Back to Journals » International Journal of General Medicine » Volume 15
The Prognostic Value of Thyroid-Stimulating Hormone in Patients with Coronary Artery Disease and Depression
Authors Li W, Qiu D, Yin H, Wang Y, Chen Y, Liu Q, Ma H, Geng Q
Received 26 February 2022
Accepted for publication 20 April 2022
Published 4 May 2022 Volume 2022:15 Pages 4675—4683
DOI https://doi.org/10.2147/IJGM.S364146
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Weiya Li,1,* Di Qiu,2,* Han Yin,1 Yu Wang,1 Yilin Chen,3 Quanjun Liu,3 Huan Ma,1 Qingshan Geng1,3
1Guangdong Cardiovascular Institute, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Guangzhou, People’s Republic of China; 2Department of Anesthesiology, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, People’s Republic of China; 3School of Medicine, South China University of Technology, Guangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qingshan Geng, Guangdong Cardiovascular Institute, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Guangzhou, People’s Republic of China, Tel +86 20 83827812, Email [email protected]
Purpose: Patients with the comorbidity of coronary artery disease (CAD) and depression are very common and always have poor prognosis. The relationship between thyroid-stimulating hormone (TSH) levels and major cardiovascular event (MACE) in these patients is still unknown. We aimed to explore this association.
Patients and Methods: We enrolled 203 CAD patients proven by coronary angiography (CAG). In the meanwhile, they were all assessed to have depression symptom by professional psycho-cardiologists. After an average follow-up of 23.7 months, patients were divided into two groups (high TSH group with TSH ≥ 1.395μIU/mL and low TSH group with TSH < 1.395μIU/mL) according to the cut-off value of baseline TSH. The impact of two different TSH groups for adverse events in CAD patients with depression was evaluated.
Results: The average age of these patients was 64.9 years old. The two TSH groups had no significant difference in the comparison of other baseline data. Area under the receiver operating characteristic (ROC) curves (AUC) analysis indicated the well-discriminatory power of TSH levels for the occurrence of MACE (AUC = 0.61, 95% CI: 0.52– 0.70, P = 0.03). In the KM survival analysis, high TSH group had a higher risk of MACE (P = 0.029). After multi-factor adjustment, there still existed a higher risk of MACE in high TSH group (HR = 2.05, 95% CI: 1.08– 3.88, P = 0.028).
Conclusion: In patients with the comorbidity of CAD and depression, higher TSH levels are associated with the occurrence of MACE. More researches need to be conducted to prove this association and explore whether the drug-related TSH reduction can decrease the occurrence of adverse events in the future.
Keywords: thyroid-stimulating hormone, TSH, coronary artery disease, CAD, depression, MACE
Introduction
Coronary artery disease (CAD), one of the major forms of cardiovascular diseases (CVDs), is usually defined as ischemic symptoms associated with the evidence of 50% or more blockage in at least one major coronary artery by coronary angiographic (CAG), previous hospitalization for a myocardial infarction (MI), or angina.1 CVDs were the primary cause of mortality in non-communicable diseases and accounted for about one-third of all deaths worldwide (17.5 million deaths) in 2012 according to the World Health Organization Reports.2 CAD and depression are two huge challenges that global public health needs to face, especially in the developed and developing countries.1,3 In China, the prevalence of depression in CAD patients from the community ranged from 34.6% to 45.8% and hospitalized patients with the comorbidity of depression and CAD even reached 51%.4
Previous studies have proved the upper part of the reference range of thyroid-stimulating hormone (TSH) levels was associated with endothelial dysfunction,5 systolic and diastolic blood pressure,6 arterial stiffness7 and coronary atherosclerosis,8 less favourable lipid levels9 and myocardial infarction.10 Other evidence also showed that a higher level of TSH was closely related to the occurrence, severity of CAD and poor prognosis in CAD patients.8,11–14 TSH is also believed to have associations with depression, but some debates exist. In some studies, the conclusion is that TSH has a negative correlation with depression.15–19 Some researches support the view that they are positively related.17,20
CAD patients with the comorbidity of depression always have a poor prognosis.21 Hypothalamic-pituitary-thyroid axis, as an important part of neuroendocrine system, is a vital mechanism of the comorbidity of CAD and depression.22 TSH is the most sensitive marker of thyroid function23 and is associated with both CAD and depression. The association between TSH and prognostic value in CAD patients with depression is unknown. Our study aimed to explore the predictive power of TSH levels for the major cardiovascular event (MACE) in these patients.
Patients and Methods
Study Population
Our study enrolled 705 patients who have undergone CAG surgery in the Cardiology Department of Guangdong Provincial People’s Hospital from October 2017 to January 2018. Patients with the missing TSH and follow-up data, thyroid disease, usage of drugs affecting TSH recently or other cardiac severe comorbidities were excluded. And we also excluded those who were assessed without depression or did not complete the Patient Health Questionnaire-9 (PHQ-9). A total of 203 patients who were proved at least one epicardial coronary artery stenosis ≥50% through CAG and with mild depression or above were included in our final analysis.
Our study is a prospective observational study aimed to investigate the predicting effect of patients’ baseline TSH to poor prognosis. The Medical Ethics Committee of Guangdong Provincial People’s Hospital had reviewed and approved our proposal (No. GDREC2017203H). This study was conducted in accordance with the Declaration of Helsinki. We have obtained written informed consents from every participant.
Depression Assessment
PHQ-924 is a widely used instrument to screen depression, and its validity in Chinese CAD patients has been verified.25 Patients with a PHQ-9 score ≥5 were defined as having depression symptoms. A higher score means more severe depression. Our professional psycho-cardiologists assessed the depression status for all patients one day before the CAG through the PHQ-9 scale.
Diagnostic Criteria of Other Variables
Body mass index (BMI) was calculated via weight divided by height. Hypertension was defined as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg for twice at different times, or currently receiving antihypertensive therapy. Diabetes specifically refers to type 2 diabetes and was diagnosed with blood glucose ≥ 7.0mmol /L, random blood glucose ≥11.1mmol/L, 2h blood glucose ≥11.1mmol/L after glucose load or under the hypoglycemic treatment.
The severity of coronary artery stenosis was dependent on the number of three main vessels with stenosis ≥50% as shown by CAG, while patients with a stenosis of left main coronary artery ≥30% would be defined as the highest severity level. Education background was divided into four levels according to the years of receiving education. There were four levels including less than 6 years, 7–9 years, 10–12 years and more than 12 years, respectively. We used the Cockcroft-Gault formula to calculate the creatinine clearance (CCR) through the serum creatinine tested at admission.26
Biochemical Examination
The nurses extracted patients’ venous blood samples in the early morning, thyroid function including TSH, Free Triiodothyronine (FT3), Free Tetraiodothyronine (FT4) were measured through direct chemical lighting method (US Siemens company). The reference range of TSH is 0.56–5.91 μIU/mL. Other indicators include blood lipids, Hs-CRP, which were measured by a fully automated luminescent immunoassay.
Follow-Up and Endpoint Events
All patients were followed up by trained cardiovascular physicians by telephone or in-person at 1 year, and 2 years after discharges. The average follow-up time was 23.7 ± 6.3 months. MACE was considered as the endpoint of our follow-up. MACE included death due to cardiovascular events, non-fatal stroke, non-fatal myocardial infarction, non-fatal heart failure, and revascularization. Patients for whom we could not obtain accurate terminal events through follow-up were excluded.
TSH Groups and Statistical Analysis
At the data analysis stage, all 203 CAD patients with depression were separated into two groups according to the condition of baseline TSH and MACEs. Receiver operating characteristic (ROC) curves showed the most discriminating cutoff point values of TSH to predict the occurrences of MACE. Then, we got the cutoff point value of TSH was 1.395 μIU/mL, and patients were divided into two groups according to this threshold value (high TSH group with TSH ≥1.395 and low TSH group with TSH <1.395).
Measurement data in accordance with normal distribution was described as mean ± SD, the non-normal distribution of metrology was expressed in the form of median (interquartile range), and counting data was represented as number and percentage. The data were analyzed by the chi-squared statistic tests, Fisher’s exact tests, independent sample t-tests, the one-way analysis of variance test, or the Kruskal–Wallis test when appropriate. Cox proportional hazards regression models and Kaplan–Meier (KM) survival analysis were used to evaluate the differences of MACE between the two TSH groups.
The baseline data were first compared. Due to the limitation of small sample size and in order not to omit variables that might affect the outcome, the criteria of being included in the univariate Cox regression analysis was relaxed to with a baseline difference level of less than 0.25 (gender, blood glucose, HDLC, CCR, BUN, FT4, Hs-CRP, LVEF, type of CAD were included). In univariate Cox regression analysis, variables with a significance level of 0.05 (only gender with a p-value = 0.029) were regarded as correction variables for multivariate Cox regression. Other variables considered to be most closely related to MACE, such as age and severity of coronary artery stenosis, were also included in the multivariate Cox regression. Data were analyzed using SPSS version 25.
Results
Baseline Characteristics
A total of 203 patients who were proved at least one epicardial coronary artery stenosis ≥50% through CAG and with mild depression or above were included in our final analysis. There are 72 stable angina pectoris, 92 patients with unstable angina, and 39 acute MI patients in our population. Of all 203 CAD patients with depression, 138 (68%) were male, 65 (32%) were female. The average age of the patients was 64.9 y. 126 (62.1%) and 83 (40.9%) were diagnosed with hypertension and diabetes, respectively. Table 1 shows the baseline demographic laboratory tests as well as social and medical history in two TSH groups. The two groups had no significant difference in the comparison of the baseline.
 |
Table 1 Baseline Characteristics Among Participants Grouped by TSH |
TSH for Predicting the Outcomes
All the patients were followed up for an average of about 24 months (ranged from several days to 29 months). There were 42 MACEs happened in our study. Area under the ROC curves (AUC) analysis indicated the well-discriminatory power of TSH levels for the presence of MACE (AUC = 0.61, 95% CI: 0.52–0.70, P = 0.03, Figure 1). In the KM survival analysis, high TSH group had a higher risk of MACE (P = 0.029, Figure 2). After adjusting for all potential confounders including age, gender, and severity of coronary artery stenosis, there still existed a higher risk of MACE in high TSH group (HR = 2.05, 95% CI: 1.08–3.88, P = 0.028, Figure 3, Table 2).
 |
Table 2 Unadjusted and Adjusted Predictive Value of TSH Levels for MACE Events in CAD Patients with Depression |
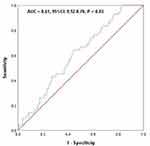 |
Figure 1 ROC curves showed discriminatory power of TSH levels on MACE. |
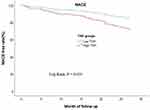 |
Figure 2 Kaplan–Meier curve for MACE events grouped by TSH level in CAD patients with depression. |
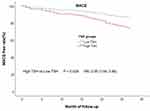 |
Figure 3 Cox regression curve for MACE events grouped by TSH level in CAD patients with depression after adjusting for age, sex, and the severity of coronary artery stenosis. |
Discussion
The prevalence of depression is high in patients with CAD.22 These patients with the comorbidity of depression and CAD still easily experienced MACE even after percutaneous coronary intervention (PCI) treatment. To our knowledge, this is the first study to explore the predictive value of TSH in patients with the comorbidity of depression and CAD. We found that MACE was more likely to occur in patients with higher TSH (TSH ≥1.395) with or without adjustment for multifactorial variables.
Association Among TSH, CAD and Depression
Several studies have explored the effect of TSH to CAD patients, they found higher TSH had diagnostic and prognostic significance of CAD and was associated with the severity of CAD.11–13 Previous studies have shown that TSH will calcify coronary artery by combining TSH receptor on vascular smooth muscle cells.27,28 Yoneda et al found the injection of TSH in conduit arteries could significantly impair endothelial vasodilation,29 which might aggravate the symptoms of CAD patients and affect their prognosis.
Serum TSH was also proved to increase inflammatory molecules and inhibit nitric oxide production.12,30 The increased inflammatory reaction will accelerate the atherosclerosis process and inhibit endothelial cell functions, such as migration and angiogenesis.29,31 What is more, chronic low-grade inflammation was believed to be one important pathogenesis of depression.32 In our study, patients with high TSH levels had a higher hypersensitive-c-reactive-protein (Hs-CRP) but did not reach a statistical significance (Median value 4.1 vs 2.6 mg/L).
As we all know, serum lipid is one of the recognized risk factors of CAD, TSH levels were found positively associated with serum lipid concentrations.9 What is more, in a national study with a large sample in Korean, a significant association was observed between the high level of HDL-C, triglyceride and depression.33 TSH was also proved positively related to HDLC in depression patients.34 TSH may cause poor prognosis by indirectly affecting the blood lipids in patients with coronary heart disease and depression.
TSH can also stimulate the production of cytokines interleukin 6 (IL-6) secretion by adipocytes and tumour necrosis factor-α (TNF-α) secretion by bone marrow cells, these cytokines were associated with the damage of endothelium-dependent vasodilation and oxidative stress.35 Cytokines are strongly associated with depression. He et al found the concentration of cytokines such as IL-6 and vascular endothelial growth factor (VEGF) increased in mice with depression and these cytokines may become predictive biomarkers for novel diagnostic as well as therapeutic of depression.36
In the study of Yang et al, higher levels of TSH were independently related to the presence of CAD only among participants ≤65 years old.14 There is still no suitable explanation to age-related differences on CAD, while the age of TSH groups in our study has no statistical difference. FT4 is a prohormone that cannot be transported by myocytes and has no relationship to adaptive response to myocardial ischemia in CAD patients.29,37 In our study, it may be limited by the small sample size that the level of FT4 has a significant difference at baseline. In statistical analysis, FT4 did not contribute to MACE in univariate Cox regression, which might also indicate that the difference in FT4 was accidental.
The association between thyroid function and psychiatric disorders, particularly mood disorders, has long been recognized and described more than 200 years ago.38 Lee et al found the highest TSH tertile group was 1.92 times more likely to have depressive symptoms in Korea.17 A retrospective cohort study that included 13,017 subjects described the same conclusion that the highest tertile TSH level owed higher risk of depressive symptom.20 Higher TSH reduces the efficacy of antidepressant therapy by affecting brain-derived neurotrophic factor levels in depressed patients.23 Some studies indicated that TSH was negatively correlated with depression, and low TSH values might be considered either a compensating physiological response to stress or a pathological element in a co-existing depression.15,39 Joffe and Levitt’s study showed the low-normal TSH group was significantly more depressed and had higher suicidal tendencies than the high-normal group.40 The real effect of TSH in depression is not very sure and needs larger as well as higher quality research to prove in different sex, age, races and regions.
Strengths and Limitations
The strength of our study is that we continuously enroll patients with angiography-proven CAD in three months. This approach significantly decreases the potential errors in the diagnosis of the disease. All included patients have finished the depression scales under the guidance of professional doctors. This is the first study to explore the relationship of TSH in CAD patients with depression. It has important implications for improving the prognosis of part of the special patients with CAD. Due to the sample quantity and the limit of the endpoint events, we did not analyze the patients with MI or angina pectoris individually. There are still some limitations in our study. At first, our research was conducted in a single center from a southern central hospital, which cannot represent patients in the entire China or other regions. Secondly, the small sample size might lead to inaccurate conclusions. Thirdly, since the subsequent TSH data is not obtained, the impact of TSH changes on poor prognosis cannot be evaluated. Finally, the influence of high TSH to MACE might be underestimated because patients who experienced emergency PCI surgery and always had a bad prognosis were not included.
Conclusion
In patients with the comorbidity of CAD and depression, higher TSH levels are associated with the occurrence of MACE. More researches need to be conducted to prove this association and explore whether the drug-related TSH reduction can decrease the occurrence of adverse events in the future.
Acknowledgments
We wish to thank all the study participants and research staff who participated in this research.
Disclosure
All the authors declare that they don’t have any conflict of interest in the study.
References
1. Mavrides N, Nemeroff C. Treatment of depression in cardiovascular disease. Depress Anxiety. 2013;30(4):328–341. doi:10.1002/da.22051
2. Zhu KF, Wang YM, Zhu JZ, et al. National prevalence of coronary heart disease and its relationship with human development index: a systematic review. Eur J Prev Cardiol. 2016;23(5):530–543. doi:10.1177/2047487315587402
3. Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J. 2006;27(23):2763–2774. doi:10.1093/eurheartj/ehl338
4. Ren Y, Yang H, Browning C, et al. Prevalence of depression in coronary heart disease in China: a systematic review and meta-analysis. Chin Med J. 2014;127(16):2991–2998.
5. Volzke H, Robinson DM, Spielhagen T, et al. Are serum thyrotropin levels within the reference range associated with endothelial function? Eur Heart J. 2009;30(2):217–224. doi:10.1093/eurheartj/ehn508
6. Asvold BO, Bjoro T, Nilsen TI, et al. Association between blood pressure and serum thyroid-stimulating hormone concentration within the reference range: a population-based study. J Clin Endocrinol Metab. 2007;92(3):841–845. doi:10.1210/jc.2006-2208
7. Lambrinoudaki I, Armeni E, Rizos D, et al. High normal thyroid-stimulating hormone is associated with arterial stiffness in healthy postmenopausal women. J Hypertens. 2012;30(3):592–599. doi:10.1097/HJH.0b013e32834f5076
8. Auer J, Berent R, Weber T, et al. Thyroid function is associated with presence and severity of coronary atherosclerosis. Clin Cardiol. 2003;26(12):569–573. doi:10.1002/clc.4960261205
9. Asvold BO, Vatten LJ, Nilsen TI, et al. The association between TSH within the reference range and serum lipid concentrations in a population-based study. The HUNT study. Eur J Endocrinol. 2007;156(2):181–186. doi:10.1530/eje.1.02333
10. Westerink J, van der Graaf Y, Faber DR, et al. Relation between thyroid-stimulating hormone and the occurrence of cardiovascular events and mortality in patients with manifest vascular diseases. Eur J Prev Cardiol. 2012;19(4):864–873. doi:10.1177/1741826711416045
11. Dutka R, Chmyr N, Svitlyk H, et al. Prolactin, cortisol, free thyroxine and thyroid-stimulating hormone - markers of staging of metabolic syndrome as a risk factor of coronary artery disease and type 2 diabetes mellitus. Georgian Med News. 2019;297:80–83.
12. Ortolani PD
13. Ndrepepa G, Braun S, Mayer K, et al. Prognostic value of thyroid-stimulating hormone within reference range in patients with coronary artery disease. Metabolism. 2015;64(10):1308–1315. doi:10.1016/j.metabol.2015.07.009
14. Yang L, Zou J, Zhang M, et al. The relationship between thyroid stimulating hormone within the reference range and coronary artery disease: impact of age. Endocr J. 2013;60(6):773–779. doi:10.1507/endocrj.EJ12-0448
15. Kvetny J, Ellervik C, Bech P. Is suppressed thyroid-stimulating hormone (TSH) associated with subclinical depression in the Danish General Suburban Population Study?. Nord J Psychiatry. 2015;69(4):282–286. doi:10.3109/08039488.2014.972454
16. Forman-Hoffman V, Philibert RA. Lower TSH and higher T4 levels are associated with current depressive syndrome in young adults. Acta Psychiatr Scand. 2006;114(2):132–139. doi:10.1111/j.1600-0447.2005.00703.x
17. Lee S, Oh SS, Park EC, et al. Sex differences in the association between thyroid-stimulating hormone levels and depressive symptoms among the general population with normal free T4 levels. J Affect Disord. 2019;249:151–158. doi:10.1016/j.jad.2019.02.027
18. Panicker V, Evans J, Bjoro T, et al. A paradoxical difference in relationship between anxiety, depression and thyroid function in subjects on and not on T4: findings from the HUNT study. Clin Endocrinol (Oxf). 2009;71(4):574–580. doi:10.1111/j.1365-2265.2008.03521.x
19. Bunevicius R, Kusminskas L, Mickuviene N, et al. Depressive disorder and thyroid axis functioning during pregnancy. World J Biol Psychiatry. 2009;10(4):324–329. doi:10.3109/15622970903144038
20. Kim EY, Kim SH, Rhee SJ, et al. Relationship between thyroid-stimulating hormone levels and risk of depression among the general population with normal free T4 levels. Psychoneuroendocrinology. 2015;58:114–119. doi:10.1016/j.psyneuen.2015.04.016
21. Tully PJ, Ang SY, Lee EJ, et al. Psychological and pharmacological interventions for depression in patients with coronary artery disease. Cochrane Database Syst Rev. 2021;12:CD008012. doi:10.1002/14651858.CD008012.pub4
22. Vaccarino V, Badimon L, Bremner JD, et al. Depression and coronary heart disease: 2018 position paper of the ESC working group on coronary pathophysiology and microcirculation. Eur Heart J. 2020;41(17):1687–1696. doi:10.1093/eurheartj/ehy913
23. Baek JH, Kang ES, Fava M, et al. Thyroid stimulating hormone and serum, plasma, and platelet brain-derived neurotrophic factor during a 3-month follow-up in patients with major depressive disorder. J Affect Disord. 2014;169:112–117. doi:10.1016/j.jad.2014.08.009
24. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi:10.1046/j.1525-1497.2001.016009606.x
25. Zhu Y, Blumenthal JA, Shi C, et al. Sedentary behavior and the risk of depression in patients with acute coronary syndromes. Am J Cardiol. 2018;121(12):1456–1460. doi:10.1016/j.amjcard.2018.02.031
26. Malavasi VL, Valenti AC, Ruggerini S, et al. Kidney function according to different equations in patients admitted to a cardiology unit and impact on outcome. J Clin Med. 2022;11(3):891. doi:10.3390/jcm11030891
27. Zhang Y, Kim BK, Chang Y, et al. Thyroid hormones and coronary artery calcification in euthyroid men and women. Arterioscler Thromb Vasc Biol. 2014;34(9):2128–2134. doi:10.1161/ATVBAHA.114.303889
28. Satomi-Kobayashi S, Kinugasa M, Kobayashi R, et al. Osteoblast-like differentiation of cultured human coronary artery smooth muscle cells by bone morphogenetic protein endothelial cell precursor-derived regulator (BMPER). J Biol Chem. 2012;287(36):30336–30345. doi:10.1074/jbc.M111.329110
29. Balli M, Cetin M, Tasolar H, et al. The relationship between serum thyroid hormone levels, subclinical hypothyroidism, and coronary collateral circulation in patients with stable coronary artery disease. Turk Kardiyol Dern Ars. 2016;44(2):130–136. doi:10.5543/tkda.2015.00905
30. Desideri G, Bocale R, Milardi D, et al. Enhanced proatherogenic inflammation after recombinant human TSH administration in patients monitored for thyroid cancer remnant. Clin Endocrinol (Oxf). 2009;71(3):429–433. doi:10.1111/j.1365-2265.2008.03485.x
31. Kuo L, Davis MJ, Cannon MS, et al. Pathophysiological consequences of atherosclerosis extend into the coronary microcirculation. Restoration of endothelium-dependent responses by L-arginine. Circ Res. 1992;70(3):465–476. doi:10.1161/01.RES.70.3.465
32. Lamon-Fava S, So J, Mischoulon D, et al. Dose- and time-dependent increase in circulating anti-inflammatory and pro-resolving lipid mediators following eicosapentaenoic acid supplementation in patients with major depressive disorder and chronic inflammation. Prostaglandins Leukot Essent Fatty Acids. 2021;164:102219. doi:10.1016/j.plefa.2020.102219
33. Oh J, Kim TS. Serum lipid levels in depression and suicidality: the Korea National Health and Nutrition Examination Survey (KNHANES) 2014. J Affect Disord. 2017;213:51–58. doi:10.1016/j.jad.2017.02.002
34. Peng R, Dai W, Li Y. Low serum free thyroxine level is correlated with lipid profile in depressive patients with suicide attempt. Psychiatry Res. 2018;266:111–115. doi:10.1016/j.psychres.2018.05.059
35. Onat A, Aydin M, Can G, et al. Normal thyroid-stimulating hormone levels, autoimmune activation, and coronary heart disease risk. Endocrine. 2015;48(1):218–226. doi:10.1007/s12020-014-0269-z
36. He Y, Fu X, Li L, et al. AaSPL9 affects glandular trichomes initiation by positively regulating expression of AaHD1 in Artemisia annua L. Plant Sci. 2022;317:111172. doi:10.1016/j.plantsci.2021.111172
37. Davis PJ, Davis FB. Nongenomic actions of thyroid hormone on the heart. Thyroid. 2002;12(6):459–466. doi:10.1089/105072502760143827
38. Hage MP, Azar ST. The link between thyroid function and depression. J Thyroid Res. 2012;2012:590648. doi:10.1155/2012/590648
39. Williams MD, Harris R, Dayan CM, et al. Thyroid function and the natural history of depression: findings from the Caerphilly Prospective Study (CaPS) and a meta-analysis. Clin Endocrinol (Oxf). 2009;70(3):484–492. doi:10.1111/j.1365-2265.2008.03352.x
40. Joffe RT, Levitt AJ. Basal thyrotropin and major depression: relation to clinical variables and treatment outcome. Can J Psychiatry. 2008;53(12):833–838. doi:10.1177/070674370805301209
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
