Back to Journals » International Journal of General Medicine » Volume 16
The Predictive Value of the CHA2DS2-VASc Score for In-Stent Restenosis Among Patients with Drug-Eluting Stents Implantation
Authors Zhao J, Hou L, Zhu N, Huang R, Su K, Lei Y, Li Y
Received 3 October 2022
Accepted for publication 28 December 2022
Published 5 January 2023 Volume 2023:16 Pages 69—76
DOI https://doi.org/10.2147/IJGM.S391312
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Jinbo Zhao,1,* Ling Hou,2,* Ni Zhu,3,* Rui Huang,1 Ke Su,1 Yuhua Lei,1 Yuanhong Li1
1Cardiovascular Disease Center, Central Hospital of Tujia and Miao Autonomous Prefecture, Hubei University of Medicine, Enshi Prefecture, Hubei Province, 445000, People’s Republic of China; 2Department of Central Hospital of Tujia and Miao Autonomous Prefecture, Hubei University of Medicine, Shiyan, Hubei Province, 442000, People’s Republic of China; 3Department of Pathology, Central Hospital of Tujia and Miao Autonomous Prefecture, Hubei University of Medicine, Enshi Prefecture, Hubei Province, 445000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yuanhong Li, Email [email protected]
Objective: The CHA2DS2-VASc score, a system which has been initially recommended for the assessment of thromboembolic risk in patients with atrial fibrillation (AF), arouses attention in the field of adverse coronary events. The purpose of this study was to explore the predictive value of preprocedural CHA2DS2-VASc score on ISR in patients after drug-eluting stent (DES) implantation.
Methods: To further investigate the relationship between CHA2DS2-VASc scores and ISR after DES, a retrospective study of DES was carried on. Additionally, the preoperative variables for the ISR and control groups were contrasted. Predictive factors were chosen using the optimal subset regression. We validate the model using internal validation. The prediction model was evaluated using the receiver operator characteristic (ROC) analysis.
Results: We used a 3:7 ratio to create an experimental group and a validation group, and then ran a stepwise regression with the data from each of the two groups. The results showed that CHA2DS2-VASc score was an independent risk factor for ISR in both the experimental (p = 0.0139) and validation groups (p = 0.0014), and both had significant predictive value for ISR. The area of the ROC curve was greater than 0.5 in both groups (AUC = 0.78, 0.719, respectively) indicating that the model fit was good in both groups.
Conclusion: The CHA2DS2-VASc score is a reliable predictor of in-stent restenosis (ISR) after DES implantation.
Keywords: CHA2DS2-VASc score, drug-eluting stents, DES, percutaneous coronary intervention, PCI, in-stent restenosis, ISR
Background
Human health is seriously threatened by cardiovascular disease.1 Cardiac interventional techniques have advanced rapidly after myocardial infarction, and drug-eluting stent implantation has now become routine treatment. ISR is one of the frequent post-PCI side effects.2 Although the incidence of ISR after DES implantation has been significantly reduced compared with the era of bare metal stents, the chances of patients with complex, high-risk coronary lesions having revascularization after PCI can still reach 5% to 10%.3,4 The occurrence of this complication can lead to increased consumption of healthcare resources, longer hospital stays and higher mortality rates.
The CHA2DS2-VASc score is a classical scoring system constructed to assess the risk of thromboembolism in patients with non-valvular AF and to guide anticoagulation therapy, and has been shown to predict the occurrence of coronary artery disease1,5,6 and the long-term prognosis of patients after PCI.7,8 Also, the variables that make up the CHA2DS2-VASc score have been shown in numerous studies to be risk factors for death and adverse events in patients with acute STEMI.9–13 In magnetic resonance imaging, higher CHADS2 scores are similarly associated with coronary microvascular dysfunction,14 and in patients without comorbid atrial fibrillation, high CHADS2 scores can increase the risk of peripheral arterial vascular disease.15 Additionally, it has recently been demonstrated that CHA2DS2-VASc scores are related to prognosis in patients receiving transcatheter aortic valve replacement.16 Thus, CHADS2 scores may be used to predict the occurrence of adverse coronary events, including in-stent restenosis.
Although a few prior research have looked into potential factors of the high incidence rate of ISR, such as poor stent expansion, poor apposition, and residual stenosis17 and have shown that the CHA2DS2-VASc score can be used to predict events related to ISR after metal stent implantation,18 there are still limitations including the limitation of clinical practice, the lack of latest clinical factors inflecting inflammatory responses and lipid metabolism. Thus, finding simpler and more effective clinical predictors of restenosis and building newest model is something we need to consider in the clinical setting.
Methods
This study was given the go-ahead by the Ethics Committee of the Central Hospital of Enshi Autonomous Prefecture in accordance with the Declaration of Helsinki. As patient consent to review their medical records was not required by the Ethics Committee of the Central Hospital of Enshi Autonomous Prefecture. Patient agreement was not required because this study is retrospective, retrospective studies do not require informed consent from the patient, but possibly from the ethics committee, so we have provided a certificate of approval from the ethics committee to the editor. The reasons for not requiring informed consent from patients have been marked in the ethical certificate as follows: Firstly, this study collects clinical case data and does not lead to adverse reactions or harm to patients. Secondly, all patient data used in this article is completely anonymous and the data has been anonymised prior to access and analysis, therefore their medical records were examined without their permission. This study was an analysis of an observational cohort study that was carried out at Enshi Central Hospital in China from January 2017 to December 2020. There were 1017 CAD patients who underwent PCI with DES in total. Patients who (1) did not review for coronary angiography after PCI, (2) did not take statins and anti-platelet aggregation drugs regularly after surgery, (3) had other postoperative cardiovascular adverse events, and (4) lacked massive clinical and angiographic information, were excluded from the study (Figure 1).
 |
Figure 1 The selection procession of selected subjects. |
The CHA2DS2-VASc score (congestive heart failure [CHF]; hypertension; age >75 years [doubled]; type 2 diabetes; prior stroke or transient ischemic attack [doubled]; vascular disease; age 65–74 years; and sex [female]) was calculated in this data. The basic stenosis score for each coronary artery is multiplied by a factor for that lesion site to give a score for that lesion vessel, and the sum of the scores for each lesion vessel is the total score (the Genisi score) for the degree of stenosis of the patient’s coronary artery lesion.
We added variables to the data including CHA2DS2-VASc score, the neutrophil/lymphocyte ratio, Genisi score.19 Internal validation of the data in a 3:7 ratio was applied to the data. In the model feature selection process, we exclude feature parameters that are already included in the CHARDS score in order to exclude multicollinearity. We screened all variables according to the clinical context in conjunction with the literature and included the screened variables in the initial regression model. We also utilized optimal subset + multi-factor logistic regression analysis to identify the main drivers of ISR (In-stent restenosis is defined as a new official lumen diameter stenosis greater than or equal to 50% in the stented segment, proximal segment and distal 5mm segment on coronary angiography, with the reference vessel being the normal vessel distal to the stent17) and assess the strengths and weaknesses of the models in light of the significant number of factors affecting ISR.
R software version 4.0.5 was used for statistical analysis, and two-tailed analysis with P. For continuous variables that satisfy a normal distribution we use a t-test to compare differences between groups. The chi-square test or Fisher’s exact test was utilized pointing to categorical variables. In cases of skewed distribution, data were reported as an interquartile range (IQR) and compared using the Mann–Whitney U-test.
We assessed the fit and performance of the model using the area under the ROC curve AUC, for both the experimental and validation groups. Acceptable diagnostic value for models is AUC >0.5.
Results
Baseline Information
Seventy patients had in-stent restenosis. Baseline information comparing 70 patients with ISR and 185 patients without ISR are displayed in Table 1.
 |
Table 1 The Baseline Characteristics of the Subjects Between ISR Group and Non-ISR Group |
According to Table 1, these factors are not statistically significant, including age, leukocyte, platelet, hemoglobin, platelet distribution width, mean platelet volume, red cell distribution width, glucose, neutrophil/lymphocyte ratio, Platelet pressure. However, monocytes, lymphocytes and thyroid-stimulating hormone were more prevalent in patients with ISR.
Regarding PCI-related aspects, there was no statistically significant difference in the number of stents implanted between the two groups. For liver and kidney function and lipid metabolism, the creatinine level in the ISR group was lower than that in the control group with statistical significance. There were also differences between the two groups in indicators such as UC and low-density lipoprotein cholesterol (p<0.05).
Optimal Subset Regression Models and Internal Validation
All variables from the baseline data were included in the initial logistic regression model for the selection of the optimal subset model, and a multi-factor logistic regression was conducted using the backward method to select the ideal subset based on the guiding principle of selecting the model with the lowest AIC value as the optimal model. We found that age, AF score, ACEI and creatinine were closely related to the occurrence of ISR (Table 2, AIC=−757.47), and CHARDS score had the greatest influence on it, because the area under the ROC curve of the optimal subset of each group was 0.78 (Figure 2) and 0.719 (Figure 3), respectively, both greater than 0.5, the CHARDS score was an independent risk factor for ISR.
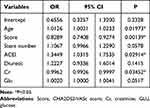 |
Table 2 Regression Results for the Optimal Subset |
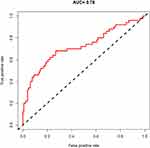 |
Figure 2 The receiver operator characteristic curve for the train group. |
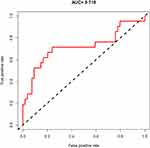 |
Figure 3 The receiver operator characteristic curve for the test group. |
Discussion
The atrial fibrillation embolic risk assessment system CHA2DS2-VASc score, originally constructed to assess the risk of thromboembolism in patients with non-valvular AF and to guide anticoagulation therapy, consists of several classical cardiovascular disease risk factors and can be used as an important tool to assess patients’ cardiovascular prognosis.20 Several previous studies have suggested that the CHA2DS2-VASc score can predict the prognosis of patients with various cardiovascular diseases (eg, hypertension, heart failure) regardless of the combination of atrial fibrillation16,21 as well as the low left internal mammary artery (LIMA) flow in patients underwent coronary bypass surgery.22 And it also can be an independent predictor of in-hospital and long-term prognosis in patients with acute myocardial infarction.23 In patients with acute coronary syndromes, the CHA2DS2-VASc score is also associated with the occurrence of adverse cardiovascular events and associated with the thrombus burden in patients with acute myocardial infarction undergoing SVG-PCI.24 For example, a study that included 13,422 patients with ACS showed that elevated CHA2DS2-VASc scores were associated with 30 d, 1-year death and MACE events.25 In a study by Unal et al,26 the CHA2DS2-VASc score >2 was found to be an independent predictor of the incidence of stent thrombosis. Above all, compared with other available ISR risk stratification tools, the CHA2DS2 VASc score is a reliable and easily calculated scoring tool that can be used in daily practice to the evaluation of circulatory diseases.
DES implantation is one of the clinical treatments for ACS. Although several studies have revealed27,28 that DES can reduce the incidence of ISR compared with BMS implantation, ISR after DES with a high still needed attention for its high probability of 5–10%. Therefore, although Alfonso et al18 have found that the CHARDS score is associated with the occurrence of ISR after BMS, we still conducted this study with the aim of further exploring the predictive value of the CHARDS score for ISR after DES based on the previous study.
Numerous earlier studies have shown that diabetes, age, smoking, stent number, creatinine, post-operative use of different drugs and anterior descending lesions are linked to restenosis following the placement of DES.4,17,29,30 With the optimal subset regression, a new method of machine learning, we screened for above risk factors which has reported in previous study, for newest factors which appear to be associated with lipid metabolism, and for newest scoring system. Finally, we constructed a model that included age, stent number, creatinine, glucose and post-operative use of diuretics or ACEI, in addition to previously reported factors, as well as CHARDS scores. In this study, the CHARDS score showed good predictive value for ISR, and our model had a better fit and better diagnostic value than the previous model.
Nevertheless, the research still has several limitations. First of all, there was no external validation for this single-center study. The prediction model may not be generalizable despite internal validation. The study’s retrospective design and insufficient degree of evidence were its final flaws.
Conclusion
In conclusion, we found that CHARDS score can be an independent risk factor for ISR after drug-eluting stenting implanting and the model based on CHARDS score, multivessel lesions, left main stem lesion, triglycerides, and HDL cholesterol showed satisfactory predictive value.
Funding
This work was funded by the National Natural Science Foundation of China (No.82160072) and the Science and Technology Support Project of Enshi Prefecture Science and Technology Bureau (D20210024).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zhao D, Liu J, Wang M, et al. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16(4):203–212. doi:10.1038/s41569-018-0119-4
2. Jimenez-Quevedo P, Serrador A, Perez de Prado A, et al. Spanish Cardiac Catheterization and Coronary Intervention Registry. 25th official report of the Spanish Society of Cardiology Working Group on cardiac catheterization and interventional cardiology (1990–2015). Rev Esp Cardiol. 2016;69(12):1180–1189. doi:10.1016/j.rec.2016.08.016
3. Peng N, Liu W, Li Z, et al. Drug-coated balloons versus everolimus-eluting stents in patients with in-stent restenosis: a pair-wise meta-analysis of randomized trials. Cardiovasc Ther. 2020;2020:1042329. doi:10.1155/2020/1042329
4. Piccolo R, Bonaa KH, Efthimiou O, et al. Drug-eluting or bare-metal stents for percutaneous coronary intervention: a systematic review and individual patient data meta-analysis of randomised clinical trials. Lancet. 2019;393(10190):2503–2510. doi:10.1016/S0140-6736(19)30474-X
5. Chang CF, Lin CC. Current concepts of contrast-induced nephropathy: a brief review. J Chin Med Assoc. 2013;76(12):673–681. doi:10.1016/j.jcma.2013.08.011
6. Sato A, Aonuma K, Watanabe M, et al. Association of contrast-induced nephropathy with risk of adverse clinical outcomes in patients with cardiac catheterization: from the CINC-J study. Int J Cardiol. 2017;227:424–429. doi:10.1016/j.ijcard.2016.11.019
7. Huang FY, Huang BT, Pu XB, et al. CHADS(2), CHA(2)DS(2)-VASc and R(2)CHADS(2) scores predict mortality in patients with coronary artery disease. Intern Emerg Med. 2017;12(4):479–486. doi:10.1007/s11739-017-1608-x
8. Yao HM, Wan YD, Zhang XJ, et al. Long-term follow-up results in patients undergoing percutaneous coronary intervention (PCI) with drug-eluting stents: results from a single high-volume PCI centre. BMJ Open. 2014;4(8):e004892. doi:10.1136/bmjopen-2014-004892
9. Cooper HA, Domanski MJ, Rosenberg Y, et al. Acute ST-segment elevation myocardial infarction and prior stroke: an analysis from the Magnesium in Coronaries (MAGIC) trial. Am Heart J. 2004;148(6):1012–1019. doi:10.1016/j.ahj.2004.02.017
10. Cotter G, Cannon CP, McCabe CH, et al. Prior peripheral arterial disease and cerebrovascular disease are independent predictors of adverse outcome in patients with acute coronary syndromes: are we doing enough? Results from the Orbofiban in Patients with Unstable Coronary Syndromes-Thrombolysis In Myocardial Infarction (OPUS-TIMI) 16 study. Am Heart J. 2003;145(4):622–627. doi:10.1067/mhj.2003.6
11. Granger CB, Goldberg RJ, Dabbous O, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163(19):2345–2353. doi:10.1001/archinte.163.19.2345
12. Kytö V, Sipilä J, Rautava P. Gender and in-hospital mortality of ST-segment elevation myocardial infarction (from a multihospital nationwide registry study of 31,689 patients). Am J Cardiol. 2015;115(3):303–306. doi:10.1016/j.amjcard.2014.11.001
13. Morrow DA, Antman EM, Charlesworth A, et al. TIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation: an intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation. 2000;102(17):2031–2037. doi:10.1161/01.CIR.102.17.2031
14. Kirigaya H, Kato S, Gyotoku D, et al. Higher CHADS2 score is associated with impaired coronary flow reserve: a study using phase contrast cine magnetic resonance imaging. Int J Cardiol. 2016;221:800–805. doi:10.1016/j.ijcard.2016.07.116
15. Hsu PC, Chiu CA, Chu CY, et al. CHADS2 score and risk of new-onset peripheral arterial occlusive disease in patients without atrial fibrillation: a Nationwide Cohort Study in Taiwan. J Atheroscler Thromb. 2015;22(5):490–498. doi:10.5551/jat.27284
16. Melgaard L, Gorst-Rasmussen A, Lane DA, et al. Assessment of the CHA2DS2-VASc score in predicting ischemic stroke, thromboembolism, and death in patients with heart failure with and without atrial fibrillation. JAMA. 2015;314(10):1030–1038. doi:10.1001/jama.2015.10725
17. Alraies MC, Darmoch F, Tummala R, et al. Diagnosis and management challenges of in-stent restenosis in coronary arteries. World J Cardiol. 2017;9(8):640–651. doi:10.4330/wjc.v9.i8.640
18. Alfonso F, Díez-Villanueva P, Rivero F. CHA(2)DS(2)-VAS(C) clinical score to predict in-stent restenosis. Angiology. 2018;69(8):653–656. doi:10.1177/0003319717736159
19. Rampidis GP, Benetos G, Benz DC, et al. A guide for gensini score calculation. Atherosclerosis. 2019;287:181–183. doi:10.1016/j.atherosclerosis.2019.05.012
20. Lip GY, Nieuwlaat R, Pisters R, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–272. doi:10.1378/chest.09-1584
21. Mazzone C, Cioffi G, Carriere C, et al. Predictive role of CHA(2)DS(2)-VASc score for cardiovascular events and death in patients with arterial hypertension and stable sinus rhythm. Eur J Prev Cardiol. 2017;24(15):1584–1593. doi:10.1177/2047487317726068
22. Soylemez N, Balli M, Koksal F, et al. A new current to the armamentarium: is the CHA2DS2-Vasc-HS score predictive of low left internal mammary artery (lima) flow in patients underwent coronary bypass surgery? Heart Surg Forum. 2021;24(4):E631–E636. doi:10.1532/hsf.3837
23. Rozenbaum Z, Elis A, Shuvy M, et al. CHA2DS2-VASc score and clinical outcomes of patients with acute coronary syndrome. Eur J Intern Med. 2016;36:57–61. doi:10.1016/j.ejim.2016.09.010
24. Maden O, Çakmak Karaaslan Ö, Kanal Y, et al. Association of CHA2DS2-VASc score with thrombus burden in patients with acute myocardial infarction undergoing SVG-PCI. Herz. 2022;47(5):456–464. doi:10.1007/s00059-021-05070-x
25. Kim KH, Kim W, Hwang SH, et al. The CHA2DS2VASc score can be used to stratify the prognosis of acute myocardial infarction patients irrespective of presence of atrial fibrillation. J Cardiol. 2015;65(2):121–127. doi:10.1016/j.jjcc.2014.04.011
26. Ünal S, Açar B, Yayla Ç, et al. Importance and usage of the CHA2DS2-VASc score in predicting acute stent thrombosis. Coron Artery Dis. 2016;27(6):478–482. doi:10.1097/MCA.0000000000000388
27. Dangas GD, Claessen BE, Caixeta A, et al. In-stent restenosis in the drug-eluting stent era. J Am Coll Cardiol. 2010;56(23):1897–1907. doi:10.1016/j.jacc.2010.07.028
28. Lee MS, Banka G. In-stent Restenosis. Interv Cardiol Clin. 2016;5(2):211–220. doi:10.1016/j.iccl.2015.12.006
29. Shehadeh N, Raz I, Nakhleh A. Cardiovascular benefit in the limelight: shifting type 2 diabetes treatment paradigm towards early combination therapy in patients with overt cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):117. doi:10.1186/s12933-018-0760-6
30. Luo Y, Cui S, Zhang C, et al. Prognostic role of fasting remnant cholesterol with in-stent restenosis after drug-eluting stent implantation. Int J Gen Med. 2022;15:1733–1742. doi:10.2147/IJGM.S348148
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
