Back to Journals » International Journal of General Medicine » Volume 17
The Prevalence of Hyperuricemia and the Association Between Hyperuricemia and Age in Patients with Psychiatric Disorders to a General Hospital: A Cross-Section Study
Authors Yang G, Zhou S, Feng Y, Lang J, Chen Y, Ren H
Received 13 December 2023
Accepted for publication 6 April 2024
Published 17 April 2024 Volume 2024:17 Pages 1467—1477
DOI https://doi.org/10.2147/IJGM.S454670
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Redoy Ranjan
Guodong Yang,1– 3 Shuang Zhou,4 Yue Feng,5 Jiaran Lang,1– 3 Yaxin Chen,1– 3 Huipeng Ren1– 3
1Mental Health Center, Hebei Medical University and Hebei Technical Innovation Center for Mental Health Assessment and Intervention, Shijiazhuang, Hebei, 050000, People’s Republic of China; 2The First Hospital of Hebei Medical University, Shijiazhuang, Hebei, 050000, People’s Republic of China; 3Department of Psychiatry, the First Hospital of Hebei Medical University, Shijiazhuang, Hebei, 050000, People’s Republic of China; 4The Sixth People’s Hospital of Hebei Province, Baoding, Hebei, 071000, People’s Republic of China; 5Maternity & Child Care Center of Qinhuangdao, Qinhuangdao, Hebei, 066000, People’s Republic of China
Correspondence: Huipeng Ren, The First Hospital of Hebei Medical University, 89 Donggang Road, Shijiazhuang, Hebei, 050000, People’s Republic of China, Email [email protected]
Purpose: In clinical work, it has been found that the prevalence of hyperuricemia (HUA) is significantly higher in younger patients with psychiatric disorders, but there are few studies in this area. The present study aims to evaluate the prevalence of HUA and the relationship between the HUA and age in hospitalized patients with psychiatric disorders in the real world, and to provide a theoretical basis for clinical staff to pay attention to the metabolic indicators of younger patients and for future related studies.
Methods: This is a cross-sectional evaluation of a cohort of 1761 patients with psychiatric disorders of hospitalized. The categories of disorders designed for study included: Depression, Bipolar disorder, Schizophrenia, Anxiety, Obsessive-Compulsive disorder, Acute and transient psychotic disorder, Dissociative(conversion) disorders, Conduct disorders and Tic disorders. In addition, based on age, the participants are stratified into three groups. The authors used Kruskal–Wallis tests, chi-square tests, and multiple linear logistic regression to verify the relationship between HUA and age among hospitalized patients with psychiatric disorders.
Results: Overall, the estimated prevalence of HUA was 35.4%. The prevalence of HUA was significantly higher in individuals with 17 years and under compared to those with 45 years and above (P < 0.001). After adjusting for confounders, the prevalence of HUA remained higher at 17 years and under than at 45 years and above. Bipolar disorder can lead to an increased prevalence of HUA (P< 0.05).
Conclusion: The prevalence of HUA was higher in hospitalized patients with psychiatric disorders, and the prevalence was inversely proportional to age.
Keywords: hyperuricemia, uric acid, age, psychiatric disorders, bipolar disorder
Introduction
Due to the rapid economic development, the lifestyle of most people has significantly changed, and their diet habit has gradually changed to a purine-rich food pattern.1 Unlike most mammals, human serum uric acid (SUA) becomes the end product of purine nucleotide metabolism due to the absence of uricase.2,3 Abnormal SUA metabolism can cause hyperuricemia (HUA) and gout. HUA is not only the pathological underlying cause of gout but is also an independent risk factor for obesity,4,5 hypertension,6,7 diabetes,8 dyslipidemia,9,10 liver dysfunction,11 kidney dysfunction,12 metabolic syndrome13 and cardiovascular disease.14
Purine metabolism can influence the activity of other neurotransmitters, including dopamine and gamma-aminobutyric acid (GABA) energy, which are involved in the pathophysiology of emotion-related diseases.15,16 Previous studies have shown that the purine system is associated with a variety of neuropsychiatric disorders,17 including disturbance of sleep,18 anhedonia,19 a drop in energy, cognitive impairment,20 and psychomotor agitation.21
The complex interactions between cognitive and affective processes and their underlying neurobiological underpinnings have been the focus of much research.22,23 Previous studies have shown that pituitary adenylate cyclase-activating polypeptides and vasoactive intestinal peptides play important roles in both metabolic and neurological diseases, so this may be the neural mechanism of the higher prevalence of hyperuricemia in psychiatric patients.24 In clinical work, it has been noted that the probability of detecting HUA in patients with psychiatric disorders is high. Still, it is unclear whether elevated uric acid is a risk factor, mediator, or marker of psychiatric disorders.
Several studies have confirmed that age independently predicts HUA development.25 However, there is no consensus on the effect of age on HUA. There has been less research about the effect of age on the prevalence of HUA in people with psychiatric disorders, especially in the real world, where data are lacking. Therefore, in this study, patients with psychiatric disorders were grouped by age to study the effect of age on the prevalence of hyperuricemia.
Materials and Methods
We conducted a cross-sectional study from March 2023 to November 2023. Subjects comprised 1761 patients with psychiatric disorders (665 males and 1096 females) admitted to the First Hospital of Hebei Medical University. All patients who met the inclusion criteria were hospitalized during this period and were recruited. This study reviewed the medical records of hospitalized patients with psychiatric disorders. Inclusion criteria: Chinese citizen and both genders and diagnosed with at least one psychiatric disorder according to the International Classification of Diseases 10 (ICD-10) diagnostic criteria, confirmed by two or more attending psychiatrists. Exclusion criteria:26 The patient who refused to receive a blood sample or missing blood sample results, was unable to communicate normally, had severe hepatic and renal insufficiency, severe cardiovascular and cerebrovascular diseases and any infectious diseases, a history of drug addiction and alcohol consumption, taking uric acid–lowering drugs, angiotensin-receptor blockers, or diuretics within 2 weeks before access, and pregnant or breastfeeding.
Ethics approval was obtained for the study from the ethics committee of The First Hospital of Hebei Medical University. Results were collected in an anonymous database. All methods were performed following the Declaration of Helsinki. Informed consent was obtained from all participants, and for patients who lack self-awareness or are below the age of 16, informed consent was obtained from their guardians.
Using standardized scales, we obtained general demographic, lifestyle, and medical history information. Besides, we also got the patient’s age, sex, smoking history, alcohol history, previous disease history, medication, and recent diet. A uniform standard method measured blood pressure, height, and weight upon admission.23 It was recorded by two different doctors, then checked by a third doctor who found different data and checked again. Register the above information of the patients. The BMI was calculated using the weight (kg)/height2 (m2) formula.
Fasting blood samples were collected from the participants by venipuncture after overnight fasting (8–12 hours) on the second day of admission. Blood samples were collected in the morning from 7:00 am to 8:00 am. Blood samples were sent to the hospital laboratory department for blood sample analysis within 1 hour. Triglyceride (TG), Total cholesterol (TC), High-density lipoprotein cholesterol (HDL-C), Creatinine (Cr), platelets, and SUA were measured by the biochemical automatic analyzer. The measurement accuracy is maintained regularly through method standard calibration. Trained professionals performed all laboratory tests.
Definitions: In the present study, hyperuricemia was defined as SUA>7.0 mg/dL (420.0mol/L) in men and SUA> 6.0 mg/dL (357.0 mol/L) in women.27,28 Hypertension was defined by SBP ≥ 140 mm Hg and/or DBP ≥ 90 mm Hg or intake of anti-hypertensive drugs during data collection.29 According to the WHO’s latest age classification standards for developing countries, we categorized age into three groups: 17 years and under, 18–44 years old, 45 years and above.
We tested the continuous variables’ distribution of, with none agreeing with normal distribution. We displayed continuous variables as the median (interquartile range) and categorical variables as numbers and percentages. Kruskal–Wallis and chi-square tests estimated participants’ differences in biochemical and clinical features for constant and categorical variants, respectively. The association between the HUA and age was tested using multivariable logistic regression models, with odds ratios (ORs) and 95% confidence intervals (CIs) calculated. General additive models were applied to obtain a smoothing curve and identify any non-linear association between SUA and age. All statistical analyses were performed using IBM SPSS Statistics 25.0 software (IBM SPSS, Chicago, IL), EmpowerStats Software (Inc., Boston, MA) and GraphPad Prism version 8.0.1 for Windows (GraphPad Software, San Diego). Two-sided P values under 0.05 for hypothesis tests were regarded as statistically significant.
Results
Clinical and Biochemical Characteristics of the Participants
The specific diagnosis and screening process is shown (Figure 1). A total of 1761 subjects were analyzed in this study, of which 665 were male and 1096 were female. We summarized the participants’ basic and biochemical features of the study (Table 1). Overall, the estimated prevalence of HUA was 35.4%. The highest prevalence of HUA was in group 17 years and under, and the lowest in group 45 years and above (P<0.001). Body mass index (BMI), systolic blood pressure (SBP), diastolic blood pressure (DBP), triglyceride (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), alanine aminotransferase (ALT) increased with age (P<0.05). There were no differences in HDL-C in the three groups (P>0.05). There was no significant difference in the prevalence of HUA between the 17 years and under group and the 18–44 years old group (P=0.661) (Figure 2A).
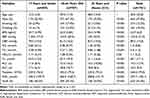 |
Table 1 Baseline Characteristics of the Participants by Age Groups (n = 1761) |
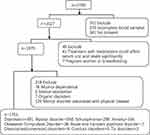 |
Figure 1 Participant selection process and specific diagnosis. |
 |
Figure 2 (A) Prevalence of hyperuricemia by age. (B) Prevalence of hyperuricemia by gender and age. |
Clinical and Biochemical Characteristics of the Participants Grouped by Gender
In both men and women, subjects in the 17 years and under group had the highest prevalence of HUA, but there was no significant difference in females (P=0.088). BMI, SBP, DBP, TG, and TC increased with age (P<0.05). There were no differences in HDL-C in the three groups (P>0.05) (Table 2). The male prevalence rate was higher than that of females in the 17 years and under group and the 18–44 years old group. However, the male prevalence rate was lower than that of females in the 45 years and above group (Figure 2B).
 |
Table 2 Characteristics of the Participants According to Gender and Age Groups (n = 1761) |
Multinomial Logistic Regression Analysis to Evaluate the Association Between HUA and Age
In regression analysis, the relationship between HUA and age in the three models was analyzed. The prevalence of HUA was associated with age, except that there was no statistical significance in group 18–44 years old of female patients in Model A, and the prevalence was negatively correlated with age. After adjusting for mixing factors, the association between the prevalence of HUA and age was strengthened (Table 3). Due to the interaction between the various drugs, only antipsychotics taken in a single were chosen. 1469 patients were taking antipsychotics, and 987 were on one medication. The most commonly used antipsychotics, including quetiapine, olanzapine, risperidone, and aripiprazole, had no effect on the prevalence of HUA (P>0.05). Bipolar disorder (BD) had a statistically significant effect on the prevalence of HUA (P<0.05).
 |
Table 3 Relationship Between Hyperuricemia and Age |
SUA is Non-Linear Related to Age
Because the 18–44 years old group has the highest SUA levels, general additive models were adopted to show whether a non-linear relationship existed between SUA and age. A smoothing curve indicated a non-linear correlation in the additive model, indicating two stages of change between SUA and age (Figure 3A) was found. SUA increases first and then decreases with age. The scatter plot shows the distribution of SUA and age (Figure 3B).
 |
Figure 3 (A) The curve fitting line for SUA and age. (B) Scatter plot of the distribution for SUA and age. |
Discussion
It is the first study of all patients with psychiatric disorders in a general hospital. In our study, we found that the prevalence of HUA was higher in hospitalized patients with psychiatric disorders than in the general population; subjects in the 17 years and under group were at a higher risk of HUA than those in the other two groups. Subjects in the 17 years and under group were 8.38-fold more likely to have HUA than those 45 years and above. The main finding of this current study was that age was indicated as an essential correlation factor of HUA for both genders in hospitalized patients with psychiatric disorders. The study aims to provide data support for the relationship between HUA and age.
In this study, the results showed that the prevalence of HUA in hospitalized patients with psychiatric disorders was 35.4% (male:41.8%, female:31.5%). An Italian study showed the prevalence of hyperuricemia in BD was 30.7%, the overall prevalence of HUA in Obsessive–Compulsive Disorder, Major Depressive Disorder (MDD) and Schizophrenia (SZ) was 6.7%.30 In a French study, the prevalence of HUA in patients with schizophrenia was 19.6%.31 The prevalence of HUA is also higher in the younger group than in the others. The same is true for results grouped by gender. These data implied that age is a protective factor for HUA, consistent with the previous findings.32,33 Therefore, we should pay more attention to the influence of SUA to prevent the occurrence of HUA, especially in patients with psychiatric disorders at a young age.
In line with the previous findings, the prevalence of HUA was higher in males than in females.34 It may be the effect of estrogen that causes lower uric acid levels in women.35 As women get older, estrogen levels decline, affecting the renal tubule’s reabsorption of SUA, which leads to increased excretion of SUA.36 Also, hormone replacement therapy is effective in reducing SUA, which confirms the viewpoint above.37 That is because low levels or inadequate function of steroid hormones may lead to weight gain and abnormal glucose metabolism in postmenopausal women, which may affect the level of SUA.38 In our study, we found that in the elderly group, females had a higher prevalence of HUA than males, further confirming the hypothesis that estrogen can reduce uric acid.
The potential reasons for the higher prevalence of HUA in the younger age could be explained as that the age range is wide; few studies have involved people under the age of 18. Other possible causes include Inflammation, the type of disease, dietary pattern, ethnicity, lifestyle, and comorbidities. Previous studies demonstrated a positive correlation between hyperthymic and irritable temperament scores and the SUA level,39 particularly for impulsivity and excitement-seeking behaviors.40 Impulsivity and excitement-seeking behavior are more common in younger people with BD. In a study of French children, SUA levels were correlated positively with hyperactivity, impulsivity, and anger control.41 In addition, genetic factors have a significant influence on SUA. It was reported that 60% of the variation in SUA level can be explained by genetic factors.42 There is evidence of a significant relationship between SUA and attention-deficit hyperactivity disorder at the genetic level.43
SUA is the end product of purine metabolism; impaired purine metabolism can increase the SUA, resulting in HUA. It not only causes gout, but also can be considered one of the risk factors for diabetes, kidney diseases, cardiovascular diseases and others.44 Uric acid also drives a canonical inflammatory response and may act as an endogenous adjuvant that directs immune activities.45 HUA has been implicated in the initiation of urate crystal formation. The existing body of evidence strongly indicates that urates significantly promote inflammation.46 The occurrence of urate crystals in HUA primarily triggers gout attacks by activating monocytes and macrophages, inducing the production of nucleotide oligomerization domain-like receptor protein (NLRP) 3 inflammatory vesicles, which in turn release interleukin (IL)-1β. Additionally, this process elicits numerous local and systemic pro-inflammatory responses, along with the influx and activation of neutrophils in the affected joints.47 Consistent with the findings of urate crystals, soluble uric acid salts also promote inflammation through the same pathway.48 SUA may function as an alarmin, triggering the activation of the NLRP3 inflammasome and potentially enhancing nuclear factor-κB activity, oxidative stress, and inflammatory stress.49 A positive correlation exists between elevated SUA levels and various pro-inflammatory markers, including C-reactive protein, white blood cell count, interleukin-6, interleukin-17, and TNF-α.50 Chronic peripheral inflammation, as indicated by the presence of tumor necrosis factor-alpha (TNF-α) and other pro-inflammatory cytokines (PICs), significantly contributes to the pathophysiology of SZ, BD, and MDD.
Australia, the United Kingdom, Spanish, and other countries have found that unhealthy diets among adolescents were associated with an increased prevalence of common psychiatric disorders such as depression.51,52 An unhealthy diet is excessive consumption of alcohol and purine-rich foods (such as red meat, seafood, some vegetables, and animal proteins). These foods can increase the risk of HUA.53 Unhealthy diets among children during the last decades have resulted in an increasing prevalence of risk factors for chronic diseases, such as obesity, high blood pressure and high cholesterol levels in children.54 Unfortunately, previous studies have shown that the vast majority of adolescent actually have an unhealthy diet.55 The prevalence of metabolic syndrome in adolescents is on the rise in many countries.56 Abnormal SUA levels have been associated with various psychiatric disorders, such as depression, schizophrenia, and bipolar disorder.50 So, one possible reason for high SUA in younger people is unhealthy diet patterns. Interestingly, the frequency of eating spicy food and the extent of pungency were positively associated with HUA. Compared with people who never consumed spicy food, those who ate them frequently were more likely in younger man group.57
Psychotropic medications can affect biochemical markers of patients, such as SUA, BMI, and TG(Triglyceride).58,59 The most explicit thing was the use of antipsychotics, especially atypical antipsychotics.60 The metabolic side effects of antipsychotic drugs in the clinical population are now well established.61 Norepinephrine, epinephrine and catecholamine are hormones that are very important in the regulation of many metabolic processes. These hormones have been shown to play an essential role in the metabolic side effects of antipsychotics, both in human and animal studies,62,63 which revealed a dose-dependent increase in rodent models.64 The strong affinity of antipsychotics for 5-HT2C and H1 receptors is considered the primary cause of weight gain.65 Besides, metabolic dysfunction is associated with higher insulin resistance and leptin production, both of which could significantly impact the SUA secretion system, resulting in an elevated level of SUA.66 This study showed that antipsychotics had no significant effect on the prevalence of hyperuricemia. Our results are consistent with the meta-analysis from 2022.50 We should be aware that SUA disturbances may not only be a consequence of the disease and aforementioned antipsychotics, but also be a consequence of smoking, dietary patterns, metabolic abnormalities or other reasons that are not yet clear.
Different types of diseases also affect the prevalence of HUA. In recent years, a large number of studies have found that the level of UA in peripheral blood of BD patients is significantly higher than that of other psychiatric patients and normal people. Previous articles have shown that oxidative stress might be of importance in the pathophysiology of BD.14 Elevated SUA has been associated with mood-related disorders. Previous studies have found that the level of SUA in patients with depression and anxiety was lower than that in normal control; and the severity and duration of symptoms were negatively associated with uric acid.67,68 There are no clear results on uric acid levels in patients with schizophrenia, but studies have shown a positive correlation between uric acid and cognitive function.69 Even in the absence of a psychiatric diagnosis, elevated UA levels are associated with specific manic characteristics such as impulsivity, irritability, increased drive, and hyperthymia.70 BD patients exhibit elevated central and peripheral pro-inflammatory factors (cytokines, chemokines, acute phase reactants, oxidation/nitride substances), increased expression of inflammatory genes, and abnormal activation of cells (t cells, monocytes, microglia) and complement.71 Because SUA levels are elevated in people with bipolar disorder, higher SUA is predictive of bipolar conversion in people with current depression.72 In addition, purines may be associated with behavioral changes typical of people with BD,73 such as passivity, reduced activity, altered sleep rhythms, overeating aggressive behavior, and social interaction.74 More factors may have yet to be discovered and need further research.
Study limitations and strengths: Firstly, the cross-sectional nature of the data does not demonstrate a causal relationship between HUA and age. Second, although extensive adjustments were made in our study, unmeasured confounding factors such as dietary habits, physical activity levels, socioeconomic status, and comorbidities may influence the results, and as many influencing factors as possible should be excluded in subsequent studies. Due to the existence of recall bias in the drugs applied to patients before admission and the interaction between various drugs, we only analyzed participants who were taking a single antipsychotic, not thoroughly analyzed to determine whether there were differences in drug doses and types between the HUA and non-HUA treatment groups. Thirdly, because we want to analyze the situation of psychiatric disorder patients in the whole hospital, we analyze most diseases, and the classification of diseases is not very strict. Fourthly, our subjects are hospitalized patients, and we excluded outpatients. Therefore, it may not apply to all people with psychiatric disorders. However, the strengths of this study are its population-based design, large sample size, and the study of the real world. Our study can provide strong evidence of an association between the age and HUA. It has been observed that age could affect SUA. However, the underlying mechanism of increased SUA in younger patients remains to be explored. In the future, more research is needed to determine the mechanisms underlying the association between HUA and age in psychiatric disorders.
Conclusion
In conclusion, our study observed significant associations between HUA and age in this cross-sectional study. We mainly showed that younger patients were associated with an increased risk of HUA. The prevalence of HUA in psychiatric disorders was 35.4%. Especially in the 17 years and under group, the prevalence reached 40.5%. Therefore, we should pay attention to SUA during treatment and recommend that patients maintain a healthy diet and living habits.
Data Sharing Statement
The data presented in this study are available on request from the corresponding author.
Ethics Approval and Informed Consent
The study was conducted in accordance with the Declaration of Helsinki, and approved by the ethics committee of The First Hospital of Hebei Medical University (protocol code S00112 and date of 2023-03). for studies involving humans. Results were collected in an anonymous database. Informed consent was obtained from all subjects involved in the study. For patients who lack self-awareness or are below 16, informed consent was obtained from their guardians.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Project of Hebei Provincial Finance Department (LNB202016) and Hebei Provincial Department of Science and Technology (21377712D).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Zhai F-Y, He Y-N, Ma G-S, et al. [Study on the current status and trend of food consumption among Chinese population]. Zhonghua Liu Xing Bing Xue Za Zhi. 2005;26(7):485–488. Chinese.
2. Li M, Hou W, Zhang X, Hu L, Tang Z. Hyperuricemia and risk of stroke: a systematic review and meta-analysis of prospective studies. Atherosclerosis. 2014;232(2):265–270. doi:10.1016/j.atherosclerosis.2013.11.051
3. Heinig M, Johnson RJ. Role of uric acid in hypertension, renal disease, and metabolic syndrome. Cleve Clin J Med. 2006;73(12):1059–1064. doi:10.3949/ccjm.73.12.1059
4. You A, Li Y, Shen C, et al. Associations of non-traditional cardiovascular risk factors and body mass index with metabolic syndrome in the Chinese elderly population. Diabetol Metab Syndr. 2023;15(1):129.
5. Ali N, Perveen R, Rahman S, et al. Prevalence of hyperuricemia and the relationship between serum uric acid and obesity: a study on Bangladeshi adults. PLoS One. 2018;13(11):e0206850. doi:10.1371/journal.pone.0206850
6. Ali N, Mahmood S, Islam F, et al. Relationship between serum uric acid and hypertension: a cross-sectional study in Bangladeshi adults. Sci Rep. 2019;9(1):9061. doi:10.1038/s41598-019-45680-4
7. Long T, Liu L. Research progress on the relationship between dietary patterns and hyperuricemia. Appl Bionics Biomech. 2022;2022:5658423. doi:10.1155/2022/5658423
8. Haque T, Rahman S, Islam S, Molla NH, Ali N. Assessment of the relationship between serum uric acid and glucose levels in healthy, prediabetic and diabetic individuals. Diabetol Metab Syndr. 2019;11:49. doi:10.1186/s13098-019-0446-6
9. Chen S, Yang H, Chen Y, et al. Association between serum uric acid levels and dyslipidemia in Chinese adults: a cross-sectional study and further meta-analysis. Medicine. 2020;99(11):e19088. doi:10.1097/MD.0000000000019088
10. Ali N, Rahman S, Islam S, et al. The relationship between serum uric acid and lipid profile in Bangladeshi adults. BMC Cardiovasc Disord. 2019;19(1):42. doi:10.1186/s12872-019-1026-2
11. Molla NH, Kathak RR, Sumon AH, et al. Assessment of the relationship between serum uric acid levels and liver enzymes activity in Bangladeshi adults. Sci Rep. 2021;11(1):20114. doi:10.1038/s41598-021-99623-z
12. Barman Z, Hasan M, Miah R, et al. Association between hyperuricemia and chronic kidney disease: a cross-sectional study in Bangladeshi adults. BMC Endocr Disord. 2023;23(1):45. doi:10.1186/s12902-023-01304-7
13. Ali N, Miah R, Hasan M, et al. Association between serum uric acid and metabolic syndrome: a cross-sectional study in Bangladeshi adults. Sci Rep. 2020;10(1):7841. doi:10.1038/s41598-020-64884-7
14. Burnier M. Gout and hyperuricaemia: modifiable cardiovascular risk factors? Front Cardiovasc Med. 2023;10:1190069. doi:10.3389/fcvm.2023.1190069
15. Machado-Vieira R, Lara DR, Souza DO, Kapczinski F. Purinergic dysfunction in mania: an integrative model. Med Hypotheses. 2002;58(4):297–304. doi:10.1054/mehy.2001.1543
16. Tanaka M, Szabó Á, Vécsei L, Giménez-Llort L. Emerging translational research in neurological and psychiatric diseases: from in vitro to in vivo models. Int J Mol Sci. 2023;24:21. doi:10.3390/ijms242115739
17. Abbracchio MP, Burnstock G, Verkhratsky A, Zimmermann H. Purinergic signalling in the nervous system: an overview. Trends Neurosci. 2009;32(1):19–29. doi:10.1016/j.tins.2008.10.001
18. Huang ZL, Urade Y, Hayaishi O. The role of adenosine in the regulation of sleep. Curr Top Med Chem. 2011;11(8):1047–1057. doi:10.2174/156802611795347654
19. Csölle C, Baranyi M, Zsilla G, et al. Neurochemical changes in the mouse hippocampus underlying the antidepressant effect of genetic deletion of P2X7 receptors. PLoS One. 2013;8(6):e66547. doi:10.1371/journal.pone.0066547
20. Salamone JD, Correa M. Dopamine/adenosine interactions involved in effort-related aspects of food motivation. Appetite. 2009;53(3):422–425. doi:10.1016/j.appet.2009.07.018
21. Wei CJ, Li W, Chen JF. Normal and abnormal functions of adenosine receptors in the central nervous system revealed by genetic knockout studies. Biochim Biophys Acta. 2011;1808(5):1358–1379. doi:10.1016/j.bbamem.2010.12.018
22. Battaglia S, Di Fazio C, Mazzà M, Tamietto M, Avenanti A. Targeting human glucocorticoid receptors in fear learning: a multiscale integrated approach to study functional connectivity. Int J Mol Sci. 2024;25:2. doi:10.3390/ijms25020864
23. Di Gregorio F, Steinhauser M, Maier ME, Thayer JF, Battaglia S. Error-related cardiac deceleration: functional interplay between error-related brain activity and autonomic nervous system in performance monitoring. Neurosci Biobehav Rev. 2024;157:105542. doi:10.1016/j.neubiorev.2024.105542
24. Tanaka M, Szabó Á, Körtési T, Szok D, Tajti J, Vécsei L. From CGRP to PACAP, VIP, and beyond: unraveling the next chapters in migraine treatment. Cells. 2023;12:22. doi:10.3390/cells12222649
25. Qu X, Zheng L, Zu B, Jia B, Lin W. Prevalence and clinical predictors of hyperuricemia in Chinese bariatric surgery patients. Obes Surg. 2022;32(5):1508–1515. doi:10.1007/s11695-021-05852-6
26. Chen J, Chen H, Feng J, et al. Association between hyperuricemia and metabolic syndrome in patients suffering from bipolar disorder. BMC Psychiatry. 2018;18(1):390. doi:10.1186/s12888-018-1952-z
27. Lee JW, Kwon BC, Choi HG. Analyses of the relationship between hyperuricemia and osteoporosis. Sci Rep. 2021;11(1):12080. doi:10.1038/s41598-021-91570-z
28. Liu R, Han C, Wu D, et al. Prevalence of hyperuricemia and gout in mainland China from 2000 to 2014: a systematic review and meta-analysis. Biomed Res Int. 2015;2015:762820. doi:10.1155/2015/762820
29. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–1252. doi:10.1161/01.HYP.0000107251.49515.c2
30. Albert U, De Cori D, Aguglia A, Barbaro F, Bogetto F, Maina G. Increased uric acid levels in bipolar disorder subjects during different phases of illness. J Affect Disord. 2015;173:170–175. doi:10.1016/j.jad.2014.11.005
31. Godin O, Leboyer M, Gaman A, et al. Metabolic syndrome, abdominal obesity and hyperuricemia in schizophrenia: results from the FACE-SZ cohort. Schizophr Res. 2015;168(1–2):388–394. doi:10.1016/j.schres.2015.07.047
32. Gephardt MC, Hanlon TJ, Matson CF. Blood uric acid values as related to sex and age. JAMA. 1964;189:1028–1029. doi:10.1001/jama.1964.03070130048019
33. Zeng J, Lawrence WR, Yang J, et al. Association between serum uric acid and obesity in Chinese adults: a 9-year longitudinal data analysis. BMJ Open. 2021;11(2):e041919. doi:10.1136/bmjopen-2020-041919
34. Ting K, Gill TK, Keen H, Tucker GR, Hill CL. Prevalence and associations of gout and hyperuricaemia: results from an Australian population-based study. Intern Med J. 2016;46(5):566–573. doi:10.1111/imj.13006
35. Guan S, Tang Z, Fang X, et al. Prevalence of hyperuricemia among Beijing post-menopausal women in 10 years. Arch Gerontol Geriatr. 2016;64:162–166. doi:10.1016/j.archger.2016.02.002
36. Yahyaoui R, Esteva I, Haro-Mora JJ, et al. Effect of long-term administration of cross-sex hormone therapy on serum and urinary uric acid in transsexual persons. J Clin Endocrinol Metab. 2008;93(6):2230–2233. doi:10.1210/jc.2007-2467
37. Sumino H, Ichikawa S, Kanda T, Nakamura T, Sakamaki T. Reduction of serum uric acid by hormone replacement therapy in postmenopausal women with hyperuricaemia. Lancet. 1999;354(9179):650. doi:10.1016/S0140-6736(99)92381-4
38. Varlamov O, Bethea CL, Roberts CT. Sex-specific differences in lipid and glucose metabolism. Front Endocrinol. 2014;5:241. doi:10.3389/fendo.2014.00241
39. Karam EG, Saab D, Jabbour S, Karam GE, Hantouche E, Angst J. The role of affective temperaments in bipolar disorder: the solid role of the cyclothymic, the contentious role of the hyperthymic, and the neglected role of the irritable temperaments. Eur Psychiatry. 2023;66(1):e37. doi:10.1192/j.eurpsy.2023.16
40. Sutin AR, Cutler RG, Camandola S, et al. Impulsivity is associated with uric acid: evidence from humans and mice. Biol Psychiatry. 2014;75(1):31–37. doi:10.1016/j.biopsych.2013.02.024
41. Barrera CM, Ruiz ZR, Dunlap WP. Uric acid: a participating factor in the symptoms of hyperactivity. Biol Psychiatry. 1988;24(3):344–347. doi:10.1016/0006-3223(88)90205-3
42. Richette P, Bardin T. Gout. Lancet. 2010;375(9711):318–328. doi:10.1016/S0140-6736(09)60883-7
43. Kafle OP, Wang X, Cheng S, et al. Genetic correlation analysis and transcriptome-wide association study suggest the overlapped genetic mechanism between gout and attention-deficit hyperactivity disorder. Can J Psychiatry. 2021;66(12):1077–1084. doi:10.1177/0706743720970844
44. Barbieri L, Verdoia M, Pergolini P, et al. Uric acid and high-residual platelet reactivity in patients treated with clopidogrel or ticagrelor. Nutr, Metab Cardiovasc Dis. 2016;26(4):352–358. doi:10.1016/j.numecd.2015.12.015
45. Ghaemi-Oskouie F, Shi Y. The role of uric acid as an endogenous danger signal in immunity and inflammation. Curr Rheumatol Rep. 2011;13(2):160–166. doi:10.1007/s11926-011-0162-1
46. Mei Y, Dong B, Geng Z, Xu L. Excess uric acid induces gouty nephropathy through crystal formation: a review of recent insights. Front Endocrinol. 2022;13:911968. doi:10.3389/fendo.2022.911968
47. Stamp LK, Farquhar H, Pisaniello HL, et al. Management of gout in chronic kidney disease: a G-CAN Consensus Statement on the research priorities. Nat Rev Rheumatol. 2021;17(10):633–641. doi:10.1038/s41584-021-00657-4
48. Braga TT, Forni MF, Correa-Costa M, et al. Soluble Uric Acid Activates the NLRP3 Inflammasome. Sci Rep. 2017;7:39884. doi:10.1038/srep39884
49. Morris G, Puri BK, Olive L, et al. Endothelial dysfunction in neuroprogressive disorders-causes and suggested treatments. BMC Med. 2020;18(1):305. doi:10.1186/s12916-020-01749-w
50. Borovcanin MM, Janicijevic SM, Mijailovic NR, et al. Uric acid potential role in systemic inflammation and negative symptoms after acute antipsychotic treatment in schizophrenia. Front Psychiatry. 2021;12:822579. doi:10.3389/fpsyt.2021.822579
51. Wang Y, Liu J, Compher C, Kral TVE. Associations between dietary intake, diet quality and depressive symptoms in youth: a systematic review of observational studies. Health Promot Perspect. 2022;12(3):249–265. doi:10.34172/hpp.2022.32
52. Alfaro-González S, Garrido-Miguel M, Martínez-Vizcaíno V, López-Gil JF. Mediterranean dietary pattern and psychosocial health problems in Spanish adolescents: the EHDLA study. Nutrients. 2023;15:13. doi:10.3390/nu15132905
53. Choi HK, Liu S, Curhan G. Intake of purine-rich foods, protein, and dairy products and relationship to serum levels of uric acid: the third national health and nutrition examination survey. Arthritis Rheum. 2005;52(1):283–289. doi:10.1002/art.20761
54. Song P, Zhang Y, Yu J, et al. Global prevalence of hypertension in children: a systematic review and meta-analysis. JAMA Pediatr. 2019;173(12):1154–1163. doi:10.1001/jamapediatrics.2019.3310
55. Kourlaba G, Kondaki K, Grammatikaki E, Roma-Giannikou E, Manios Y. Diet quality of preschool children and maternal perceptions/misperceptions: the GENESIS study. Public Health. 2009;123(11):738–742. doi:10.1016/j.puhe.2009.10.005
56. Chen ZY, Liu L, Zhuang XX, et al. Lipid accumulation product is a better predictor of metabolic syndrome in Chinese adolescents: a cross-sectional study. Front Endocrinol. 2023;14:1179990. doi:10.3389/fendo.2023.1179990
57. Luo Q, Ding R, Chen L, et al. The association between spicy food intake and risk of hyperuricemia among Chinese adults. Front Public Health. 2022;10:919347. doi:10.3389/fpubh.2022.919347
58. Kryzhanovskaya L, Schulz SC, McDougle C, et al. Olanzapine versus placebo in adolescents with schizophrenia: a 6-week, randomized, double-blind, placebo-controlled trial. J Am Acad Child Adolesc Psychiatry. 2009;48(1):60–70. doi:10.1097/CHI.0b013e3181900404
59. Solmi M, Fornaro M, Ostinelli EG, et al. Safety of 80 antidepressants, antipsychotics, anti-attention-deficit/hyperactivity medications and mood stabilizers in children and adolescents with psychiatric disorders: a large scale systematic meta-review of 78 adverse effects. World Psychiatry. 2020;19(2):214–232. doi:10.1002/wps.20765
60. Wu Q, Zhang X, Liu Y, Wang Y. Prevalence and risk factors of comorbid obesity in Chinese patients with bipolar disorder. Diabetes Metab Syndr Obes. 2023;16:1459–1469. doi:10.2147/DMSO.S404127
61. Yuen JWY, Kim DD, Procyshyn RM, et al. A focused review of the metabolic side-effects of clozapine. Front Endocrinol. 2021;12:609240. doi:10.3389/fendo.2021.609240
62. Boyda HN, Ho AA, Tse L, et al. Differential effects of acute treatment with antipsychotic drugs on peripheral catecholamines. Front Psychiatry. 2020;11:617428. doi:10.3389/fpsyt.2020.617428
63. Ashraf GM, Alghamdi BS, Alshehri FS, et al. Empagliflozin effectively attenuates olanzapine-induced body weight gain in female Wistar rats. Front Pharmacol. 2021;12:578716. doi:10.3389/fphar.2021.578716
64. Boyda HN, Pham M, Huang J, et al. Antipsychotic drug-induced increases in peripheral catecholamines are associated with glucose intolerance. Front Pharmacol. 2022;13:765905. doi:10.3389/fphar.2022.765905
65. Agarwal SM, Stogios N, Ahsan ZA, et al. Pharmacological interventions for prevention of weight gain in people with schizophrenia. Cochrane Database Syst Rev. 2022;10(10):Cd013337. doi:10.1002/14651858.CD013337.pub2
66. Li S, Lu X, Chen X, et al. The prevalence and associated clinical correlates of hyperuricemia in patients with bipolar disorder. Front Neurosci. 2022;16:998747. doi:10.3389/fnins.2022.998747
67. Meng X, Huang X, Deng W, Li J, Li T. Serum uric acid a depression biomarker. PLoS One. 2020;15(3):e0229626. doi:10.1371/journal.pone.0229626
68. Black CN, Bot M, Scheffer PG, Snieder H, Penninx B. Uric acid in major depressive and anxiety disorders. J Affect Disord. 2018;225:684–690. doi:10.1016/j.jad.2017.09.003
69. Yuan Z, Liu H, Zhang X, et al. Role of uric acid as a biomarker of cognitive function in schizophrenia during maintenance period. Front Psychiatry. 2023;14:1123127. doi:10.3389/fpsyt.2023.1123127
70. Lorenzi TM, Borba DL, Dutra G, Lara DR. Association of serum uric acid levels with emotional and affective temperaments. J Affect Disord. 2010;121(1–2):161–164. doi:10.1016/j.jad.2009.05.023
71. SayuriYamagata A, Brietzke E, Rosenblat JD, Kakar R, McIntyre RS. Medical comorbidity in bipolar disorder: the link with metabolic-inflammatory systems. J Affect Disord. 2017;211:99–106. doi:10.1016/j.jad.2016.12.059
72. Dos Santos Oliveira PM, Santos V, Coroa M, Ribeiro J, Madeira N. Serum uric acid as a predictor of bipolarity in individuals with a major depressive episode. Bipolar Disord. 2019;21(3):235–243. doi:10.1111/bdi.12708
73. Bonnín CDM, Reinares M, Martínez-Arán A, et al. Improving functioning, quality of life, and well-being in patients with bipolar disorder. Int J Neuropsychopharmacol. 2019;22(8):467–477. doi:10.1093/ijnp/pyz018
74. Li S, Lu X, Qiu Y, et al. Association between uric acid and cognitive dysfunction: a cross-sectional study with newly diagnosed, drug-naïve with bipolar disorder. J Affect Disord. 2023;327:159–166. doi:10.1016/j.jad.2023.01.105
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
