Back to Journals » Nursing: Research and Reviews » Volume 12
The Preterm Birth Rate in a Resource-Stricken Rural Area of the Limpopo Province, South Africa
Authors Malwela T , Maputle MS
Received 7 September 2021
Accepted for publication 18 February 2022
Published 15 April 2022 Volume 2022:12 Pages 67—75
DOI https://doi.org/10.2147/NRR.S338161
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Natasha Hodgkinson
Thivhulawi Malwela, Maria Sonto Maputle
Department of Advanced Nursing, University of Venda Thohoyandou, Limpopo, South Africa
Correspondence: Thivhulawi Malwela, University of Venda, Private Bag X 5050, Limpopo, 0950, South Africa, Tel +27159628840, Email [email protected]
Background: Midwives play a pivotal role in providing primary prevention of preterm birth. Midwives screen and diagnose pre-existing medical conditions, manage all conditions as guided by their scope of practice and refer all cases to other relevant team members.
Purpose: The study aimed to determine and describe factors contributing to the escalating preterm birth rate in Limpopo, South Africa.
Methods: Descriptive survey was used to determine factors related to increased preterm births. The non-probability purposive sampling selected 55 midwives, and data were collected using self-administered questionnaires. Data were analyzed through SPSS version 23.
Results: Health facilities in Limpopo province had constrained resources as evidenced by a shortage of midwives, a lack of medical supply, poorly maintained, and old infrastructure. The skills of midwives and their working environment were affected by this constrained resource. The results from midwives that were perceived to affect them were 66% of participants reported lack of equipment, 29.1% participants agreed that pregnant women were presenting after 12 weeks to initiate antenatal care, while 45.3% pointed out they used steroids to prevent preterm labor. Record-keeping was viewed as an essential aspect to manage PTB when providing care. Despite the constrained resources, midwives were providing care to prevent PTB. This was evidenced by 78.2% agreeing that keep records from the first booking until the last antenatal visit, while 96.2% monitored the fetal heart rate, 98.1% screened for infections, and 90.9% referred all women at risk to the doctor. Thus, most of the midwives were competent with a confidence interval of (95%) and a prevalence of 9% and 9.5% that, is 9/10, which could prevent PTB.
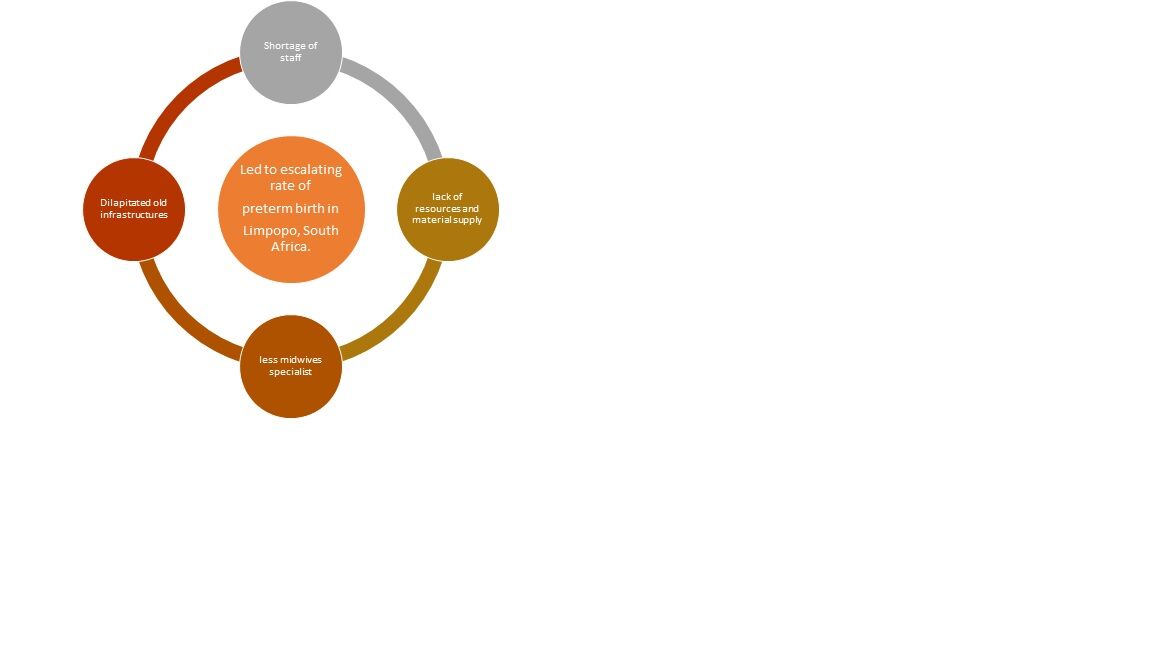
Conclusion: Lack of resources, including staffing and specialized care, contributed to escalating PTB at health facilities in Limpopo province.
Keywords: midwives, maternal and neonatal care, obstetric units, preterm birth, preterm death
Graphical Abstract:
Introduction
Preterm birth (PTB) is defined as the baby’s birth before completing full 37 gestational age, contributing to more complications that lead to neonatal deaths worldwide.1 South Africa is also faced with an escalating rate of preterm birth and is currently having an increasing rate of 59% occurring mainly at the community health centers and district hospitals.2 The National New Born Care report of 2012–2013 showed the provincial preterm birth statistics as follows: Gauteng Province had the highest rate at 414,840 followed by Kwa-Zulu Natal province at 381,264; Limpopo Province at 254,249; Eastern Cape Province at 234,841; Mpumalanga Province at 153,206; North West Province at 115,828 and Free State Province at 94,139.3 The escalating rate was supported by neonatal deaths rate reported by Rhoda and Pattinson (2018) whose study recorded 5237 neonatal deaths in 2012–2013. The deaths were related to neonatal immaturity and complications of immature neonates. Many preterm birth causes were identified, including intrauterine inflammation, placental malfunctioning, and placental abnormality.4–7 Additional preterm birth complications resulting in neonatal deaths were hyaline membrane diseases, meconium aspiration, neonatal asphyxia, hypoglycemia, hypoxia, inability to feed, and hypoxemia. And a spectrum of neurodevelopment conditions and ultimately neonatal demise leading to an increased neonatal death rate in Limpopo, South Africa. For midwives to reduce this rate of preterm birth occurrence, they need to provide promotive and preventive care during antenatal care challenges that are not accessible due to limited resources in rural settings like Limpopo province, South Africa.8 Preconception care such as reducing weight, provision of oral vitamin supplementation, advising smoking women to stop during pregnancy, and so on can play a significant role in reducing preterm births.9 In South Africa, the Nursing Council (SANC) considers the midwife a primary registered practitioner who provides care and supports the mother and baby to achieve and maintain good health during pregnancy, labor, and puerperium.10 In addition, there are Basic Antenatal Care (BANC) guidelines that are used by in-service midwives on how to identify the pre-existing chronic conditions that can complicate pregnancy and can as well predispose women to preterm births.11 Ronan (2013) in her study emphasized that a well-trained midwife could provide maternal care that reduces the occurrences of delivery before the completion of 37th week. If they fail to prevent preterm birth, they are well equipped to offer professional neonatal care to help the immature neonate survive.12
Many other authors also confirmed that midwives could prevent preterm birth through promotive and preventive measures, including educating mothers about the risk of falling pregnant at early ages less than 18 years and advanced age above 35 years. Inform the mother of a well-balanced diet and micronutrient supplements in preparation for pregnancy.13 Most importantly, they educate them on the importance of timely antenatal care attendance, proper birth plan, and attending classes to prepare for birth.13–15 South Africa, like other developing countries, lacks the staff to prevent the increasing rate of preterm birth16 Limpopo Province alone had 3097 newborn babies under 2500 grams, within the units that lack incubators and malfunctioning thermometers for measuring room the temperatures in the units, thus increasing neonatal mortality. Leam and McCandlish, confirm that limited working tools can affect the provision of skilled care to reduce the occurrence of preterm birth in obstetrics units in Limpopo province.17
Salam et al indicated that professional midwives are the most relevant maternal and child health professionals who need to and can play a pivotal role in reducing preterm births and infant mortality in South Africa. Consequently, midwives are expected to provide maternal health education, identify and refer women with maternal conditions predisposing them to preterm birth, and management of women at high risk of PTB, they ought to prevent pregnancy.18 The study aimed to determine and describe what is escalating the preterm birth rate in Limpopo province, South Africa.
Materials and Methods
Research Method and Design
The study was conducted in three selected districts of Limpopo province; this district had the highest population of preterm births, namely, Capricorn, Vhembe, and Sekhukhune. A quantitative research approach was adopted, wherein a non-experimental, descriptive design was used. Twelve hospitals with the highest preterm birth registered from the three districts were purposively sampled. The population comprised all midwives with 12 months of working experience in the obstetric units. The target population of the midwives during the period of study was 151 inclusive of day/night and those on leave, while the actual total midwives on duty, including night staff and those on holiday, were 96. The researcher used non-probability convenient sampling to sample 55/96, accounting for (57%) of midwives. The total number of midwives who participated was 55 (57%) because only those who were not on leave or night duty who voluntarily agreed to participate were given a questionnaire to complete.
A self-administered questionnaire with closed-ended questions was administered to all midwives who were on duty and were willing to participate; this was completed during lunch breaks using the resting rooms in their workplace. The questionnaire had the following: demographic characteristics, midwifery care to reduce preterm birth, and available resources (staff, equipment, drugs, and medical supplies). The Statistical Package for Social Sciences (SPSS) version 25 was employed to analyze data. Data were presented using Tables 1–5 with numbers and percentages. Validity was ensured: the research instrument was submitted to experts’ maternal health care services; they checked the construction and content of the devices.19 The tool was piloted by 13 midwives who did not form part of the main study. The pilot assisted the researcher in picking up ambiguous and incomplete questions; the researcher amended the questionnaire before commencement with the actual research.19
 |
Table 1 List of Selected Facilities and Population Sampled |
 |
Table 2 Age Distribution, Qualification and Years of Experience in Current Position |
 |
Table 3 Care to Prevent Preterm Birth During Antenatal |
 |
Table 4 Care to Prevent Preterm Birth if Contractions Start |
 |
Table 5 Available Resources (Staff, Equipment, Drugs, and Medical Supplies) to Prevent Preterm Birth |
Ethics Consideration
To ensure that the study was authentic, the researchers sought an ethical certificate, and the University of Venda Research Ethics Committee (UREC) granted them an ethical clearance project no: SHS/16/PDC/10/1608. After receiving the UREC certificate, the researchers applied for access to obstetric units of the Limpopo Department of Health. The Limpopo Department of Health granted the searchers permission to collect data from the obstetric units. Ethical aspects of voluntary participation, anonymity and confidentiality were adhered to. All respondents signed consent forms to ensure their voluntary participation.
Presentation of Results
Sample Size
Table 3 reveals that 29.1% of midwives made sure pregnant mothers booked antenatal care before 12 weeks gestation. 78.2% of midwives kept records of antenatal pregnant women from the first to the last visit. 96.3% of midwives took first visit blood specimens for investigations; 98.2% midwives recorded the baseline data; 92.7% midwives checked the results and made sure all results needed attention was shown to the medical practitioners. Approximately 90.9% of midwives referred all mothers with special needs to other team members, 98.1% of midwives screened the pregnant mothers for all types of infections, 96.2% of midwives and managers assessed and classified women according to high or low risk, and 81.1% midwives ensured that all pregnant mothers had five or more visits recommended to the clinic for proper management and reduce the risk of preterm births and deaths.
Table 4 shows that 94.4% of midwives took entire history when admitting pregnant mothers with labor and record, 96.2% of midwives transferred all expectant mothers with preterm labor to the hospital for further management, 54.7% of midwives provided pregnant mothers with preterm labor with steroids before moving them to hospital, 85.2% midwives, assessed the contributory factors of preterm labor and gave proper advice and 67.8% midwives cut the episiotomy when assisting pregnant mothers with the preterm labor to avoid neonatal injuries. About 94.4% of midwives prepared the labor room warmly if they anticipated preterm labor, 85.2% midwives alerted the nursery in time when delivering the preterm neonate, 94.4% midwives prepared the resuscitation area well in advance when anticipating preterm birth, and 33.7% midwives agreed that labor units were provided with trained neonatal/pediatric nurse covering all shifts.
Resources to Reduce Preterm Birth
Table 5 shows that 86.2% agreed on ensuring that all units (antenatal, labor, postnatal, and neonatal) have a well explained midwifery-centered policy supporting preterm care. About 76.4% agreed that they are provided with a particular room for preterm babies. Only 34% agreed that there was enough equipment supply, 38.2% agreed that all units had specialists, and 34% agreed that there were drug and medical supplies.
Discussion
The statements that had fewer respondents agreeing on include “All women book before 12 weeks of their gestation” at 29.1% agree rate and 70.9% disagree rate. The World Health Organization (WHO) recommended that pregnant women book before 12 weeks of gestation.20 Equally, the South African guidelines for maternal care echo the same sentiment.21 Even so, the findings of this research are congruent to studies conducted in Nigeria and Ethiopia, respectively,22,23 wherein it was found that pregnant women book later than 12 weeks for antenatal care. Interestingly, it was also found in a study conducted in the United Kingdom (UK) that from 2009 to 2014 wherein overall pregnant women booked late for antenatal care.24 However, the latter authors studied the management of HIV (Human Immunodeficiency Virus) during antenatal care, wherein they further claimed that the late booking is associated with cultural and demographic factors.24 The results of this study are congruent to another study done in South Africa. It was found that pregnant women from underdeveloped communities were also booking after twelve weeks of gestation, unlike those living in developed societies.25 Therefore, it becomes evident that the challenge of pregnant women securing after 12 weeks of pregnancy for antenatal care is a problem phenomenon, especially in developing countries. However, the resources available to manage the results of this challenge, such as preterm birth, might be a defining factor for the developed and developing contexts. Pregnant women of African descent tend to book late for antenatal care within the UK. Furthermore, it is found in this research that 78% of midwives agreed that they kept records of antenatal pregnant women from the first to the last visit. This evidence comes as a concern, while there is a universal rule in nursing that “what is not recorded is regarded as not being done”.26 This emphasizes good record-keeping across nursing and midwifery practices, as it is considered integral to the quality and effective care. Congruently, the South African guidelines for maternal care prescribe standards for medical record-keeping during antenatal care.21 Even under these clear policy guidelines, the findings of this research were consistent with a study conducted in Gauteng.26 Moreover, these findings were found in the study conducted in Rwanda27 where poor record-keeping during antenatal care was found. On the other hand, this finding was contrary to a study conducted in Italy where it was found that a digital record-keeping format is efficient and comprehensive for antenatal care.28 Therefore, poor record-keeping becomes an evident challenge in developing contexts like Africa.
In addition, this research showed that the equipment and supplies were less than 40%, meaning that there was less provision of tools to midwives though competent they could not reduce preterm births. These results are supported by Thopola and Lekhuleni,29, where 94% of midwives acknowledged their competency in their daily execution of maternal and neonatal care based on their qualifications and experience in maternity services.29 Various studies showed that lack of equipment and material supplies is the leading contributor to substandard maternal care in developing countries, including South Africa.18,21 A study in the United States of America (USA), one of the developed countries with a quality health system, showed a decline in preterm birth in the USA.20 This declining preterm birth rate was because there was improvement and promulgation of practical policy guidelines in the management of teenage pregnancy and other risk factors for preterm birth. The policies included good management of multiple pregnancies provision of troctolitic and steroids drugs to women with preterm labor. In addition, there was the prioritization of staffing and equipping of obstetric and neonatal units.20
These results indicate that <60% agreed that midwives in Limpopo province rarely use preterm labor steroids before transferring the pregnant women to hospitals to prepare for fetal lung maturity. It is recommended by maternal guidelines that it is always preferable to give betamethasone or dexamethasone as part of preterm labor management.21 Importantly, the administration of steroids is recommended because they are beneficial for cell and organ growth for the fetus.30 Notwithstanding the benefits mentioned, Newnham et al31 found that the positives of administering steroids might be outweighed by potential risks wherein the administration’s timing is of clinical significance. Thus, clinical improvement is only seen in the neonate’s health, provided the birth occurred within 24 hours to seven days of steroids administration. Under these facts’ findings, it becomes somewhat uncertain about concluding that midwives’ relatively rare use of steroids in Limpopo can be said to be escalating PTB.31 Furthermore, the statement with the least percentages of respondents is “A trained specialist midwife is covering all shifts.” The findings confirmed that few specialists were allocated to mend the obstetric units of Limpopo Province, at 33.7% disagreed and 67.3% agreed. Notably, in their study, Uys and Klopper 32 indicated that maternal services rendered by specialized trained personnel reduced the risk of dying. Furthermore, their investigation revealed that maternity units of South Africa had only 20% of specialized trained nurses leading to increased preterm birth in obstetric units of South Africa.33 In addition, a study in the United Kingdom and the Gambia revealed that equipping of midwives and other primary caregivers with skills played a great deal in reducing maternal and neonatal adverse outcomes.34 Another study in Indonesia proved that midwives had received enough training and the skills needed to reduce neonatal mortality by timeous and efficient antenatal care. However, the lack of evidence-based policy and resources to provide efficient antenatal care services retarded the effort.34 Therefore, the lack of specialists is found to be escalating PTB.35
These results show that providing medical equipment and supplies is a challenge in the Limpopo province. Hence, 34% (agree) and 66% (disagree) indicate that equipment needed to provide quality care is not always available. Congruently, these findings are supported by a study in South Sudan where lack of medical supplies, poor staffing, and lack of utilities like water and electricity was a barrier to the execution of quality maternal and child care by highly specialized or trained doctors and midwives.35 Furthermore, various studies showed that lack of equipment and material supplies is the leading contributor to poor maternal and child health care in developing countries similar to South Africa.18 In addition, one of the developed countries with a quality health system showed a decline in preterm birth in USA32. This declining preterm birth rate was due to the improvement and promulgation of practical policy guidelines in the management of teenage pregnancy risk factors of preterm birth. The policies included good management of multiple pregnancies provision of troctolitic and steroids drugs to women with preterm labor. In addition, there was the prioritization of staffing and equipping of obstetric and neonatal units.36 Circumstantially, these challenges lead to increased maternal and neonatal mortality in the hands of knowledgeable practitioners.36 Another study predicting the neonatal mortality risks from the United Kingdom and the Gambia support the findings by adding that due to lack of advanced neonatal equipment in the Gambia intensive care unit, there was more neonatal mortality amongst neonate of less than 2000g, this confirms that developing countries with lack of intensive equipment are at risk of increased neonatal death amongst their sick neonates.37 Therefore, this meant that the obstetric units were not well mended considering staff equipment and supplies, leading to the unresolved occurrences of preterm birth.37
Conclusion
It is concluded in this study that PTB in the rural Limpopo province escalates because of late bookings of pregnant women for initiation of antenatal care. Hence, timely presentation by pregnant women at antenatal health care facilities alleviates obstetric complications, therefore, minimizing the risk of preterm birth. Worryingly, even though the nursing practice prides itself on good record keeping, it is evident in this research that poor staffing and less material supply remain a challenge in rural areas like Limpopo province, potentiating a higher risk of poor-quality care, which results in PTB. Notably, developing contexts, such as South Africa are resource-stricken contexts where medical supplies are scanty, specialists’ nurses and doctors are at the lowest numbers. Hence, this finding becomes integral to PTB escalation. On the other hand, preterm labor steroids are associated with escalating PTB.
Acknowledgments
Researchers acknowledge the midwives for participating in the study, the University of Venda for funding and providing the ethics certificate, and Limpopo Department of Health for providing the approval letter to access the obstetric units.
Disclosure
The authors declare that they had no financial or personal relationships, which may have inappropriately influenced them in writing this article.
References
1. Medley N, Vogel JP, Care A, Alfirevic Z. Interventions during pregnancy to prevent preterm birth: an overview of Cochrane systematic reviews. Cochrane Database Syst Rev. 2018;11.doi:10.1002/14651858.CD012505.pub2
2. Dippenaar J, Da Serra D. Seller’s Midwifery.
3. Allanson ER, Muller M, Pattinson RC. Causes of perinatal mortality and associated maternal complications in a South African province: challenges in predicting poor outcomes. BMC Pregnancy Childbirth. 2015;15(1):1–7. doi:10.1186/s12884-015-0472-9
4. Rhoda NR, Velaphi S, Gebhardt GS, Kauchali S, Barron P. Reducing neonatal deaths in South Africa: progress and challenges. S Afr Med J. 2018;108(3):9–16. doi:10.7196/SAMJ.2017.v108i3b.12804
5. Romero R, Dey SK, Fisher SJ. Preterm labor: one syndrome, many causes. Science. 2014;345(6198):760–765. doi:10.1126/science.1251816
6. Weiner E, Dekalo A, Feldstein O, et al. The placental factor in spontaneous preterm birth in twin vs. singleton pregnancies. Eur J Obstet Gynecol Reprod Biol. 2017;1(214):1–5.
7. Stanek J. Comparison of placental pathology in preterm, late-preterm, near-term, and term births. Am J Obstet Gynecol. 2014;210(3):234–e1. doi:10.1016/j.ajog.2013.10.015
8. Newnham JP, Dickinson JE, Hart RJ, Pennell CE, Arrese CA, Keelan JA. Strategies to prevent preterm birth. Front Immunol. 2014;19(5):584.
9. Toivonen KI, Oinonen KA, Duchene KM. Preconception health behaviors: a scoping review. Prev Med. 2017;1(96):1–5. doi:10.1016/j.ypmed.2016.11.022
10. Council SA, Verpleging SA. Nursing Act 2005 (Act No. 33 of 2005). Government Gazette. Pretoria: Government Printers; 2005.
11. Ngxongo TS. Basic antenatal care approach to antenatal care service provision. In: Selected Topics in Midwifery Care. Intech Open; 2018.doi: 10.5772/intechopen.79361
12. Ronan CB. Making STARs: reaching successful transition to at-breast feeds in the premature infant. J Neonatal Nurs. 2013;19(4):206–212. doi:10.1016/j.jnn.2013.01.004
13. Tsegaye B, Kassa A. Prevalence of adverse birth outcome and associated factors among women who delivered in Hawassa town governmental health institutions, south Ethiopia, in 2017. Reprod Health. 2018;15(1):0–1. doi:10.1186/s12978-018-0631-3
14. Davidson MR, London ML, Ladewig PW. Olds’ Maternal-Newborn Nursing & Women’s Health Across the Lifespan. Pearson; 2012.
15. Blencowe H, Cousens S, Chou D, et al. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health. 2013;10(1):1–4. doi:10.1186/1742-4755-10-S1-S2
16. World Health Organization. Managing Complications in Pregnancy and Childbirth: a Guide for Midwives and Doctors. World Health Organization; 2017.
17. MacLellan J. Claiming an ethic of care for midwifery. Nurs Ethics. 2014;21(7):803–811. doi:10.1177/0969733014534878
18. Salam RA, Das JK, Ali A, Bhaumik S, Lassi ZS. Diagnosis and management of preeclampsia in community settings in low and middle-income countries. J Fam Med Prim Care Rev. 2015;4(4):501. doi:10.4103/2249-4863.174265
19. Brink H, Van der Walt C, Van Rensburg G. Fundamentals of Research Methodology for Health Care Professionals. Juta and Company Ltd; 2012.
20. World Health Organization. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience: summary: highlights and Key Messages from the World Health Organization’s 2016 Global Recommendations for Routine Antenatal Care. World Health Organization; 2018.
21. Malherbe HL, Woods DL, Aldous C, Christianson AL. Review of the 2015 guidelines for maternity care with relevance to congenital disorders. S Afr Med J. 2016;106(7):669–671. doi:10.7196/SAMJ.2016.v106i7.10813
22. Ifenne DI, Utoo BT. Gestational age at booking for antenatal care in a tertiary health facility in north-central, Nigeria. Niger J Med Assoc. 2012;53(4):236. doi:10.4103/0300-1652.107602
23. Abuka T, Alemu A, Birhanu B. Assessment of the timing of first antenatal care booking and associated factors among pregnant women who attend antenatal care at health facilities in Dilla town, Gedeo zone, southern nations, nationalities and peoples region, Ethiopia, 2014. J Preg Child Health. 2016;3(258):2.
24. French CE, Thorne C, Byrne L, Cortina‐Borja M, Tookey PA. Presentation for care and antenatal management of HIV in the UK, 2009− 2014. HIV Med. 2017;18(3):161–170. doi:10.1111/hiv.12410
25. Ebonwu J, Mumbauer A, Uys M, Wainberg ML, Medina-Marino A. Determinants of late antenatal care presentation in rural and peri-urban communities in South Africa: a cross-sectional study. PLoS One. 2018;13(3):e0191903.
26. Patience NT, Sibiya MN, Gwele NS. Evidence of application of the basic antenatal care principles of reasonable care and guidelines in pregnant women’s antenatal care records. Afr J Prim Health Care Fam Med. 2016;8(2):1–6. doi:10.4102/phcfm.v8i2.1016
27. Rurangirwa AA, Mogren I, Ntaganira J, Govender K, Krantz G. Quality of antenatal care services in Rwanda: assessing practices of health care providers. BMC Health Serv Res. 2018;18(1):0–1. doi:10.1186/s12913-018-3694-5
28. Borsari L, Stancanelli G, Guarenti L, et al. An innovative mobile health system to improve and standardize antenatal care among underserved communities: a feasibility study in an Italian hosting center for asylum seekers. J Immigr Minor Health. 2018;20(5):1128–1136. doi:10.1007/s10903-017-0669-2
29. Thopola MK, Lekhuleni ME. An evidence-based model for enhancing optimal midwifery practice in maternity units of public hospitals, Limpopo province (Doctoral dissertation, University of Limpopo); 2016.
30. Mgawadere F, Unkels R, Kazembe A. van den Broek N. Factors associated with maternal mortality in Malawi: application of the three delays model. BMC Pregnancy Childbirth. 2017;17(1):1–9. doi:10.1186/s12884-017-1406-5
31. Newnham JP, Kemp MW, White SW, Arrese CA, Hart RJ, Keelan JA. Applying precision public health to prevent preterm birth. Public Health Front. 2017;5(5):66. doi:10.3389/fpubh.2017.00066
32. Schoen CN, Tabbah S, Iams JD, Caughey AB, Berghella V. Why the United States preterm birth rate is declining. Am J Obstet Gynecol. 2015;213(2):175–180. doi:10.1016/j.ajog.2014.12.011
33. Uys LR, Klopper HC. What is the ideal ratio of categories of nurses for the South African public health system? S Afr J Sci. 2013;109(5):1–4. doi:10.1590/sajs.2013/a0015
34. Lassi ZS, Bhutta ZA. Community based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database Syst Rev. 2015;2015(3). doi:10.1002/14651858.CD007754.pub3
35. Mugo NS, Dibley MJ, Damundu EY, Alam A. Barriers faced by the health workers to deliver maternal care services and their perceptions of the factors preventing their clients from receiving the services: a qualitative study in South Sudan. Matern Child Health J. 2018;22(11):1598–1606. doi:10.1007/s10995-018-2555-5
36. Anggraini D, Abdollahian M, Marion K. Improving the information availability and accessibility of antenatal measurements to ensure safe delivery: a research-based policy recommendation to reduce neonatal mortality in Indonesia. Int Journal Women’s Health. 2020;12:369. doi:10.2147/IJWH.S247213
37. Medvedev MM, Brotherton H, Gai A, et al. Development and validation of a simplified score to predict neonatal mortality risk among neonates weighing 2000 g or less (NMR-2000): an analysis using data from the UK and The Gambia. Lancet Child Adolesc Health. 2020;4(4):299–311. doi:10.1016/S2352-4642(20)30021-3
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
