canadian Cardiovascular Score). To evaluate the risk of operation the EuroScore Logistic 2 scale was used. Data relevant to the postoperative process involved the length of intubation time, duration of hospitalization, and length of treatment in the intensive care unit (ICU), as well as early (at 30 days) and delayed mortality. The frequency and distribution of postoperative complications was evaluated. Additionally, the postoperative condition of the patients was evaluated during postoperative in-patient and telephone follow-up visits. The BMI index for every patient was calculated using the height and weight measurements according to the standard formula; BMI = weight [kg]/height2 [m]. The standards recommended by the World Health Organization (WHO) were used to interpret the results, with normal weight defined as a BMI greater than or equal to 18.5 to 24.9 kg/m2, overweight –25 to 29.9 kg/ m2, obesity – a BMI greater than or equal to 30 kg/m2 and extreme obesity if the values of BMI were greater than or equal to 30 kg/m2.6
Study Group
The patients included in the study were allocated into two subgroups depending on the BMI index. The first subgroup included patients with BMI<40, while the second with BMI≥40. The division into two subgroups is presented in Figure 1.
 |
Figure 1 Study flowchart. Notes: Test log rank p=0.019. Blue line is BMI<40, Red Line is BMI≥40. |
Ethical Issues
The study was performed in accordance with the Declaration of Helsinki and Good Clinical Practice. It received a waiver from the Bioethical Committee of the Pomeranian Medical University due to its retrospective observational character (decision no. KB-0012/237/12/19). Before each operation, every patient must have signed an informed consent for the surgery, which included an agreement for data collection. All data analysis was performed with full patient anonymity.
Statistical Analysis
The data was analyzed using the licensed software Statistica 13 (StatSoft Inc., Tulsa, OK, USA). To evaluate the normality of the distribution of the studied variables the Shapiro–Wilk test was used. Numbers and percentages to present categorical variables and the Chi-square test to compare the groups were used; with Yates correction if the subgroup size was insufficient. The data are presented as means and standard deviations for continuous variables. Mann–Whitney U-test was used to compare the characteristics between patients in Group I (with BMI≥40) and Group II (BMI<40). Univariate and multivariate logistic regression analyses were performed. The multivariate logistic regression was corrected for potentially distorting data (gender, statistically significant preoperative data). The Kaplan–Meier analysis calculated the probability of survival in the study group. Statistical significance was determined as a p-value below 0.05.
Results
The demographical data and data from the anamnesis are presented in Table 1. The baseline characteristics for Group I and Group II were mean age 64.07±7.76 vs 65.10±9.68 years (p=0.123), mean BMI 42.13±2.44 vs 28.55±4.23 (p<0.001), with more females in Group I (58.04% vs 29.06%) and more males in Group II (70.94% vs 29.06%), p<0.001. The predicted perioperative risk using the EuroScore Logistics scale was higher in group with BMI≥40 (p<0.001). When considering comorbidities, statistically significant differences between both groups in were noticed, especially regarding the prevalence of diabetes (p<0.001), hypertension (p=0.006), gout (p=0.011), diseases of the biliary ducts (p=0.003), chronic obstructive pulmonary diseases (COPD) (p=0.003), unstable angina (p=0.049) which were more prevalent in Group I. When analyzing the laboratory tests, significant differences regarding the value of C-reactive protein (CRP) (p=0.017) and glycated hemoglobin (p<0.001) were demonstrated.
 |
Table 1 Characteristic of Demographical Data and Medical Data Before Operation |
The intraoperative data did not differ significantly between both groups. The only difference was related to the number of grafts BIMA (p=0.032) and the postoperative kidney function. In the group with BMI≥40, we observed a higher level of serum creatinine (p=0.021) and glomerular filtration rate (GFR) (p=0.002). The detailed data are presented in Table 2.
 |
Table 2 Characteristic of Intra- and Postoperative Data |
In addition, a further analysis using univariate regressions, with the separation the study cohort into three groups according to the BMI (normal weight, overweight, obesity) was performed, with the results presented in Table 3. Overweight patients were much more likely to suffer from paroxysmal atrial fibrillation (FAP) with positive anamnesis (OR=1.554), p=0.016), needed postoperative hemofiltration (OR=1.410, p<0.001), or were diagnosed with pneumonia (OR=1.310, p<0.001), postoperative respiratory failure (OR=1.555, p<0.001). The 30-day mortality (OR=1.757, p<0.001), mortality at the equal time of observation (114 days) (OR=1.730, p<0.001), 5-year mortality (OR=1.579, p<0.001), 10-year mortality (OR=1.468, p=0.010) for overweight patients was higher. Patients with obesity (BMI≥30 kg/m2) suffered from FAP (OR=1.241, p=0.005), had FAP in anamnesis (OR=1.627, p=0.009), acute kidney injury staged as AKIN I (OR=1.174, p=0.043) or required postoperative hemofiltration (OR=1.321, p=0.011). The 30-day mortality (OR=1.786, p<0.001), mortality at the equal time of observation (114 days) (OR=1.538, p<0.001) and 5-year mortality (OR=1.422, p<0.001) were higher for obese patients.
 |
Table 3 Univariate Logistic Regression of Postoperative Complication Depending on Index BMI (Normal, Overweight, Obese) |
Univariate and multivariate logistic regression analyses were performed, with the presented in Table 4. After adjusting the results for confounding factors, a statistically significant relationship was found between BMI≥40 and postoperative respiratory failure (OR=1.760, p=0.043), acute kidney injury staged as AKIN2 (OR=2.082, p=0.044) or AKIN3 (OR=2.743, p=0.039). In the univariate analysis, the 30-day mortality showed a statistically significant relationship, however, after modifying the results with interfering factors, no statistical significance was obtained.
 |
Table 4 Logistic Regression of Postoperative Complication Depending on BMI≥40 |
The Kaplan–Meier curve is presented in Figure 2 and shows that the probability of survival after surgery at day 30 was significantly lower in Group I for patients with BMI≥40 (p=0.019).
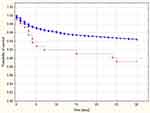 |
Figure 2 Kaplan–Meier curve illustrating the probability of patients’ survival depending on BMI. |
Discussion
In this study, we demonstrated that the group of patients with extreme obesity, expressed by a BMI factor ≥40, showed a higher incidence of postoperative acute kidney injury and the development of respiratory failure. The probability of survival after surgery at day 30 was significantly lower in patients with BMI≥40 although it is related to the dominant comorbidities.
Our results demonstrates the statistical saliency of extreme obesity and a higher risk of acute renal insufficiency. Previous research regarding this association has shown a correlation between acute renal failure and extreme obesity.13–16 It is necessary to mention that obesity, by itself, has a negative effect on renal function due to fluid retention, which predisposes to a state of chronic and acute renal insufficiency.17,18 Serra et al observed that excess adipose tissue correlated with the insulin resistance mechanism. This mechanism leads to, through hormones and cytokines, incorrect activation of the renin-angiotensin-aldosterone axis, which in turn increases the oxidative stress in the kidneys and contributes to the development of renal insufficiency.19
Furthermore, acute renal insufficiency after cardiac surgery develops in a mechanism of inbalanced chronic insufficiency, which is intensified by hypertension and diabetes combined with obesity.20,21 Acute kidney injury may also be associated with the status of microvascular circulation which is frequently compromised in obese patients. Cardiac surgery with the use of cardiopulmonary bypass and non-pulsatile blood flow generated by CPB may lead to impairment of microcirculatory perfusion with a risk of multiple organ dysfunction, including renal insufficiency. A recent study has shown that three days after surgery, microcirculatory perfusion was equally disturbed during cardiac surgery with CPB in metabolically healthy obese patients as compared to non-obese patients.22
Another important group of postoperative complications are those associated with the respiratory system. In this study, we ascertained the significant influence of extreme obesity on the increased incidence of postoperative respiratory failure, whereas we cannot confirm a significant effect of obesity on the development of postoperative pneumonia. Most authors confirm the influence of obesity, especially extreme, on an increased occurrence of postoperative respiratory failure in cardiac surgery.1,14,16,23 The impairment of respiratory function can be caused by a tendency for accumulation of anesthetic drugs in the adipose tissue and delayed release into the bloodstream.14 This theory seems to confirm the fact that the time of mechanical ventilation is shorter when using anesthesia drugs with a shorter terminal half-life. This fact may have an impact on the development of postoperative respiratory failure.24
Furthermore, obesity changes the physiology of the respiratory system as patients with extreme obesity have lower lung volume. This fact contributes to an increased incidence of Pickwick syndrome which causes hypoxia.25 It is important to mention that obesity-conceived conditions increase pulmonary resistance and decrease pulmonary volume.26
Ditillo and co-authors proved that the most severe respiratory system complications are related to extreme obesity.27 The increasing number of cases of acute respiratory failure in the group of patients with extreme obesity causes longer hospitalization duration and generates additional costs.28 Patients with extreme obesity have a lower adaptive potential of the respiratory system because of the adverse relationship between perfusion and ventilation.13 Moreover, extreme obesity causes a decrease in vital capacity, residual volume, and total lung capacity, which result in profoundly dysfunctional ventilation.29 Patients with extreme obesity are also usually less physically active, which causes a decline in lung efficiency. Furthermore, only a few researchers distinguish a classification of respiratory system compilation to respiratory failure and pneumonia. Yazdanian and co-authors did not prove any statistically significant differences between the incidence of pneumonia and extreme obesity.23
Our study showed a higher risk of 30-day mortality in the group of patients with BMI≥40. Borracci and co-authors also proved that extreme obesity in the group of patients undergoing cardiac surgery constitutes a risk factor for 30-day mortality. It is necessary to mention that Boracci’s research group of people with extreme obesity consisted of only 21 patients, which could be insufficient to prove an objective relationship.30
According to the Scientific Statement from the American Heart Association about obesity and cardiovascular diseases, obesity leads to the development of cardiovascular diseases and mortality due to cardiovascular diseases. The main management of obesity is changing the lifestyle by increasing physical activity and through diet modifications, as well as pharmacological interventions. In preventing the development of metabolic syndrome it is important to reduce body weight and limit the progression of obesity to a BMI over 40.31
Study Strengths and Limitations
A major and unquestionable strength of this analysis, making this study unique, is a very large cohort of patients included in the analysis and a long observation period. Yet, certain limitations of this study also need to be mentioned. It is single-center research, so extending the observation into a multicenter study would be useful. Although the number of patients included in the analysis was very high, the nature of the analysis was retrospective, therefore some data may not be retrievable.
Conclusions
The risk of postoperative acute respiratory failure and acute kidney injury was increased in patients with BMI≥40. The probability of 30-day survival of patients after cardiac surgery was much lower in patients with extreme obesity, although it was related to the dominant comorbidities. The 10-year survival was comparable in both groups.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Bioethical Committee of the Pomeranian Medical University (decision no. KB-0012/237/12/19).
Informed Consent Statement
Due to the retrospective nature of the study, informed consent was not required.
Funding
This research received no external funding.
Disclosure
The authors declare no conflict of interest.
References
1. Bell T, Stokes S, Jenkins PC, Hatcher L, Fecher AM. Prevalence of cardiovascular and respiratory complications following trauma in patients with obesity. Heart Lung. 2018;46:347–350.
2. Straznicky N, Grima M, Sari C, et al. The relation of glucose metabolism to left ventricular mass and function and sympathetic nervous system activity in obese subjects with metabolic syndrome. J Clin Endocrinol Metab. 2013;98:227–237.
3. Che L, Xu L, Wang MY, Huang YG. Obesity paradox among elderly patients with coronary artery disease undergoing non-cardiac surgery. J Geriatr Cardiol. 2018;15(9):598–604.
4. Sansone V, Applefield RC, De Luca P, et al. Does a high-fat diet affect the development and progression of osteoarthritis in mice?: a systematic review. Bone Joint Res. 2020;8(12):582–592.
5. Björntorp P. Visceral obesity: a “civilization syndrome”. Obes Res. 1993;1:206–222. doi:10.1002/j.1550-8528.1993.tb00614.x
6. Weir CB, Jan A. BMI Classification Percentile and Cut off Points. Treasure Island. FL: StatPearls, StatPearls Publishing; 2020.
7. Kovac N, Grymyr LMD, Gerdts E, et al. Markers of Subclinical Atherosclerosis in Severe Obesity and One Year after Bariatric Surgery. J Clin Med. 2022;11:2237. doi:10.3390/jcm11082237
8. Szymocha M, Bryła M, Maniecka-Bryła I. Epidemia otyłości w XXI wieku. Zdr Publ. 2009;1192:207–212.
9. WHO Export Committee. Physical Status: The Use and Interpretation of Antropometry; Report of WHO Expert Committee. WHO Technical Report Series. 312-340. Geneva: World Health Organization;1995.
10. Brown CVR, Velmahos GC. The consequences of obesity on trauma, emergency surgery, and surgical critical care. World J Emerg Surg. 2006;1:27.
11. Nashef SA, Roques F, Sharples LD, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41:734–744.
12. Bustamante-Munguira J, Herrera-Gómez F, Ruiz-álvarez M, Hernández-Aceituno A, Figuerola-Tejerina A, New Surgical A. Site Infection Risk Score: infection Risk Index in Cardiac Surgery. J Clin Med. 2019;8:480. doi:10.3390/jcm8040480
13. Wigfield CH, Lindsey JD, Muñoz A, Chopra PS, Edwards NM, Love RB. Is extreme obesity a risk factor for cardiac surgery? An analysis of patients with a BMI > or = 40. Eur J Cardiothorac Surg. 2006;29:434–440. doi:10.1016/j.ejcts.2006.01.016
14. Ghanta RK, LaPar D, Zhang Q, et al. Obesity Increases Risk‐Adjusted Morbidity, Mortality, and Cost Following Cardiac Surgery. J Am Heart Assoc. 2017;6:e003831. doi:10.1161/JAHA.116.003831
15. Aguiar C, MacLeod J, Yip A, et al. Impact of Obesity on Postoperative Outcomes following cardiac Surgery (The OPOS study): rationale and design of an investigator-initiated prospective study. BMJ Open. 2019;9:e023418. doi:10.1136/bmjopen-2018-023418
16. Gao M, Sun J, Young N, et al. Impact of Body Mass Index on Outcomes in Cardiac Surgery. J Cardiothorac Vasc Anesth. 2016;30:1308–1316. doi:10.1053/j.jvca.2016.03.002
17. Kambham N, Markowitz GS, Valeri AM, et al. Obesity-related glomerulopathy: an emerging epidemic. Kidney Int. 2001;59:1498–1509.
18. Hsu CY, McCulloch CE, Iribarren C, et al. Body mass index and risk for end-stage renal disease. Ann Intern Med. 2006;144:21–28.
19. Serra A, Romero R, Lopez D, et al. Renal injury in the extremely obese patients with normal renal function. Kidney Int. 2008;73:947–955.
20. Billings FTT, Pretorius M, Schildcrout JS, et al. Obesity and oxidative stress predict AKI after cardiac surgery. J Am Soc Nephrol. 2012;23:1221–1228.
21. Hertzberg D, Sartipy U, Holzmann MJ. Type 1 and type 2 diabetes mellitus and risk of acute kidney injury after coronary artery bypass grafting. Am Heart J. 2015;170:895–902.
22. Boly CA, Venhuizen M, Dekker NAM, Vonk ABA, Boer C, Brom CE. Comparison of Microcirculatory Perfusion in Obese and Non-Obese Patients Undergoing Cardiac Surgery with Cardiopulmonary Bypass. J Clin Med. 2021;10:469. doi:10.3390/jcm10030469
23. Yazdanian F, Faritous SZ, Mollasadeghi G, Farasatkish R, Ghaffari Nejad MH, Khamoushi AJ. Impact of Body Mass Index on In-Hospital Mortality and Morbidity after Coronary Artery Bypass Grafting Surgery. J Tehran Heart Cent. 2008;3:25–30.
24. Krdzalic A, Kosjerina A, Jahic E, Rifatbegovic Z, Krdzalic G. Influence of remifentanil/propofol anesthesia on ventilator-associated pneumonia occurrence after major cardiac surgery. Med Arch. 2013;67:407–409.
25. Liu T, Chen JJ, Bai XJ, Zheng GS, Gao W. The effect of obesity on outcomes in trauma patients: a meta-analysis. Injury. 2013;44:1145–1152.
26. Varon J, Marik P. Management of the obese critically ill patient. Crit Care Clin. 2001;17:187–200.
27. Ditillo M, Pandit V, Rhee P, et al. Morbid obesity predisposes trauma patients to worse outcomes: a National Trauma Data Bank analysis. J Trauma Acute Care Surg. 2014;761:176–179.
28. Rose DK, Cohen MM, Wigglesworth DF, et al. Critical respiratory events in the postanesthesia care unit: patient, surgical and anesthetic factors. Anesthesiology. 1994;81:410–418.
29. Ray CS, Sue DY, Bray G, Hansen JE, Wasserman K. Effects of obesity on respiratory function. Am Rev Respir Dis. 1983;128:501–506.
30. Borracci R, Ingino C, Miranda JM. Association of body mass index with short-term outcomes after cardiac surgery: retrospective study and meta – analysis. Medicina. 2018;78(3):171–179.
31. Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and Cardiovascular Disease: a Scientific Statement From the American Heart Association. Circulation. 2021;143:e984–e1010.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
