Back to Journals » International Journal of General Medicine » Volume 16
The Potential Value of Systemic Inflammation Response Index on Delirium After Hip Arthroplasty Surgery in Older Patients: A Retrospective Study
Authors Lu W , Lin S , Wang C, Jin P, Bian J
Received 25 June 2023
Accepted for publication 18 October 2023
Published 21 November 2023 Volume 2023:16 Pages 5355—5362
DOI https://doi.org/10.2147/IJGM.S427507
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Wenbin Lu,* Shengwei Lin,* Cheng Wang, Peipei Jin, Jinjun Bian
Faculty of Anesthesiology, Changhai Hospital, Naval Medical University/Second Military Medical University, PLA, Shanghai, 200433, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Peipei Jin; Jinjun Bian, Faculty of Anesthesiology, Changhai Hospital, Naval Medical University, 168, Changhai Road, Shanghai, 200433, People’s Republic of China, Tel/Fax +86-021-31161886 ; +86-021-31161841, Email [email protected]; [email protected]
Purpose: To explore the relationship between the systemic inflammation response index (SIRI) and postoperative delirium (POD) in older patients with hip arthroplasty surgery.
Patients and Methods: Older patients who underwent elective hip arthroplasty surgery were included in this retrospective study. SIRI, neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) were collected from blood routine examination at admission. Binary logistic regression analysis was performed to evaluate the association between SIRI levels and POD was analyzed.
Results: Ultimately, 116 older patients who met the inclusion criteria were assessed. Thirty-four (29%) of 116 patients diagnosed with POD were defined as the POD group, and the rest consisted of the Non-POD group. Compared with non-POD patients, POD patients showed significantly higher levels of SIRI (P < 0.001) and NLR (P = 0.002) at admission. There was no significance in the levels of PLR between two groups. SIRI was independently associated with the occurrence of POD in multivariate logistic regression analysis [odds ratio (OR) = 3.34, 95% confidence interval (95% CI) = 1.26– 8.85, P = 0.016]. Receiver operating characteristic curve analysis indicated that SIRI with an optimal cutoff value of 0.987 predicted the POD with a sensitivity of 88.2% and specificity of 74.4%, and the area under the curve was 0.82 (95% CI, 0.74– 0.90, P < 0.01).
Conclusion: Preoperative SIRI and NLR levels in the blood are associated with the occurrence of POD. Moreover, preoperative SIRI level is a useful candidate biomarker to identify delirium after elective hip arthroplasty surgery in older patients.
Keywords: geriatric, hip arthroplasty, neutrophil to lymphocyte ratio, postoperative delirium, platelet to lymphocyte ratio, systemic inflammation response index
Introduction
Postoperative delirium (POD) remains one of most common complication in older patients receiving surgery, which is characterized by acute and fluctuating alteration in the level of consciousness and cognition.1 Previous study reported that the incidence of delirium after surgery ranges from 20% to 45% among older patients.2 POD is linked to with neuropsychiatric symptoms, longer hospital stay, higher medical expenditures and lower in activities of daily living,3–5 especially in older patients. More importantly, POD can also potentially be associated with the long-term cognitive dysfunction, dementia and even an increase in mortality.6,7 Recent study showed that POD is harbinger of postoperative cognitive decline which have more significant long-term repercussion on patient health.8 Although pathological mechanisms associated with POD have been investigated, its treatment remains a challenge for clinicians.9 Therefore, identifying the risk factors of delirium can contribute to the prevention and early recognition of delirium after hip arthroplasty surgery in older patients.
Despite that series of risk scores and predictive model for postoperative delirium have been identified,10–12 easily accessible and effective prediction of delirium after surgery remains unknown. Previous clinical and animal studies have shown that surgery and anesthesia-induced acute peripheral inflammation and neuroinflammation may lead to delirium after surgery.13,14 Mounting evidence has shown that inflammatory markers including elevated neutrophil, monocyte and reduced lymphocyte count, have been reported in various clinical setting.15–17 Indeed, elevated neutrophil and reduced lymphocyte count has also reported in delirium in older adults.18 Systemic Inflammation Response Index (SIRI) is a more easily accessible and comprehensive inflammation marker derived from monocyte, neutrophil, and lymphocyte count, which has been investigated to assess the prognosis of cancer and infectious diseases.19–21 However, the relationship between SIRI and POD has yet to be investigated.
Therefore, the purpose of this study is to evaluate the association between SIRI and delirium after hip arthroplasty surgery in older patients and to examine the value of SIRI on predicting POD. For this aim, the present study was conducted to provide a new method for the early recognition and perioperative management of POD in older patients who underwent hip arthroplasty.
Materials and Methods
Study Design and Patients
We conducted a retrospective study of patients who underwent elective hip arthroplasty in the Faculty of Anesthesiology of Changhai Hospital between March 2019 and October 2019. The Ethics Committee of our hospital approved this study (CHE2018-133) which was registered in Clinicaltrials.gov (NCT05797194). All eligible patients gave written informed consent.
Eligible patients were scheduled to undergo elective hip arthroplasty under spinal anesthesia (using an Isobaric solution of 0.75% bupivacaine 1.5–2 mL) with an anticipated length of stay of at least 3 days and received postoperative patient-controlled analgesia. Patients with 65 years of age and above, American Society of Anesthesiologists (ASA) physical status I–III, elementary education or above, able to communicate, and Mini-mental State Examination (MMSE) scores ≥22 points were included. Exclusion criteria included preoperative delirium, history of nervous system diseases, severe mental diseases, chronic infectious diseases, and autoimmune-illness or malignancies.
Data Collection
Baseline characteristics on age, gender, body mass index (BMI), ASA Physical Status Classification, preoperative MMSE scores, educational level, operation during, and medical history were recorded in this study. Medical history included history of cardiac disease (atrial fibrillation, history of heart failure, valvular disease, coronary artery disease), hypertension, diabetes mellitus and hyperlipidemia. In addition, neutrophil, lymphocyte, monocyte and platelet were recorded from blood routine examination at admission. NLR was calculated as neutrophil count/lymphocyte count, PLR was calculated as platelet count/lymphocyte count, and SIRI was calculated as neutrophil count × monocyte count/lymphocyte count.19
Assessment of Delirium and Cognition
Delirium assessment was performed at the preoperative baseline visit, then twice daily for 3 days after surgery. Cognition assessment was conducted at preoperative visit, 24 h after surgery and 72 h after surgery. The morning and evening delirium assessments were made before 10 AM and after 5 PM in the ward. The confusion assessment method (CAM) questionnaire and cognition assessment method for MMSE were performed by qualified doctor who trained with CAM and MMSE training manual. Patients were determined to have incident postoperative delirium by a positive CAM questionnaire after surgery.22 In this study, we used the Chinese mini-mental status (CMMS) test, a Chinese version of the MMSE revised by Professor Zhang Mingyuan,23 to assess cognitive function.
Statistical Analysis
Statistical analyses were performed by the SPSS 23.0 and R 4.1.3 software. Continuous variables with normally distributed data were presented as mean (SD) and were compared using Student’s t-test. Mann–Whitney U-test was used to compare continuous variables in non-normal distribution data described as medians (quartiles). Categorical variables were presented as frequency and χ²-test, or Fisher’s exact test was used to compare differences between survivors and non-survivors where appropriate. The optimal cut-off value for SIRI was calculated by receiver operating characteristic curve analysis with the highest Youden’s index (sensitivity + specificity – 1) to predict POD. After adjusting for confounding factors such as age, gender, BMI, preoperative MMSE scores, education, operation duration and ASA Physical Status Classification, the relationship between SIRI, NLR, PLR and POCD was analyzed by binary logistic regression analysis using the enter method, P<0.05 was considered statistically significant.
Results
In total, 116 older patients were eligible in the study, where 34 patients (29%) diagnosed with POD were defined as the POD group. The rest consisted of the Non-POD group (Supplementary Figure 1).
Baseline Characteristics and Inflammation Indicators
Table 1 shows baseline information for all patients. We found that patients with delirium after surgery had lower postoperative MMSE scores than patients without delirium (P < 0.001). Compared with Non-POD group, POD group had significantly higher levels of SIRI (P < 0.001) and NLR (P = 0.002). However, there was no difference between two groups in other variables. Besides, the violin plots also showed the differences in the distribution of the SIRI levels between two groups (Figure 1).
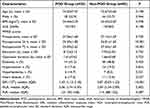 |
Table 1 Baseline Characteristics and Inflammatory Parameters of the Study Population |
Predictors of Delirium After Surgery
We conducted univariate and multivariate logistic regression analyses in order to investigate the association between inflammation indicators and delirium after orthopedics surgery. We found that high level of SIRI was an independent risk factor for POD (OR = 3.34, 95% CI = 1.26–8.85, P = 0.016) after adjusting for age, gender, BMI, preoperative MMSE scores, educational level, NLR and PLR (Table 2).
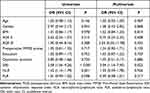 |
Table 2 Univariate and Multivariate Logistic Regression Analysis Showing the Independent Predictors of POD |
Receiver operator characteristics curve analysis indicated that the SIRI had the best predictive power for POD among the inflammatory indicators, and the area under the curve was 0.82 (95% CI, 0.74–0.90, P < 0.01) (Figure 2). The optimal cut-off value for SIRI to predict POD was 0.987 calculated by highest Youden’s index with an 88.2% sensitivity and 74.4% specificity.
Discussion
In our study, the relationship between SIRI level and POD was investigated for the first time. Our results showed that nearly one-third of patients developed POD, and patients with high levels of SIRI and NLR were susceptible to POD. In addition, we found that SIRI > 0.987 was a valuable marker for predicting POD with a sensitivity of 88.2% and specificity of 74.4%.
A growing number of studies have shown that preoperative inflammatory mediators were associated with delirium after surgery, and surgery or anesthesia-induced inflammation and immune response involved in the pathogenesis of POD.24,25 Preoperative dexamethasone administration can reduce the incidence and severity of early cognitive decline after surgery by decreasing inflammatory response prompted by surgery.26 Previous studies have shown that NLR was related to delirium and cognitive decline after surgery which was consistent with our research.27,28 Neutrophils, lymphocytes and monocytes are an important part of peripheral immune system. And the immune inflammatory response in the brain, which is driven by proinflammatory cytokines derived from peripheral immune cells, may cause the activation of microglial cells resulting in delirium after surgery.29,30 Therefore, as comprehensive inflammation index, NLR and SIRI may be better predictive parameters of immunity and inflammatory diseases.
NLR and SIRI are calculated from neutrophils, monocytes and lymphocytes which are major contributors to acute inflammation.31 Stress response involved in trauma, surgery and anesthesia can result in activation of peripheral immune system, increasing neutrophils and monocytes count as well as lowering lymphocytes count.32 Once activated, neutrophils and monocytes can release oxygen-free radicals, chemokines and inflammatory cytokines which might be potential mechanisms for POD. In addition, recent studies have shown that SIRI was associated with clinical outcomes in patients with stroke.33,34 Furthermore, previous study showed that SIRI was an independent risk factor for mortality in patients with acute myocardial infarction.35 In the present study, we found that patients with POD had higher NLR and SIRI before surgery. In addition, we showed that preoperative SIRI was a better predictor for delirium after surgery among the inflammatory indicators.
Our investigation mainly suggested that older patients with SIRI > 0.987 were more prone to suffering from delirium after surgery. In addition, this study added an important evidence on the association between alteration in peripheral immune cells and delirium after surgery. Monitoring dynamic changes in NLR and SIRI was an accessible and effective method for POD screening and management. Higher preoperative SIRI could give some clinical clues to perioperative clinicians in order to early recognition and management of delirium after surgery. This may also provide a new insight into the prevention and treatment of POD.
There are some unavoidable limitations in this study. Firstly, we collected a single SIRI and NLR, instead of dynamic changes of them, which may contribute to understanding of development for POD. Secondly, this is a single-center study recruiting patient with hip arthroplasty only which may result in bias. Thirdly, patients with MMSE < 22 were rejected, which affects the generalizability of the results. Fourthly, the sample size calculation was not performed due to the retrospective exploratory study. Lastly, multi-center clinical large samples need to verify the value of SIRI on the prediction for delirium after surgery in older patients. Despite these limitations, it is the first study to investigate the link between SIRI and POD in older patients with hip arthroplasty surgery.
Conclusion
In summary, our study revealed that the levels of preoperative SIRI and NLR were associated with delirium after hip arthroplasty surgery among older patients. More importantly, we found that SIRI was an independent risk factor for delirium after hip arthroplasty surgery. Therefore, peripheral immune indicators may provide a measure for initial assessment and provide new insights into the prevention and treatment of delirium after hip arthroplasty surgery in older patients.
Data Sharing Statement
The data supporting the findings of this study can be obtained from the corresponding author according to reasonable request, and the corresponding author/s can be directly contacted for further inquiry.
Ethics Statement
The study concerning human participants was reviewed and approved by the ethics committee of Shanghai Changhai Hospital. The patients/participants participated in the study by providing written informed consent. The study project conforms to the ethical guidelines of the Declaration of Helsinki. In order to publish any potentially identifiable images or data contained in this article, written informed consent was obtained from the individual(s).
Acknowledgments
We thank all those who support and participate in the study, including our staff, patients and their family members. We also thank Xueqian Leng (Faculty of Anesthesiology, Changhai Hospital, Naval Military Medical University) for guidance in revising the manuscript and submission of the manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by the National Natural Science Foundation of China (81871579 and 82272205). The sponsor had no role in the manuscript’s design, conduct, drafting, or publication.
Disclosure
The authors state that the study was conducted without any commercial or financial relationships and potential conflicts of interest.
References
1. Tao M, Zhang S, Han Y, et al. Efficacy of transcranial direct current stimulation on postoperative delirium in elderly patients undergoing lower limb major arthroplasty: a randomized controlled trial. Brain Stimul. 2023;16(1):88–96. doi:10.1016/j.brs.2023.01.839
2. Daiello LA, Racine AM, Yun Gou R, et al. Postoperative delirium and postoperative cognitive dysfunction: overlap and divergence. Anesthesiology. 2019;131(3):477–491. doi:10.1097/ALN.0000000000002729
3. Yang KL, Detroyer E, Van Grootven B, et al. Association between preoperative anxiety and postoperative delirium in older patients: a systematic review and meta-analysis. BMC Geriatr. 2023;23(1):198. doi:10.1186/s12877-023-03923-0
4. Barnes J, Sewart E, Armstrong RA, et al. Does melatonin administration reduce the incidence of postoperative delirium in adults? Systematic review and meta-analysis. BMJ open. 2023;13(3):e069950. doi:10.1136/bmjopen-2022-069950
5. Zhao S, Sun T, Zhang J, Chen X, Wang X. Risk factors and prognosis of postoperative delirium in nonagenarians with Hip fracture. Sci Rep. 2023;13(1):2167. doi:10.1038/s41598-023-27829-4
6. Patel M, Onwochei DN, Desai N. Influence of perioperative dexmedetomidine on the incidence of postoperative delirium in adult patients undergoing cardiac surgery. Br J Anaesth. 2022;129(1):67–83. doi:10.1016/j.bja.2021.11.041
7. Kunicki ZJ, Ngo LH, Marcantonio ER, et al. Six-year cognitive trajectory in older adults following major surgery and delirium. JAMA Intern Med. 2023;183:442. doi:10.1001/jamainternmed.2023.0144
8. Glumac S, Kardum G, Karanovic N. Postoperative cognitive decline after cardiac surgery: a narrative review of current knowledge in 2019. Med Sci Monit. 2019;25:3262–3270. doi:10.12659/MSM.914435
9. Oh ES, Fong TG, Hshieh TT, Inouye SK. Delirium in older persons: advances in diagnosis and treatment. JAMA. 2017;318(12):1161–1174. doi:10.1001/jama.2017.12067
10. Li GH, Zhao L, Lu Y, et al. Development and validation of a risk score for predicting postoperative delirium after major abdominal surgery by incorporating preoperative risk factors and surgical Apgar score. J Clin Anesth. 2021;75:110408. doi:10.1016/j.jclinane.2021.110408
11. de la Varga-Martínez O, Gómez-Pesquera E, Muñoz-Moreno MF, et al. Development and validation of a delirium risk prediction preoperative model for cardiac surgery patients (DELIPRECAS): an observational multicentre study. J Clin Anesth. 2021;69:110158. doi:10.1016/j.jclinane.2020.110158
12. de la Varga-Martínez O, Gómez-Pesquera E, Muñoz-Moreno MF, et al. Influence of intraoperative and postoperative factors on the predictive capacity of the delirium risk model for cardiac surgery patients (DELIPRECAS): an observational multicentre study. J Clin Anesth. 2021;72:110282. doi:10.1016/j.jclinane.2021.110282
13. Vasunilashorn SM, Dillon ST, Chan NY, et al. Proteome-wide analysis using somascan identifies and validates chitinase-3-like protein 1 as a risk and disease marker of delirium among older adults undergoing major elective surgery. J Gerontol a Biol Sci Med Sci. 2022;77(3):484–493. doi:10.1093/gerona/glaa326
14. Li J, Li L, He J, Xu J, Bao F. The NLRP3 inflammasome is a potential mechanism and therapeutic target for perioperative neurocognitive disorders. Front Aging Neurosci. 2022;14:1072003. doi:10.3389/fnagi.2022.1072003
15. Mirza E, Oltulu R, Katipoğlu Z, Mirza GD, Özkağnıcı A. Monocyte/HDL ratio and lymphocyte/monocyte ratio in patients with pseudoexfoliation syndrome. Ocul Immunol Inflamm. 2020;28(1):142–146. doi:10.1080/09273948.2018.1545913
16. Oltulu R, Katipoğlu Z, Gündoğan AO, Mirza E, Belviranlı S. Evaluation of inflammatory biomarkers in patients with keratoconus. Eur J Ophthalmol. 2022;32(1):154–159. doi:10.1177/11206721211000644
17. Katipoglu B, Aydinli B, Demir A, Ozmen H. Preoperative red cell distribution width to lymphocyte ratio as biomarkers for prolonged intensive care unit stay among older patients undergoing cardiac surgery: a retrospective longitudinal study. Biomark Med. 2022;16(14):1067–1075. doi:10.2217/bmm-2022-0341
18. Katipoglu B, Naharci MI. Could neutrophil-to-lymphocyte ratio predict mortality in community-dwelling older people with delirium superimposed on dementia? Aging Clin Exp Res. 2022;34(8):1819–1826. doi:10.1007/s40520-022-02108-w
19. Hua X, Long ZQ, Huang X, et al. The preoperative systemic inflammation response index (SIRI) independently predicts survival in postmenopausal women with breast cancer. Curr Probl Cancer. 2020;44(4):100560. doi:10.1016/j.currproblcancer.2020.100560
20. Sun L, Hu W, Liu M, et al. High systemic inflammation response index (SIRI) indicates poor outcome in gallbladder cancer patients with surgical resection: a single institution experience in China. Can Res Treat. 2020;52(4):1199–1210. doi:10.4143/crt.2020.303
21. Jin Z, Wu Q, Chen S, et al. The associations of two novel inflammation indexes, SII and SIRI with the risks for cardiovascular diseases and all-cause mortality: a ten-year follow-up study in 85,154 individuals. J Inflamm Res. 2021;14:131–140. doi:10.2147/JIR.S283835
22. Mao M, Wang LY, Zhu LY, et al. Higher serum PGE2 is a predicative biomarker for postoperative delirium following elective orthopedic surgery in elderly patients. BMC Geriatr. 2022;22(1):685. doi:10.1186/s12877-022-03367-y
23. Zhang MY, Katzman R, Salmon D, et al. The prevalence of dementia and Alzheimer’s disease in Shanghai, China: impact of age, gender, and education. Ann Neurol. 1990;27(4):428–437. doi:10.1002/ana.410270412
24. Noah AM, Almghairbi D, Evley R, Moppett IK. Preoperative inflammatory mediators and postoperative delirium: systematic review and meta-analysis. Br J Anaesth. 2021;127(3):424–434. doi:10.1016/j.bja.2021.04.033
25. Wang Y, Shen X. Postoperative delirium in the elderly: the potential neuropathogenesis. Aging Clin Exp Res. 2018;30(11):1287–1295. doi:10.1007/s40520-018-1008-8
26. Glumac S, Kardum G, Sodic L, Supe-Domic D, Karanovic N. Effects of dexamethasone on early cognitive decline after cardiac surgery: a randomised controlled trial. Eur J Anaesthesiol. 2017;34(11):776–784. doi:10.1097/EJA.0000000000000647
27. He R, Wang F, Shen H, Zeng Y, Lijuan Z. Association between increased neutrophil-to-lymphocyte ratio and postoperative delirium in elderly patients with total Hip arthroplasty for Hip fracture. BMC Psychiat. 2020;20(1):496. doi:10.1186/s12888-020-02908-2
28. Lu W, Zhang K, Chang X, Yu X, Bian J. The association between systemic immune-inflammation index and postoperative cognitive decline in elderly patients. Clin Interv Aging. 2022;17:699–705. doi:10.2147/CIA.S357319
29. Bettcher BM, Tansey MG, Dorothée G, Heneka MT. Peripheral and central immune system crosstalk in Alzheimer disease - A research prospectus. Nat Rev Neurol. 2021;17(11):689–701. doi:10.1038/s41582-021-00549-x
30. Wang P, Velagapudi R, Kong C, et al. Neurovascular and immune mechanisms that regulate postoperative delirium superimposed on dementia. Alzheimer’s Dem. 2020;16(5):734–749. doi:10.1002/alz.12064
31. Margraf A, Perretti M. Immune cell plasticity in inflammation: insights into description and regulation of immune cell phenotypes. Cells. 2022;11(11):1824. doi:10.3390/cells11111824
32. Bongers SH, Chen N, van Grinsven E, et al. Kinetics of neutrophil subsets in acute, subacute, and chronic inflammation. Front Immunol. 2021;12:674079. doi:10.3389/fimmu.2021.674079
33. Cheng W, Bu X, Xu C, et al. Higher systemic immune-inflammation index and systemic inflammation response index levels are associated with stroke prevalence in the asthmatic population: a cross-sectional analysis of the NHANES 1999–2018. Front Immunol. 2023;14:1191130. doi:10.3389/fimmu.2023.1191130
34. Zhang YX, Shen ZY, Jia YC, et al. The association of the neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, lymphocyte-to-monocyte ratio and systemic inflammation response index with short-term functional outcome in patients with acute ischemic stroke. J Inflamm Res. 2023;16:3619–3630. doi:10.2147/JIR.S418106
35. Wang Y, Chen H. A nonlinear relationship between systemic inflammation response index and short-term mortality in patients with acute myocardial infarction: a retrospective study from MIMIC-IV. Front Cardiov Med. 2023;10:1208171. doi:10.3389/fcvm.2023.1208171
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


