Back to Journals » Journal of Inflammation Research » Volume 16
The Prognostic Value of Blood Eosinophil Level in AECOPD is Influenced by Corticosteroid Treatment During Hospitalization
Authors Li J , Liang L , Feng L , Cao S, Cai YS, Li X, Qian Z, Brightling CE, Tong Z
Received 16 May 2023
Accepted for publication 24 July 2023
Published 2 August 2023 Volume 2023:16 Pages 3233—3243
DOI https://doi.org/10.2147/JIR.S421605
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tara Strutt
Jiachen Li,1 Lirong Liang,1 Lin Feng,1 Siyu Cao,2 Yutong Samuel Cai,3 Xiaobo Li,4 Zhenbei Qian,2 Christopher E Brightling,5 Zhaohui Tong2
1Department of Clinical Epidemiology, Beijing Institute of Respiratory Medicine and Beijing Chao-Yang Hospital, Capital Medical University, Beijing, People’s Republic of China; 2Department of Respiratory and Critical Care Medicine, Beijing Institute of Respiratory Medicine and Beijing Chao-Yang Hospital, Capital Medical University, Beijing, People’s Republic of China; 3Centre for Environmental Health and Sustainability, Department of Population Health Sciences, University of Leicester, Leicester, UK; 4Beijing Key Laboratory of Environmental Toxicology, School of Public Health, Capital Medical University, Beijing, People’s Republic of China; 5Institute for Lung Health, NIHR Leicester Biomedical Research Centre, University of Leicester, Leicester, UK
Correspondence: Lirong Liang, Department of Clinical Epidemiology, Beijing Institute of Respiratory Medicine and Beijing Chao-Yang Hospital, Capital Medical University, No. 8 Gongren Tiyuchang Nanlu, Chaoyang District, Beijing, 100020, People’s Republic of China, Tel +86 010-85231547, Email [email protected]
Purpose: Blood eosinophil is a promising biomarker for phenotyping patients with acute exacerbation of COPD (AECOPD). We aimed to evaluate the prognostic value of eosinophil on short- and long-term outcomes stratified by corticosteroid treatment among AECOPD inpatients.
Patients and Methods: In this retrospective cohort study, we included patients hospitalized for AECOPD from July 2013 to June 2021 in Beijing, China. Clinical data were collected from electronic medical records. The blood eosinophil count was measured within 24h after admission. Eosinophilic AECOPD was defined as having an eosinophil percentage ≥ 2%. The study outcomes were length of stay (LOS), treatment failure, and AECOPD readmission risk within 3 years of discharge. Multivariable models were used to analyze the associations between blood eosinophil count and outcomes stratified by corticosteroid treatment during hospitalization.
Results: A total of 2406 AECOPD patients were included. The median LOS of AECOPD patients was 10 (interquartile range: 8– 14) days. The eosinophil percentage was negatively associated with LOS (P-trend=0.014). Compared with the non-eosinophilic AECOPD group, the eosinophilic group had a 58% lower risk of treatment failure (OR=0.42, 95% CI: 0.20– 0.89) in patients treated with systemic corticosteroids, but no association was observed in those treated with inhaled corticosteroids (ICS) only (OR=0.95, 95% CI: 0.60– 1.52). The eosinophilic group had an increased risk of 90-day re-admission in patients treated with ICS only (HR=1.51, 95% CI: 1.00– 2.29), but not in patients treated with systemic corticosteroids during hospitalization (HR=0.67, 95% CI: 0.39– 1.15). No statistically significant results were found for 180-day, 1-year, or 3-year readmission risk.
Conclusion: Elevated blood eosinophils in AECOPD were associated with shorter length of stay and improved response to treatment with systemic corticosteroids, but not inhaled corticosteroids. Our study suggested that a therapeutic approach of using systemic corticosteroid may benefit patients present with eosinophilic AECOPD.
Keywords: chronic obstructive pulmonary disease, eosinophilic inflammation, glucocorticoids, interaction
Introduction
Chronic obstructive pulmonary disease (COPD) is currently one of the three leading causes of death worldwide in 2019.1 Tobacco smoking is a major risk factor for the incidence and exacerbation of COPD. Acute exacerbations of COPD (AECOPD) are associated with accelerated loss of lung function, elevated risk of further hospitalization and mortality, as well as a substantial burden of healthcare costs. AECOPD is heterogeneous, and the identification of phenotypes through specific biomarkers might facilitate risk stratification and individualized treatment.2
The blood eosinophil count has been implicated as an important biomarker in AECOPD. Bafadhel et al identified an eosinophilic-predominant phenotype based on peripheral eosinophils and other inflammatory biomarkers.3 Studies found that eosinophilic AECOPD patients had less requirement for mechanical ventilation, shorter length of hospital stay, and lower mortality compared with non-eosinophilic AECOPD patients.4–7 The underlying mechanisms are not fully understood. Eosinophilic AECOPD may represent a milder phenotype because eosinophil level is inversely related to bacterial infection.8–10 Another possible explanation is that patients with higher levels of eosinophil tend to have a better response to corticosteroid treatment.11–13 Moreover, eosinophil levels have been found to be predictive of short- and long-term exacerbations. However, the findings were inconsistent,4,6,14–19 which may be attributed to population heterogeneity and relatively small sample sizes, as well as to a lack of studies evaluating the complex interactions such as patient characteristics and different combinations of corticosteroid treatment.
Systemic corticosteroids have been a cornerstone of treatment for AECOPD.1 There is, however, a discrepancy between international guidelines and clinical practice in China, where many AECOPD patients did not receive systemic corticosteroids due to concerns about its adverse effects. About 40% of hospitalized AECOPD patients received only inhaled corticosteroid (ICS) treatment in China.20 Blood eosinophil count has the potential to guide corticosteroid treatment to minimize the cumulative dose, and current guidelines recommend using eosinophil levels to guide ICS treatment in stable COPD.21,22 In AECOPD, the use of systemic corticosteroids guided by eosinophils is still debated.23,24 It is therefore imperative to investigate how blood eosinophil level interacts with corticosteroid treatment (inhaled or systemic) on outcomes among AECOPD patients in different real-world settings.
We hypothesized that systemic corticosteroid treatment would modify the associations of blood eosinophils and in-hospital outcomes and readmissions among AECOPD inpatients. To test this hypothesis, we conducted a retrospective cohort study to examine the association between blood eosinophils and treatment failure stratified by corticosteroid use in AECOPD inpatients. We also investigated whether blood eosinophils could predict short- and long-term AECOPD readmissions.
Materials and Methods
Study Subjects
We conducted an electronic medical record (EMR)-based retrospective study of hospitalized AECOPD patients in a tertiary hospital in Beijing, China. This study was approved by the Research Ethics Board of Beijing Chaoyang Hospital (2020-ke-511). Informed consent was waived by the Research Ethics Board of Beijing Chaoyang Hospital due to the retrospective nature of the study. Patient data was anonymized before analysis. All methods were carried out in accordance with the Declaration of Helsinki.
The EMR data of all patients admitted to Beijing Chao-Yang Hospital from July 2013 to June 2021 were anonymized and extracted. AECOPD patients were identified based on the International Classification of Diseases 10th Revision (ICD-10) code. We included patients aged ≥ 40 years with a primary discharge diagnosis code of J44. The rationale for the age criterion was that most COPD cases were diagnosed in people over 40 years, and airflow limitation in people below 40 years was more likely due to asthma and other causes than COPD. Patients were excluded if they: had missing data in admission notes, blood routine tests, and inpatient prescriptions; had comorbid asthma, pneumothorax, pulmonary embolism, acute coronary syndrome, lung cancer, systemic fungal infection, severe mental illness, and pneumonia at entry; received invasive mechanical ventilation within 48 h after admission; had no blood eosinophil measured within 24 h after admission; had extreme values in eosinophil level (count > 2000 cells/μL or percentage > 20%); had a length of stay (LOS) > 50 days. For patients who had multiple AECOPD admissions during the study period, only the first admission was included.
Exposure and Covariates
Blood eosinophil count measured within 24 h after admission was obtained from the Laboratory Information System (LIS). The blood eosinophil count was analyzed by fluorescence flow cytometry. A cutoff value of 2% in eosinophil percentage was used to define the eosinophilic group and non-eosinophilic group because it is sensitive for predicting eosinophilic airway inflammation and eosinophil-associated exacerbations according to previous studies.3,7 To reflect the absolute burden of eosinophils, we also classified AECOPD patients based on eosinophil count, with cutoff values of 150 and 300 cells/μL.
Age, sex, and comorbidities were collected from the front page of discharge records. Charlson Comorbidity Index was calculated.25 Self-reported smoking status (Never, former, current, missing) was extracted from the unstructured texts in EMR using natural language processing. Smoking status was asked and recorded by the physician during the inquiry of medical history. Former smokers referred to patients who had ever smoked in their lifetime but had quit smoking before admission, regardless of how long they had quit. To obtain the frequency of AECOPD hospitalizations in the preceding year, we linked the ID of our participants to a citywide database that covered all hospital admissions in Beijing.26 Information on medication use during hospitalization was extracted from the electronic prescription system. Patients were categorized into three groups according to corticosteroid treatment during hospitalization: no corticosteroids, only nebulized ICS, and systemic corticosteroids (including nebulized ICS combined with systemic corticosteroids). ICS delivered via inhalers were not included because they were not suitable and rarely used for AECOPD inpatients.
Study Outcomes
The study outcomes were LOS, treatment failure, and AECOPD readmission risk within 3 years of discharge. Treatment failure was a composite outcome to describe the effect of AECOPD treatment. According to previous recommendations27 and data availability, the components of treatment failure included death during hospitalization or within 30 days after discharge, require invasive mechanical ventilation, transfer to intensive care unit (ICU), and AECOPD readmission within 30 days after discharge. Patients who had any one of these events were considered to have treatment failure. LOS and in-hospital events were collected from EMR.
Patients discharged alive were followed up for AECOPD readmissions up to 3 years. The follow-up ended at the first AECOPD readmission, death, or 30 June 2021, whichever occurred first. The follow-up was conducted by electronic linkage to a citywide hospitalization database maintained by Beijing Municipal Health Commission Information Center.26 Readmission date and discharge diagnoses were obtained. Fewer than 1% of the patients (n=20) could not be linked to the hospitalization database and thus had no follow-up data.
Statistical Analysis
We described the distribution of blood eosinophil in AECOPD patients using histograms. Spearman correlation coefficient was calculated to assess the concordance between eosinophil count and percentage. Baseline characteristics were compared between eosinophilic and non-eosinophilic groups using t-test for continuous variables and chi-squared test for categorical variables.
Generalized linear models with gamma distribution and log link were used to examine the association between eosinophil levels and LOS. A cubic polynomial was included to capture the potential non-linear relationship. Linear trend was tested by including the continuous LOS in the model. Logistic models were used to investigate the association between eosinophil group and treatment failure. Model covariates were selected based on prior knowledge, including sex, age, Charlson index, smoking status, white blood cell count, antibiotics use, bronchodilator use, emergency hospitalization, and number of AECOPD hospitalizations in the previous year. We calculated the 90-day, 180-day, 1-year, and 3-year AECOPD readmission rates. Patients with incomplete follow-up time (eg included between July 2018 to June 2021 and did not have COPD readmission during the follow-up period) were treated as censored data. Competing-risks regression models28 were used to investigate the association between eosinophil group and the risk of AECOPD readmission accounting for death as a competing risk. LOS of the baseline hospitalization was further adjusted for in the analysis of readmission risk.
We performed overall and subgroup analyses by corticosteroid use during hospitalization. Only 276 patients were not treated with corticosteroids, so we mainly presented results of the ICS-only group and the systemic corticosteroid group. Statistical interactions between eosinophil level and corticosteroids treatment (ICS only vs systemic corticosteroids) on outcomes were tested using likelihood ratio test which compared models with and without a cross-product term. We performed all analyses using Stata (version 15.1, StataCorp). The significant level was 0.05 for a two-tailed test.
Results
A total of 5611 AECOPD admissions were identified from 2013 to 2021, of which 3282 were eligible for our study. After excluding multiple admissions of the same patient, we included 2406 patients in the analysis (Figure 1). The mean age (SD) of these patients was 70.8 (9.7) years, and 74.9% were men. The median pack-year in ever smokers was 40 (interquartile range: 20–52.5). The median arterial oxygen saturation at admission was 94.7% (interquartile range: 91.3%-96.7%).
 |
Figure 1 Flowchart of inclusion and exclusion process. Abbreviations: COPD, chronic obstructive pulmonary disease; LOS, length of stay. |
The distribution of blood eosinophils measured at admission for AECOPD was shown in Additional File 1: Figure S1. The median (interquartile range) of eosinophil count and percentage were 100 (20–210) cells/μL and 1.6% (0.3%-3.2%), respectively. More than half of AECOPD patients had an eosinophil count lower than 150 cells/μL (61.0%) or an eosinophil percentage lower than 2% (55.8%). There was a positive linear correlation (ρ=0.963, P<0.001) between eosinophil count and percentage (Additional File 1: Figure S2), and an agreement rate of 90.5% (Kappa=80.6%) was found between the two classifications using 2% and 150 cells/μL thresholds (Additional File 1: Table S1).
Compared with AECOPD patients with lower levels of eosinophil, those with higher levels of eosinophil were younger, more likely to be male, less likely to have AECOPD hospitalization in the previous year, and had lower white blood cell count and C-reactive protein (CRP). Most of the AECOPD patients were treated with corticosteroids during hospitalization (n=2130, 88.5%). Among them, 1378 (64.7%) patients were treated with ICS only, and 752 (35.3%) patients were treated with systemic corticosteroids (with or without ICS). The mean duration of systemic corticosteroid treatment was 4.4±5.2 days. Patients with eosinophil ≥ 2% had shorter duration of systemic corticosteroid treatment than those with eosinophil < 2% (3.8±3.8 versus 5.0±5.3 days). Patients with lower levels of eosinophil were more likely to be treated with systemic corticosteroids (Table 1). Characteristics of patients by corticosteroid use during hospitalization were shown in Additional File 1: Table S2.
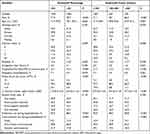 |
Table 1 Characteristics of AECOPD Patients by Blood Eosinophil Level at Entry (n=2406) |
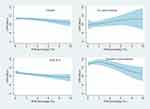
The median LOS of AECOPD patients was 10 (interquartile range: 8–14) days. The eosinophilic group (≥2%) had a shorter median LOS (10 days) than the non-eosinophilic (<2%) group (11 days). Patients treated with systemic corticosteroids had longer median LOS (12 days) than patients without corticosteroid treatment (9 days) and patients treated with ICS only (10 days). Overall, the LOS decreased almost linearly with increasing eosinophil percentage (P-trend=0.014) (Figure 2). In stratified analyses, eosinophil percentage was negatively associated with LOS in patients treated with ICS only (P-trend=0.002), while no significant association was found in patients who were not treated with corticosteroids (P-trend=0.333). For patients treated with systemic corticosteroids, a decreasing trend was observed when the eosinophil percentage was greater than 2%, although the overall trend was not statistically significant (P-trend=0.199). A similar result was found for the relationship between eosinophil count and LOS (Additional File 1: Figure S3).
There were 164 (6.8%) treatment failure events occurring, including 45 (1.9%) ICU transfer cases, 23 (1.0%) invasive mechanical ventilation cases, 30 (1.2%) deaths within 30 days, and 103 (4.3%) 30-day AECOPD readmissions. The rates of treatment failure were 8.5% and 4.7% for the non-eosinophilic and eosinophilic groups, respectively. After multivariate adjustment, the eosinophilic group had a lower risk of ICU transfer (OR=0.34, 95% CI: 0.14–0.82) compared with the non-eosinophilic group. In subgroup analysis by corticosteroid use, the eosinophilic phenotype was associated with a 58% lower risk of treatment failure among patients treated with systemic corticosteroids (OR=0.42, 95% CI: 0.20–0.89). No significant difference in treatment failure rate between eosinophilic groups was found among patients who only used ICS (OR=0.95, 95% CI: 0.60–1.52). There was a statistical interaction between eosinophil level and corticosteroid treatment on the risk of treatment failure (P for interaction=0.020) (Table 2). Similar results were found for eosinophil count (Additional File 1: Table S3).
 |
Table 2 Blood Eosinophil Percentage and Hospitalization Outcomes Among AECOPD Inpatients |
In the analysis of readmission risk, we excluded in-hospital deaths (n=21) and patients with incomplete or invalid follow-up data (n=25). A total of 2360 patients who were discharged alive were included. The median follow-up time was 2.95 years. Of all included patients, 37.0% were readmitted for AECOPD during follow-up. After accounting for competing risks, the eosinophilic phenotype was associated with an increased risk of 90-day readmission in patients only treated with ICS (HR=1.51, 95% CI: 1.00–2.29), but not in patients treated with systemic corticosteroids during hospitalization (HR=0.67, 95% CI: 0.39–1.15). There was an interaction between systemic corticosteroid use and eosinophil percentage on the risk of 90-day readmission (P for interaction=0.022). No statistically significant results were found for 180-day, 1-year, and 3-year readmission risk (Figure 3).
Discussion
In this EMR-based observational study of AECOPD patients, we found that increased blood eosinophils were associated with shorter LOS. Moreover, eosinophilic patients treated with systemic corticosteroids had a lower risk of treatment failure and short-term readmission. No associations were found between blood eosinophil levels at admission and long-term AECOPD readmissions.
Eosinophilic inflammation plays a role in the progression and exacerbation of COPD. Studies have shown that blood eosinophil counts are higher in COPD patients than in healthy controls.29,30 Nearly 30% of AECOPD were associated with sputum eosinophilia.3 The identification of eosinophilic AECOPD is often based on blood test because blood eosinophil is an accessible proxy for sputum eosinophil count.31 The increased peripheral eosinophils indicate eosinophilic airway inflammation and a higher risk of COPD exacerbations. Both absolute count and percentage could be used to evaluate blood eosinophil level, and different cut-off values have been suggested. Cut-off values of 2% and 150 cells/μL have been widely used in previous studies as they are sensitive for identifying sputum eosinophilia.32 An analysis in the ECLIPSE (Evaluation of COPD longitudinally to identify Predictive Surrogate End-points) cohort showed 88% concordance between blood eosinophil thresholds of 2% and 150 cells/μL among stable COPD patients.33 Similarly, our study in AECOPD hospitalized patients found a concordance rate of 90.5% between the two thresholds. We used the threshold of 2% and found that more than 40% of patients were eosinophilic AECOPD, indicating that eosinophilic inflammation is a common phenotype in AECOPD hospitalized patients.
Compared with non-eosinophilic AECOPD, eosinophilic AECOPD appears to have a more favorable prognosis. Blood eosinophil plays a protective role in the immune response against allergens, parasites, and viral infections. Research has demonstrated that high levels of eosinophils have beneficial effects on lung function, quality of life, and survival in COPD patients.34 Increasing evidence has revealed that hospitalized patients with eosinophilic AECOPD have shorter LOS.4,6,7 However, these studies were conducted among patients with an average LOS of about 5 days. It is unclear whether the association between blood eosinophils and LOS holds in patients with longer LOS. Our study found a negative association between eosinophils and LOS among hospitalized AECOPD patients with a median LOS of 10 days. Taking into account the continuous nature of eosinophil counts, we found that LOS decreased almost linearly as eosinophil counts increased in overall patients. It has been suggested that a longer LOS may indicate a more severe case of AECOPD.35 Our results provide evidence for using blood eosinophil as a biomarker to predict LOS in severe AECOPD patients.
An intriguing finding of the present study is that corticosteroid treatment during hospitalization could modify the association between eosinophil and AECOPD hospitalization outcomes. Among AECOPD patients without corticosteroid treatment during hospitalization, increased eosinophil count was not associated with a shorter LOS. Based on this result, the protective effect of eosinophils may be explained by better corticosteroid responsiveness in patients with higher levels of eosinophils. Eosinophilic inflammation has been identified as a treatable trait of COPD.36 Blood eosinophil count could help predict the effect of ICS on lung function and exacerbation risk in patients with stable COPD.21 But there is still debate on using eosinophils to guide systemic corticosteroid treatment during exacerbations, and more clinical data is warranted.23,24 Systemic corticosteroids have been shown to improve lung function and reduce breathlessness in hospitalized AECOPD patients, and patients with a blood eosinophil percentage greater than 2% may be more sensitive to systemic corticosteroids.13 We observed an interaction between eosinophil and corticosteroid type on AECOPD treatment failure in a real-world setting, demonstrating a significantly lower risk of treatment failure in patients treated with systemic corticosteroids, but not those with no systemic corticosteroid treatment.
It can thus be suggested that eosinophilic AECOPD patients might benefit more from systemic corticosteroid treatment. Nevertheless, we found that eosinophilic patients were less likely to be treated with systemic corticosteroids than non-eosinophilic patients. It is possible that systemic corticosteroids are not currently prescribed in clinical practice in China based on blood eosinophil counts, but on the clinician’s experience and the severity of the patient’s symptoms. Previous studies have shown that non-eosinophilic patients tend to present more severe symptoms and, as a result, are more likely to receive systemic corticosteroid treatment.6 Despite recent studies suggesting that systemic corticosteroids may be less efficacious to treat AECOPD patients with lower levels of blood eosinophils,3,13,37 the eosinophil-guided systemic corticosteroids treatment is not yet recommended for routine clinical use due to the lack of evidence from large samples of prospective studies.
Eosinophilic inflammation may also be associated with short- and long-term risk of AECOPD readmissions. It has been shown that COPD patients with high eosinophil counts in stable phase tend to have more frequent exacerbations.14,38,39 But the predictive value of eosinophil levels at exacerbation period on AECOPD readmission risk remains controversial, especially for long-term readmission. Several studies reported no association between eosinophils and readmission rates for AECOPD.4,18,40,41 Inconsistent results were seen in another two studies, where eosinophilic AECOPD patients had an increased risk of COPD-related readmission or relapse.15,16 These studies were of a small sample size (<500) and had limited statistical power to analyze readmission rates. In our study of more than 2000 AECOPD inpatients, the association between blood eosinophils and risk of short-term readmission depended on corticosteroid treatment during hospitalization. The eosinophilic phenotype was associated with an increased risk of 30-day and 90-day readmission only in patients without systemic corticosteroid treatment. Accordingly, the use of only ICS might not be sufficient to prevent short-term readmission in patients with severe eosinophilic AECOPD. As a marker of disease severity and quality of care, short-term readmission is influenced by in-hospital treatment. It is possible that the interaction might partly explain the inconsistent results observed in previous studies regarding blood eosinophilic as a predictor of short-term readmissions, since the proportion of participants treated with systemic corticosteroids varied across different populations. When it comes to long-term AECOPD readmissions, a single eosinophil measurement at admission and in-hospital treatment is of less importance than the management of stable COPD. As expected, we found no significant difference in the 3-year readmission risk between the eosinophilic and non-eosinophilic groups. These findings suggest that blood eosinophils at exacerbation could help identify patients at high risk of short-term readmission with AECOPD, but might not predict long-term AECOPD readmission risk.
In addition to eosinophil count, several other inflammatory markers are involved in the diagnosis and treatment of AECOPD, including CRP, Procalcitonin (PCT), and white blood cell count. These biomarkers are typically employed to guide antibiotic therapy, representing a phenotype dominated by bacterial infection. Previous study showed that increased CRP was associated with adverse outcome of AECOPD.42 We found that AECOPD patients with higher blood eosinophils had lower CRP and white blood cell counts, and these eosinophilic patients had better outcomes if treated with systemic corticosteroids. Hence, a combination of blood eosinophils and infection biomarkers could potentially enhance phenotyping and individualized treatment of AECOPD. Pulmonary surfactant proteins are immune biomarkers that are also associated with COPD outcomes. A recent study suggested that surfactant protein B was a lung-specific prognostic biomarker in COPD.43 Dysregulation of surfactant proteins is associated with many eosinophilic lung diseases.44 Future studies are needed to elucidate the role of surfactant proteins in eosinophilic exacerbation of COPD.
The strengths of this study include the relatively large sample size, rigorous exclusion criteria, and various clinical outcomes. We included 2406 hospitalized AECOPD patients based on EMR data. Patients with comorbid asthma were excluded to avoid the potential confounding. We used database linkage to capture citywide readmission events and reduce the rate of loss to follow-up. The large number of cases enabled us to perform subgroup analyses by corticosteroid treatment. The findings contribute to a better understanding of the eosinophilic phenotype of AECOPD as well as the impact of systemic corticosteroid therapy on their prognosis.
There are also limitations of the study. First, we only analyzed the eosinophil count at admission, but the eosinophil count might change over time. Further studies with repeated measurements are needed to investigate the effect of persistent eosinophilic inflammation during exacerbation and stable periods. Second, COPD severity could not be determined because spirometry data was not available in this retrospective study. COPD severity is associated with the onset and prognosis of AECOPD. However, previous studies have demonstrated no difference in eosinophil levels across GOLD (Global Initiative for Chronic Obstructive Lung Disease) stages,45 indicating that COPD severity is not likely to be a confounder in our analysis. Third, data on corticosteroid use after discharge were not available, which might to some extent bias the association of blood eosinophils with the long-term prognosis of COPD patients. Fourth, a lack of relevant information prevented us from adjusting the use of regular anti-COPD medication prior to exacerbation onset. The association between eosinophils and outcome would be biased towards the null due to the potential misclassification of eosinophilic patients who used ICS before admission into the non-eosinophilic group, potentially lowering the risk in the non-eosinophilic group.
Conclusion
Blood eosinophils could be used as a biomarker to identify patients with higher risks of adverse hospitalization outcomes and short-term (30 and 90 days) readmission in AECOPD. Moreover, the prognostic value of blood eosinophils at admission is influenced by corticosteroid treatment during hospitalization. Higher blood eosinophils might indicate improved response to systemic corticosteroid treatment during exacerbations. Therefore, based on the real-world findings of this study, it’s crucial for clinicians to take into account not only the severity of the patient’s condition but also their blood eosinophil levels when prescribing systemic corticosteroids for AECOPD patients. This is particularly important as patients with higher eosinophil levels are more likely to benefit from systemic corticosteroid treatment.
Data Sharing Statement
The datasets used during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
This study was approved by the Research Ethics Board of Beijing Chaoyang Hospital (2020-ke-511). Informed consent was waived by the Research Ethics Board of Beijing Chaoyang Hospital (2020-ke-511) due to the retrospective nature of the study. Patient data was anonymized before analysis. All methods were carried out in accordance with the Declaration of Helsinki.
Funding
This work was supported by grants from the Beijing Municipal Science & Technology Commission (No. Z201100005520028, Z201100005520029), Beijing Key Specialists in Major Epidemic Prevention and Control, Financial Budgeting Project of Beijing Institute of Respiratory Medicine (Ysbz2023002), and Clinical Research Incubation Project, Beijing Chao-Yang Hospital, Capital Medical University (CYFH202210). The funder had no role in the study design, data collection, data analysis and interpretation, writing of the report, or the decision to submit the article for publication.
Disclosure
Professor Christopher E Brightling reports grants, personal fees from GSK, AZ, Chiesi, BI, Sanofi, Regeneron, Genentech, Roche, Mologic, Novartis, Areteia, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2022 Report). Available from: https://goldcopd.org/2022-gold-reports-2/.
2. Vogelmeier CF, Roman-Rodriguez M, Singh D, Han MK, Rodriguez-Roisin R, Ferguson GT. Goals of COPD treatment: focus on symptoms and exacerbations. Respir Med. 2020;166:105938.
3. Bafadhel M, McKenna S, Terry S, et al. Acute exacerbations of chronic obstructive pulmonary disease: identification of biologic clusters and their biomarkers. Am J Respir Crit Care Med. 2011;184(6):662–671.
4. Bafadhel M, Greening NJ, Harvey-Dunstan TC, et al. Blood Eosinophils and Outcomes in Severe Hospitalized Exacerbations of COPD. Chest. 2016;150(2):320–328.
5. Cui Y, Zhan Z, Zeng Z, et al. Blood Eosinophils and Clinical Outcomes in Patients With Acute Exacerbation of Chronic Obstructive Pulmonary Disease: a Propensity Score Matching Analysis of Real-World Data in China. Frontiers in Medicine. 2021;8:653777.
6. Jabarkhil A, Moberg M, Janner J, et al. Elevated blood eosinophils in acute COPD exacerbations: better short- and long-term prognosis. Eur Clin Respir J. 2020;7(1):1757274.
7. Ko FW, Chan KP, Ngai J, et al. Blood eosinophil count as a predictor of hospital length of stay in COPD exacerbations. Respirology. 2020;25(3):259–266.
8. Kolsum U, Donaldson GC, Singh R, et al. Blood and sputum eosinophils in COPD; relationship with bacterial load. Respir Res. 2017;18(1):88.
9. Choi J, Oh JY, Lee YS, et al. The association between blood eosinophil percent and bacterial infection in acute exacerbation of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2019;14:953–959.
10. Chen PK, Hsiao YH, Pan SW, Su KC, Perng DW, Ko HK. Independent factors associate with hospital mortality in patients with acute exacerbation of chronic obstructive pulmonary disease requiring intensive care unit admission: focusing on the eosinophil-to-neutrophil ratio. PLoS One. 2019;14(7):e0218932.
11. Pavord ID, Lettis S, Locantore N, et al. Blood eosinophils and inhaled corticosteroid/long-acting beta-2 agonist efficacy in COPD. Thorax. 2016;71(2):118–125.
12. Siddiqui SH, Guasconi A, Vestbo J, et al. Blood Eosinophils: a Biomarker of Response to Extrafine Beclomethasone/Formoterol in Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2015;192(4):523–525.
13. Bafadhel M, McKenna S, Terry S, et al. Blood eosinophils to direct corticosteroid treatment of exacerbations of chronic obstructive pulmonary disease: a randomized placebo-controlled trial. Am J Respir Crit Care Med. 2012;186(1):48–55.
14. Vedel-Krogh S, Nielsen SF, Lange P, Vestbo J, Nordestgaard BG. Blood Eosinophils and Exacerbations in Chronic Obstructive Pulmonary Disease. The Copenhagen General Population Study. Am J Respir Crit Care Med. 2016;193(9):965–974.
15. Couillard S, Larivee P, Courteau J, Vanasse A. Eosinophils in COPD Exacerbations Are Associated With Increased Readmissions. Chest. 2017;151(2):366–373.
16. Prins HJ, Duijkers R, Lutter R, et al. Blood eosinophilia as a marker of early and late treatment failure in severe acute exacerbations of COPD. Respir Med. 2017;131:118–124.
17. Hegewald MJ, Horne BD, Trudo F, et al. Blood Eosinophil Count and Hospital Readmission in Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease. Int J Chron Obstruct Pulmon Dis. 2020;15:2629–2641.
18. Csoma B, Bikov A, Toth F, Losonczy G, Muller V, Lazar Z. Blood eosinophils on hospital admission for COPD exacerbation do not predict the recurrence of moderate and severe relapses. ERJ Open Res. 2021;7(1):56.
19. Yu S, Zhang J, Fang Q, Tong Z. Blood Eosinophil Levels and Prognosis of Hospitalized Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease. Am J Med Sci. 2021;362(1):56–62.
20. Zhang J, Zheng J, Huang K, Chen Y, Yang J, Yao W. Use of glucocorticoids in patients with COPD exacerbations in China: a retrospective observational study. Ther Adv Respir Dis. 2018;12:1753466618769514.
21. Bafadhel M, Peterson S, De Blas MA, et al. Predictors of exacerbation risk and response to budesonide in patients with chronic obstructive pulmonary disease: a post-hoc analysis of three randomised trials. Lancet Respir Med. 2018;6(2):117–126.
22. Chronic Obstructive Pulmonary Disease Group of Chinese Thoracic Society, Chronic Obstructive Pulmonary Disease Committee of Chinese Association of Chest Physician. [Guidelines for the diagnosis and management of chronic obstructive pulmonary disease (revised version 2021)]. Zhonghua Jie He He Hu Xi Za Zhi. 2021;44(3):170–205. Chinese.
23. Camp J, Cane JL, Bafadhel M. Shall We Focus on the Eosinophil to Guide Treatment with Systemic Corticosteroids during Acute Exacerbations of COPD?: PRO. Med Sci. 2018;6(3):74.
24. Marcos PJ, López-Campos JL. Shall We Focus on the Eosinophil to Guide Treatment with Systemic Corticosteroids during Acute Exacerbations of Chronic Obstructive Pulmonary Disease (COPD)? CON. Med Sci. 2018;6(2):49.
25. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383.
26. Liang L, Li C, Shen Y, Rong H, Jing H, Tong Z. Long-Term Trends in Hospitalization and Outcomes in Adult Patients with Exacerbation of Chronic Obstructive Pulmonary Disease in Beijing, China, from 2008 to 2017. Int J Chron Obstruct Pulmon Dis. 2020;15:1155–1164.
27. Suehs CM, Zysman M, Chenivesse C, et al. Prioritising outcomes for evaluating eosinophil-guided corticosteroid therapy among patients with acute COPD exacerbations requiring hospitalisation: a Delphi consensus study. BMJ open. 2020;10(7):e035811.
28. Fine JP, Gray RJ. A Proportional Hazards Model for the Subdistribution of a Competing Risk. J Am Stat Assoc. 1999;94(446):496–509.
29. Kolsum U, Southworth T, Jackson N, Singh D. Blood eosinophil counts in COPD patients compared to controls. Eur Respir J. 2019;54(4):676.
30. Hartl S, Breyer MK, Burghuber OC, et al. Blood eosinophil count in the general population: typical values and potential confounders. Eur Respir J. 2020;55(5):89.
31. Bafadhel M, Pavord ID, Russell REK. Eosinophils in COPD: just another biomarker? Lancet Respir Med. 2017;5(9):747–759.
32. Brusselle G, Pavord ID, Landis S, et al. Blood eosinophil levels as a biomarker in COPD. Respir Med. 2018;138:21–31.
33. Singh D, Kolsum U, Brightling CE, et al. Eosinophilic inflammation in COPD: prevalence and clinical characteristics. Eur Respir J. 2014;44(6):1697–1700.
34. Tine M, Biondini D, Semenzato U, et al. Reassessing the Role of Eosinophils as a Biomarker in Chronic Obstructive Pulmonary Disease. J Clin Med. 2019;8(7):962.
35. Rushton J, Evans I, Carr S, et al. Impact of disease severity and comorbidities on length of stay (LOS) in COPD. Eur Respir J. 2016;48(suppl 60):A4157.
36. David B, Bafadhel M, Koenderman L, De Soyza A. Eosinophilic inflammation in COPD: from an inflammatory marker to a treatable trait. Thorax. 2021;76(2):188–195.
37. Sivapalan P, Lapperre TS, Janner J, et al. Eosinophil-guided corticosteroid therapy in patients admitted to hospital with COPD exacerbation (CORTICO-COP): a multicentre, randomised, controlled, open-label, non-inferiority trial. Lancet Respir Med. 2019;7(8):699–709.
38. Pascoe S, Locantore N, Dransfield MT, Barnes NC, Pavord ID. Blood eosinophil counts, exacerbations, and response to the addition of inhaled fluticasone furoate to vilanterol in patients with chronic obstructive pulmonary disease: a secondary analysis of data from two parallel randomised controlled trials. Lancet Respir Med. 2015;3(6):435–442.
39. Yun JH, Lamb A, Chase R, et al. Blood eosinophil count thresholds and exacerbations in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2018;141(6):2037–2047 e2010.
40. Greulich T, Tuffers J, Mager S, et al. High eosinophil blood counts are associated with a shorter length of hospital stay in exacerbated COPD patients - a retrospective analysis. Respir Res. 2020;21(1):106.
41. Thong L, O’Driscoll M, Casey C, et al. Eosinophils and COPD Readmission. Chest. 2017;151(3):724–725.
42. Duman D, Aksoy E, Agca MC, et al. The utility of inflammatory markers to predict readmissions and mortality in COPD cases with or without eosinophilia. Int J Chron Obstruct Pulmon Dis. 2015;10:2469–2478.
43. D’Ascanio M, Viccaro F, Pizzirusso D, et al. Surfactant Protein B Plasma Levels: reliability as a Biomarker in COPD Patients. Biomedicines. 2023;11(1):962.
44. Ledford JG, Addison KJ, Foster MW, Que LG. Eosinophil-associated lung diseases. A cry for surfactant proteins A and D help? Am J Respir Cell Mol Biol. 2014;51(5):604–614.
45. Song JH, Lee CH, Kim JW, et al. Clinical implications of blood eosinophil count in patients with non-asthma-COPD overlap syndrome COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:2455–2464.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.