Back to Journals » Journal of Hepatocellular Carcinoma » Volume 10
The Predictive Role of Inflammatory Biomarkers for Treatment Response and Progression-Free Survival in Patients with Hepatocellular Carcinoma Receiving Hepatic Arterial Infusion Chemotherapy with FOLFOX Regimen: A Preliminary Study
Authors Zhao Y, Liu J, Xiong Z, Gu S , Xia X
Received 5 April 2023
Accepted for publication 20 June 2023
Published 8 July 2023 Volume 2023:10 Pages 1037—1049
DOI https://doi.org/10.2147/JHC.S413283
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr David Gerber
Yang Zhao,1,* Jun Liu,2,* Zhengping Xiong,1 Shanzhi Gu,1 Xibin Xia2
1Department of Interventional Therapy, Hunan Cancer Hospital, The Affiliated Cancer Hospital of Xiangya School of Medicine, Central South University, Changsha, Hunan, 410006, People’s Republic of China; 2Department of Radiology, Hunan Cancer Hospital, The Affiliated Cancer Hospital of Xiangya School of Medicine, Central South University, Changsha, Hunan, 410006, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Shanzhi Gu, Department of Interventional Therapy, Hunan Cancer Hospital, The Affiliated Cancer Hospital of Xiangya School of Medicine, Central South University, Changsha, Hunan, 410006, People’s Republic of China, Email [email protected] Xibin Xia, Department of Radiology, Hunan Cancer Hospital, The Affiliated Cancer Hospital of Xiangya School of Medicine, Central South University, Changsha, Hunan, 410006, People’s Republic of China, Email [email protected]
Objective: This retrospective study aimed to investigate whether pre-treatment inflammatory biomarkers, including the prognostic nutritional index (PNI), monocyte-lymphocyte ratio (MLR), systemic immune inflammation index (SII), and platelet-lymphocyte ratio (PLR), could predict treatment response and prognosis in patients with hepatocellular carcinoma (HCC) receiving hepatic arterial infusion chemotherapy (HAIC) with the oxaliplatin, leucovorin, and fluorouracil (FOLFOX) regimen.
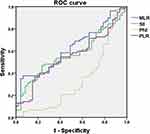
Methods: Based on the cut-off values identified using the receiver-operating characteristic (ROC) curve, 124 patients with HCC who received HAIC with the FOLFOX regimen were divided into low- and high-score MLR, PLR, PNI, and SII groups. Univariate and multivariate regression analyses were performed to identify independent predictors of treatment response and progression-free survival (PFS).
Results: The cut-off values were 0.569 for MLR (area under the curve [AUC]: 0.621), 177.01 for PLR (AUC: 0.554), 713.05 for SII (AUC: 0.570), and 46.85 for PNI (AUC: 0.665). Multivariate Cox regression analysis revealed that the modified albumin-bilirubin (mALBI) grade (hazard ratio [HR]: 2.027; P=0.032), high MLR (HR: 7.250; P=0.002), and low PNI (HR: 0.296; P=0.003) were independent predictors of HAIC non-response, with an AUC value of 0.746 (95% CI: 0.658– 0.833). A high MLR (HR: 1.714, 95% CI: 1.086– 2.704, P=0.021) was also an independent predictor of PFS. Kaplan–Meier analysis showed that the patients with a high MLR had shorter PFS than those with a low MLR (median PFS: 6 vs 10 months, P=0.011).
Conclusion: The pre-treatment MLR and PNI were predictors of non-response in patients with HCC receiving HAIC with the FOLFOX regimen. The MLR also was an independent predictor of PFS.
Keywords: hepatocellular carcinoma, inflammatory biomarkers, treatment response, hepatic arterial infusion chemotherapy, progression-free survival
Introduction
Liver cancer is a common malignancy of the digestive system. According to the latest data on the global burden of cancer in 2020, there were up to 906,000 new cases of primary liver cancer and 830,000 deaths worldwide,1 of which hepatocellular carcinoma (HCC) accounted for the majority, far more than intrahepatic cholangiocarcinoma and other rare types. Because HCC has non-specific symptoms, a high degree of malignancy, and rapid development, most HCC cases are diagnosed at the middle or advanced stage of the tumour, and the opportunity for surgical resection and the optimal period for radical treatment are missed.2
Currently, sorafenib and lenvatinib are recognised as first-line therapies for advanced HCC based on their proven survival benefit and non-inferiority. However, the objective response rate of tumours to this treatment is low, and the survival advantage of sorafenib in these patients is only modest.3,4 Therefore, seeking new effective treatments for middle- and advanced-stage HCC is key to improving the overall survival of patients with HCC. In recent years, some studies have conducted innovative reforms in HAIC to apply the oxaliplatin-based FOLFOX regimen, which improved the survival rate.5–7 In addition, some retrospective studies have shown that the HAIC responders had significantly higher survival rates than HAIC non-responders.8,9 Therefore, it can be used as an effective alternative for the first-line treatment of advanced HCC. The ability to predict treatment response and select patients who will not respond to HAIC is of great significance for the clinical management of unresectable HCC.
In recent years, a growing number of studies have revealed a relationship between inflammatory responses and malignant tumours.10 Inflammation usually occurs before a tissue becomes cancerous and plays a vital role in tumour progression, including initiation, angiogenesis, invasion, and metastasis. Evidence suggests that some inflammatory biomarkers, including the PLR, MLR, PNI, and SII, can predict the treatment response and prognosis in patients with HCC.11–14 However, to the best of our knowledge, no studies have explored the predictive value of these inflammatory biomarkers for determining the postoperative efficacy and prognosis of HAIC using the FOLFOX regimen.
Therefore, we conducted a retrospective study with HCC cases treated with HAIC and aimed to investigate pre-treatment parameters including MLR, PLR, PNI, and SII for their ability to predict treatment response and prognosis in patients with HCC receiving HAIC with FOLFOX regimen.
Materials and Methods
Patients
A total of 124 patients with HCC who received HAIC with the FOLFOX regimen as the initial treatment at the hospital from November 2020 and October 2021 were included. This retrospective single-centre study was conducted in accordance with Declaration of Helsinki and complied with relevant data protection and privacy regulations. The study protocol has been approved by the Medical Ethics Committee of Hunan Cancer Hospital, the Affiliated Cancer Hospital of Xiangya School of Medicine, Central South University. Written informed consent was waived, given the retrospective study design. The primary inclusion criteria were as follows: (1) patients diagnosed with HCC through pathological or imaging examination according to the American Association for the Study of Liver Diseases practice guidelines; (2) patients without other HCC-related treatments before HAIC; (3) expected survival of more than 3 months; (4) Child-Pugh stage A or B; and (5) performance status (PS) score < 2. The exclusion criteria were as follows: (1) loss to follow-up or incomplete follow-up data; (2) lack of sufficient clinical data to assess treatment response and PFS; and (3) history of other malignant tumours.
HAIC Therapy Procedure
The patients were informed of the treatment protocols, and informed consent was obtained. The Seldinger technique was used to puncture the unilateral femoral artery, and a 5F RH catheter was used to perform celiac and common hepatic artery angiography (if necessary, superior mesenteric artery, right renal artery, and phrenic artery angiography) to confirm the location, number, size, and target vessels of the tumour. The microcatheter was then used to superselectively enter the tumour-feeding artery, indwelling catheter, and catheter sheath, and was returned to the ward for FOLFOX4 chemotherapy. The FOLFOX4 regimen on day 1: oxaliplatin 85 mg/m2 infusion, leucovorin 200 mg/m2 infusion, followed by fluorouracil (400 mg/m2 intravenous bolus; 600 mg/m2 22h continuous infusion); on day 2: leucovorin 200 mg/m2 infusion, followed by fluorouracil (400 mg/m2 intravenous bolus; 600 mg/m2, 22h continuous infusion). All chemotherapy drugs were infused using an indwelling arterial catheter every 3 weeks for the treatment cycle.
Follow-Up and Definitions
All enrolled patients underwent blood tests within three days before HAIC treatment, routine blood examinations every three weeks, and imaging examinations every six weeks. The criteria for treatment termination included image-proven progressive disease (PD), intolerable adverse events, death, or patient refusal for further treatment. The primary endpoint was PFS, defined as the time from the start of treatment to the time of imaging evaluation of progression, death, or end day of follow-up. The objective response rate (ORR) was defined as the percentage of patients with complete remission (CR) and partial remission (PR), and the disease control rate (DCR) was defined as the percentage of patients with CR, PR, and stable disease (SD). We compared the HAIC treatment response between non-responders (PD + SD) and responders (CR + PR). To reduce the possibility of errors, two radiologists independently evaluated the treatment response using the RECIST criteria. The follow-up ended in October 2022.
Data Collection
Neutrophil, lymphocyte, monocyte, and platelet counts were recorded from the peripheral blood before the initial HAIC. Clinical laboratory examinations included hepatitis B virus (HBV), alpha-fetoprotein (AFP), aspartate transaminase (AST), alanine aminotransferase (ALT), total bilirubin (TBIL), albumin (ALB), and prothrombin time (PT). The albumin-bilirubin (ALBI) score was calculated using the following formula: −0.085 × (albumin g/l) + 0.66 × log (bilirubin μmol/l). The modified ALBI grade (mALBI grade) was defined by the following: ≤ −2.60 = Grade 1; > −2.60 to ≤ −2.27 = Grade 2a; > −2.27 to ≤ −1.39 = Grade 2b; > −1.39 = Grade 3.15 Four inflammatory biomarkers (SII, PNI, PLR, and MLR) were used to predict the prognosis of patients with HCC after HAIC. The formula is as follows:
Statistical Analysis
Statistical analyses were performed using the R3.5.1 software and SPSS (version 20.0; IBM SPSS, Armonk, NY, USA) and statistical significance was set at p < 0.05. The optimal cut-off values for MLR, PLR, PNI, and SII were calculated according to the HAIC response using ROC curves. The patients were divided into low- and high-scoring groups based on these cut-off values. We compared patient demographics using the χ2 or Fisher’s exact test. PFS was calculated according to the Kaplan–Meier method, and differences were assessed using the log–rank test. To screen for significant prognostic factors for PFS, we conducted univariate and multivariate Cox proportional hazard regression analyses and calculated hazard ratios (HRs) and confidence intervals (CI).
Results
Patient Characteristics
A total of 124 patients receiving HAIC with the FOLFOX regimen were enrolled in this study (median age, 52.5; interquartile range (IQR), 43–60 years; 15 women and 109 men), and their clinical characteristics are summarised in Table 1. The numbers of patients who presented with CR, PR, SD, and PD were 0 (0%), 47 (37.9%), 31 (25.0%), and 46 (37.1%), respectively. The ORR and DCR were 37.9% and 62.9%, respectively. Patients were divided into high- and low-score groups based on the cut-off values of MLR (0.569, AUC = 0.621), PLR (177.01, AUC = 0.554), SII (713.05, AUC = 0.570), and PNI (46.85, AUC = 0.665) (Figure 1).
 |
Table 1 Baseline Characteristics of the 124 Patients |
Associations Between Inflammatory Biomarkers and Response to HAIC
Among the 124 patients, 47 (37.9%) were defined as HAIC responders (CR + PR) and 77 (62.1%) were defined as HAIC non-responders (SD + PD). In univariate analysis, the following six variables were significantly associated with HAIC non-response: ALB ≤ 35 (P = 0.034), mALBI grade (P = 0.002), high PLR (P = 0.024), high MLR (P = 0.001), high SII (P = 0.011), and low PNI (P < 0.001). Furthermore, these variables were integrated into a multivariate logistic regression analysis. Multivariate analysis indicated that mALBI grade (HR = 2.027; P = 0.032), high MLR (HR = 7.250; P = 0.002), and low PNI (HR = 0.296; P = 0.003) were independent predictors of HAIC non-response, with an AUC value of 0.746 (95% CI = 0.658–0.833) (Table 2). A nomogram of these results for HAIC non-response risk is shown in Figure 2.
 |
Table 2 Univariate and Multivariate Analyses for Evaluation of HAIC Response |
Associations Between MLR, PNI and Baseline Characteristics
To further investigate the prognostic value of the MLR and PNI in patients with HCC after HAIC treatment, we analysed the relationship between the MLR, PNI, and related clinical features. We found that high levels of MLR were significantly associated with ALB ≤ 35 (P = 0.007), PT > 13s (P = 0.032), and mALBI grade (P = 0.012). A low PNI was significantly associated with Child-Pugh class B (P = 0.003), AST > 40U/L (P = 0.025), ALB ≤ 35 (P < 0.001), and mALBI grade (P < 0.001) (Table 3).
 |
Table 3 Association Between Inflammatory Markers and Clinical Data |
Prognostic Factors for PFS
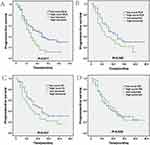
The median PFS was 8 months (range: 1–24) in this study. Twenty-one (16.9%) patients died at the end of the follow-up period. In univariate analysis, the following two variables were associated with PFS: age ≥ 60 years (P = 0.049), and a high MLR (P = 0.017). In the multivariate analysis, only the high MLR (HR = 1.714, P = 0.021, 95% CI: 1.086–2.704) was an independent predictor of PFS (Table 4). Furthermore, Kaplan–Meier curve indicated that patients with a high MLR level had shorter PFS than those with a low MLR level (median PFS: 6 vs 10 months, P = 0.011). In contrast, there were no statistical differences in PFS between the high and low PLR, SII, and PNI groups (Figure 3).
 |
Table 4 Cox Regression Analysis for PFS of HCC Patients |
Discussion
In recent years, the limitations of first-line therapy for patients with advanced HCC have attracted considerable attention, and improving the long-term survival of these patients has become a focus of clinical research. According to Guidelines for HCC Management by the American Association for the Study of Liver Diseases, sorafenib is a first-line therapy for patients with advanced HCC.16,17 In addition to sorafenib, which is recommended by the guidelines of many countries, other molecular-targeted drugs such as lenvatinib and regorafenib, and PD1 monoclonal antibodies such as nivolumab and pembrolizumab, have also made great progress in the treatment of advanced HCC.18–20 However, the overall 5-year survival rate of patients with advanced HCC remains relatively low. Therefore, there is an urgent need for new remedial or alternative treatments.
Previous studies have confirmed that FOLFOX-based HAIC therapy for advanced HCC significantly improves the survival of patients with acceptable toxicity. However, although HAIC has a good therapeutic effect in advanced HCC, the low ORR significantly limits the prognosis of advanced HCC, especially in patients with venous invasion. Therefore, the effective evaluation of treatment response and prognosis before starting HAIC remains an unsolved clinical problem.
HCC is a typical type of inflammation-driven carcinoma, and most cases occur due to chronic inflammation and liver fibrosis.21 The tumour microenvironment contains a variety of cytokines and chemokines that can promote tumour growth and inhibit white blood cells from attacking tumour cells.22 Neutrophils can promote the adhesion and seeding of tumour cells in distant organs by circulating growth factors such as vascular endothelial growth factor (VEGF) and secreting proteases.23,24 Lymphocytes play an important role in adaptive immune responses to tumours or viral infections. By inhibiting the tumour cells from proliferating and metastasising, lymphocytes maintain the immune balance of cancer cells to inhibit tumor development.25,26 A low lymphocyte count is associated with systemic inflammatory response and may accelerate cancer progression by affecting cell-mediated immunity.
Lymphocytes within the tumour microenvironment are of vital importance in determining the efficacy of immune surveillance and lethality.27 In addition, some studies have shown that activated circulating monocytes secrete various pro-inflammatory cytokines and participate in the occurrence and progression of tumours.28 Therefore, modulation of the tumour inflammatory microenvironment and inflammatory markers is part of the systemic inflammatory response, which is closely connected to all stages of cancer development and has an impact on the treatment response and the disease prognosis.29,30
According to several studies, the levels of PNI, MLR, PLR, and SII before treatment may be independent prognostic factors for advanced HCC. These inflammatory markers, which are inexpensive clinical parameters that do not require complicated detection, have broad clinical application prospects. In this study, we evaluated the HAIC response of patients in the high PNI, MLR, PLR, and SII group and the low PNI, MLR, PLR, and SII group, respectively. In the univariate analysis, in addition to common clinical prognostic factors (ALB level and mALBI grade), PNI, MLR, PLR, and SII were all correlated with a negative response to HAIC treatment. In multivariate analyses, only the mALBI grade, PNI, and MLR remained independent prognostic factors for treatment response to HAIC. Meanwhile, through ROC curve analysis, this study concluded that the optimal cut-off values of PNI and MLR were 46.85 and 0.569, respectively, and the areas under the ROC curve were 0.665 and 0.621, respectively. Furthermore, the area under the ROC curve was 0.746 (95% CI = 0.658–0.833) when the mALBI grade, PNI, and MLR were combined to predict the response to HAIC treatment, which showed higher reliability.
We further studied the relationship between these inflammatory indices and the survival benefits. The univariate COX analysis found that MLR and age ≥ 60 were important factors affecting PFS in patients with HCC receiving HAIC treatment. In multivariate COX analyses, only MLR was used as an independent predictor of PFS. Therefore, our study suggests that inflammatory markers, particularly MLR, may be more effective than traditional clinical prognostic factors for predicting the efficacy and prognosis of HAIC treatment.
The cost of MLR inspection is low and it can be obtained by repeated calculations of the monocyte/lymphocyte ratio. Mao et al12 suggested that MLR was an independent prognostic factor for recurrence-free survival (RFS) in AFP-negative HCC after surgical resection, and an MLR-based nomogram model for RFS showed high predictive accuracy. Wu et al31 reported that a combined model including MLR and other clinical risk factors may help clinicians identify patients with high-risk HCC with early recurrence and improve their prognosis.
In addition, our study found that a low PNI was significantly associated with non-response to HAIC in univariate and multivariate analyses. Mei et al13 demonstrated that PNI is the best tool for predicting treatment response and prognosis in patients with liver cancer receiving PD-1 treatment compared with other inflammatory markers. The PNI, the combination of lymphocytes and albumin, reflects the nutritional and inflammatory status of the organism. Low serum albumin levels indicate a state of malnutrition, which weakens the patient’s cellular and humoral immunity, as well as other defence mechanisms. Some studies have found that nutritional status is closely related to the therapeutic effect and prognosis of patients with advanced liver cancer receiving anti-PD-1 treatment.32
Our study also showed that the levels of MLR and PNI were correlated with the clinical characteristics of patients with HCC, such as Child-Pugh class, mALBI grade, ALB level, and PT. This suggests that, to a certain extent, high MLR and low PNI can reflect the severity of HCC. Therefore, our findings provide individualised treatment options for patients with HCC in clinical practice by evaluating baseline inflammatory biomarkers before treatment. Patients with high MLR and low PNI levels can be selected for first-line treatments, such as sorafenib and apatinib, instead of HAIC.
However, this study had some limitations. This was a retrospective study conducted at a single institution. In addition, the number of patients included was relatively small, and the reliability of the results needs to be demonstrated in more centres and patients. Furthermore, many factors affect the postoperative prognosis of patients. Therefore, more comprehensive indicators are needed to evaluate the prognosis of patients with HCC treated with HAIC.
Conclusion
In conclusion, the pre-treatment MLR and PNI showed favourable performance in predicting treatment response and prognosis in patients with HCC receiving HAIC with the FOLFOX regimen. The nomogram based on MLR and PNI can be applied by clinicians to choose the reasonable option to reduce unnecessary HAIC treatment.
Author Contributions
All authors made substantial contribution to the work reported, whether that is in the conception, execution, study design, acquisition of data, interpretation and analysis, or in all these areas; took part in drafting the article or revising it critically; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work has been supported by the Natural Science Foundation of Hunan Province (Grant Number: 2021JJ30423, Changsha, China), and the Hunan Cancer Hospital Climb Plan (Grant Number: ZX2020002, Changsha, China).
Disclosure
There was no conflict of interest in this paper for all authors.
References
1. Sung H, Ferlay J, Siegel R, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Galle PR, Forner A, Llovet JM, et al. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236. doi:10.1016/j.jhep.2018.03.019
3. Marrero J, Kudo M, Venook A, et al. Observational registry of sorafenib use in clinical practice across Child-Pugh subgroups: the GIDEON study. J Hepatol. 2016;65(6):1140–1147.
4. Cheng A, Kang Y, Chen Z, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a Phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10(1):25–34.
5. Lyu N, Kong Y, Mu L, et al. Hepatic arterial infusion of oxaliplatin plus fluorouracil/leucovorin vs. sorafenib for advanced hepatocellular carcinoma. J Hepatol. 2018;69(1):60–69.
6. He M, Zou R, Li Q, et al. Phase II study of sorafenib combined with concurrent hepatic arterial infusion of oxaliplatin, 5-fluorouracil and leucovorin for unresectable hepatocellular carcinoma with major portal vein thrombosis. Cardiovasc Intervent Radiol. 2018;41(5):734–743.
7. Korean Liver Cancer Association. 2018 Korean Liver Cancer Association-National Cancer Center Korea practice guidelines for the management of hepatocellular carcinoma. Korean J Radiol. 2019;20(7):1042–1113.
8. Nagano H, Wada H, Kobayashi S, et al. Long-term outcome of combined interferon-α and 5-fluorouracil treatment for advanced hepatocellular carcinoma with major portal vein thrombosis. Oncology. 2011;80:63–69.
9. Miyaki D, Aikata H, Honda Y, et al. Hepatic arterial infusion chemotherapy for advanced hepatocellular carcinoma according to Child-Pugh classification. J Gastroenterol Hepatol. 2012;27(12):1850–1857.
10. Templeton A, McNamara M, Šeruga B, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):dju124. doi:10.1093/jnci/dju124
11. Liu Y, Shi M, Chen S, et al. Intermediate stage hepatocellular carcinoma: comparison of the value of inflammation-based scores in predicting progression-free survival of patients receiving transarterial chemoembolization. J Cancer Res Ther. 2021;17(3):740–748. doi:10.4103/jcrt.jcrt_29_21
12. Mao S, Yu X, Shan Y, Fan R, Wu S, Lu C. Albumin-Bilirubin (ALBI) and Monocyte to Lymphocyte Ratio (MLR)-based nomogram model to predict tumor recurrence of AFP-negative hepatocellular carcinoma. J Hepatocell Carcinoma. 2021;8:1355–1365. doi:10.2147/JHC.S339707
13. Mei J, Sun X, Lin W, et al. Comparison of the prognostic value of inflammation-based scores in patients with hepatocellular carcinoma after Anti-PD-1 therapy. J Inflamm Res. 2021;14:3879–3890. doi:10.2147/JIR.S325600
14. Xin Y, Yang Y, Liu N, et al. Prognostic significance of systemic immune-inflammation index-based nomogram for early stage hepatocellular carcinoma after radiofrequency ablation. J Gastrointest Oncol. 2021;12(2):735–750. doi:10.21037/jgo-20-342
15. Atsushi H, Takashi K, Kunihiko T, et al. Validation of modified ALBI grade for more detailed assessment of hepatic function in hepatocellular carcinoma patients: a multicenter analysis. Liver Cancer. 2018;7:1–9. doi:10.1159/000487148
16. Bruix J, Gores G, Mazzaferro V. Hepatocellular carcinoma: clinical frontiers and perspectives. Gut. 2014;63(5):844–855. doi:10.1136/gutjnl-2013-306627
17. Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020–1022. doi:10.1002/hep.24199
18. Dawkins J, Webster R. The hepatocellular carcinoma market. Nat Rev Drug Discov. 2019;18(1):13–14. doi:10.1038/nrd.2018.146
19. Bruix J, Qin S, Merle P, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, Phase 3 trial. Lancet. 2017;389(10064):56–66. doi:10.1016/S0140-6736(16)32453-9
20. El-Khoueiry A, Sangro B, Yau T, et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, Phase 1/2 dose escalation and expansion trial. Lancet. 2017;389(10088):2492–2502.
21. Keenan B, Fong L, Kelley R. Immunotherapy in hepatocellular carcinoma: the complex interface between inflammation, fibrosis, and the immune response. J Immunother Cancer. 2019;7(1):267. doi:10.1186/s40425-019-0749-z
22. Binnewies M, Roberts E, Kersten K, et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat Med. 2018;24(5):541–550.
23. Cools-Lartigue J, Spicer J, McDonald B, et al. Neutrophil extracellular traps sequester circulating tumor cells and promote metastasis. J Clin Invest. 2013;123(8):3446–3458.
24. Rossi L, Santoni M, Crabb S, et al. High neutrophil-to-lymphocyte ratio persistent during first-line chemotherapy predicts poor clinical outcome in patients with advanced urothelial cancer. Ann Surg Oncol. 2015;22(4):1377–1384.
25. Pauken K, Wherry E. Overcoming T cell exhaustion in infection and cancer. Trends Immunol. 2015;36(4):265–276.
26. Park S, Buzzai A, Rautela J, et al. Tissue-resident memory CD8 T cells promote melanoma-immune equilibrium in skin. Nature. 2019;565(7739):366–371.
27. Chraa D, Naim A, Olive D, Badou A. T lymphocyte subsets in cancer immunity: friends or foes. J Leukoc Biol. 2019;105(2):243–255.
28. Lippitz B, Harris R. Cytokine patterns in cancer patients: a review of the correlation between interleukin 6 and prognosis. Oncoimmunology. 2016;5(5):e1093722.
29. Ramakrishna G, Rastogi A, Trehanpati N, Sen B, Khosla R, Sarin S. From cirrhosis to hepatocellular carcinoma: new molecular insights on inflammation and cellular senescence. Liver Cancer. 2013;2:367–383.
30. Chen Q, Li F, Zhong C, et al. Inflammation score system using preoperative inflammatory markers to predict prognosis for hepatocellular carcinoma after hepatectomy: a cohort study. J Cancer. 2020;11(17):4947–4956.
31. Wu Y, Tu C, Shao C. Inflammatory indexes in preoperative blood routine to predict early recurrence of hepatocellular carcinoma after curative hepatectomy. BMC Surg. 2021;21(1):178.
32. Jiang Y, Tu X, Zhang X, et al. Nutrition and metabolism status alteration in advanced hepatocellular carcinoma patients treated with anti-PD-1 immunotherapy. Support Care Cancer. 2020;28(11):5569–5579.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.